Abstract
The purpose of this study was to document current practices of dentist anesthesiologists who are members of the American Society of Dentist Anesthesiologists regarding the supplemental use of local anesthesia for children undergoing dental rehabilitation under general anesthesia. A survey was administered via e-mail to the membership of the American Society of Dentist Anesthesiologists to document the use of local anesthetic during dental rehabilitations under general anesthesia and the rationale for its use. Seventy-seven (42.1%) of the 183 members responded to this survey. The majority of dentist anesthesiologists prefer use of local anesthetic during general anesthesia for dental rehabilitation almost always or sometimes (90%, 63/70) and 40% (28/70) prefer its use with rare exception. For dentist anesthesiologists who prefer the administration of local anesthesia almost always, they listed the following factors as very important: “stabilization of vital signs/decreased depth of general anesthesia” (92.9%, 26/28) and “improved patient recovery” (82.1%, 23/28). There was a significant association between the type of practice and who determines whether or not local anesthesia is administered during cases. The majority of respondents favor the use of local anesthesia during dental rehabilitation under general anesthesia.
Key Words: Local anesthesia, Hospital dentistry, General anesthesia, Restorative dentistry
General anesthesia is a form of advanced behavior management utilized by dentists to provide quality dental care for children otherwise unable to tolerate dentistry in an outpatient setting.1 The use of local anesthesia in conjunction with general anesthesia is an area with conflicting research.
The addition of local anesthesia during dental rehabilitations has some potential benefits: decreased postoperative pain, improved hemorrhage control, and reduced need for anesthesiologist intervention. In regards to postoperative pain, Noble et al found in a randomized controlled trial that patients undergoing extractions under general anesthesia in the absence of systemic analgesics were less likely to be distressed upon recovery if local anesthetic infiltration was also utilized.2 Atan et al also found a significant decrease in pain at the operation site in patients who received supplemental local anesthesia.3 In a randomized controlled study, Sammons et al showed a statistically significant decrease in pain following extractions if local anesthesia was added; however, this difference was significant only after 5 minutes.4
The use of local anesthesia with general anesthesia has been advocated to improve physiological parameters during general anesthesia. Watts et al found the heart rate and end-tidal carbon dioxide stayed stable for patients undergoing dental treatment with supplemental local anesthesia versus children under general anesthesia without local anesthesia. In addition, patients with local anesthesia required less frequent anesthesiologist intervention. The change in heart rate and end-tidal CO2 was statistically lower in children with local anesthesia versus children without it.5 Although these physiologic changes are statistically significant, the temporary increase in heart rate and respiratory rate following extraction or crown placement may not be clinically meaningful in the treatment of a healthy child.5,6
Conflicting studies have shown no difference in postoperative pain with the use of local anesthetic in conjunction with general anesthesia.7–9 Al-Bahlani et al did not study postoperative pain but did report a “clear and marked increased in the measures of distress post-operatively” in anesthetized children who received infiltration with local analgesic.10 Topical anesthetics have also been suggested to reduce postoperative pain following general anesthesia, but Gazal et al did not find a difference compared to when topical anesthetics were not used.11 Although some authors have expressed concern that the addition of local anesthesia would increase lip and cheek biting, a statistically significant association between lip and cheek biting and local anesthesia has not been shown.7,8
A recent survey of pediatric dentist and general dentist members of the American Academy of Pediatric Dentistry (AAPD) about their use of local anesthesia on children undergoing dental rehabilitations under general anesthesia found a spectrum of practices and rationales.12
The purpose of this study was to document the current practices of dentists who are members of the American Society of Dentist Anesthesiologists (ASDA) regarding their use of local anesthesia on children undergoing dental rehabilitations under general anesthesia.
METHODS
A survey designed to address this study's purpose was developed on the SurveyMonkey Web site. A pilot of the questionnaire was administered to 5 dentists with extensive experience performing dental rehabilitations for children under general anesthesia and 2 medical anesthesiologists who provide anesthesia for dental rehabilitations on a routine basis. Feedback from the pilot study was used to revise the survey instrument to improve reliability, thereby strengthening the validity of conclusions drawn from survey results. The survey was approved by the Institutional Review Board of Louisiana State University Health Science Center (#7653). E-mail addresses for ASDA members were retrieved from the public Web site http://www.asdahq.org/ on February 8, 2012. The 20-question survey was e-mailed with a letter of introduction stating the survey's purpose and the confidential nature of the survey.
The purpose of the first 2 questions was to establish demographic information. The remaining questions were developed to identify the practitioner's use of local anesthetic during general anesthesia, when they used it, and their rationale. Practitioners were asked if they preferred local anesthesia almost all of the time (>97% of pediatric cases under general anesthesia), some of the time, or almost never (<3% of pediatric cases under general anesthesia). This categorization scheme allowed practitioners to take into account rare exceptions to their preferences. No other questions were asked if the respondent indicated that he or she did not administer anesthesia for dental rehabilitations in patients 12 years of age and younger. Those who did treat patients in this age range were asked about the number of patients they treated in a month, what analgesics were used, and their preferences regarding local anesthesia supplementation. If the respondents reported they preferred local anesthetic at least some of the time, they were asked to report the preferred type of local anesthetic, time of administration, and preferred method of administering it. Respondents reported factors influencing the decision to either administer or not administer local anesthetic in the final 3 questions by reporting if the factor was “very important,” “somewhat important,” “not important,” or “not applicable.”
The responses were exported from SurveyMonkey and analyzed with SAS 9.2 (SAS Institute Inc, Cary, NC) to compute descriptive statistics in addition to using Spearman's correlation, the exact chi-square test, the Wilcoxon rank sums test, and the Kruskal-Wallis tests for hypothesis testing.
A previous study in a different population found that 86% of pediatric dentists used general anesthesia for dental rehabilitation.12 Prior to initiating the current study, a power analysis using 86% as the expected proportion revealed that 70 respondents would allow estimation of the true proportion of dentist anesthesiologists using general anesthesia for dental rehabilitation with a precision of 8%. But the actual sample size obtained in the study (n = 77) and the observed proportion of dentist anesthesiologists using general anesthesia for dental rehabilitation (90.9%) allowed greater precision in the estimation of the true proportion than anticipated (within 6.4%).
RESULTS
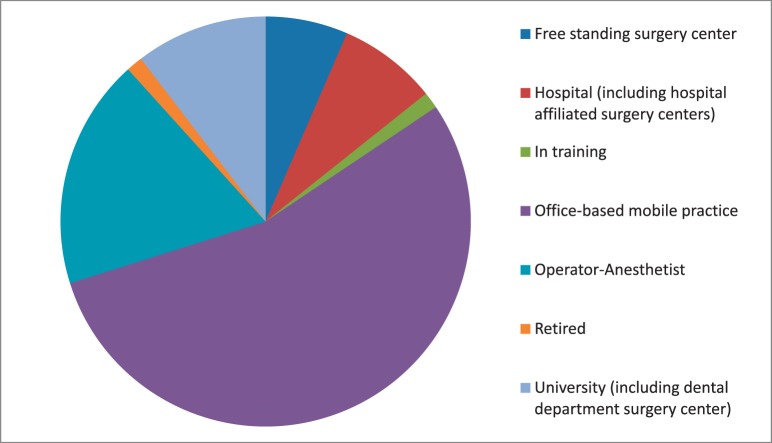
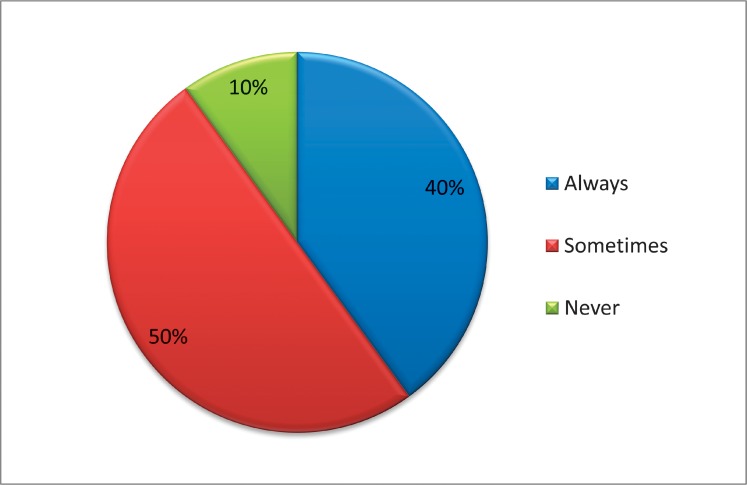
Of the 191 e-mail addresses retrieved from the Web site, 5 had opted out of receiving SurveyMonkey e-mails. Three respondents sent a personal e-mail to the author stating that they did not treat children. Usable responses were received from 77 dentist anesthesiologists, yielding a 42.1% (77/183) response rate. The majority of respondents (54.6%, 42/77) treated children in an office-based mobile practice; the second most common type of practitioner was an operator-anesthetist team concept (18.2%, 14/77). The remaining respondents practiced in a university setting (10.4%, 8/77), hospital setting (7.8%, 6/77), or freestanding surgery center (6.5%, 5/77), as shown in Figure 1. The most common age group represented was practitioners 41–50 years of age (31.2%, 24/77), as shown in Figure 2. Male respondents comprised 79.2% of the sample (61/77). The majority of dentists (90.9%, 70/77) provided general anesthesia for children younger than 12 years of age for dental rehabilitation, with the highest percentage of dentist anesthesiologists (54.3%, 38/77) reporting that they saw less than 30 cases per month.
Figure 1.
Anesthesia practice type of respondents.
Figure 2.
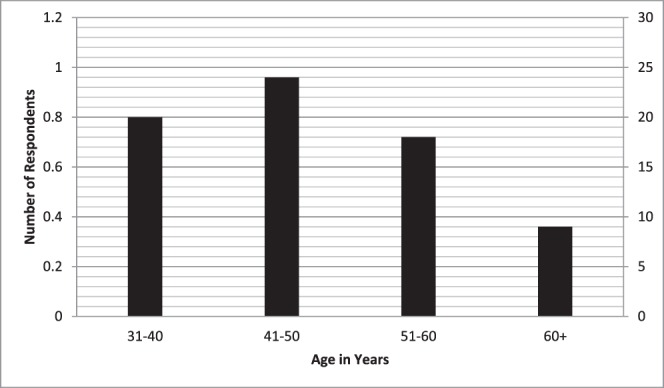
Age distribution of respondents.
Practitioners reported they most commonly used nonsteroidal anti-inflammatory drugs for postoperative pain relief (55.7%, 39/77) for general anesthesia cases, with local anesthesia being the second most commonly used modality (14.3%, 10/77) and opioids the third most commonly used agent (11.4%, 8/77).
The majority of dentist anesthesiologists preferred to supplement their general anesthesia with a local anesthetic for dental rehabilitations almost always or sometimes (90%, 63/70), as shown in Figure 3. The highest proportion of respondents left the decision to the operating dentist (31.4%, 22/70), although 27.1% (19/70) reported administering the local anesthetic themselves. The remaining respondents either informed the dentist to administer/not to administer local anesthetics (18.6%, 13/70) or requested that the dentist administer/not administer local anesthetic (22.86%, 16/70). If the decision was left to the operating dentist, the anesthesiologist informed the dentist of his or her preference 69.6% of the time (16/23).
Figure 3.
Frequency of administration of local anesthetic during dental rehabilitation under general anesthesia (N = 70).
For dentist anesthesiologists who preferred the supplemental use of local anesthetic at least some of the time, the majority preferred to use lidocaine (85.71%, 54/63). Articaine was the second most commonly preferred (5/63, 7.9%), followed by no preference (3/63, 4.8%). The majority of respondents preferred the local anesthetic to be administered prior to treatment (96.8%, 61/63). Infiltration was the preferred route of administration (77.8%, 49/63) followed by no preference (9.5%, 6/63).
Dentist anesthesiologists who preferred the administration of local anesthesia almost always listed the following factors as very important: “stabilization of vital signs/decreased depth of general anesthesia” (92.9%, 26/28), “improved patient recovery” (82.1%, 23/28), “avoid activation of deep pain pathways” (60.7%; 17/28), “shortened recovery time” (57.1%, 16/28), and “hemorrhage control” (46.4%, 13/28). The only factor listed as not important by the majority of respondents was “influence of residency training” (53.6%, 15/28).
For dentist anesthesiologists who preferred supplementation with local anesthesia some of the time, the following 3 factors were listed as very important: “improved patient recovery,” “stabilization of vital signs/decreased depth of general anesthesia,” and “hemorrhage control” (64.7%, 22/34; 48.6%, 17/35; and 45.7%, 16/35 respectively). “Influence of residency training” was again listed as “not important” by the majority of respondents (54.5%, 18/33). When asked what factors affected their choice to administer local anesthesia in a particular case, the following factors were listed as very important by the most respondents: “need for extraction of permanent teeth” (85.7%, 30/35), “need for extraction of primary teeth” (62.9%, 22/35), “extent of treatment” (45.5%, 15/33), and need for hemorrhage control (41.2%, 14/34 ). The following factors were listed as not important by most respondents: “need for stainless steel crowns” (52.9%, 18/34), “older age of patient” (50.0%, 17/34), and “need for pulpotomies” (44.1%, 15/34).
Practitioners who did not prefer the administration of local anesthetics were asked which factors were important in this belief. “Postoperative lip and cheek biting” (85.7%, 6/7) and “unnecessary for pain control if patient receives systemic analgesics” (57.1%, 4/7) were the factors most commonly listed as “very important.” Factors listed as not important by this group were “prolonged recovery” (86.7%, 6/7), “increased risk of toxic reaction” (71.4%, 5/7), and “influence of residency training” (71.4%, 5/7).
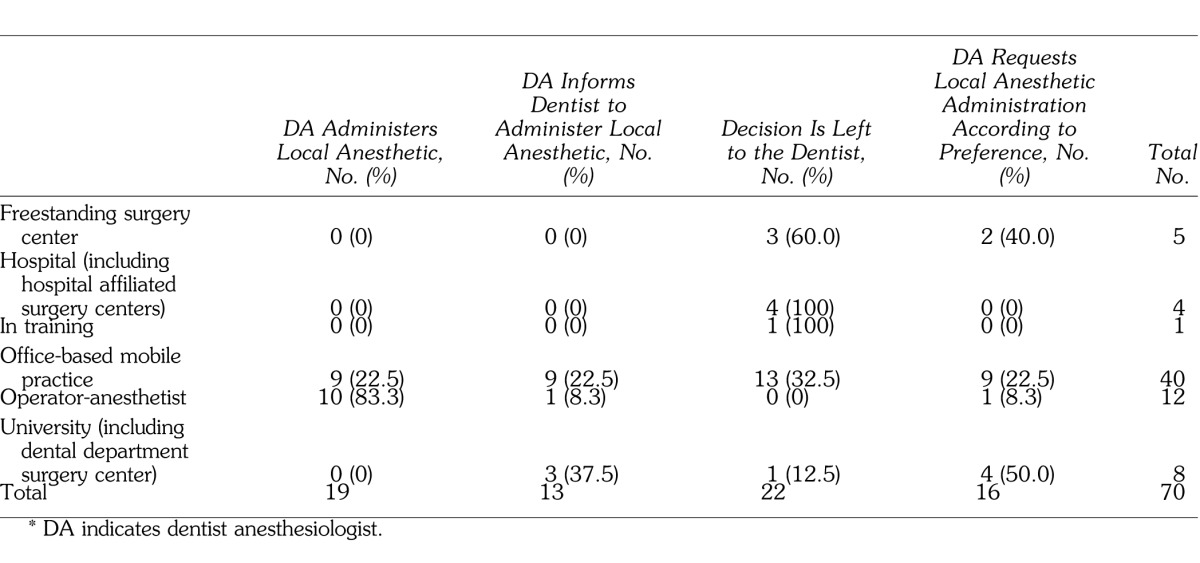
There was a significant association between type of practice and what determined whether or not local anesthesia was administered during cases (χ2 = 42.5, df =15, P < .001) as shown in the Table. Most operator-anesthetists (83%, 10/12) said they administered local anesthetic themselves, whereas the most common choice for respondents from an office-based mobile practice, hospital, or freestanding surgery center and from respondents who were in training was to let the dentist decide whether or not local anesthesia is administered.
Relationship Between Practice Type and Who Determines Administration of Local Anesthetic*
DISCUSSION
The results of the current study indicate that the majority of dentist anesthesiologists (90%) prefer local anesthesia at least some of the time. Although half of them make this decision on a case by case basis, 40% prefer it with very rare exceptions. Improved patient recovery and stabilization of vital signs were the most common reasons for this preference, although other factors were involved such as avoiding deep pain pathways.
Current theories of pain seem to support this practice of preemptive local anesthesia to assist in postoperative pain control and prevent the activation of deep pain pathways. Woolf hypothesized that noxious stimuli that produce tissue injury can generate prolonged poststimulus sensory disturbances that include increased sensitivity to noxious stimuli in the future, or pain following innocuous stimuli.13 This theory of neuroplasticity contributing to postoperative pain has led to studies in the medical field that suggest preemptive regional or local anesthesia can prevent the activation of deep pain pathways.14 The clinical relevance of these findings from basic science and medical research to restorative and surgical dental procedures for children has yet to be demonstrated. There is no clear understanding of how children perceive the sensation of having received local anesthetic, especially in the oral cavity, and if this can cause distress.
Needleman et al reported that children having extractions in dental rehabilitation under general anesthesia were 7 times more likely than other subjects to report pain after returning home.15 However, they also pointed out that there was no significant relationship between extractions and pain postoperatively in the recovery unit, and that increased pain was only evident after local anesthetic would have worn off, at least 2–3 hours later.
Ashkenazi et al found that patients receiving stainless steel crowns with or without pulpotomy had a significantly higher incidence of pain compared to patients having extractions, restorations, and sealants.16 Costa et al found that the number of space maintainers and crowns was associated with increased postoperative pain immediately following the procedure, but there was no relationship between any specific procedure and postoperative pain at any other time.17
In contrast to the findings of the current study, a previous study found that surveyed general dentist and pediatric dentist members of the AAPD were significantly less likely (P < .001) to always administer local anesthesia (8.13%, 66/708, compared to 40.0%, 28/70 in the current study) and significantly less likely (P = .018) to administer local anesthesia at least some of the time compared to dentist anesthesiologists (79.92%, 649/708, vs 90.0%, 63/70 in the current study).12 In the previous study, dentists and dentist anesthesiologists who administered local anesthesia at least part of the time identified the same 3 factors as very important as the current study: “improved patient recovery,” “stabilization of vital signs/decreased depth of general anesthesia,” and “hemorrhage control.”12 Although dentist anesthesiologists did, AAPD members did not identify the following factors as very important: “avoid activation of deep pain pathways” and “shortened recovery time.” AAPD members listed “anesthesiologist request” and “influence of residency trainings” as not important.12 AAPD members may have less involvement with patient recovery, so recovery time may not be a major concern for them.
Both AAPD and ASDA members who preferred local anesthesia some but not all of the time identified “need for extraction of permanent teeth,” “need for extraction of primary teeth,” “need for hemorrhage control,” and “extent of treatment” as very important factors in making that decision.12 Both AAPD and ASDA members who did not give local anesthesia listed “postoperative lip and cheek biting” as very important, although most AAPD members did not list “unnecessary for pain control” as unimportant.12
It was interesting to note that “anesthesiologist request” was the second most commonly listed factor as unimportant by AAPD members (after “influence of residency training”), but 90% (63/70) of dentist anesthesiologists reported that they either gave local anesthesia, informed the dentist to give it, requested the dentist give it, or informed the dentist of their preference.12 One potential explanation is that most AAPD members work with medical anesthesiologists with little input on this issue.
The response rate of 42% in the current study exceeded the 17% response rate for AAPD members.12 Possible reasons for the low response rate in the previous study may have been an inadequate introduction to the survey, unclear survey questions, lack of nonresponder follow-up, and AAPD member frustration with a high number of e-mail surveys. The higher response rate by ASDA may be a reflection of their enthusiasm for this topic. As a side note, the first author received some very pleasant phone calls and e-mails from members wishing to discuss this topic further. Previous research on mail surveys among dentists found that nonresponse bias did not affect the results obtained from dental surveys.18 The study found no differences in views or demographic characteristics between responders to first mailed questionnaires and those who did not respond, and conclusions drawn from initial responders would have been the same as those based on the complete sample.18 But this finding has not been reproduced in Web-assisted surveys.
Analgesia and postoperative pain control is an important part of the treatment plan, especially during dental rehabilitations under general anesthesia. The dentist and anesthesia provider should collaborate to anticipate and reduce patients' postoperative pain. To date, no prospective double-blind studies have been published to definitively show the necessity, or lack thereof, of using local anesthesia for all or some clinical dental procedures performed on a child who is under general anesthesia.
Possible areas for future research include:
-
1.
Double-blind clinical trials evaluating the supplemental use of local anesthesia during dental rehabilitations under general anesthesia with adequate sample size, monitoring postoperative pain both in the hospital recovery room and at home after discharge.
-
2.
Patterns of education on the use of analgesia and local anesthesia in children.
-
3.
Deep pain pathway activation in children due to dental procedures.
-
4.
Clinical studies on postoperative pain and administration of general anesthesia due to dental treatment.
-
5.
Pain assessment specific to dentistry in children under general anesthesia.
-
6.
Strategies for assessing dental pain in young/nonverbal children.
CONCLUSION
-
1.
Ninety-one percent of responding dentist anesthesiologists use local anesthesia at least part of the time during dental rehabilitations under general anesthesia, and 40% use it with rare exceptions.
-
2.
“Stabilization of vital signs/decreased depth of general anesthesia,” “improved patient recovery,” and “avoid activation of deep pain pathways” were the most commonly cited reasons for administering local anesthetic.
-
3.
The most common dental procedures for which local anesthetic was used were reported to be “need for extraction of permanent teeth” and “need for extraction of primary teeth.”
REFERENCES
- 1.American Academy of Pediatric Dentistry Guideline on behavior guidance for the pediatric dental patient. Pediatr Dent. 2012;34:170–182. [Google Scholar]
- 2.Noble DW, Raab GM, MacLean D, Maclachlan D. Prilocaine infiltration as postoperative analgesia for children having dental extractions under general anesthesia. Reg Anesth. 1994;19:126–131. [Google Scholar]
- 3.Atan S, Ashley P, Gilthrope MS, Scheer B, Mason C, Roberts G. Morbidity following dental treatment of children under intubation general anaesthesia in a day-stay unit. Int J Paediatr Dent. 2004;14:9–16. doi: 10.1111/j.1365-263x.2004.00520.x. [DOI] [PubMed] [Google Scholar]
- 4.Sammons HM, Unsworth V, Ray C, Choonara I, Cherrill J, Quirke W. Randomized controlled trial of the intraligamental use of a local anaesthetic (lignocaine 2%) versus controls in paediatric tooth extraction. Int J Paediatr Dent. 2007;17:297–303. doi: 10.1111/j.1365-263X.2007.00832.x. [DOI] [PubMed] [Google Scholar]
- 5.Watts AK, Thikkurissy S, Smiley M, McTigue DJ, Smith T. Local anesthesia affects physiologic parameters and reduces anesthesiologist intervention in children undergoing general anesthesia for dental rehabilitation. Pediatr Dent. 2009;31:414–419. [PubMed] [Google Scholar]
- 6.Needleman HL. Local anesthesia during dental rehabs, “To use, or not to use: that (still) is the question.”. Pediatr Dent. 2010;32:7. [PubMed] [Google Scholar]
- 7.Townsend JA, Ganzberg S, Thikkurissy S. The effect of local anesthetic on quality of recovery characteristics following dental rehabilitation under general anesthesia in children. Anesth Prog. 2009;56:115–122. doi: 10.2344/0003-3006-56.4.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leong KJ, Roberts GJ, Ashley PF. Perioperative local anaesthetic in young paediatric patients undergoing extractions under outpatient “short-case” general anaesthesia. A double-blind randomized controlled trial. Br Dent J. 2007;203:334–339. doi: 10.1038/bdj.2007.724. [DOI] [PubMed] [Google Scholar]
- 9.Coulthard P, Rolfe S, Mackie IC, Gazal G, Morton M, Jacson-Leech J. Intraoperative local anaesthesia for paediatric postoperative oral surgery pain–a randomized controlled trial. Int J Oral Maxillofac Surg. 2006;35:1114–1119. doi: 10.1016/j.ijom.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 10.Al-Bahlani S, Sherriff A, Crawford PJM. Tooth extraction, bleeding and pain control. J R Coll Surg Edinb. 2001;46:261–264. [PubMed] [Google Scholar]
- 11.Gazal G, Bowman R, Worthington HV, Mackie IC. A double-blind randomized controlled trial investigating the effectiveness of topical bupivacaine in reducing distress in children following extractions under general anesthesia. Int J Paediatr Dent. 2004;14:425–431. doi: 10.1111/j.1365-263X.2004.00587.x. [DOI] [PubMed] [Google Scholar]
- 12.Townsend JA, Martin A, Hagan JL, Needleman H. The user of local anesthesia during dental rehabilitations: a survey of AAPD members. Pediatr Dent. 2013;35:422–425. [PubMed] [Google Scholar]
- 13.Woolf CJ. Evidence for a central component of post-injury pain hypersensitivity. Nature. 1983;306:686–688. doi: 10.1038/306686a0. [DOI] [PubMed] [Google Scholar]
- 14.Katz J, Kavanagh BP, Sandler AN, et al. Preemptive analgesia: Clinical evidence of neuroplasticity contributing to postoperative pain. Anesthesiology. 1992;77:439–446. doi: 10.1097/00000542-199209000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Needleman HL, Harpavat S, Wu S, Allred EN, Berde C. Postoperative pain and other sequelae of dental rehabilitations performed on children under general anesthesia. Pediatr Dent. 2008;30:111–121. [PubMed] [Google Scholar]
- 16.Ashkenazi M, Blumer S, Eli I. Post-operative pain and use of analgesic agents in children following intrasulcular anaesthesia and various operative procedures. Br Dent J. 2007;202:E13. doi: 10.1038/bdj.2007.81. [DOI] [PubMed] [Google Scholar]
- 17.Costa LR, Harrison R, Aleksejuniene J, Nouri M, Gartner A. Factors related to postoperative discomfort in young children following dental rehabilitation under general anesthesia. Pediatr Dent. 2011;33:321–326. [PubMed] [Google Scholar]
- 18.Hovland EJ, Romberg E, Moreland EF. Nonresponse bias to mail survey questionnaires within a professional population. J Dent Educ. 1980;44:270–274. [PubMed] [Google Scholar]