Abstract
Context:
Identification of impaired balance as a risk factor for lower extremity injury regardless of injury history has led to subsequent investigation of variables that may adversely affect balance in healthy individuals.
Objectives:
To investigate the relationship among core and lower extremity muscle function, foot posture, and balance.
Design:
Descriptive laboratory study.
Setting:
Musculoskeletal injury biomechanics laboratory.
Patients or Other Participants:
A total of 108 individuals (40 men, 68 women; age = 22.8 ± 4.7 years, height = 168.5 ± 10.4 cm, mass = 69.9 ± 13.3 kg) participated in the study.
Main Outcome Measure(s):
Core endurance was assessed during 1 time-to-failure trial, and isometric hip and ankle strength were assessed using a handheld dynamometer and isokinetic dynamometer, respectively. Foot structure was quantified using the digital photographic measurement method. Single-limb–stance time to boundary was assessed using a force plate during an eyes-closed condition. Hierarchical multiple regression analyses were performed to predict balance using lower extremity strength, foot posture, and core endurance.
Results:
Foot posture (β = −0.22, P = .03) and ankle-inversion strength (β = −0.29, P = .006) predicted mediolateral balance. Increasing arch posture and ankle-inversion strength were associated with decreased mediolateral single-limb–stance balance.
Conclusions:
Increasing arch height was associated with decreased mediolateral control of single-limb stance. The relationship between time to boundary and injury risk, however, has not been explored. Therefore, the relationship between increasing arch height and injury due to postural instability cannot be determined from this study. If authors of future prospective studies identify a relationship between decreased time to boundary and increased injury risk, foot structure may be an important variable to assess during preparticipation physical examinations. The relationship between increasing ankle-inversion strength and decreased balance may require additional study to further elucidate the relationship between ankle strength and balance.
Key Words: foot structure, pronation, supination, balance, postural control
Key Points
Increasing arch posture and increasing ankle-inversion strength were associated with decreasing mediolateral postural stability during single-limb stance.
Prospective studies need to be conducted to determine if decreased mediolateral time to boundary is a risk factor for lower extremity injury.
The relationship between increasing ankle-inversion strength and decreasing balance needs to be studied further to determine the relationship between ankle strength and balance.
If authors of future prospective studies identify a relationship between decreased time to boundary and increased injury risk, clinicians may need to screen foot structure during preparticipation physical examinations.
The recognition of impaired postural stability as a risk factor for lower extremity injury regardless of injury history1,2 has led to subsequent investigation of variables that may adversely affect postural stability in apparently healthy individuals.3–6 The ultimate goal of the research has been to find variables that allied health professionals can use during injury-screening protocols (eg, preparticipation physical examinations) to identify individuals who may be at increased risk of future injury.
Researchers have reported (1) decreased postural stability in individuals with abnormal foot postures,4,6 (2) positive and negative correlations between core strength and postural stability,3 (3) positive correlations between body mass index (BMI) and body sway amplitude,3 and (4) BMI is a predictor of postural instability.5 Although foot posture, core strength, and BMI have been reported to influence postural stability, they primarily have been studied independently. A composite of anthropometric, strength, endurance, and structural variables, however, likely would more completely describe postural stability than any single measure. If this is the case, programs aimed at improving postural stability deficits need to identify and address the multiple factors that are modifiable. Furthermore, the clinical relevance of several previous studies also may be limited due to the methods used to classify foot posture and to quantify postural stability. To be clinically relevant, the method or methods used to classify foot posture must have moderate to high intratester and intertester reliability. The measures used in previous studies have moderate to high intratester reliability but low intertester reliability.7–10 For quantifying postural stability, measures that consider both the position of the center of pressure (COP) relative to the stability limits of an individual and the COP velocity may be better suited to identify postural instability than traditionally used measures, such as COP displacement.11,12
Other potentially important variables that have not been investigated include ankle and hip strength. Decreased ankle13 and hip14 strength both have been identified as risk factors for lower extremity injury, yet how the factors increase injury risk has not been identified. One potential mechanism is that decreased ankle and hip strength may result in postural instability. Specifically, weakness of the ankle and hip musculature may decrease the effectiveness of the ankle and hip strategies, respectively, used to control postural stability.15 Therefore, the purpose of our study was to investigate the relationship among core and lower extremity muscle function, foot posture, BMI, and postural stability using foot-posture measures with moderate to high intratester and intertester reliability and a postural-stability measure that considers both COP position and velocity. We hypothesized that a composite of anthropometric, strength, endurance, and foot-posture variables would be predictors of anteroposterior and mediolateral postural stability.
METHODS
Participants
We conducted 2 preliminary power analyses to determine the appropriate number of participants required to detect a moderate effect size with a power of 80% at an α level of .05. For the first power analysis, we assumed no multicollinearity would exist between predictor variables and included all 14 potential predictor variables. For the second power analysis, we assumed multicollinearity would exist between half the variables in the predictor groups that contained more than 1 predictor and included 8 predictor variables. Results of the 2 power analyses indicated that 135 or 109 participants, respectively, would be needed for the study. Therefore, we decided to recruit 110 participants who had no lower extremity injuries within the 6 months before the study and no history of lower extremity surgery. The data from 2 participants could not be used due to a foot touchdown during the balance trials; therefore, 108 participants (40 men, 68 women; age = 22.8 ± 4.7 years [range = 18–44 years], height = 168.5 ± 10.4 cm, mass = 69.9 ± 13.3 kg, BMI = 24.6 ± 4.4 kg/m2 [range = 18.6–47.8 kg/m2]) were included in the subsequent data analysis. Before testing, all participants provided written informed consent, and the Institutional Review Board of the University of Wisconsin–Milwaukee approved the study.
Postural Stability
Before postural-stability testing, we used a force plate to weigh the participants (model OR6-7-2000; Advanced Mechanical Technologies Inc, Watertown, MA or model FP4060NC; Bertec Corporation, Columbus, OH). Next, we assessed dominant-limb, single-limb–stance position postural stability on a force plate sampling at 100 Hz during three 10-second trials of the eyes-closed condition. The dominant limb was defined as the limb with which one would kick a ball. The eyes-closed condition was selected to increase the challenge to the somatosensory system and musculoskeletal components of the postural-control system.16 All participants wore the same style of sandals (model Hana; Maui and Sons, Pacific Palisades, CA), and we used a 90° angle (Framing Wizard; Swanson Tool Co, Inc, Frankfort, IL) to standardize foot position. The decision to test participants in sandals versus barefoot was based on 2 considerations. First, for the time-to-boundary (TTB) calculation, using sandals only required the dimensions of interest to be measured 1 time for each sandal size rather than for each participant. Second, we believed that testing in the shod condition might be more clinically relevant given that most activities of daily living and recreational and sporting activities are performed shod. During all trials, we instructed participants to place each hand on the contralateral shoulder and flex the knee of the nonweight-bearing limb to approximately 90°. When participants believed they were balanced with their eyes closed, they provided oral acknowledgment of readiness and attempted to remain motionless for the remainder of the trial. If they lost balance during a trial, participants were permitted to move their upper extremities and nonweight-bearing limb to regain balance. Participants were not permitted to step down with the nonweight-bearing limb or to touch the nonweight-bearing limb to the weight-bearing limb. If either occurred, the trial was repeated. We always performed postural-stability testing first to prevent potential fatigue effects associated with lower extremity and core strength testing. After postural stability, we tested core endurance, foot posture, and then lower extremity strength.
Core Endurance
Anterior, posterior, and lateral core muscular-endurance testing consisted of a single time-to-failure trial in each position as described by McGill et al.17 For lateral core strength, they did not report differences between the right and left sides, so we tested only the right side-lying position.17 We timed all trials using a digital hand-held stopwatch (model Triathlon; Timex Group USA, Middlebury, CT). A 5-minute rest period was provided between testing positions, and the order of testing was counterbalanced to control for fatigue effects.
Foot Posture
Dominant-limb arch index (AI) and navicular index (NI) ratios during 10% and 90% weight-bearing conditions were quantified using a digital photographic measurement method.18 The AI is the ratio of the height of the dorsum of the foot at 50% of the total foot length to the truncated foot length (the length from the first metatarsophalangeal joint to the most posterior aspect of the calcaneus).19 The NI is the ratio of the navicular tuberosity to the truncated foot length.19 The digital photographic measurement method quantifies foot posture using a digital still camera and a custom-written software program (MATLAB version 7.6.0; The MathWorks, Inc, Natick, MA). It computes foot posture with moderate to high intratester and intertester reliability and has moderate to high concurrent validity with traditional clinical measurement methods.18
Lower Extremity Strength
We assessed maximal isometric hip strength (flexion, extension, abduction, adduction, lateral rotation, medial rotation) using a handheld dynamometer (Lafayette Instrument Company, Lafayette, IN) and methods previously described.20 For each position, we used a nonelastic strap to secure the handheld dynamometer 5 cm proximal to the end of the distal joint segment. Participants performed 3 maximal isometric trials against the nonelastic strap in each testing position. We also used a sliding caliper (model GPM 101; Seritex Inc, Tinton Falls, NJ) to measure thigh (distance from the greater trochanter to the lateral femoral epicondyle) and leg (distance from the medial femoral epicondyle to the medial malleolus) lengths for subsequent muscle-torque computation. We chose handheld dynamometry because of the previously reported high reliability for measurement of hip strength21 and the greater availability of handheld than isokinetic dynamometers in clinical settings.
We used an isokinetic dynamometer (Biodex Medical Systems, Shirley, NY) to test maximal isometric ankle plantar flexion, dorsiflexion, inversion, and eversion torque using the method recommended by the manufacturer. We assessed ankle strength using isokinetic dynamometry versus handheld dynamometry because of the lack of reliability data to support using handheld dynamometry for measuring ankle strength and the potential for participants with strong plantar flexors to exceed the maximal load of the handheld dynamometer. Participants again performed 3 maximal isometric trials in each testing position. We selected the peak isometric hip and ankle strength trial for each muscle group for subsequent analysis.
Data Analysis
After data collection, we used a custom-written program (MATLAB version 7.6.0) to compute anteroposterior and mediolateral TTB using the mean and standard deviation (SD) of all TTB minimas22 during each trial. Time to boundary is the amount of time, which is calculated from the instantaneous position of the COP relative to the anteroposterior and mediolateral stability limits and the instantaneous COP velocity, needed for the COP of a participant to cross the anteroposterior and mediolateral stability limits if it continued in the current direction and at its current velocity. The mean TTB provides an estimate of the magnitude of time that individuals have to make postural corrections before their COPs cross their stability limits. A smaller mean TTB is associated with less time to make postural corrections and, therefore, less stability. The SD of the TTB provides information regarding the level of constraint on the sensorimotor system.12 Less TTB variability is associated with increased resistance to perturbations but less flexibility and adaptability when a change in postural state is needed.23 Conversely, increased TTB variability is associated with less resistance to perturbations but more flexibility and adaptability when a change in postural state is needed.23 Therefore, depending on the task being performed, decreased TTB variability may be associated with increased or decreased stability. During single-limb stance, decreased TTB variability has been hypothesized to be associated with musculoskeletal pathologic conditions and increased injury risk.11 If this is the case, then decreased variability during the eyes-closed, single-limb stance would be interpreted as an indicator of decreased stability.
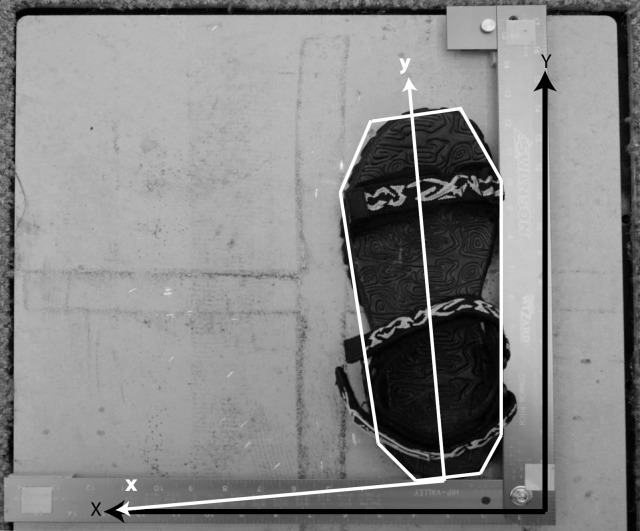
The custom-written MATLAB program was used to transform the ground reaction force data from the global force-plate reference system into a local sandal reference system, calculate COP position from the ground reaction force data, and compute TTB using multisegmented-polygon-defined stability limits (Figure).16 Specifically, medial and lateral boundaries were defined in the rearfoot, midfoot, and forefoot regions of the foot (Figure). Within each region, a line from the most distal (toward the toes) to the most proximal (toward the calcaneus) point of the region (Figure) was constructed using the equation yi − yp = m (xi − xp), where m is the slope of the line ([yd − yp]/[xd − xp]); yd and yp are the anterior and posterior coordinates of the most distal and proximal points of the region, respectively; and xd and xp are the medial and lateral coordinates of the most distal and proximal points of the region (Figure).16 To compute the TTB in the mediolateral direction, the known anteroposterior COP position at time i was input as the yi, and the mediolateral position (xi) at the known yi position was calculated. The calculated xi position was subtracted from the known horizontal COP position at time i to compute the TTB. The same procedures were used to compute anteroposterior TTB, except the given equation was solved for yi in lieu of xi, and the calculated yi position was subtracted from the known anteroposterior COP position at time i. We interpreted less TTB as decreased postural stability.
Figure.
For each sandal, the anteroposterior axis (y) of the local sandal coordinate system was the unit vector oriented from the midpoint of the rearfoot of the sandal to the midpoint of the forefoot of the sandal. The mediolateral axis (x) was defined as the cross product of the y axis of the local sandal coordinate system and the global vertical axis of the force-plate coordinate system (Z). The origin of the local sandal coordinate system was located at the posterior heel of each sandal. Multisegment polygon-stability limits were defined using the length of the sandal and the widths of the distal sandal, forefoot, rearfoot, and proximal sandal. The definition partitioned the sandal into toe (>74.5% of the total sandal length), forefoot (21.3%–74.5% of the total sandal length), and heel (<21.3% of the total sandal length) regions.
Hip strength, expressed as torque (Nm), was calculated by converting the peak force of the 3 trials assessed in kilograms to newtons and multiplying by the appropriate limb lengths (m). To obtain hip and ankle strength values independent of body size, we normalized the joint torques to body mass multiplied by height.20
Statistical Analysis
We used hierarchical multiple regression analyses to predict dominant-limb anteroposterior and mediolateral postural stability with lower extremity strength, foot posture, core endurance, and BMI. This technique allows blocks of variables to be entered in a predetermined order versus stepwise regression in which computer algorithm determines the entry order.24 Before performing hierarchical multiple regression analyses, we conducted preliminary analyses to investigate the assumptions of normality, linearity, homoscedasticity, and presence of multicollinearity. Normality, linearity, and homoscedasticity assumptions were confirmed via observation of both the normality probability plots of the regression standardized residual plots and the standardized residual versus the regression standardized predicted value scatterplots.24 We defined multicollinearity as a Pearson product moment correlation coefficient between 2 variables of equal to or greater than 0.7. We used SPSS (version 19; IBM Corporation, Armonk, NY) for statistical analyses. The α level for all analyses was established at .05.
RESULTS
Our preliminary analyses confirmed the assumptions for the hierarchical analyses were met. The Pearson product moment correlations revealed multicollinearity between the abduction and adduction (r = 0.74), abduction and flexion (r = 0.68), abduction and extension (r = 0.68), adduction and extension (r = 0.70), and adduction and flexion (r = 0.72) hip-strength measures; all of the foot-posture measures (AI 10% weight bearing and AI 90% weight bearing [r = 0.92], NI 10% weight bearing and NI 90% weight bearing [r = 0.88], AI 10% weight bearing and NI 10% weight bearing [r = 0.83], AI 90% and NI 90% [r = 0.82]); and anterior-lateral core strength (r = 0.70). For each multicollinear variable pair, we made a clinical decision to keep the variable that likely would have the greatest effect on balance performance and injury risk. For the foot-structure variables, we selected the NI 10% weight-bearing condition because we believed the 10% condition provided the most appropriate measure of foot structure. We believed the 90% weight-bearing ratio represented a composite of foot structure and flexibility. The means and SDs of the variables that subsequently were included in the hierarchical multiple regression analyses are presented in Table 1, and the order in which the variables were entered into the model are presented in Table 2.
Table 1. .
Hierarchical Regression Model Predictor Variables
| Predictor Variable |
Mean ± SD |
| Normalized ankle strength, Nm/kg·m | |
| Plantar flexion | 0.58 ± 0.16 |
| Dorsiflexion | 0.24 ± 0.06 |
| Inversion | 0.15 ± 0.05 |
| Eversion | 0.11 ± 0.03 |
| Foot posture | |
| Navicular index, 10% weight bearing | 0.28 ± 0.03 |
| Normalized hip strength, Nm/kg·m | |
| Abduction | 0.82 ± 0.20 |
| Medial rotation | 0.20 ± 0.06 |
| Lateral rotation | 0.18 ± 0.06 |
| Core endurance or endurances | |
| Lateral | 55.70 ± 31.38 |
| Posterior | 89.70 ± 51.27 |
| Body mass index, N/kg·m2 | 24.65 ± 4.40 |
Table 2. .
Hierarchical Regression Analysis Variables Entered to Predict Anteroposterior and Mediolateral Postural Stability
| Step |
Predictor Variable |
| 1: Ankle strength | Dorsiflexion |
| Plantar flexion | |
| Inversion | |
| Eversion | |
| 2: Foot posture | Navicular index, 10% weight bearing |
| 3: Hip strength | Abduction |
| Medial rotation | |
| Lateral rotation | |
| 4: Core endurance | Lateral |
| Posterior | |
| 5: Body mass index | Body mass index |
Anteroposterior Time to Boundary
When using the mean of all the TTB minima to represent postural stability (TTB mean = 2.64 ± 0.79 seconds), foot posture (β = −0.220, P = .03) predicted anteroposterior TTB variability after controlling for the effects of ankle strength. However, the model did not predict TTB (F5,102 = 1.92, P = .10; Table 3). When the SD of all the TTB minima was used to represent postural stability (TTB mean = 2.93 ± 1.25 seconds), none of the variables (P > .05) predicted anteroposterior TTB variability.
Table 3. .
Hierarchical Multiple Regression Analysis with Mean Anteroposterior Postural Stability as Criterion
| Step |
Predictor Variable |
R2 |
ΔR2 |
Standardized β |
| 1: Ankle strength | 0.042 | |||
| Dorsiflexion | −0.170 | |||
| Plantar flexion | 0.036 | |||
| Inversion | −0.042 | |||
| Eversion | −0.068 | |||
| 2: Foot posture | 0.086 | 0.044a | ||
| Navicular index, 10% weight bearing | −0.220a | |||
| 3: Hip strength | 0.091 | 0.005 | ||
| Abduction | 0.089 | |||
| Medial rotation | 0.013 | |||
| Lateral rotation | −0.026 | |||
| 4: Core endurance | 0.105 | 0.014 | ||
| Lateral | 0.082 | |||
| Posterior | 0.093 | |||
| 5: Body mass index | 0.108 | 0.003 | ||
| Body mass index | 0.058 |
Indicates P < .05.
Mediolateral Time to Boundary
When using the mean of all the TTB minima to represent postural stability (TTB mean = 0.97 ± 0.28 seconds), ankle-inversion strength (β = −0.291, P = .006) predicted mediolateral TTB variability, and the model predicted TTB (F4,103 = 2.79, P = .03; Table 4). In addition, foot posture (β = −0.216, P = .03) predicted mediolateral TTB variability after controlling for the effects of ankle strength, and the model continued to predict TTB (F5,102 = 3.32, P = .008; Table 4). The negative standardized coefficients for ankle-inversion strength and foot posture suggest that increases in inversion strength and larger NI 10% weight-bearing ratios (higher-arch foot posture) were associated with decreased mediolateral TTB (less mediolateral stability) and vice versa for decreasing inversion strength and NI 10% weight-bearing ratios (low-arch foot posture). When the SD of all the TTB minima was used to represent postural stability (TTB mean = 1.27 ± 0.51 seconds), none of the variables (P < .05) predicted mediolateral TTB variability.
Table 4. .
Hierarchical Multiple Regression Analysis with Mean Mediolateral Postural Stability as Criterion
| Step |
Predictor Variable |
R2 |
ΔR2 |
Standardized β |
| 1: Ankle strength | 0.098a | |||
| Dorsiflexion | −0.065 | |||
| Plantar flexion | −0.035 | |||
| Inversion | −0.291a | |||
| Eversion | 0.054 | |||
| 2: Foot posture | 0.140a | 0.042a | ||
| Navicular index, 10% weight bearing | −0.216a | |||
| 3: Hip strength | 0.160 | 0.02 | ||
| Abduction | −0.027 | |||
| Medial rotation | 0.179 | |||
| Lateral rotation | −0.039 | |||
| 4: Core endurance | 0.169 | 0.008 | ||
| Lateral | −0.037 | |||
| Posterior | 0.111 | |||
| 5: Body mass index | 0.173 | 0.005 | ||
| Body mass index | −0.079 |
Indicates P < .05.
DISCUSSION
We investigated the ability of foot posture, core and lower extremity muscle function, and BMI to predict postural stability. We hypothesized that a composite of anthropometric, strength, endurance, and foot-posture variables would predict anteroposterior and mediolateral postural stability. When the mean of all the TTB minima was used to quantify balance, our hypothesis was supported by the ability of the NI during 10% weight bearing to predict anteroposterior postural stability and the ability of both ankle-inversion strength and NI during 10% weight bearing to predict mediolateral postural stability. The fact that none of the variables predicted anteroposterior or mediolateral postural stability when the SD of all the TTB minima was used to quantify balance did not support our hypothesis. The ability of the aforementioned variables to predict mean mediolateral TTB but not the variability of TTB may suggest that the variables affect the time an individual has to make postural corrections but not the flexibility and adaptability of the postural-control system.25
Foot Posture
Foot posture was a predictor variable accounting for 4.4% and 4.2% of anteroposterior and mediolateral postural stability variance, respectively. However, given that the anteroposterior model did not predict postural stability, we discuss only the results of the mediolateral model. As stated, the negative correlation coefficients suggest that increased arch height (a larger NI/10% weight-bearing ratio) is associated with decreased mediolateral postural stability (lower TTB score). The relationship between a high-arched foot posture and postural instability in our study is in partial agreement with the findings of Hertel et al,6 who reported greater mean COP excursion area (decreased postural stability) in participants with high-arch than pes rectus foot postures during eyes-open single-limb–stance position testing. However, no difference in postural stability between foot-posture groups was revealed when mean COP velocity was used to quantify postural stability. The negative correlation coefficient suggesting a relationship between low-arch posture and improved postural stability does not agree with the findings of Cobb et al.4 Those authors reported decreased anteroposterior postural stability (root mean square COP velocity) during eyes-open and eyes-closed single-limb–stance condition testing in participants with low-arch structures.4 Whereas our results are in partial agreement with those in the previous literature, different methods used to determine foot posture and to quantify postural stability make direct comparisons between the studies difficult. The different methods used to determine foot posture may not have measured the same foot-posture characteristics. Furthermore, both Hertel et al6 and Cobb et al4 determined foot-posture groups using methods with moderate to high intratester reliability but low intertester reliability,7,8 which, as stated, may limit the clinical relevance of the studies. For quantifying postural stability, Hertel et al6 used mean COP excursion area and mean COP velocity; Cobb et al4 defined postural stability using the root mean square COP velocity; and we used TTB. The different methods may capture different aspects of postural stability,11 and of the measures used, only TTB considers both the position of the COP relative to the stability limits and the COP velocity. A final consideration in comparing the study results is the statistical designs of the studies. We reported a relationship between high-arch foot posture and postural instability; we did not compare differences between foot-posture groups, as did the authors of the previous studies.
The cause of the relationship between high-arch posture and mediolateral postural instability may be an anterior and lateral shift in COP and decreased foot mobility often associated with high-arch postures. Decreased mobility may limit the medial displacement of the COP during weight bearing, resulting in more frequent and rapid laterally directed COP movement of the already anteriorly and laterally positioned COP. Conversely, the relationship between a lower-arch posture and improved mediolateral postural stability may be associated with a more centralized COP position. A more centrally located COP position may provide increased distance to the mediolateral stability limits even if COP velocity is greater due to increased foot mobility, as suggested by Cobb et al.4 In the case of a rigid flat foot, the increased contact area associated with the lowered arch and increased forefoot splay also may provide a more stable base of support.
Core Endurance and Lower Extremity Strength
Our hypothesis that core endurance and hip strength would predict postural stability was not supported. In a prospective study investigating the relationship between core-stability measures and lower extremity injury risk, Leetun et al14 reported decreased hip strength was a predictor of lower extremity injury risk. Specifically, injured athletes had less hip-abductor and hip lateral-rotator strength than uninjured athletes and decreased hip lateral-rotator strength was a predictor of injury risk. Anterior, posterior, and lateral core endurance, however, was not different between injured and uninjured athletes and did not predict injury risk. The finding that hip lateral-rotation strength did not predict postural stability in our study suggests that injury risk associated with decreased hip lateral-rotation strength may not be due to decreased postural stability. Furthermore, our results do not support the general clinical belief that increased core endurance is associated with increased balance. However, before discounting the role of the core in balance, the relationship of core strength rather than endurance requires further investigation. Similarly, further study of the relationship between hip muscular endurance or eccentric strength and postural stability also is warranted before conclusions regarding the influence of hip muscle function on balance can be determined.
Finally, our hypothesis that ankle strength would be a predictor of postural stability was partially supported, with ankle strength accounting for 9.8% of the mediolateral postural-stability variance. Our results that revealed ankle-inversion strength predicted mediolateral postural stability are inconsistent with those of Lin et al,26 who did not find a correlation between ankle eversion-to-inversion isokinetic strength ratio and single-limb–stance postural stability. However, differences in the variables used to compute ankle strength and postural stability (COP excursion, mean COP speed, and area of the 95% confidence ellipse) make direct comparison between the studies difficult. Whereas it is difficult to theorize how increased ankle-inversion strength would be associated with decreased postural stability, the results of a prospective study in which Baumhauer et al13 investigated the relationship between ankle strength and ankle injury risk may provide a plausible explanation. Specifically, they identified ankle-strength imbalance as a risk factor for ankle injury. Therefore, the relationship between increased strength of the invertors and decreased postural stability may be the result of an imbalance between the strength of the invertors and the surrounding ankle musculature rather than a deleterious effect associated with stronger invertor musculature. In addition, further research into the relationship between ankle muscular endurance or eccentric strength and postural stability is warranted before conclusions regarding the influence of ankle muscle function on balance can be determined.
Body Mass Index
The inability of BMI to account for a large amount of postural-stability variance is inconsistent with the findings of Hue et al,5 who investigated the contribution of body weight to the prediction of balance. In addition to the use of different measures to quantify postural stability, inconsistency between the studies may be related to the age and BMI of the study participants. Their participants were older (mean age = 40.5 ± 9.5 years, range = 24–61 years) and had greater BMIs (mean = 35.2 ± 11.7 kg/m2, range = 17.4–63.8 kg/m2) than our participants (mean age = 22.8 ± 4.7 years, range 18–44 years; mean BMI = 24.6 ± 4.4 kg/m2, range = 18.6–47.8 kg/m2).5 Body mass index is possibly a greater predictor of postural stability in older and severely obese individuals.
Limitations
Before drawing conclusions about our results, we should consider several limitations. First, all foot-posture measures included in the study design were structural measures. We did not measure foot mobility. To maximize the clinical relevance of the results, we included only foot-posture measures with moderate to high intratester and intertester reliability in the study design; however, none of the available mobility measures met both criteria.18 Continued development and evaluation of mobility measures with moderate to high intratester and intertester reliability may be important, as rigid high-arch and mobile high-arch foot postures or mobile low-arch and rigid low-arch foot postures may function differently. Second, although a relationship between increasing arch posture and postural instability does exist, a threshold of postural instability at which injury risk is increased has not been identified. Therefore, the potential injury risk associated with increasing arch posture due to postural instability cannot be determined. Third, the NI during 10% weight bearing and ankle strength were predictors of mediolateral postural stability, accounting for 14% of the total mediolateral postural stability variance, but 86% of the variance remained unexplained.
Another important consideration is the fact that these data were collected on healthy individuals. Therefore, the results are not generalizable to injured populations. Similar studies in which researchers investigate the relationship among foot posture, core muscle and lower extremity function, and postural stability in injured populations, such as patients with chronic ankle instability, are warranted.
CONCLUSIONS
Increasing arch posture quantified as the NI during 10% weight bearing and increasing ankle-inversion strength were associated with decreased mediolateral postural stability during single-limb stance. Before we can draw conclusions about the relationship between foot posture and injury risk, prospective studies need to be conducted to determine if decreased mediolateral TTB is a risk factor for lower extremity injury. If researchers confirm this relationship in future prospective studies, it may be important for allied health professionals to include foot-posture assessment as a component of injury-screening procedures, such as preparticipation physical examinations.
The relationship between foot posture and postural stability also suggests that, to avoid including participants with decreased postural stability in reference groups, researchers should consider foot posture as an inclusionary criterion for control or uninjured groups in future postural-stability studies. The relationship between increased ankle-inversion strength and decreased postural stability is more difficult to interpret. Additional research into the relationship between ankle strength and balance is warranted.
ACKNOWLEDGMENTS
We thank Dr Susan E. Cashin for her assistance with the statistics.
REFERENCES
- 1.Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc. 1984;16(1):64–66. [PubMed] [Google Scholar]
- 2.McGuine TA, Greene JJ, Best T, Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10(4):239–244. doi: 10.1097/00042752-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Angyán L, Téczely T, Angyán Z. Factors affecting postural stability of healthy young adults. Acta Physiol Hung. 2007;94(4):289–299. doi: 10.1556/APhysiol.94.2007.4.1. [DOI] [PubMed] [Google Scholar]
- 4.Cobb SC, Tis LL, Johnson BF, Higbie EJ. The effect of forefoot varus on postural stability. J Orthop Sports Phys Ther. 2004;34(2):79–85. doi: 10.2519/jospt.2004.34.2.79. [DOI] [PubMed] [Google Scholar]
- 5.Hue O, Simoneau M, Marcotte J, et al. Body weight is a strong predictor of postural stability. Gait Posture. 2007;26(1):32–38. doi: 10.1016/j.gaitpost.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Hertel J, Gay MR, Denegar CR. Differences in postural control during single-leg stance among healthy individuals with different foot types. J Athl Train. 2002;37(2):129–132. [PMC free article] [PubMed] [Google Scholar]
- 7.Elveru RA, Rothstein JM, Lamb RL. Goniometric reliability in a clinical setting: subtalar and ankle joint measurements. Phys Ther. 1988;68(5):672–677. doi: 10.1093/ptj/68.5.672. [DOI] [PubMed] [Google Scholar]
- 8.Evans AM, Copper AW, Scharfbillig RW, Scutter SD, Williams MT. Reliability of the foot posture index and traditional measures of foot position. J Am Podiatr Med Assoc. 2003;93(3):203–213. doi: 10.7547/87507315-93-3-203. [DOI] [PubMed] [Google Scholar]
- 9.Smith-Oricchio K, Harris BA. Interrater reliability of subtalar neutral, calcaneal inversion, and eversion. J Orthop Sports Phys Ther. 1990;12(1):10–15. doi: 10.2519/jospt.1990.12.1.10. [DOI] [PubMed] [Google Scholar]
- 10.Vinicombe A, Raspovic A, Menz HB. Reliability of navicular displacement measurement as a clinical indicator of foot posture. J Am Podiatr Med Assoc. 2001;91(5):262–268. doi: 10.7547/87507315-91-5-262. [DOI] [PubMed] [Google Scholar]
- 11.Hertel J, Olmsted-Kramer LC. Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture. 2007;25(1):33–39. doi: 10.1016/j.gaitpost.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 12.Van Emmerik RE, Van Wegan EE. On variability and stability in human movement. J Appl Biomech. 2000;16(4):394–406. [Google Scholar]
- 13.Baumhauer JF, Alosa DM, Renström AF, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23(5):564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- 14.Leetun DT, Ireland ML, Willson JD, Ballantyne BT, Davis IM. Core stability measures as risk factors for lower-extremity injury in athletes. Med Sci Sports Exerc. 2004;36(6):926–934. doi: 10.1249/01.mss.0000128145.75199.c3. [DOI] [PubMed] [Google Scholar]
- 15.Winter DA. Human balance and posture control during standing and walking. Gait Posture. 1995;3(4):193–214. [Google Scholar]
- 16.Cobb SC, Joshi MN, Bazett-Jones DM, Earl-Boehm JE. The effect of boundary shape and minima selection on single limb stance postural stability. J Appl Biomech. 2012;28(5):608–615. doi: 10.1123/jab.28.5.608. [DOI] [PubMed] [Google Scholar]
- 17.McGill SM, Childs A, Liebenson C. Endurance times for low back stabilization exercises: clinical targets for testing and training from a normal database. Arch Phys Med Rehabil. 1999;80(8):941–944. doi: 10.1016/s0003-9993(99)90087-4. [DOI] [PubMed] [Google Scholar]
- 18.Cobb SC, James CR, Hjertstedt M, Kruk J. A digital photographic measurement method for quantifying foot posture: validity, reliability, and descriptive data. J Athl Train. 2011;46(1):20–30. doi: 10.4085/1062-6050-46.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams DS, McClay IS. Measurements used to characterize the foot and the medial longitudinal arch: reliability and validity. Phys Ther. 2000;80(9):864–871. [PubMed] [Google Scholar]
- 20.Bazett-Jones DM, Cobb SC, Joshi MN, Cashin SE, Earl JE. Normalizing hip muscle strength: establishing body-size-independent measurements. Arch Phys Med Rehabil. 2011;92(1):76–82. doi: 10.1016/j.apmr.2010.08.020. [DOI] [PubMed] [Google Scholar]
- 21.Jaramillo J, Worrell TW, Ingersoll CD. Hip isometric strength following knee surgery. J Orthop Sports Phys Ther. 1994;20(3):160–165. doi: 10.2519/jospt.1994.20.3.160. [DOI] [PubMed] [Google Scholar]
- 22.Hertel J, Olmsted-Kramer LC, Challis JH. Time-to-boundary measures of postural control during single leg quiet standing. J Appl Biomech. 2006;22(1):67–73. doi: 10.1123/jab.22.1.67. [DOI] [PubMed] [Google Scholar]
- 23.Van Emmerik RE, Van Wegan EE. On the functional aspects of variability in postural control. Exerc Sport Sci Rev. 2002;30(4):177–183. doi: 10.1097/00003677-200210000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Pallant J. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using SPSS for Windows. 3rd ed. New York, NY: The McGraw-Hill Companies;; 2007. [Google Scholar]
- 25.Van Wegen EE, Van Emmerik RE, Riccio GE. Postural orientation: age-related changes in variability and time-to-boundary. Hum Mov Sci. 2002;21(1):61–84. doi: 10.1016/s0167-9457(02)00077-5. [DOI] [PubMed] [Google Scholar]
- 26.Lin WH, Liu YF, Hsieh CC, Lee AJ. Ankle eversion to inversion strength ratio and static balance control in the dominant and non-dominant limbs of young adults. J Sci Med Sport. 2009;12(1):42–49. doi: 10.1016/j.jsams.2007.10.001. [DOI] [PubMed] [Google Scholar]