Abstract
Context:
Plyometric exercise has been recommended to prevent lower limb injury, but its feasibility in and effects on those with functional ankle instability (FAI) are unclear.
Objective:
To investigate the effect of integrated plyometric and balance training in participants with FAI during a single-legged drop landing and single-legged standing position.
Design:
Randomized controlled clinical trial.
Setting:
University motion-analysis laboratory.
Patients or Other Participants:
Thirty athletes with FAI were divided into 3 groups: plyometric group (8 men, 2 women, age = 23.20 ± 2.82 years; 10 unstable ankles), plyometric-balance (integrated)–training group (8 men, 2 women, age = 23.80 ± 4.13 years; 10 unstable ankles), and control group (7 men, 3 women, age = 23.50 ± 3.00 years; 10 unstable ankles).
Intervention(s):
A 6-week plyometric-training program versus a 6-week integrated-training program.
Main Outcome Measure(s):
Postural sway during single-legged standing with eyes open and closed was measured before and after training. Kinematic data were recorded during medial and lateral single-legged drop landings after a 5-second single-legged stance.
Results:
Reduced postural sway in the medial-lateral direction and reduced sway area occurred in the plyometric- and integrated-training groups. Generally, the plyometric training and integrated training increased the maximum angles at the hip and knee in the sagittal plane, reduced the maximum angles at the hip and ankle in the frontal and transverse planes in the lateral drop landing, and reduced the time to stabilization for knee flexion in the medial drop landing.
Conclusions:
After 6 weeks of plyometric training or integrated training, individuals with FAI used a softer landing strategy during drop landings and decreased their postural sway during the single-legged stance. Plyometric training improved static and dynamic postural control and should be incorporated into rehabilitation programs for those with FAI.
Key Words: plyometric training, balance training, landings, ankle injuries
Key Points
After 6 weeks of isolated plyometric or combined plyometric and balance training, people with functional ankle instability demonstrated increased lower extremity maximal sagittal-plane angles and decreased maximal frontal-plane and transverse-plane angles on ground contact.
Static and dynamic postural control improved with plyometric training, which should be included in rehabilitation programs for patients with functional ankle instability.
Ankle sprains often occur during physical activities such as basketball and soccer that require sudden stops, jumping, landing, and rotation around a planted foot. Although a patient with an ankle sprain may recover without experiencing persistent pain and swelling, most patients go on to develop chronic dysfunction, such as recurrent ankle sprain or instability.1 Athletes report a 73% recurrence rate of lateral ankle sprain,2 and the impairments associated with ankle sprain persist in 40% of patients 6 months after injury.3 These findings demonstrate that prolonged ankle dysfunction or disability is commonly attributable to ankle sprain.
Functional ankle instability (FAI) is identified in those with symptoms such as frequent episodes of ankle giving way and feelings of ankle instability4 after ankle sprains and often presents with sensorimotor deficits in muscle reaction time, joint position sense, postural sway, and time to stabilization (TTS) of ground reaction force.5,6 Several outcome measures, including center-of-pressure (COP) sway, leg reaching with the Star Excursion Balance Test, surface electromyography, and kinematics, are used to evaluate the neuromuscular and biomechanical characteristics of individuals with FAI. Measurement of COP sway during the single-legged stance is an easy way to evaluate static postural stability.7 People with ankle instability had greater variation in the magnitude of medial-lateral COP than a healthy group.8 In addition, TTS is effective for detecting differences between unstable and healthy groups.9,10 The TTS for ground reaction force is the time required to achieve stability after a dynamic perturbation, and this time is longer in those with FAI.9,11 In addition to TTS for ground reaction force, TTS for kinematics is a novel method to investigate the ability to regain balance in people with FAI; participants with FAI took longer TTS for ankle inversion after 1-legged hopping.12 The advantage of using TTS for kinematics instead of TTS for ground reaction force is to provide more specific information about dynamic neuromuscular control of body segments.
Rehabilitation programs for ankle sprain include muscle-strengthening, balance-training, neuromuscular-training, and proprioceptive-training protocols. The use of balance training for ankle reeducation has become common in recent years and is effective in reducing episodes of inversion.13 Balance training focuses on improving the ability to maintain a position through conscious and subconscious motor control.14 Certain tools, such as the balance board,15 Dura Disc, minitrampoline,16 biomechanical ankle platform system (BAPS),17 and Star Excursion Balance Test,18 can be used to assist training. In individuals with FAI, a 12-week BAPS exercise program with progressive testing reduced the radius of COP in single-legged standing.17 Another study19 showed that 4 weeks of balance improved shank-rearfoot coupling stability during walking. Proprioceptive training attempts to restore proprioceptive sensibility, retrain afferent pathways, and enhance the sensation of joint movement.14 Eils and Rosenbaum20 found that 6 weeks of multi-station proprioceptive exercise in individuals with ankle instability reduced the standard deviation of COP (referring to the 68.2% range of COP dispersion) and maximum sway of COP (referring to the maximum range of COP dispersion) in the medial-lateral direction. However, Coughlan and Caulfield21 reported no change in ankle kinematics during treadmill walking and running after a 4-week neuromuscular training program with the “both sides up” (BOSU) balance trainer.
Plyometric training has positive effects on sport performance, including distance running,22 jumping,23 sprinting, and leg-extension force.24 The focus of plyometric training is the stretch-shortening cycle induced in the muscle-tendon complex, where soft tissues repeatedly lengthen and shorten.25 Plyometric exercise is described as “reactive neuromuscular training”26 because it increases the excitability of the neurologic receptors and improves reactivity of the neuromuscular system. Plyometric training desensitizes the Golgi tendon organs through adaptation to the stretch-shortening exercise, which allows the elastic components of muscles to tolerate greater stretching.27 Previously, plyometric training was theorized to improve neuromuscular control and dynamic stability, reduce the incidence of serious knee injuries,28 and reduce the risk of injury by increasing functional joint stability of the lower limbs.23,28 Furthermore, 6 weeks of plyometric exercise enhanced results on functional performance testing in athletes after lateral ankle sprain.29 Plyometric exercise is thought to enable segments to absorb joint force effectively by promoting the mechanical advantage of soft tissue structures30 through increasing initial and maximal knee and hip flexion during the jump-landing task.30 The increased knee-flexion and hip-flexion angles during landing protect the knee via hamstrings tension.31,32
To date, investigations on the effect of plyometric training have emphasized functional performance28,29 or preventing anterior cruciate ligament injuries.33,34 Data on the feasibility and effectiveness of plyometric training in those with FAI are very limited.29 Therefore, our purposes were to determine the effects on lower extremity biomechanics of a 6-week plyometric-training program or a 6-week integrated program with plyometric and balance training in athletes with FAI. We hypothesized that both training programs would increase maximum joint angles in the sagittal plane and reduce the time needed to regain stability during drop-landing tasks. We further hypothesized that the integrated training would reduce postural sway during single-legged stance and decrease the center of mass (COM)-COP deviation during drop-landing tasks.
METHODS
Participants
Thirty collegiate athletes with ankle instability (10 participants in each group), aged 18 to 30 years, were recruited from local campuses (Table 1). All participants were screened with the Cumberland Ankle Instability Tool questionnaire.35 The inclusion criteria were (1) membership in a sport team (eg, basketball, rugby, soccer, volleyball) and performance of regular exercise; (2) at least 1 acute ankle-inversion sprain that resulted in swelling, pain, and dysfunction; (3) recurrent ankle sprains or ankle “giving way” in the past 12 months; (4) score of less than 24 on the Cumberland Ankle Instability Tool; and (5) clinically negative anterior drawer and talar tilt tests. For those with bilateral ankle injuries who met the inclusion criteria, the ankle with the lowest Cumberland Ankle Instability Tool score was selected. Thus, the total number of unstable ankles was 10 in each group. Any person who had any neurologic disorder, any severe lower extremity injury that affected equilibrium, or an ankle sprain within the past month was excluded. All participants were informed about the procedure and the purposes of this study and then gave informed consent. All procedures were approved by the Human Experiment and Ethics Committee of the University Hospital.
Table 1. .
Participant Demographics (Mean ± SD)
| Variable |
Group |
||
| Plyometric |
Balance + Plyometric (Integrated) |
Control |
|
| Sex | 8 men, 2 women | 8 men, 2 women | 7 men, 3 women |
| Total unstable ankles, No. (bilateral/unilateral) | 10 (3/7) | 10 (3/7) | 10 (2/8) |
| Age, y | 23.20 ± 2.82 | 23.80 ± 4.13 | 23.50 ± 3.00 |
| Height, cm | 169.30 ± 10.17 | 174.40 ± 7.56 | 170.60 ± 7.23 |
| Mass, kg | 69.40 ± 12.41 | 69.60 ± 8.64 | 70.30 ± 9.17 |
| Body mass index, kg/m2 | 24.14 ± 3.44 | 22.90 ± 2.55 | 24.15 ± 2.74 |
| Previous sprains in past 6 mo, No. | 1.60 ± 0.97 | 1.50 ± 1.08 | 1.70 ± 1.25 |
| Previous sprains in past 2 y, No. | 4.00 ± 2.54 | 3.50 ± 2.10 | 4.50 ± 2.78 |
| Baseline Cumberland Ankle Instability Tool score | 19.05 ± 2.88 | 17.56 ± 4.47 | 19.90 ± 3.41 |
Experimental Procedures
Single-Legged Standing Balance
Each participant was instructed to perform a single-legged stance on either the dominant side or the affected side with eyes open and eyes closed. Each participant was barefoot and kept the arms crossed at the chest. During the eyes-open condition, he or she was asked to look at an eye-level target 3 m ahead. Each successful trial required the person to remain as motionless as possible for 20 seconds.
Single-Legged Drop Landing
For the single-legged drop landing, the participant was instructed to hop medially or laterally off a 16-cm-high platform (Figure 1). He or she had to maintain the single-legged stance with hands on the waist while standing on the platform for 3 seconds as a preparatory posture. In response to an auditory cue, the person hopped down onto a force plate and regained stability as rapidly as possible, keeping the body erect and facing forward. The participant maintained the single-legged stance for 5 more seconds. A failure was defined as repetitive hopping on the force plate, taking the foot off the ground to regain balance, or moving the hands away from the waist.
Figure 1. .
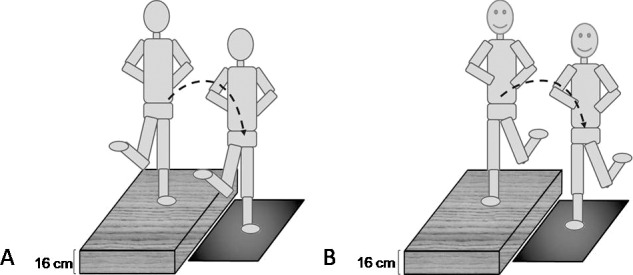
Illustration of dynamic postural-control tasks. A, Lateral drop-landing task (posterior view). B, Medial drop-landing task (anterior view).
We used a motion-capture system (model ProReflex MCV, type 170240; Qualisys AB, Gothenburg, Sweden) with 6 infrared cameras to collect marker trajectories at 200 Hz and synchronized it with 2 force plates (model AM FP4060-07-1000; Bertec Corporation, Columbus, OH) at a sampling rate of 1000 Hz. A modified Helen Hayes marker set with 23 markers was used. The markers were applied to the sacrum, bilateral anterior-superior iliac spines, lateral thighs, lateral knees, lateral shanks, lateral malleoli, toes (between second and third), posterior heels, and first and fifth metatarsal heads. The remaining 4 markers were applied to bilateral medial knee joints and medial malleoli for a static trial.
Data Reduction
Single-Legged Standing Balance
The middle 10 seconds of relative stability were analyzed. The standard deviation (SD) of the medial-lateral and anterior-posterior COP displacement in each trial represented the distribution of the COP sway level. The maximum ranges of the medial-lateral and anterior-posterior COP were the difference between maximum and minimum in the corresponding axis. The long and short axes of the ellipse were defined by 2 SDs of the medial-lateral and the anterior-posterior COP sway, respectively, and were used to construct the 95% elliptical sway area of COP.
Single-Legged Drop Landing
Kinematic data were filtered using a low-pass, fourth-order Butterworth filter at 8 Hz. The maximum and minimum angles at the hip (sagittal and transverse planes), knee (sagittal plane), and ankle (sagittal, frontal, and transverse planes) between contact and 500 milliseconds after contact were marked for analysis.36 Because the relative displacement between COM and COP is an important and sensitive value for examining postural stability,37 the maximum relative displacement between COM and COP was calculated at 2000 milliseconds after contact. The COM was assumed to be located at the pelvis center as determined by the markers on the bilateral anterior-superior iliac spine and 1 marker on the sacrum.
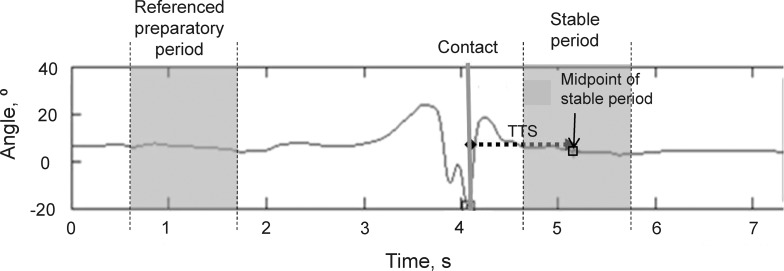
The TTS represented the time taken from foot contact on the ground to the midpoint of the stable condition (Figure 2).12 The stable period was detected with a 2000-millisecond moving window and was determined to occur when the mean joint angles of the hip, knee, and ankle fell within the range of ±1 SD of the corresponding mean angle of the referenced preparatory period. The referenced preparatory period was the time interval between 2000 and 3000 milliseconds before contact.
Figure 2. .
Measurement of the ankle-joint time to stabilization (TTS) in the drop-landing tasks (dorsiflexion [+], plantar flexion [−]). The TTS is the time from foot contact on the ground to the midpoint of the stable period.
Training Program
Participants were randomly assigned to the control group, plyometric-training group, or plyometric-with-balance (integrated)–training group. Each training program continued for 6 weeks, with 3 sessions per week (Table 2).15,38–41 Each individual was requested to participate in the training program for at least two-thirds of the sessions (ie, 12 of 18) to avoid being withdrawn from the study. Of the recruited participants, 2 were excluded due to ankle sprains incurred right after enrolling in the study. One licensed physical therapist trained all the participants and adjusted the intensity of the training protocol according to the ability and performance of each person.
Table 2. .
Plyometric- and Integrated-Training Exercise Programs38–41,a
| Weeks |
Plyometric Training |
Repetitions |
Session |
Integrated: Plyometric-Plus-Balance Training |
Repetitions or Time |
Sets |
| 1, 2 | Squat jumps | 10 | 2 | Squat jumps | 10 | 2 |
| Ankle jumps | 10 | 2 | Balanced squat | 10 | 2 | |
| Jump for distance | 10 | 2 | Balanced dribble | 20 | 5 | |
| Forward zigzag jumps | 10 | 3 | Forward zigzag jumps | 10 | 3 | |
| Lateral sawtooth jumps | 10 | 3 | Lateral sawtooth jumps | 10 | 3 | |
| Jump up on step | 8 | 2 | Jump up on step | 8 | 2 | |
| 3, 4 | Split-squat jumps (right/left) | 10 | 2 | Split-squat jumps (right/left) | 10 | 2 |
| Hop for distance (right/left) | 10 | 2 | Balance lunge (1 disc, right/left) | 10 | 2 | |
| Forward zigzag hops (right/left) | 10 | 3 | Forward zigzag hops (right/left) | 10 | 3 | |
| Lateral sawtooth hops (right/left) | 10 | 3 | Balanced single-leg standing (right/left) | 10 s | 5 | |
| Tuck jump | 10 | 2 | Tuck jump | 10 | 2 | |
| Diagonal hop | 8 | 2 | Balanced catch ball | 8 | 2 | |
| Jump up on step | 10 | 2 | Jump up on step | 10 | 2 | |
| 5, 6 | Cycled single-leg squat jumps | 10 | 2 | Cycled single-legged squat jumps | 10 | 2 |
| Hop on target (right/left) | 12 | 2 | Balance lunge (2 discs, right/left) | 12 | 2 | |
| Jump for distance and height | 10 | 2 | Jump for distance and high | 10 | 2 | |
| Forward zigzag hops (right/left) | 10 | 3 | Forward zigzag hops (right/left) | 10 | 3 | |
| Lateral sawtooth hops (right/left) | 10 | 3 | Balanced, single-legged standing dribble (right/left) | 20 | 5 | |
| Tuck jump | 10 | 2 | Tuck jump | 10 | 2 | |
| Agility ladder | 3 | 1 | Agility ladder | 3 | 1 | |
| Jump up on step | 10 | 2 | Jump up on step | 10 | 2 |
Each training section consisted of 3 minutes of general stretching exercise and 7 minutes of aerobic exercise (800-m run) as a warm-up. Between exercises in each training session, a 2-minute rest was allowed. For the cool-down phase, participants performed general stretching again for 5 minutes.
Statistical Analysis
Group demographics were compared with 1-way analysis of variance (ANOVA) using the Tukey post hoc test. Two-way, repeated-measures ANOVAs were used to evaluate the main effects of pretest-posttest and group and the interaction between pretest-posttest and group. Independent variables were the groups as the between-subjects variable and the conditions as the within-subject variable (pretraining, posttraining). If 1 or more of the overall tests was significant, we used the follow-up test to determine simple main effects. For the between-subjects factor, 1-way ANOVA with the Tukey post hoc test was used as the follow-up test; for the within-subject factor, the paired t test was used for follow-up.42 All statistical analyses were performed with SPSS for Windows (version 15.0; SPSS Inc, Chicago, IL).
RESULTS
Static Postural Sway
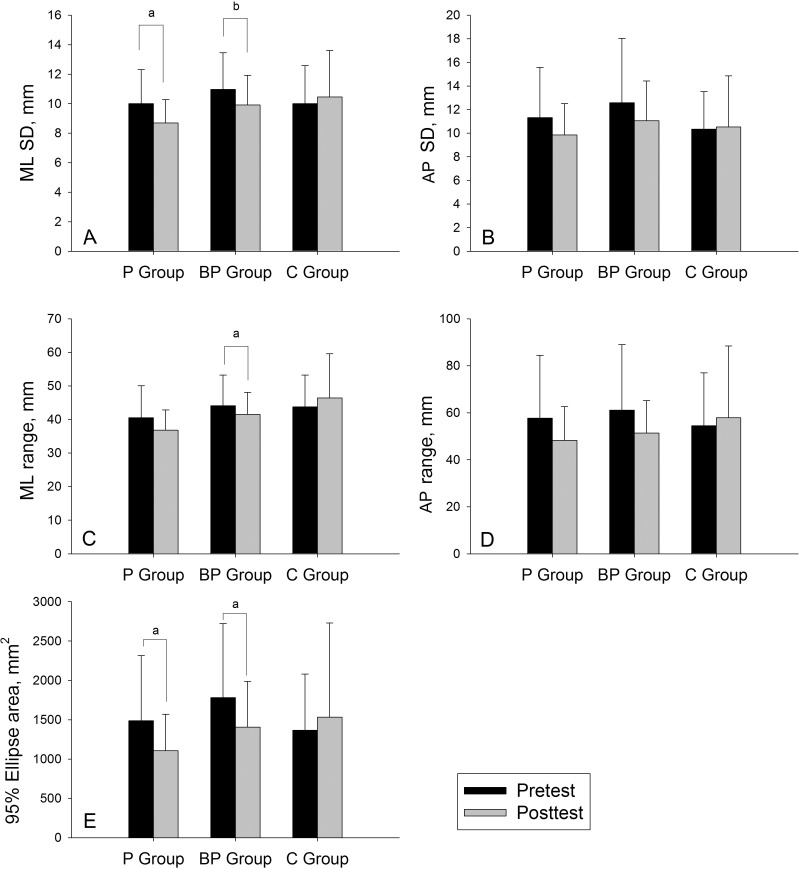
During single-legged standing, no significant main effect or interaction occurred for postural sway with eyes open or in the SD or maximal range of COP displacement in the anterior-posterior direction with eyes closed. During single-legged standing with eyes closed, both the plyometric group and integrated group had reduced SD of COP displacement in the medial-lateral direction (plyometric: t = 2.699, P = .013; integrated: t = 3.784, P = .001) and reduced sway area (plyometric: t = 2.739, P = .012; integrated: t = 2.279, P = .030); the integrated group also demonstrated reduced maximum range of COP displacement in the medial-lateral direction (t = 2.918, P = .007; Figure 3). In addition, a group effect was noted in the SD (F = 4.137, P = .019) and maximum range of medial-lateral direction (F = 6.521, P = .002), and further post hoc testing showed the plyometric group displayed smaller values than the control group after training.
Figure 3. .
Postural sway in single-legged standing with eyes closed in the plyometric (P), balance + plyometric (PB), and control (C) groups. A, Center of pressure (COP) SD in the medial-lateral (ML) and B, anterior-posterior (AP) directions. C, Maximal COP sway range in the ML and D, AP directions. E, 95% COP sway ellipse area. a P < .005. b P < .05.
Kinematics
The hip-, knee-, and ankle-joint angles during lateral drop landing and medial drop landing are summarized in Tables 3 and 4. In the lateral drop landing, both the plyometric and integrated groups showed increased maximum hip flexion, decreased maximum hip internal rotation, increased maximum knee flexion, and decreased maximum ankle inversion after training. The plyometric group also showed increased maximum ankle dorsiflexion, whereas the integrated group showed decreased maximum ankle external rotation. In the medial drop landing, the plyometric and integrated groups had increased maximum hip flexion and the integrated group increased maximum knee flexion and decreased maximum ankle eversion. Maximal ankle inversion decreased in all 3 groups.
Table 3. .
Lateral Drop-Landing Task: Joint Kinematic Variables and Results of Analysis of Variance and Post Hoc Tests
| Joint, Plane |
Kinematic Variable |
Group, Mean ± SD (95% Confidence Interval) |
Interaction Effect (F2,87) |
Group Effect (F2,87) |
Test-Time Effect (F1,88) |
|||||
| Plyometric |
Integrated: Balance + Plyometric |
Control |
||||||||
| Pretest |
Posttest |
Pretest |
Posttest |
Pretest |
Posttest |
|||||
| Hip, sagittal | Maximum flexion (+) | 28.91 ± 4.18 (27.35, 30.47) | 39.27 ± 9.62a (35.68, 42.86) | 28.37 ± 3.29 (27.14, 29.60) | 38.24±4.57a (36.54, 39.95) | 30.14±6.13 (27.86, 32.43) | 29.93±6.63b (27.46, 32.41) | F = 21.688 | F = 5.571 | F = 81.356 |
| P < .001 | P = .005 | P < .001 | ||||||||
| Maximum extension (−) | 20.03 ± 2.95 (18.93, 21.13) | 18.31 ± 5.35 (16.31, 20.31) | 20.16 ± 2.33 (19.29, 21.03) | 19.26 ± 5.06 (17.37, 21.14) | 19.62 ± 3.08 (18.47, 20.77) | 18.73 ± 2.30 (17.87, 19.59) | F = 0.292 | F = 0.362 | F = 5.241 | |
| P = .748 | P = .697 | P = .024 | ||||||||
| Hip, transverse | Maximum external rotation (+) | 3.72 ± 4.31 (2.11, 5.33) | 2.72 ± 5.77 (0.57, 4.87) | 2.78 ± 5.61 (0.68, 4.88) | 2.25 ± 4.94 (0.40, 4.10) | 2.80 ± 4.60 (1.08, 4.51) | 3.00 ± 4.47 (1.33, 4.66) | F = 0.278 | F = 0.247 | F = 0.452 |
| P = .758 | P = .781 | P = .503 | ||||||||
| Maximum internal rotation (−) | −13.25 ± 5.21 (−15.19, −11.30) | −10.81 ± 5.16 (−12.73, −8.88) | −13.44 ± 5.03 (−15.32, −11.57) | −10.3 ± 4.84c(−12.12, −8.50) | −12.84 ± 4.65 (−14.58, −11.10) | − 14.4 ± 4.93d (−16.31, −12.63) | F= 4.735 | F = 2.050 | F = 3.712 | |
| P = .011 | P = .135 | P = .057 | ||||||||
| Knee, sagittal | Maximum flexion (+) | 50.18 ± 6.45 (47.77, 52.59) | 53.14 ± 8.51e (49.96. 56.31) | 48.04 ± 6.66 (45.44, 50.53) | 52.33 ± 7.47e (49.54, 55.12) | 48.85 ± 5.58 (46.76, 50.93) | 49.04 ± 5.13 (47.12, 50.95) | F = 4.293 | F = 1.471 | F = 18.148 |
| P = .017 | P = .235 | P < .001 | ||||||||
| Maximum extension (−) | 12.73 ± 5.11 (10.82, 14.63) | 12.48 ± 5.98 (10.24, 14.71) | 12.74 ± 4.57 (11.04, 14.45) | 12.75 ± 4.28 (11.15, 14.35) | 13.17 ± 5.44 (11.14, 15.21) | 14.87 ± 5.33 (12.88, 16.86) | F = 1.072 | F = 0.982 | F = −0.680 | |
| P = .374 | P = .379 | P = .412 | ||||||||
| Ankle, sagittal | Maximum flexion (+) | 18.16 ± 2.56 (17.21, 19.12) | 21.21 ± 2.18f,g(20.40, 22.02) | 19.16 ± 4.61 (17.44, 20.88) | 18.50 ± 5.26 (16.53, 20.47) | 19.86 ± 3.62 (18.51, 21.21) | 20.12 ± 3.57 (18.78, 21.45) | F = 13.795 | F = 0.883 | F = 8.614 |
| P < .01 | P = .418 | P = .004 | ||||||||
| Maximum extension (−) | −17.06 ± 4.76 (−18.84, −15.28) | −16.17 ± 5.01 (−18.04, −14.29) | −16.04 ± 5.25 (−18.00, −14.08) | −14.73 ± 4.78 (−16.51, −12.94) | −15.98 ± 5.56 (−18.06, −13.91) | −16.30 ± 4.85 (−18.11, −14.49) | F = 1.187 | F = 0.549 | F = 2.001 | |
| P = .310 | P = .579 | P = .161 | ||||||||
| Ankle, frontal | Maximum inversion (+) | 8.35 ± 2.98 (7.24, 9.47) | 6.92 ± 2.71h(5.91, 7.93) | 7.98 ± 2.83 (6.92, 9.03) | 6.59 ± 2.01 (5.84, 7.34) | 6.95 ± 3.19 (5.76, 8.14) | 7.42 ± 2.77 (6.39, 8.46) | F = 3.138 | F = 0.347 | F = 4.876 |
| P = .048 | P = .708 | P = .030 | ||||||||
| Maximum eversion (−) | −1.69 ± 0.75 (−1.97, −1.41) | −1.58 ± 1.50 (−2.14, −1.02) | −1.88 ± 1.11 (−2.29, −1.47) | −1.60 ± 1.10 (−2.01, −1.18) | −1.57 ± 0.64 (−1.80, −1.33) | −1.41 ± 1.02 (−1.79, −1.03) | F = 0.098 | F = 0.989 | F = 1.183 | |
| P = .907 | P = .376 | P = .280 | ||||||||
| Ankle, transverse | Maximum external rotation (+) | 18.35 ± 6.51 (15.92, 20.79) | 17.14 ± 7.31 (14.41, 19.87) | 20.92 ± 7.09 (18.28, 23.57) | 13.92 ±7.81i (11.00, 16.84) | 19.96 ± 6.61 (17.49, 22.42) | 21.05 ± 6.52j (18.61, 23.48) | F = 8.163 | F = 2.608 | F = 7.955 |
| P = .001 | P = .079 | P = .024 | ||||||||
| Maximum internal rotation (−) | 4.06 ± 5.84 (1.88, 6.24) | 4.04 ± 5.61 (2.39, 5.68) | 4.65 ± 4.55 (2.95, 6.34) | 4.42 ± 4.41 (2.66, 6.18) | 5.96 ± 6.01 (3.71, 8.20) | 5.52 ± 5.93 (3.30, 7.73) | F = 0.035 | F = 1.250 | F = 0.122 | |
| P = .966 | P = .292 | P = .728 | ||||||||
Indicates increased maximal hip flexion in plyometric (t = −5.28, P < .001)- and integrated (t = −10.69, P < .001)-training groups.
Indicates less posttest hip maximal flexion in the control group than in the plyometric- or integrated-training groups (F = 15.00, P < .001).
Indicates decreased maximal hip internal-rotation angle in the integrated-training group (t = −2.72, P = .011).
Indicates greater posttest hip maximal internal rotation in the control group than in the integrated-training group (F = 6.25, P = .003).
Indicates increased maximal knee flexion in the plyometric (t = −2.19, P = .037)- and integrated (t = −4.30, P < .001)-training groups.
Indicates increased maximal ankle dorsiflexion in the plyometric-training group (t = −5.00, P < .001).
Indicates greater posttest ankle maximal dorsiflexion in the plyometric-training group than in the integrated-training group (F = 3.70, P = .029).
Indicates decreased maximal ankle inversion in the integrated-training group (t = 2.62, P = .014).
Indicates decreased maximal ankle external rotation in the integrated-training group (t = 4.74, P < .001).
Indicates greater maximal ankle external rotation in the control group than the integrated-training group (F = 7.31, P = .001).
Table 4. .
Medial Drop-Landing Task: Joint Kinematic Variables and Results of Analysis of Variance and Post Hoc Tests
| Joint, Plane |
Kinematic Variable |
Group, Mean ± SD (95% Confidence Interval) |
Interaction Effect (F2,87) |
Group Effect (F2,87) |
Test-Time Effect (F1,88) |
|||||
| Plyometric |
Integrated: Balance + Plyometric |
Control |
||||||||
| Pretest |
Posttest |
Pretest |
Posttest |
Pretest |
Posttest |
|||||
| Hip, sagittal | Maximal flexion (+) | 31.73 ± 6.68 (29.23, 34.22) | 40.95 ± 9.84a (37.28, 44.63) | 29.64 ± 5.34 (27.65, 31.63) | 40.96 ± 8.55a (37.76, 44.15) | 34.24 ± 7.21 (29.31, 34.93) | 32.17 ± 7.39b (29.33, 34.41) | F = 22.773 | F = 3.412 | F = 81.111 |
| P < .001 | P = .037 | P < .001 | ||||||||
| Maximal extension (−) | 13.13 ± 2.78 (12.09, 14.17) | 13.93 ± 4.68 (12.18, 15.67) | 12.58 ± 3.19 (11.39, 13.77) | 15.26 ± 5.14c (13.35, 17.18) | 13.69 ± 2.56 (12.73, 14.64) | 14.34 ± 5.53 (12.28, 16.41) | F = 1.509 | F = 0.184 | F = 6.732 | |
| P = .227 | P = .832 | P = .011 | ||||||||
| Hip, transverse | Maximal external rotation (+) | 1.26 ± 3.29 (0.04, 2.49) | 1.98 ± 4.71 (0.22, 3.74) | 1.21 ± 4.79 (−0.58, 2.99) | 1.19 ± 4.26 (−0.40, 2.78) | 2.41 ± 5.88 (0.21, 4.61) | 1.83 ± 5.04 (−0.05, 3.71) | F = 0.595 | F = 0.377 | F = 0.007 |
| P = .554 | P =.687 | P = .934 | ||||||||
| Maximal internal rotation (−) | −15.11 ± 3.08 (−16.26, −13.96) | −13.68 ± 3.04 (−14.82, −12.55) | −15.61 ± 4.07 (−17.13, −14.09) | −13.04 ± 5.72 (−15.17, −10.90) | −13.52 ± 4.63 (−15.25, −11.80) | −13.43 ± 5.8 (−15.87, −11.43) | F = 1.581 | F = 0.497 | F = 4.306 | |
| P = .212 | P = .610 | P = .041 | ||||||||
| Knee, sagittal | Maximal flexion (+) | 52.05 ± 8.45 (48.90, 55.20) | 54.46 ± 10.89 (50.39, 58.53) | 51.20 ± 9.68 (47.59, 54.82) | 56.43 ± 8.57d (53.23, 59.64) | 51.40 ± 5.68 (49.28, 53.42) | 50.31 ± 3.83e (48.88, 51.74) | F = 9.407 | F = 1.251 | F = 13.457 |
| P < .001 | P = .291 | P ≤ .001 | ||||||||
| Maximal extension (-) | 14.63 ± 3.86 (13.19, 16.07) | 16.63 ± 6.20 (14.32, 18.95) | 13.15 ± 4.98 (11.29, 15.01) | 13.77 ± 6.73 (11.26, 16.29) | 14.34 ± 4.63 (12.61, 16.07) | 14.48 ± 4.46 (12.81, 16.14) | F = 0.838 | F = 1.862 | F = 2.265 | |
| P = .436 | P = .161 | P = .136 | ||||||||
| Ankle, sagittal | Maximal flexion (+) | 21.84 ± 3.12 (20.67, 23.00) | 23.25 ± 3.12 (22.09, 24.42) | 20.05 ± 5.51 (17.99, 22.11) | 19.04 ± 5.50f (16.99, 21.09) | 22.65 ± 2.36 (21.77, 23.53) | 23.78 ± 3.10 (22.62, 24.94) | F = 2.495 | F = 10.796 | F = 1.109 |
| P = .088 | P < .001 | P = .295 | ||||||||
| Maximal extension (−) | −16.73 ± 3.44 (−18.01, −15.44) | −16.50 ± 4.18 (−18.06, −14.95) | −16.87 ± 5.28 (−18.87, −14.90) | −15.12 ± 8.86 (−18.43, −11.81) | −17.15 ± 6.08 (−19.42, −14.88) | −17.13 ± 5.05 (−19.01, −15.24) | F = 0.684 | F = 0.425 | F = 1.018 | |
| P = .507 | P = .655 | P = .316 | ||||||||
| Ankle, frontal | Maximal inversion (+) | 12.79 ± 4.87 (10.97, 14.61) | 9.28 ± 4.77g (7.50, 11.06) | 13.33 ± 6.05 (11.07, 15.59) | 8.05 ± 5.80g (5.89, 10.22) | 12.11 ± 6.10 (9.83, 14.39) | 11.06 ± 4.15g (9.51, 12.61) | F = 3.565 | F = 0.318 | F = 25.489 |
| P = .033 | P = .728 | P < .001 | ||||||||
| Maximal eversion (−) | −4.53 ± 2.76 (−5.56, −3.50) | −2.14 ± 2.32h (−3.00, −1.27) | −3.78 ± 2.46 (−4.70, −2.86) | −2.54 ± 2.86h (−3.61, −1.47) | −3.64 ± 2.05 (−4.40, −2.88) | −3.26 ± 1.37h (−2.28, −1.25) | F = 2.709 | F =1.181 | F = 14.137 | |
| P = .072 | P = .312 | P < .001 | ||||||||
| Ankle, transverse | Maximal external rotation (+) | 11.36 ± 5.82 (9.19, 13.54) | 12.03 ± 5.97 (9.80, 14.26) | 12.98 ± 4.73 (11.22, 14.75) | 12.58 ± 7.10 (9.93, 15.23) | 12.48 ± 8.61 (9.19, 15.76) | 14.81 ± 8.45 (11.65, 17.96) | F = 0.838 | F = 0.902 | F = 0.995 |
| P = .436 | P = .410 | P = .321 | ||||||||
| Maximal internal rotation (−) | 1.40 ± 3.44 (0.11, 2.69) | 0.94 ± 4.73 (−0.48, 2.35) | 1.84 ± 2.29 (0.98, 2.69) | 1.35 ± 2.64 (0.37, 2.34) | 2.33 ± 2.96(1.23, 3.44) | 2.62 ± 4.05 (1.11, 4.13) | F = 0.378 | F = 1.973 | F = 0.287 | |
| P = .686 | P = .145 | P = .594 | ||||||||
Indicates increased maximal hip flexion in the plyometric (t = − 6.553, P < .001) and integrated-training groups (F = 7.863, P < .001).
Indicates less maximal hip flexion in the control group than in the plyometric- and integrated-training groups (F = 11.459, P < .001).
Indicates decreased maximal hip extension in the integrated-training group (t = −2.665, P = .012).
Indicates increased maximal knee flexion in the integrated-training group (t = −5.203, P < .001).
Indicates less maximal knee flexion in the control group than in the integrated-training group (F = 4.248, P = .017).
Indicates less maximal ankle dorsiflexion in the integrated-training group than in the plyometric-training and control groups (F = 12.248, P < .001).
Indicates decreased maximal ankle inversion in the plyometric-training (t = 3.405, P = .012) and integrated-training (t = 3.996, P = .001) groups.
Indicates decreased maximal ankle eversion in the plyometric-training (t = −3.071, P = .005), integrated-training (t = −2.212, P = .035), and control groups (t = −4.037, P < .001).
Time to Stabilization
We found no changes in TTS for hip, knee, or ankle angles in the lateral drop landing posttraining. In the medial drop landing, TTS for knee-flexion angle was reduced in both the plyometric group (pretraining = 3.08 ± 1.05 seconds, posttraining = 1.63 ± 0.43 seconds) and the integrated group (pretraining = 2.74 ± 1.45 seconds, posttraining = 1.65 ± 0.88 seconds) posttraining (P < .001).
Center of Mass and Center of Pressure
The relative displacement between COM and COP at 2000 milliseconds after landing was reduced in the medial-lateral direction in the plyometric group (pretest = 258.38 ± 87.34 mm, posttest = 209.09 ± 102.11 mm, t = 3.425, P = .002) in the lateral drop landing.
DISCUSSION
Both experimental groups showed reduced static postural sway in single-legged standing with eyes closed. Generally, the isolated plyometric training and integrated training increased the maximum sagittal angles at the hip and knee but reduced the maximum angles in the frontal and transverse planes at the hip and ankle.
Static Postural Sway
People with unstable ankles have greater medial and lateral postural sway than those with stable ankles.43 Thus, evaluation of medial-lateral postural sway is critical to examine the effect of training on participants with FAI, even though Knapp et al44 suggested that no single balance measure from a force plate could discriminate healthy from unstable ankles. Our results showed that both the plyometric training and integrated training improved the SD of COP displacement in the medial-lateral direction during the single-legged stance with eyes closed. Therefore, both programs positively affected static postural control in those with ankle instability. Postural control relies on afferent information (ie, visual, vestibular, and somatosensory systems) and efferent response (ie, muscle contraction and reflexes),45 as well as feed-forward and feedback neuromuscular control.30,46 When vision is absent, input depends on the somatosensory and vestibular systems.43 The decreased postural sway suggests that the plyometric training or integrated training improved certain elements of postural control, such as afferent pathways or efferent pathways. The mechanoreceptors within joints may efficiently detect the changes and give more appropriate proprioceptive information after training. In addition, the afferent tract may become more efficient in transmitting the signal, and the efferent outputs (muscle contraction and the efferent tract) may improve after training. The training programs in this study were intensive, and the efferent tract may have benefitted from repetitive jump-landing or balance tasks through feed-forward and feedback neuromuscular control.
Maximum Angles
Generally, our results showed that the plyometric training and integrated training increased the maximum angles at the hip and knee in the sagittal plane and reduced the maximum angles in the transverse plane at the hip and in the frontal and transverse planes at the ankle.
Sagittal Plane
Hip- and knee-flexion angles increased after plyometric training and after integrated training in both drop-landing tasks. In another study,47 the control group had larger knee-flexion angles at single-legged landing from a vertical jump than participants with chronic ankle instability. Increased hip-flexion and knee-flexion angles during the jump-landing task enable the body to absorb joint forces more effectively40 and to promote the mechanical advantage of the soft tissue structures that provide joint stability.30,48 Increased knee-flexion angle during landing has also been considered an impact-attenuation strategy.49 Thus, both the plyometric and integrated training had positive effects on landings.
Furthermore, increased maximum ankle dorsiflexion during the lateral drop landing occurred in the plyometric group only. Delahunt et al50 found less ankle dorsiflexion from 90 to 200 milliseconds after contact in those with FAI than in healthy participants during a single-legged forward drop jump. The increased ankle motion may increase shock attenuation at the ankle joint.51 However, we found a training effect on ankle motion in the lateral drop landing but not in the medial drop landing. The main reason may be a ceiling effect such that the sagittal angle of the ankle was near its maximum range during the medial drop landing.
Frontal Plane
Isolated plyometric training and integrated training decreased maximum ankle inversion in the lateral drop landing. Thus, both programs improved ankle joint stability and prevented excessive inversion. However, decreased maximum ankle inversion during the medial drop landing occurred in all 3 groups; this is likely a self-protective strategy for participants with FAI.
Transverse Plane
Plyometric training and integrated training decreased maximum hip internal rotation in the lateral drop landing. The hip joint has been considered a primary support and a stabilizing mechanism for absorbing impact in landings.49,52 We believed that if the displacement of the proximal joint was less, the distal joint would maintain balance more easily. Because the hip joint is a ball-and-socket joint that allows multidirectional motions, the dynamic stabilizers are important for stability.53 The decreased hip internal-rotation angle displayed in the lateral drop landing may result from increased hip external-rotator strength or increased agonist and antagonist cocontraction. Yet, maximum hip external rotation increased during the medial drop landing in the integrated group. These participants tended to use greater hip range of motion in the transverse plane for regaining equilibrium. Different strategies used in the lateral drop landing and the medial drop landing were associated with movement directions. In other words, integrated training facilitated the FAI group to use the hip-stability strategy during the lateral drop landing but the hip-mobility strategy during the medial drop landing. A stability strategy tends to decrease the motion of the hip joint (a stiff landing), whereas a mobility strategy (a soft landing) tends to increase the motion of the hip joint during movement.
Center of Mass and Center of Pressure
Balance training and plyometric training improved postural sway, both in static and dynamic conditions. Myer et al33 reported that plyometric training and dynamic-stabilization training decreased the SD of the medial-lateral COP during a single-legged hop landing on the dominant side of healthy females. Paterno et al34 found similar results: A comprehensive neuromuscular protocol (combined with dynamic balance and plyometric training) improved body sway in the anterior-posterior direction. However, we believed that COP measures could not reflect actual performance on the drop-landing task, which includes a transitional period from a dynamic condition to a static condition. We thus used the relative displacement between COM and COP to analyze postural control of individuals with FAI and to determine the training effect. Although the COM was based on the pelvic markers, not a weighted sum of whole-body segments, the relative displacement between assumed COM and COP still provides information about control of postural stability.
In the lateral drop landing, relative displacement between COM and COP in the medial-lateral direction decreased in the plyometric group but not in the integrated group, although the kinematic changes in the 2 groups were similar. This finding did not support our original hypothesis that reduced relative displacement between COM and COP would occur in the integrated group, due to its greater focus on COM control compared with the plyometric group. Reducing the relative displacement between COM and COP in a single-legged stance decreases weight bearing on the stance limb by mechanical advantage, so the plyometric group used an energy-efficient method to regain balance. Additionally, the reduced relative displacement between COM and COP in the medial-lateral direction may be related to lower extremity motion. In our study, both the plyometric and integrated groups increased maximum hip- and knee-flexion angles, but only the plyometric group increased maximum ankle-dorsiflexion angle. A greater flexion angle in the sagittal plane lowers the COM. A lower COM resulting from changes in the ankle-dorsiflexion angle should be the key element to reduce the relative displacement between COM and COP in the plyometric group. In addition, decreased maximum ankle inversion may help the COM align well with COP in the medial-lateral direction and decrease COP sway.
Time to Stabilization
The TTS of joint angle represents dynamic postural control: A larger TTS value represents poorer dynamic postural control. Participants with ankle instability took longer than controls to regain stability after landing from a single-legged hop.12 The authors also suggested that when an individual takes a longer time to regain balance, the ankle is exposed to a higher risk of a sprain or rolling.
Our results revealed that TTS for knee-flexion angle decreased in the plyometric and integrated groups in the medial drop landing but not in the lateral drop landing. After landing, the knee flexes to absorb impact and reduce the COM to maintain equilibrium. After plyometric or integrated training, the knee becomes stronger and better able to cope with external disturbances. This strategy enables the knee joint to regain knee extension faster and thus decreases the TTS of the knee-flexion angle. The changes in TTS for the knee-flexion angle but lack of changes in ankle kinematics suggest that both the plyometric and integrated training improved the participants' ability to regain postural equilibrium by modulating the knee joint instead of the ankle joint. As mentioned earlier, the kinematics required for the medial drop landing and lateral drop landing are different. We suggest that enhanced knee-joint stability control may be necessary to compensate for insufficient control at the ankle joint, even though greater ankle excursion is required to regain equilibrium during the medial drop landing.
Several limitations of the present study must be acknowledged. During the group allocation, men and women were not separated. We did not expect sex to influence the interpretation because we compared training effects within participants. Athletes with bilateral ankle instability were also recruited, but only the limb with the lower Cumberland Ankle Instability Tool score was studied. In addition, although we recruited individuals with FAI, ankle instability varies among individuals and may reflect different levels of severity and different limitations on sport participation. Furthermore, we did not investigate retention of the training effect, although we will do so in the future. In addition, we assumed the COM location to be at the center of the pelvis as determined by the markers on the sacrum and bilateral anterior-superior iliac spine. A complete whole-body segment model to determine a more accurate COM is required in a future study.
CONCLUSIONS
The isolated plyometric exercise and integrated training with plyometric and balance exercise both increased the maximum angles in the sagittal plane and decreased the maximum angle in the frontal and transverse planes of the lower extremities after contact with the ground. Also, isolated plyometric training improved static and dynamic postural control and should be incorporated into rehabilitation programs for those with FAI.
REFERENCES
- 1.Freeman MA. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47(4):669–677. [PubMed] [Google Scholar]
- 2.Yeung MS, Chan KM, So CH, Yuan WY. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28(2):112–116. doi: 10.1136/bjsm.28.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653–660. doi: 10.1177/107110079801901002. [DOI] [PubMed] [Google Scholar]
- 4.Delahunt E, Coughlan GF, Caulfield B, Nightingale EJ, Lin CW, Hiller CE. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med Sci Sports Exerc. 2010;42(11):2106–2121. doi: 10.1249/MSS.0b013e3181de7a8a. [DOI] [PubMed] [Google Scholar]
- 5.Hiller CE, Nightingale EJ, Lin CW, Coughlan GF, Caulfield B, Delahunt E. Characteristics of people with recurrent ankle sprains: a systematic review with meta-analysis. Br J Sports Med. 2011;45(8):660–672. doi: 10.1136/bjsm.2010.077404. [DOI] [PubMed] [Google Scholar]
- 6.Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport. 2009;13(1):2–12. doi: 10.1016/j.jsams.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Konradsen L. Sensori-motor control of the uninjured and injured human ankle. J Electromyogr Kinesiol. 2002;12(3):199–203. doi: 10.1016/s1050-6411(02)00021-4. [DOI] [PubMed] [Google Scholar]
- 8.Wang HK, Chen CH, Shiang TY, Jan MH, Lin KH. Risk-factor analysis of high school basketball-player ankle injuries: a prospective controlled cohort study evaluating postural sway, ankle strength, and flexibility. Arch Phys Med Rehabil. 2006;87(6):821–825. doi: 10.1016/j.apmr.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 9.Wikstrom EA, Tillman MD, Borsa PA. Detection of dynamic stability deficits in subjects with functional ankle instability. Med Sci Sports Exerc. 2005;37(2):169–175. doi: 10.1249/01.mss.0000149887.84238.6c. [DOI] [PubMed] [Google Scholar]
- 10.Arnold BL, De La Motte S, Linens S, Ross SE. Ankle instability is associated with balance impairments: a meta-analysis. Med Sci Sports Exerc. 2009;41(5):1048–1062. doi: 10.1249/MSS.0b013e318192d044. [DOI] [PubMed] [Google Scholar]
- 11.Ross SE, Guskiewicz KM, Yu B. Single-leg jump-landing stabilization times in subjects with functionally unstable ankles. J Athl Train. 2005;40(4):298–304. [PMC free article] [PubMed] [Google Scholar]
- 12.de Noronha M, Refshauge KM, Crosbie J, Kilbreath SL. Relationship between functional ankle instability and postural control. J Orthop Sports Phys Ther. 2008;38(12):782–789. doi: 10.2519/jospt.2008.2766. [DOI] [PubMed] [Google Scholar]
- 13.Loudon JK, Santos MJ, Franks L, Liu W. The effectiveness of active exercise as an intervention for functional ankle instability: a systematic review. Sports Med. 2008;38(7):553–563. doi: 10.2165/00007256-200838070-00003. [DOI] [PubMed] [Google Scholar]
- 14.Dutton M. Intervention principles. In: Sutton M, editor. Orthopaedic Examination, Evaluation, and Intervention. New York, NY: McGraw-Hill;; 2004. pp. 306–308. In. ed. [Google Scholar]
- 15.Verhagen E, Bobbert M, Inklaar M, et al. The effect of a balance training programme on centre of pressure excursion in one-leg stance. Clin Biomech (Bristol, Avon) 2005;20(10):1094–1100. doi: 10.1016/j.clinbiomech.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 16.Kidgell DJ, Horvath DM, Jackson BM, Seymour PJ. Effect of six weeks of Dura Disc and mini-trampoline balance training on postural sway in athletes with functional ankle instability. J Strength Cond Res. 2007;21(2):466–469. doi: 10.1519/R-18945.1. [DOI] [PubMed] [Google Scholar]
- 17.Lee AJ, Lin WH. Twelve-week biomechanical ankle platform system training on postural stability and ankle proprioception in subjects with unilateral functional ankle instability. Clin Biomech (Bristol, Avon) 2008;23(8):1065–1072. doi: 10.1016/j.clinbiomech.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 18.Chaiwanichsiri D, Lorprayoon E, Noomanoch L. Star excursion balance training: effects on ankle functional stability after ankle sprain. J Med Assoc Thai. 2005;88(suppl 4):S90–S94. [PubMed] [Google Scholar]
- 19.McKeon PO, Paolini G, Ingersoll CD, et al. Effects of balance training on gait parameters in patients with chronic ankle instability: a randomized controlled trial. Clin Rehabil. 2009;23(7):609–621. doi: 10.1177/0269215509102954. [DOI] [PubMed] [Google Scholar]
- 20.Eils E, Rosenbaum D. A multi-station proprioceptive exercise program in patients with ankle instability. Med Sci Sports Exerc. 2001;33(12):1991–1998. doi: 10.1097/00005768-200112000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Coughlan G, Caulfield B. A. 4-week neuromuscular training program and gait patterns at the ankle joint. J Athl Train. 2007;42(1):51–59. [PMC free article] [PubMed] [Google Scholar]
- 22.Spurrs RW, Murphy AJ, Watsford ML. The effect of plyometric training on distance running performance. Eur J Appl Physiol. 2003;89(1):1–7. doi: 10.1007/s00421-002-0741-y. [DOI] [PubMed] [Google Scholar]
- 23.Kubo K, Morimoto M, Komuro T, et al. Effects of plyometric and weight training on muscle-tendon complex and jump performance. Med Sci Sports Exerc. 2007;39(10):1801–1810. doi: 10.1249/mss.0b013e31813e630a. [DOI] [PubMed] [Google Scholar]
- 24.Toumi H, Best TM, Martin A, F'Guyer S, Poumarat G. Effects of eccentric phase velocity of plyometric training on the vertical jump. Int J Sports Med. 2004;25(5):391–398. doi: 10.1055/s-2004-815843. [DOI] [PubMed] [Google Scholar]
- 25.Komi PV. Strength and Power in Sport. Hoboken, NJ: Blackwell Science Ltd;; 2003. Stretch-shortening cycle; pp. 184–202. In. [Google Scholar]
- 26.Wilk KE, Voight ML, Keirns MA, Gambetta V, Andrews JR, Dillman CJ. Stretch-shortening drills for the upper extremities: theory and clinical application. J Orthop Sports Phys Ther. 1993;17(5):225–239. doi: 10.2519/jospt.1993.17.5.225. [DOI] [PubMed] [Google Scholar]
- 27.Hutton RS, Atwater SW. Acute and chronic adaptations of muscle proprioceptors in response to increased use. Sports Med. 1992;14(6):406–421. doi: 10.2165/00007256-199214060-00007. [DOI] [PubMed] [Google Scholar]
- 28.Chimera NJ, Swanik KA, Swanik CB, Straub SJ. Effects of plyometric training on muscle-activation strategies and performance in female athletes. J Athl Train. 2004;39(1):24–31. [PMC free article] [PubMed] [Google Scholar]
- 29.Ismail MM, Ibrahim MM, Youssef EF, El Shorbagy KM. Plyometric training versus resistive exercises after acute lateral ankle sprain. Foot Ankle Int. 2010;31(6):523–530. doi: 10.3113/FAI.2010.0523. [DOI] [PubMed] [Google Scholar]
- 30.Lephart S, Abt JP, Ferris C, et al. Neuromuscular and biomechanical characteristic changes in high school athletes: a plyometric versus basic resistance program. Br J Sports Med. 2005;39(12):932–938. doi: 10.1136/bjsm.2005.019083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Renstrom P, Arms SW, Stanwyck TS, Johnson RJ, Pope MH. Strain within the anterior cruciate ligament during hamstring and quadriceps activity. Am J Sports Med. 1986;14(1):83–87. doi: 10.1177/036354658601400114. [DOI] [PubMed] [Google Scholar]
- 32.Hirokawa S, Solomonow M, Luo Z, Lu Y, D'Ambrosia R. Muscular co-contraction and control of knee stability. J Electromyogr Kinesiol. 1991;1(3):199–208. doi: 10.1016/1050-6411(91)90035-4. [DOI] [PubMed] [Google Scholar]
- 33.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric vs. dynamic stabilization and balance training on power, balance, and landing force in female athletes. J Strength Cond Res. 2006;20(2):345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 34.Paterno MV, Myer GD, Ford KR, Hewett TE. Neuromuscular training improves single-limb stability in young female athletes. J Orthop Sports Phys Ther. 2004;34(6):305–316. doi: 10.2519/jospt.2004.34.6.305. [DOI] [PubMed] [Google Scholar]
- 35.Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland Ankle Instability Tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87(9):1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 36.Ford KR, Myer GD, Smith RL, Vianello RM, Seiwert SL, Hewett TE. A comparison of dynamic coronal plane excursion between matched male and female athletes when performing single leg landings. Clin Biomech (Bristol, Avon) 2006;21(1):33–40. doi: 10.1016/j.clinbiomech.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 37.Hahn ME, Chou LS. Age-related reduction in sagittal plane center of mass motion during obstacle crossing. J Biomech. 2004;37(6):837–844. doi: 10.1016/j.jbiomech.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 38.Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 39.McGuine TA, Keene JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med. 2006;34(7):1103–1111. doi: 10.1177/0363546505284191. [DOI] [PubMed] [Google Scholar]
- 40.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34(3):445–455. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 41.Sedano Campo S, Vaeyens R, Philippaerts RM, Redondo JC, de Benito AM, Cuadrado G. Effects of lower-limb plyometric training on body composition, explosive strength, and kicking speed in female soccer players. J Strength Cond Res. 2009;23(6):1714–1722. doi: 10.1519/JSC.0b013e3181b3f537. [DOI] [PubMed] [Google Scholar]
- 42.Green SB, Salkind NJ. Using SPSS for the Windows and Macintosh: Analyzing and Understanding Data. 3rd ed. Upper Saddle River, NJ: Prentice Hall;; 2002. Two-way repeated-measures analysis of variance. In. [Google Scholar]
- 43.Mitchell A, Dyson R, Hale T, Abraham C. Biomechanics of ankle instability, part 2: postural sway-reaction time relationship. Med Sci Sports Exerc. 2008;40(8):1522–1528. doi: 10.1249/MSS.0b013e31817356d6. [DOI] [PubMed] [Google Scholar]
- 44.Knapp D, Lee SY, Chinn L, Saliba SA, Hertel J. Differential ability of selected postural-control measures in the prediction of chronic ankle instability status. J Athl Train. 2011;46(3):257–262. doi: 10.4085/1062-6050-46.3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wikstrom EA, Tillman MD, Chmielewski TL, Borsa PA. Measurement and evaluation of dynamic joint stability of the knee and ankle after injury. Sports Med. 2006;36(5):393–410. doi: 10.2165/00007256-200636050-00003. [DOI] [PubMed] [Google Scholar]
- 46.Santello M. Review of motor control mechanisms underlying impact absorption from falls. Gait Posture. 2005;21(1):85–94. doi: 10.1016/j.gaitpost.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 47.Gribble PA, Robinson RH. Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J Athl Train. 2009;44(4):350–355. doi: 10.4085/1062-6050-44.4.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Devita P, Skelly WA. Effect of landing stiffness on joint kinetics and energetics in the lower extremity. Med Sci Sports Exerc. 1992;24(1):108–115. [PubMed] [Google Scholar]
- 49.McNitt-Gray JL. Kinetics of the lower extremities during drop landings from three heights. J Biomech. 1993;26(9):1037–1046. doi: 10.1016/s0021-9290(05)80003-x. [DOI] [PubMed] [Google Scholar]
- 50.Delahunt E, Monaghan K, Caulfield B. Changes in lower limb kinematics, kinetics, and muscle activity in subjects with functional instability of the ankle joint during a single leg drop jump. J Orthop Res. 2006;24(10):1991–2000. doi: 10.1002/jor.20235. [DOI] [PubMed] [Google Scholar]
- 51.Self BP, Paine D. Ankle biomechanics during four landing techniques. Med Sci Sports Exerc. 2001;33(8):1338–1344. doi: 10.1097/00005768-200108000-00015. [DOI] [PubMed] [Google Scholar]
- 52.Decker MJ, Torry MR, Wyland DJ, Sterett WI. Richard Steadman J. Gender differences in lower extremity kinematics, kinetics and energy absorption during landing. Clin Biomech (Bristol, Avon) 2003;18(7):662–669. doi: 10.1016/s0268-0033(03)00090-1. [DOI] [PubMed] [Google Scholar]
- 53.Yamazaki J, Muneta T, Ju YJ, Sekiya I. Differences in kinematics of single leg squatting between anterior cruciate ligament-injured patients and healthy controls. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):56–63. doi: 10.1007/s00167-009-0892-z. [DOI] [PubMed] [Google Scholar]