Abstract
The effects of human immunodeficiency virus (HIV) on the immune response in patients with cutaneous leishmaniasis have not yet been fully delineated. This study quantified and evaluated the function of memory T-cell subsets in response to soluble Leishmania antigens (SLA) from patients coinfected with HIV and Leishmania with tegumentary leishmaniasis (TL). Eight TL/HIV coinfected subjects and 10 HIV seronegative subjects with TL were evaluated. The proliferative response of CD4+and CD8+T-cells and naïve, central memory (CM) and effector memory (EM) CD4+T-cells in response to SLA were quantified using flow cytometry. The median cell division indices for CD4+and CD8+T-cells of coinfected patients in response to SLA were significantly lower than those in patients with Leishmania monoinfection (p < 0.05). The proportions of CM and EM CD4+T-cells in response to SLA were similar between the coinfected patients and patients with Leishmania monoinfection. However, the median CM and EM CD4+T-cell counts from coinfected patients were significantly lower (p < 0.05). The reduction in the lymphoproliferative response to Leishmania antigens coincides with the decrease in the absolute numbers of both EM and CM CD4+T-cells in response to Leishmania antigens in patients coinfected with HIV/Leishmania.
Keywords: Leishmania, HIV, coinfection, memory CD4+ T-cells
Human immunodeficiency virus (HIV) type 1 is a human retrovirus that infects roughly 34 million people worldwide and is responsible for the majority of the acquired immune deficiency syndrome (AIDS) epidemic. The most severely affected areas are in Sub-Saharan Africa, the Caribbean, Eastern Europe and Central Asia (UNAIDS 2012). Leishmania have been recognised as opportunistic pathogens in immunocompromised individuals, including those infected with HIV (Badaro 1997, Cruz et al. 2006). Over the past decades, the HIV epidemic has spread from urban areas to suburban and rural areas, where leishmaniasis is found. In particular, Leishmania and HIV infection overlap in several sub-tropical and tropical regions around the world (Karp & Auwaerter 2007). In northern India, Sudan and Ethiopia, visceral leishmaniasis has been a major scourge in patients infected with HIV (Wolday et al. 2001, Mathur et al. 2006, ter Horst et al. 2008). In Brazil, cutaneous disease is also a common presentation of leishmaniasis in HIV-coinfected patients (Rabello et al. 2003, Carranza-Tamayo et al. 2009, Lindoso et al. 2009). These patients often present with multiple skin ulcers, disseminated lesions and nasopharyngeal and/or genital mucosal damage (Coura et al. 1987, Machado et al. 1992, Da-Cruz et al. 1999, Lindoso et al. 2009). The clinical outcome of Leishmania infection is dependent upon the balance of T-helper (Th)1 and Th2 cytokine production during the immune response (Bacellar et al. 2000, Bourreau et al. 2003). In HIV/Leishmania coinfected patients with visceral disease, HIV infection alters the Th1/Th2 balance, resulting in an increased Th2 cytokine response while levels of the Th1 cytokines interleukin (IL)-12 and IL-18 are decreased (Nigro et al. 1999, Wolday et al. 2000). This results in more aggressive and relapsing visceral leishmaniasis. The effects of HIV on the immune response in cutaneous leishmaniasis have not yet been fully delineated. Reduced interferon (IFN)-γ production, decreased IFN-γ/IL-10 ratios (Rodrigues et al. 2011) and diminished lymphoproliferative responses to Leishmania antigens have been described in HIV-infected patients with the cutaneous form of leishmaniasis (Da-Cruz et al. 1992, 1999). These findings suggest that coinfected HIV/Leishmania patients may have a memory T-cell defect. Here, we have quantified and assessed the function of memory T-cell subsets in response to soluble Leishmania antigens (SLA) from patients coinfected with HIV and Leishmania with tegumentary leishmaniasis (TL).
SUBJECTS, MATERIALS AND METHODS
Eight patients with TL and HIV infection and 10 HIV seronegative subjects with TL were included in the study. The subjects were enrolled from the AIDS clinical centre of the University Hospital Professor Edgard Santos, located in Salvador, Brazil, after informed consent. Clinical and demographic characteristics of the HIV/Leishmania coinfected subjects are presented in Table I. All Leishmania monoinfected patients had active cutaneous leishmaniasis at the time of inclusion in the study. Six of these patients had cutaneous leishmaniasis, one had disseminated cutaneous leishmaniasis and three had mucosal leishmaniasis.
TABLE 1. Clinical and epidemiological characteristics of human immunodeficiency virus (HIV)/Leishmania coinfected patients.
| Coinfected group | Gender | Age (year) | CD4+ T-cell count (cell/mm3) | Viral load (log copies/mL) | ART use | Leishmaniasis form |
| TL/HIV 03 | F | 42 | 93 | 5.4 | Unknown | Mucocutaneous active |
| TL/HIV 05 | F | 22 | 291 | 1.9 | Unknown | Cutaneous active |
| TL/HIV 06 | M | 36 | 165 | 5.3 | Unknown | Cutaneous treated |
| TL/HIV 08 | F | 62 | 415 | 2.7 | Yes | Disseminated cutaneous treated |
| TL/HIV 09 | M | 59 | 78 | 5.0 | Yes | Cutaneous active |
| TL/HIV 12 | M | 36 | 615 | 1.9 | Yes | Cutaneous active |
| TL/HIV 13 | M | 36 | 104 | 5.0 | No | Cutaneous active treated |
| TL/HIV 14 | M | 25 | 241 | 4.6 | Yes | Mucocutaneous active |
ART: antiretroviral treatment; F: female; M: male; TL: tegumentary leishmaniasis.
Peripheral blood mononuclear cells (PBMCs) were isolated by passage over a Ficoll-Hypaque gradient (Amersham Biosciences, Piscataway, NJ, USA). PBMCs (3 x 106 cells) were resuspended in RPMI-1640 medium (Sigma-Aldrich, St. Louis, MO, USA) supplemented with 2 mM L-glutamine, penicillin (100 U/mL), streptomycin (100 mg/mL) (GIBCO) and 5% heat-inactivated human AB serum. The cells were stimulated with SLA obtained from the Leishmania chagasi (MHOM/BR2000/Merivaldo2) strain [isolated from a patient with visceral leishmaniasis (Baleeiro et al. 2006)] or phytohemagglutinin (PHA) (Sigma-Aldrich). Control cultures were also established with medium alone.
To evaluate the proliferative response of T-cell subsets to SLA, 1.5 x 106 PBMC/mL were labelled with carboxyfluorescein succinimidyl ester (Invitrogen, Eugene, OR, USA) as described by the manufacturer. PBMCs were cultured in 12 × 75-mm tissue culture tubes for five days at 37ºC in a humidified 5% CO2 atmosphere. Then, the cells were washed with phosphate-buffered saline (PBS)/bovine serum albumin and surface stained with anti-CD4-phycoerythrin (PE) (Becton Dickinson, CA, USA) and anti-CD8-PE-Cy5 (eBioscience, CA, USA) for 30 min at 4ºC. After fixation in 1% formaldehyde, the cells were acquired by FACSAria (Becton Dickinson) and analysis was performed using FlowJo software version 7.6 (Tree Star Inc, Ashland, OR, USA). At least 30,000 events were analysed per sample. The proliferation intensity was determined through the percentage of the cell division index. The threshold to define positive proliferative response was a cell division index above 0.06 for CD4+ T-cells and above 0.09 for the CD8+ T-cell subset as described previously (Pinto et al. 2011).
Alternatively, to determine the frequency of memory CD4+ T-cells, 1.5 x 106 PBMCs were cultured with SLA, PHA or PBS for 18 h in supplemented RPMI-1640 medium in the presence of 0.5 µg of purified anti-CD28 antibody at 37ºC in a humidified 5% CO2 atmosphere. Then, the cells were stained with anti-CD4-(fluorescein isothiocyanate), anti-CD45RA-PE, anti-CD62L-PE-Cy5 and anti-CCR7-PE-Cy7 antibodies (Becton Dickinson). Cells were acquired by FACSAria and analysed using the Flowjo software. Naïve cells were defined as CD4+CD45RA+CD62L+CCR7+, central memory (CM) cells were defined as CD4+CD45RA-CD62L+CCR7+ and effector memory (EM) cells were defined as CD4+CD45RA-CD62L-CCR7-. Absolute naïve, CM and EM lymphocyte subpopulation counts were obtained by multiplying the subpopulation percentage by the absolute lymphocyte count.
The data are expressed as median and interquartile range (IQR). Statistical analysis was performed using GraphPad Prism 5.02 (La Jolla, CA, USA). The Mann-Whitney U test was used for group comparisons and the Wilcoxon test was used for the analyses of cell count and cell proportion in the presence and absence of antigen.
Institutional review board approvals were obtained from Brazilian National Ethical Commission, Oswaldo Cruz Foundation and the University of California San Diego Human Research Protection Program.
RESULTS
The median CD4+ T-cell count from HIV/Leishmania coinfected patients (241 cells/mm3, IQR 85-453) was significantly lower compared with that of Leishmania monoinfected patients (784 cells/mm3, IQR 599-1477) (p = 0.004). The median HIV viral load of HIV/Leishmania coinfected patients was 4.6 log copies/mL (IQR 1.9-5.2). The sex ratio and median age were similar in both groups.
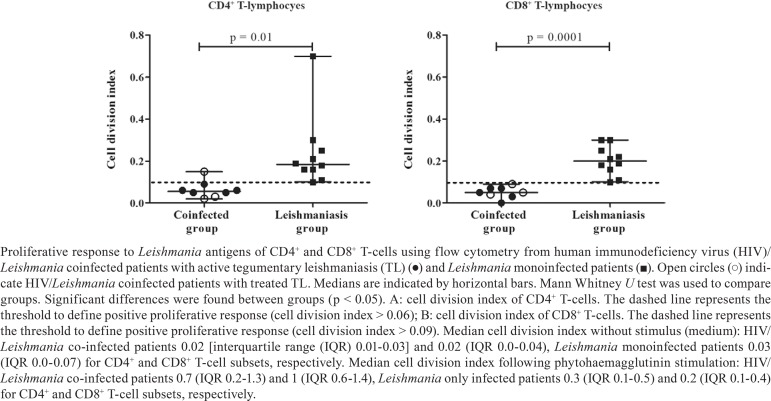
The median cell division indices in response to SLA for CD4+ (0.06, IQR 0.05-0.1) and CD8+ T-cells (0.05, IQR 0.01-0.08) from HIV/Leishmania coinfected patients were significantly lower than those from Leishmania monoinfected patients (CD4+ T-cell: 0.18, IQR 0.15-0.26; CD8+ T-cell: 0.2, IQR 0.15-0.26) (p < 0.05) (Figure). A lymphoproliferative response to SLA was detected in only one coinfected patient (TL/HIV 06) (12%) who had a previously treated cutaneous leishmaniasis infection. In contrast, CD4+ and CD8+ T-cell subsets from all Leishmania monoinfected patients proliferated in response to SLA. The CD4+ and CD8+ T-cell subsets from both HIV/Leishmania coinfected and Leishmania monoinfected patients all proliferated in response to PHA.
Fig. 1. Proliferative response to Leishmania antigens of CD4+ and CD8+ T-cells using flow cytometry from human immunodeficiency virus (HIV)/Leishmania coinfected patients with active tegumentary leishmaniasis (TL) (●) and Leishmania monoinfected patients (■). Open circles (○) indicate HIV/Leishmania coinfected patients with treated TL. Medians are indicated by horizontal bars. Mann Whitney U test was used to compare groups. Significant differences were found between groups (p < 0.05). A: cell division index of CD4+ T-cells. The dashed line represents the threshold to define positive proliferative response (cell division index > 0.06); B: cell division index of CD8+ T-cells. The dashed line represents the threshold to define positive proliferative response (cell division index > 0.09). Median cell division index without stimulus (medium): HIV/Leishmania co-infected patients 0.02 [interquartile range (IQR) 0.01-0.03] and 0.02 (IQR 0.0-0.04), Leishmania monoinfected patients 0.03 (IQR 0.0-0.07) for CD4+ and CD8+ T-cell subsets, respectively. Median cell division index following phytohaemagglutinin stimulation: HIV/Leishmania co-infected patients 0.7 (IQR 0.2-1.3) and 1 (IQR 0.6-1.4), Leishmania only infected patients 0.3 (IQR 0.1-0.5) and 0.2 (IQR 0.1-0.4) for CD4+ and CD8+ T-cell subsets, respectively.
The proportions of naïve, CM and EM CD4+ T-cells obtained after stimulation with SLA were similar between the HIV/Leishmania coinfected and Leishmania monoinfected groups (Table II). However, the median absolute counts of naïve, CM and EM CD4+ T-cells from HIV/Leishmania coinfected patients were significantly lower compared with those of Leishmania monoinfected patients (p < 0.05). Following SLA stimulation, a statistically significant increase in the median absolute counts of EM CD4+ T-cells was observed in the cultures from Leishmania monoinfected patients (p = 0.005). In contrast, there was no change in the median absolute counts of EM CD4+ T-cells of HIV/Leishmania coinfected patients in the presence of SLA and a statistically significant decrease in the CM CD4+ T-cell count was observed after culture with SLA (p = 0.02). However, there was a statistically significant increase in the absolute number of EM CD4+ T-cells from both HIV/Leishmania coinfected and Leishmania monoinfected groups following PHA stimulation.
TABLE II. Quantification of naïve, central (CM) and effector (EM) memory CD4+ T-cell subsets in response to soluble Leishmania antigens (SLA) and to phytohaemagglutinin (PHA) from of human immunodeficiency virus (HIV)/Leishmania coinfected and Leishmania monoinfected groups .
| CD4+ T-cell subset | Medium | SLA | PHA | ||||||
| Coinfected | Monoinfected | p | Coinfected | Monoinfected | p | Coinfected | Monoinfected | p | |
| Naïve | |||||||||
| n (%) | 30 (17-37) | 43 (18-80) | 0.8 | 39 (17-64) | 34 (15-57) | 0.7 | 2 (1-4)b | 4 (2-9)b | 0.5 |
| n (cell/mm3) | 9 (3-14) | 17 (5-65) | 0.02 | 3 (2-11) | 42 (25-106) | 0.03 | 2 (0-6)b | 13 (4-28) | 0.02 |
| CM | |||||||||
| n (%) | 23 (8-31) | 24 (6-32) | 0.6 | 11 (4-25) | 8 (2-23)a | 0.9 | 1 (0-4)b | 2 (1-3) | 0.3 |
| n (cell/mm3) | 55 (31-105) | 49 (19-103) | 0.001 | 3 (1-5) a | 46 (25-119) | 0.8 | 1 (0-3)b | 8 (2-16)b | 0.02 |
| EM | |||||||||
| n (%) | 12 (11-29) | 9 (6-15) | 0.2 | 21 (11-43) | 17 (14-23)a | 0.07 | 35 (20-40)b | 30 (25-38)b | 0.8 |
| n (cell/mm3) | 8 (5-11) | 36 (12-63) | 0.0009 | 6 (2-9) | 122 (69-143)a | 0.0001 | 27 (11-58)b | 175 (105-236)b | 0.0005 |
Wilcoxon test was used to compare cells cultured with medium and SLA (a) and cells cultured with medium and PHA (b) for each group. Data are presented as median (interquartile range). p: Mann-Whitney U test was used to compare HIV/Leishmania coinfected and Leishmaniasis monoinfected groups.
DISCUSSION
This study demonstrates that a reduction in the lymphoproliferative response to Leishmania antigens coincides with a decrease in the absolute numbers of both EM and CM CD4+ T-cells in response to Leishmania antigens in patients coinfected with HIV/Leishmania. Although the proportion of memory CD4+ T-cells subsets was similar between monoinfected Leishmania and coinfected HIV/Leishmania patients, the median absolute count of EM lymphocytes in coinfected patients was four-fold lower compared with that of Leishmania monoinfected patients. Moreover, following Leishmania antigen stimulus, the EM CD4+ T-cell count of HIV/Leishmania coinfected patients remained below 10 cells/mm3, whereas we observed a three-fold increase in the EM CD4+ T-cell count in the Leishmania monoinfected patients. The low number of EM CD4+ T-cells in HIV/Leishmania coinfected patients might explain the reduced IFN-γ production in response to Leishmania antigens observed in coinfected subjects as well as the atypical parasitic spread, frequent relapse and treatment failure observed in these patients (Da-Cruz et al. 1992, Cruz et al. 2006, Lindoso et al. 2009). Although memory and effector CD8+ T-cell profiles were not evaluated in our study, CD8+ T-cells from all HIV/Leishmania coinfected patients were unable to proliferate in response to SLA. Previous work has demonstrated the protective role of CD8+ T-cells in Leishmania infection, with healing of lesions associated with high IFN-γ production and an increase in the number of CD8+ T-cells (Da-Cruz et al. 1994, Muller et al. 1994).
The absence of a lymphoproliferative response to Leishmania antigens in both the CD4+ and CD8+ T-cell subsets examined in our study suggests impairment of the cellular immune response directed at the parasitic infection. Although the HIV/Leishmania coinfected group was heterogeneous with respect to clinical presentation of leishmaniasis (cutaneous vs. mucosal) and stage of treatment (active vs. treated), a significant lack of immune response to Leishmania antigens was observed across this group of subjects. Only one HIV/Leishmania coinfected patient exhibited a proliferative response to Leishmania antigens. This patient was successfully treated for TL before his inclusion in the study and his lesions were in remission. However, the two other coinfected individuals with treated TL did not develop a proliferative response. Additionally, we found that a decrease in the number of CM CD4+ T-cells occurred following SLA stimulation in all cultures of coinfected patients and EM CD4+ T-cell counts of these patients did not change regardless of presentation of leishmaniasis or stage of treatment. Previous work has shown that the restoration of CD4+ T-cell-specific responses to antigens in HIV-infected patients undergoing antiretroviral treatment (ART) requires a sustained increase of at least 60 CD4+ T-cells/µL compared with baseline levels and a reduced viral load (Li et al. 1998). In addition to the quantitative immune defect observed in HIV infection, the quality of the immune response (i.e., degree of immune memory impairment) may also be important in the host response to other pathogens such as Leishmania.
Studies in both mice and humans have demonstrated multiple CD4+ T-cell phenotypes and a broad spectrum of functions have been attributed to these cells in different viral infections (Chen et al. 2001, de Rosa et al. 2001, Roman et al. 2002). Memory T-cells are divided into subpopulations based on the expression of CCR7, a chemokine receptor involved in homing to secondary lymphoid organs and CD45RA, a cell surface molecule involved in T-cell activation. T-cells expressing CD45RA and CCR7 are termed naïve, whereas those with downregulated CD45RA are termed CM cells and produce IL-2. Memory T-cells lacking expression of CCR7 and CD45RA are termed EM T-cells and produce IFN-γ (Sallusto et al. 1999). The functional and phenotypic heterogeneity of memory T-cells are influenced by variations in antigen exposure and persistence. A dominant single IL-2 and/or IL-2/IFN-γ CD4 T-cell response is normally associated with clearance of antigen, whereas a dominant single IFN-γ CD4 T-cell response is associated with antigen persistence and high antigen levels (Harari et al. 2005). Effector CD4+ T-cells are lost in the absence of parasites, whereas CM CD4+ T-cells are maintained. Upon secondary infection, these CM T-cells become effector T-cells and mediate protection (Zaph et al. 2004). In our study, a decrease in the number of CM CD4+ T-cells was observed in the coinfected group following stimulation with SLA. It is possible that during coinfection with HIV and Leishmania, the immune activation caused by both HIV and Leishmania infection induces increased apoptosis of parasite-specific memory CD4+ T-lymphocytes (Wolday et al. 1999a, b). The decreased numbers of CM cells and EM cells would reduce the ability of the immune system to develop an adequate systemic response to control the Leishmania infection. However, the overall hyporesponsiveness of the cells to Leishmania antigen stimulation could also suggest that a qualitative defect may be contributing to this phenomenon. Thus, although an impaired memory response is known to be related to the depletion of CD4+ T-cells via mechanisms related directly or indirectly to HIV (systemic activation and replicative senescence), a defective functional memory response may also be playing a role (Moro-Garcia et al. 2012). Interestingly however, we found that our coinfected cells responded well to PHA, suggesting that the immunodeficiency was parasite-specific.
Viral suppression by ART may be a contributing factor and in this study, several of our subjects were not receiving ART. In the future, we will examine how the immune response to Leishmania is reconstituted under ART. Although the impact of HIV-1 on host cellular immune function clearly plays an important role in facilitating Leishmania infection in dually infected individuals, there is increasing evidence that other mechanisms for the interaction of these two pathogens might also be involved. Particularly, the immunological mechanisms involved in the pathogenesis of mucocutaneous lesions in HIV-infected individuals remain unclear. We hypothesise that innate immunity to Leishmania is also compromised in coinfected patients, resulting in the more severe pathogenesis of mucocutaneous lesions observed in coinfected patients. Future work will be required to evaluate the effect of coinfection on innate immunity.
Acknowledgments
To Geraldo Gileno, LPBI, Fiocruz-BA, for providing SLA.
REFERENCES
- Bacellar O, D'Oliveira A, Jr, Jeronimo S, Carvalho EM. IL-10 and IL-12 are the main regulatory cytokines in visceral leishmaniasis. Cytokine. 2000;12:1228–1231. doi: 10.1006/cyto.2000.0694. [DOI] [PubMed] [Google Scholar]
- Badaro R. When Leishmania and HIV interact, a new broad spectrum of leishmaniasis occurs. Braz J Infect Dis. 1997;1:145–148. [PubMed] [Google Scholar]
- Baleeiro CO, Paranhos-Silva M, Santos JC dos, Oliveira GG, Nascimento EG, Carvalho LP de, Santos WL dos. Montenegro's skin reactions and antibodies against different Leishmania species in dogs from a visceral leishmaniosis endemic area. Vet Parasitol. 2006;139:21–28. doi: 10.1016/j.vetpar.2006.02.033. [DOI] [PubMed] [Google Scholar]
- Bourreau E, Gardon J, Pradinaud R, Pascalis H, Prevot-Linguet G, Kariminia A, Pascal L. Th2 responses predominate during the early phases of infection in patients with localized cutaneous leishmaniasis and precede the development of Th1 responses. Infect Immun. 2003;71:2244–2246. doi: 10.1128/IAI.71.4.2244-2246.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carranza-Tamayo CO, Assis TS de, Neri AT, Cupolillo E, Rabello A, Romero GA. Prevalence of Leishmania infection in adult HIV/AIDS patients treated in a tertiary-level care center in Brasilia, Federal District, Brazil. Trans R Soc Trop Med Hyg. 2009;103:743–748. doi: 10.1016/j.trstmh.2009.01.014. [DOI] [PubMed] [Google Scholar]
- Chen G, Shankar P, Lange C, Valdez H, Skolnik PR, Wu L, Manjunath N, Lieberman J. CD8 T cells specific for human immunodeficiency virus, Epstein-Barr virus and cytomegalovirus lack molecules for homing to lymphoid sites of infection. Blood. 2001;98:156–164. doi: 10.1182/blood.v98.1.156. [DOI] [PubMed] [Google Scholar]
- Coura JR, Galvão-Castro B, Grimaldi G., Jr Disseminated American cutaneous leishmaniasis in a patient with AIDS. Mem Inst Oswaldo Cruz. 1987;82:581–582. doi: 10.1590/s0074-02761987000400019. [DOI] [PubMed] [Google Scholar]
- Cruz I, Nieto J, Moreno J, Canavate C, Desjeux P, Alvar J. Leishmania/HIV co-infections in the second decade. Indian J Med Res. 2006;123:357–388. [PubMed] [Google Scholar]
- Da-Cruz AM, Conceicao-Silva F, Bertho AL, Coutinho SG. Leishmania-reactive CD4+ and CD8+ T cells associated with cure of human cutaneous leishmaniasis. Infect Immun. 1994;62:2614–2618. doi: 10.1128/iai.62.6.2614-2618.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da-Cruz AM, Filgueiras DV, Coutinho Z, Mayrink W, Grimaldi G, Jr, De Luca PM, Mendonça SCF, Coutinho SG. Atypical mucocutaneous leishmaniasis caused by Leishmania braziliensis in an acquired immunodeficiency syndrome patient: T-cell responses and remission of lesions associated with antigen immunotherapy. Mem Inst Oswaldo Cruz. 1999;94:537–542. doi: 10.1590/S0074-02761999000400020. [DOI] [PubMed] [Google Scholar]
- Da-Cruz AM, Machado ES, Menezes JA, Rutowitsch MS, Coutinho SG. Cellular and humoral immune responses of a patient with American cutaneous leishmaniasis and AIDS. Trans R Soc Trop Med Hyg. 1992;86:511–512. doi: 10.1016/0035-9203(92)90089-u. [DOI] [PubMed] [Google Scholar]
- Rosa SC de, Herzenberg LA, Roederer M. 11-color, 13-parameter flow cytometry: identification of human naïve T cells by phenotype, function and T-cell receptor diversity. Nat Med. 2001;7:245–248. doi: 10.1038/84701. [DOI] [PubMed] [Google Scholar]
- UNAIDS . Joint United Nations Program on HIV/AIDS 2012. Global Report 2012. WHO; Geneva: 2012. 107 [Google Scholar]
- Harari A, Vallelian F, Meylan PR, Pantaleo G. Functional heterogeneity of memory CD4 T cell responses in different conditions of antigen exposure and persistence. J Immunol. 2005;174:1037–1045. doi: 10.4049/jimmunol.174.2.1037. [DOI] [PubMed] [Google Scholar]
- Karp CL, Auwaerter PG. Coinfection with HIV and tropical infectious diseases. I. Protozoal pathogens. Clin Infect Dis. 2007;45:1208–1213. doi: 10.1086/522181. [DOI] [PubMed] [Google Scholar]
- Li TS, Tubiana R, Katlama C, Calvez V, Mohand HA, Autran B. Long-lasting recovery in CD4 T-cell function and viral-load reduction after highly active antiretroviral therapy in advanced HIV-1 disease. Lancet. 1998;351:1682–1686. doi: 10.1016/s0140-6736(97)10291-4. [DOI] [PubMed] [Google Scholar]
- Lindoso JA, Barbosa RN, Posada-Vergara MP, Duarte MI, Oyafuso LK, Amato VS, Goto H. Unusual manifestations of tegumentary leishmaniasis in AIDS patients from the New World. Br J Dermatol. 2009;160:311–318. doi: 10.1111/j.1365-2133.2008.08908.x. [DOI] [PubMed] [Google Scholar]
- Machado ES, Braga MP, Da-Cruz AM, Coutinho SG, Vieira ARM, Rutowitsch MS, Cuzzi-Maya T, Grimaldi G, Jr, Menezes JA. Disseminated American muco-cutaneous leishmaniasis caused by Leishmania braziliensis braziliensis in a patient with AIDS: a case report. Mem Inst Oswaldo Cruz. 1992;87:487–492. doi: 10.1590/s0074-02761992000400005. [DOI] [PubMed] [Google Scholar]
- Mathur P, Samantaray JC, Vajpayee M, Samanta P. Visceral leishmaniasis/human immunodeficiency virus co-infection in India: the focus of two epidemics. J Med Microbiol. 2006;55:919–922. doi: 10.1099/jmm.0.46574-0. [DOI] [PubMed] [Google Scholar]
- Moro-Garcia MA, Alonso-Arias R, Lopez-Larrea C. Molecular mechanisms involved in the aging of the T-cell immune response. Curr Genomics. 2012;13:589–602. doi: 10.2174/138920212803759749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller I, Kropf P, Louis JA, Milon G. Expansion of gamma interferon-producing CD8+ T cells following secondary infection of mice immune to Leishmania major . Infect Immun. 1994;62:2575–2581. doi: 10.1128/iai.62.6.2575-2581.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigro L, Cacopardo B, Preiser W, Braner J, Cinatl J, Palermo F, Russo R, Doerr HW, Nunnari A. In vitro production of type 1 and type 2 cytokines by peripheral blood mononuclear cells from subjects coinfected with human immunodeficiency virus and Leishmania infantum . Am J Trop Med Hyg. 1999;60:142–145. doi: 10.4269/ajtmh.1999.60.142. [DOI] [PubMed] [Google Scholar]
- Pinto LA, Castro BG, Soares MBP, Grassi MFR. An evaluation of the spontaneous proliferation of peripheral blood mononuclear cells in HTLV-1-infected individuals using flow cytometry. ISRN Oncol. 20112011:326719–326719. doi: 10.5402/2011/326719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabello A, Orsini M, Disch J. Leishmania/HIV co-infection in Brazil: an appraisal. Ann Trop Med Parasitol. 2003;97(Suppl. 1):17–28. doi: 10.1179/000349803225002507. [DOI] [PubMed] [Google Scholar]
- Rodrigues MZ, Grassi MF, Mehta S, Zhang XQ, Gois LL, Schooley RT, Badaro R. Th1/Th2 cytokine profile in patients coinfected with HIV and Leishmania in Brazil. Clin Vaccine Immunol. 2011;18:1765–1769. doi: 10.1128/CVI.00076-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roman E, Miller E, Harmsen A, Wiley J, von Andrian UH, Huston G, Swain SL. CD4 effector T cell subsets in the response to influenza: heterogeneity, migration and function. J Exp Med. 2002;196:957–968. doi: 10.1084/jem.20021052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallusto F, Lenig D, Forster R, Lipp M, Lanzavecchia A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature. 1999;401:708–712. doi: 10.1038/44385. [DOI] [PubMed] [Google Scholar]
- ter Horst R, Collin SM, Ritmeijer K, Bogale A, Davidson RN. Concordant HIV infection and visceral leishmaniasis in Ethiopia: the influence of antiretroviral treatment and other factors on outcome. Clin Infect Dis. 2008;46:1702–1709. doi: 10.1086/587899. [DOI] [PubMed] [Google Scholar]
- Wolday D, Akuffo H, Demissie A, Britton S. Role of Leishmania donovani and its lipophosphoglycan in CD4+ T-cell activation-induced human immunodeficiency virus replication. Infect Immun. 1999;67:5258–5264. doi: 10.1128/iai.67.10.5258-5264.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolday D, Berhe N, Akuffo H, Britton S. Leishmania-HIV interaction: immunopathogenic mechanisms. Parasitol Today. 1999;15:182–187. doi: 10.1016/s0169-4758(99)01431-3. [DOI] [PubMed] [Google Scholar]
- Wolday D, Berhe N, Akuffo H, Desjeux P, Britton S. Emerging Leishmania/HIV co-infection in Africa. Med Microbiol Immunol. 2001;190:65–67. doi: 10.1007/s004300100082. [DOI] [PubMed] [Google Scholar]
- Wolday D, Berhe N, Britton S, Akuffo H. HIV-1 alters T helper cytokines, interleukin-12 and interleukin-18 responses to the protozoan parasite Leishmania donovani. AIDS. 2000;14:921–929. doi: 10.1097/00002030-200005260-00003. [DOI] [PubMed] [Google Scholar]
- Zaph C, Uzonna J, Beverley SM, Scott P. Central memory T cells mediate long-term immunity to Leishmania major in the absence of persistent parasites. Nat Med. 2004;10:1104–1110. doi: 10.1038/nm1108. [DOI] [PubMed] [Google Scholar]