Abstract
Context:
The release of evidence-based practice (EBP) Web-based learning modules to the membership of the National Athletic Trainers' Association has provided athletic trainers (ATs) the opportunity to enhance their knowledge of the various EBP concepts. Whereas increasing the knowledge of EBP among ATs is important, assessing whether this newfound knowledge is being translated into clinical practice and didactic education is crucial.
Objective:
To explore the effectiveness of an educational intervention regarding EBP on the didactic instruction patterns of athletic training educators and the clinical practice behaviors of clinicians.
Design:
Qualitative study.
Setting:
Individual telephone interviews.
Patients or Other Participants:
A total of 25 ATs (12 educators, 13 clinicians; experience as an AT = 16.00 ± 9.41 years) were interviewed.
Data Collection and Analysis:
We conducted 1 individual telephone interview with each participant. After transcription, the data were analyzed and coded into common themes and categories. Triangulation of the data occurred via the use of multiple researchers and member checking to confirm the accuracy of the data.
Results:
Participants perceived the EBP Web-based modules to produce numerous outcomes regarding education and clinical practice. These outcomes included perceived knowledge gain among participants, an increase in the importance and scope of EBP, a positive effect on educators' didactic instruction patterns and on instilling value and practice of EBP among students, and an enhanced ability among clinicians to implement EBP within clinical practice. However, some clinicians reported the Web-based modules had no current effect on clinical practice.
Conclusions:
Although the EBP Web-based modules were successful at enhancing knowledge among ATs, translation of knowledge into the classroom and clinical practice remains limited. Researchers should aim to identify effective strategies to help ATs implement EBP concepts into didactic education and clinical practice.
Key Words: knowledge translation, evidence-based medicine, qualitative research
Key Points
Participants perceived that the Web-based modules enhanced their knowledge and the importance of evidence-based practice (EBP).
Educators indicated a positive effect on didactic instruction patterns and on instilling the value and practice of EBP among students.
Some clinicians perceived an enhanced ability to implement EBP within clinical practice, but other clinicians reported the Web-based modules did not affect their clinical practices.
A cultural shift from the current model of athletic training practice to EBP will require dedication from every facet of the profession.
Researchers should continue to identify successful strategies to aid athletic trainers in effectively implementing EBP into education and clinical practice.
Over the past 5 years, research has expanded regarding evidence-based practice (EBP) within athletic training. In the current literature, researchers have indicated that although athletic trainers (ATs) believe EBP is important for the profession,1–5 their knowledge of the concepts involved in the process is limited.2–7 Numerous barriers preventing ATs from implementing EBP into education and clinical practice also have been identified.3,6–8 Time,3,6–8 access to resources,6–8 and knowledge3,6,8 have been the most common barriers reported. To diminish the knowledge barrier, a series of Web-based educational modules focusing on the foundational concepts of EBP was developed and made available to all National Athletic Trainers' Association (NATA) members. Welch et al9 conducted a randomized controlled trial to assess the effectiveness of these Web-based modules for enhancing knowledge among a random sample of 164 athletic training clinicians, educators, clinical preceptors, graduate students, and professional athletic training students. The modules were found to increase knowledge of the concepts involved in EBP among ATs.9
Whereas assessing attitudes and beliefs regarding EBP within the profession and knowledge gains after an educational intervention is important, determining whether ATs use this newfound knowledge to validate their didactic curricula or clinical practice also is critical. More specifically, identifying which strategies effectively induce ATs to implement EBP within daily practice is important. This involves identifying which variables influence knowledge translation and which steps ATs can take to overcome the perceived barriers preventing them from making essential changes.10 Although it is unclear whether EBP educational interventions effectively influence athletic training clinical practice, literature supports the use of educational interventions on various topics to increase knowledge and promote clinical practice changes among other health care professionals.11–14
However, whereas these interventions typically were shown to increase knowledge, the authors have reported mixed results in actually altering clinical practice. Cameron and Naylor11 used active dissemination of a clinical prediction rule, the Ottawa Ankle Rules, to reduce the number of unnecessary radiographs that physicians were ordering. Physicians reported they were confident that evidence supported the Ottawa Ankle Rules and they believed they had received enough training for implementation. However, their results indicated that the number of patients referred for ankle radiographs did not decline.11 Kennedy et al13 administered an educational intervention to family medicine residents and then qualitatively observed clinical practice behavior after the intervention. Although the intervention increased knowledge, levels of certainty and a sense of urgency among participants to make clinical decisions affected whether they incorporated the knowledge gained from the educational intervention.13
Educational interventions are a necessary component to increase knowledge within an area, but researchers must determine whether the increase in knowledge of EBP concepts after the implementation of the Web-based modules actually has translated to the incorporation of EBP into athletic training education and clinical practice. Whereas quantitative measures provide useful information when assessing changes in knowledge after the Web-based modules,9 a qualitative inquiry provides a more in-depth understanding of the experiences and perspectives ATs have and may give a richer picture of any practice changes after the educational intervention. Therefore, the purpose of our study was to explore the effectiveness of these EBP educational modules on didactic instruction patterns of educators and clinical practice of clinicians. Specifically, we aimed to assess the perceptions among educators and clinicians of whether the implementation of the EBP Web-based modules initiated immediate changes within the classroom or clinical practice setting.
METHODS
Design
The emergent study design of this investigation was modeled after the consensual qualitative research (CQR) approach. Derived from the integration of grounded theory,15 phenomenology,16 and comprehensive process analysis,17 CQR provides an in-depth descriptive analysis and theoretical framework of participants' experiences and the circumstances that promote these experiences.18 Furthermore, CQR focuses on the use of multiple researchers, the process of reaching a consensus, and a methodologic approach to constantly and repetitively analyze multiple cases to reach a comprehensive representation of the results.18 We selected the CQR approach for this qualitative inquiry to explore the experiences and theories ATs had about an educational intervention (ie, 10 EBP Web-based learning modules) that was implemented to enhance EBP within clinical practice and didactic education. The study was designed to be an inductive interpretation of what these individuals believed to be important concepts, principles, or ideas of EBP as they related to didactic education and clinical practice, as well as how these beliefs and practices were influenced by the educational intervention.
Given the consensual process of CQR, multiple researchers are essential to the construction of a solid research team. As complex issues arise within qualitative data, multiple perspectives, opinions, and levels of awareness are needed to increase the approximation of truth and simultaneously diminish researcher bias.18 The research team for this study consisted of 5 ATs: 3 researchers (C.E.W., A.L.W., J.M.M.) composed the research team, 1 held a dual role as a research team member and the internal auditor (D.A.H.), and 1 acted as the external auditor (not an author). Auditors often participate within CQR to verify the interpretations made by the research team and to provide continual appraisal during each stage of data analysis.18 They must ensure the data were closely and appropriately analyzed and multiple perspectives were considered and discussed before consensus was reached.18 For this study, the internal auditor provided detailed feedback throughout all stages of data analysis, whereas the external auditor offered additional feedback after cross-analysis. The roles and experience of each research team member for this investigation are displayed in Table 1.
Table 1. .
Roles and Experiences of the Research Team
| Researcher |
|||||
| 1 |
2 |
3 |
4 |
5 |
|
| Study role | Primary researcher and research team member | Research team member | Research team member | Research team member and internal auditor | External auditor |
| Qualitative experience | Experienced qualitative researcher with a background in consensual qualitative research | Novice qualitative researcher new to the consensual qualitative research approach | Experienced qualitative researcher with previous experience in consensual qualitative research | Experienced qualitative researcher with experience in various approaches and moderately familiar with the consensual qualitative research approach | Experienced qualitative researcher with experience in various approaches and moderately familiar with the consensual qualitative research approach |
| Evidence-based practice experience | Research experience on the topic of evidence-based practice | Moderately familiar with the concepts of evidence-based practice | Moderately familiar with the concepts of evidence-based practice | Research experience on the topic of evidence-based practice | Research experience on the topic of evidence-based practice |
Participants
Athletic trainers who were participants in the experimental group of a previous research investigation9 involving the implementation of 10 EBP Web-based learning modules (N = 164) were considered to be potential participants for this study. To recruit participants, we used stratified purposeful sampling and criterion-based sampling methods. Stratified purposeful sampling often is considered a sample within samples and allows the researchers to capture major variations that may occur across a population.19 To provide ample representativeness of the athletic training population, an equal number of clinicians and educators were invited to participate in this study. Criterion-based sampling allowed the researchers to select individuals based on a predetermined set of criteria, thereby providing meaningful results that can be more applicable to the population.18,20 To be considered a viable candidate in this study, each AT had to have been a participant within the experimental group of a previous study9 and had to have accessed all 10 Web-based learning modules, as determined via the Web-based module usage data sheet provided by the NATA office.
Given the exploratory nature of CQR, Hill et al18 suggested obtaining approximately 10 to 15 participants to attempt to achieve saturation. The interview protocol for this study consisted of 2 branches (ie, clinician branch, educator branch), so the research team aimed to include a total of 20 to 30 participants. Of the 164 ATs who accessed the Web-based modules in the previous investigation, 75 did not meet the predetermined criteria for this inquiry, reducing the potential sample group to 89 individuals. Twenty-five ATs (14 women, 11 men) responded to the request to participate in this investigation and completed the qualitative interview before the research team determined that saturation of both branches had been reached. Twelve participants were athletic training educators, and the other 13 individuals were athletic training clinicians. On average, the participants had 16.00 ± 9.41 years of athletic training experience. All ATs were given last-name pseudonyms to maintain participant anonymity (Table 2). All participants provided consent via e-mail before data collection and orally at the beginning of each individual interview, and the study was approved by the Old Dominion University Human Subjects Committee for Exempt Research.
Table 2. .
Participant Demographics
| Participant Pseudonym |
Sex |
Experience as Athletic Trainer, y |
Primary Athletic Training Role |
Clinical Practice Setting |
| Dr Birch | Male | 5.5 | Educator | Not applicable |
| Boyce | Female | 22 | Clinician | Clinic |
| Carpenter | Male | 29 | Educator | Not applicable |
| Dr Cavins | Female | 18 | Educator | Not applicable |
| Decker | Male | 10 | Clinician | College or university |
| DiLorenzo | Female | 17 | Educator | Not applicable |
| Dr Dominique | Female | 6 | Educator | Not applicable |
| Eckert | Female | 4.5 | Clinician | College or university |
| Farrar | Male | 37 | Clinician | High school |
| Dr Fosgate | Female | 17 | Educator | Not applicable |
| Dr Gangler | Female | 14 | Educator | Not applicable |
| Dr Harvey | Female | 30 | Educator | Not applicable |
| Homier | Male | 9.5 | Clinician | College or university |
| Lavoy | Female | 14 | Educator | Not applicable |
| MacIntosh | Male | 5 | Educator | Not applicable |
| Dr McDaniel | Male | 33 | Educator | Not applicable |
| Meier | Male | 15 | Educator | Not applicable |
| Moran | Female | 6 | Clinician | College or university |
| Parker | Male | 15 | Clinician | College or university |
| Pessefall | Female | 6 | Clinician | College or university |
| Rose | Male | 25 | Clinician | High school |
| Schaffer | Female | 16 | Clinician | High school |
| Schlade | Female | 18 | Clinician | College or university |
| Varner | Female | 10.5 | Clinician | High school |
| Wilson | Male | 17 | Clinician | High school |
Instrumentation
One of the essential components of CQR is using open-ended questions (ie, interviews, questionnaires) and a semistructured approach.18 Given the lack of a preexisting interview protocol that specifically addressed the research aims of this investigation, the research team developed a unique semistructured interview protocol consisting of 12 open-ended questions along with potential probe questions to be used when necessary. The primary researcher (C.E.W.) constructed the initial interview questions using the research aims of the study and available previous literature1,3,6–9,11–13,18 as guidelines for question development. To capture appropriate responses from both educators and clinicians, 2 interview branches were developed. The educator branch tailored the 12 questions to didactic education, and the clinician branch tailored the questions to clinical practice. Two members of the research team (C.E.W., D.A.H.) reviewed the initial interview protocols, and changes (eg, grammar, structure, question order) were made accordingly. Questions from the interview protocol are presented in Table 3. After review, 2 pilot interviews were conducted with ATs who had accessed the EBP Web-based modules but did not meet the predetermined inclusion criteria for this investigation. Each pilot interview helped us revise the wording of questions to ensure clarity and provided the research team with insight on the type of data that likely would be obtained during data collection.
Table 3. .
Interview Protocol Questions With Probes
| 1. Tell me about your background as an athletic trainer/athletic training educator. |
| 2. Please discuss what EBP means to you. |
| a. What role do you feel research plays in EBP process? |
| b. What role do you feel the clinician plays in the EBP process? |
| c. What role do you feel the patient plays in the EBP process? |
| d. What perceptions do you have of the EBP process? |
| 3. Why did you become interested in going through the online modules? |
| a. What expectations did you have for the online modules? |
| b. Did you have any previous EBP training prior to completing the online modules? |
| 4. What were your perceptions of the online modules after completing them? |
| 5. In what ways, if any, do you feel the online modules can be improved? |
| 6. Did the online modules change your perceptions of EBP in any way? |
| 7. Please discuss any barriers you encountered while completing the online modules. |
| 8. Do you feel these online modules had a positive or negative impact, if any, on your daily teaching style in the classroom/clinical practice? Please explain. |
| 9. What concepts, if any, did you take from the online modules and begin to implement within your didactic curriculum/clinical practice? |
| a. Are there concepts you feel like you need more information on before you can implement? |
| b. Are there any barriers preventing you from implementing these concepts? |
| 10. What strategies do you feel will be useful to educate educators/clinicians on implementing EBP within didactic curricula/clinical practice? |
| 11. Is there anything else you would like to add about EBP, athletic trainer education or clinical practice, or your own personal experience? |
| 12. Are there any questions or topics I have not asked about that you would like to discuss? |
Abbreviation: EBP, evidence-based practice.
Procedures
The primary researcher contacted the potential participants via e-mail after individuals who met the predetermined criteria were identified and the sample was stratified. The e-mail included the purpose of the investigation, contact information, and a request for his or her voluntary participation. Given the anticipated locations of the ATs participating in this research, the primary mode of data collection was via telephone. After a candidate agreed to participate, an individual 30- to 40-minute interview was scheduled via telephone, and the participant completed a brief demographic questionnaire via e-mail. Based on the semistructured interview protocol designed for this study, the primary researcher placed ATs into 1 of the 2 interview protocol branches. Data collection for this investigation began 6 months after the participants accessed the Web-based modules in the previous study (November 2011) and continued until data saturation was met in each interview branch (December 2011).
After an individual interview was completed, a transcriptionist transcribed the audio file. Proper names, places, and any other identifying information were masked within each transcript to protect the anonymity of participants.18 We sent participants the transcripts of their interviews to enhance trustworthiness. Member checks allowed participants to provide any additions or clarifications to the transcript.21 However, we clearly instructed participants that the information already presented within the transcripts could not be deleted or altered in any way. Of the 25 participants in this study, 2 individuals provided further insight into their individual transcript responses, and the additional information was included during the coding phase of data analysis.
Data Analysis and Management
Data analysis for the CQR approach was an intricate process involving 4 progressive stages: (1) ascertaining initial code domains, (2) extracting core ideas from each domain, (3) cross-analyzing multiple participant interviews via development of categories and themes, and (4) identifying the frequency of participant cases per category. Initial code domains were used to group data around similar topics.18 After the domains were identified, the 4 research team members coded the initial transcripts and placed the data in a domain as they saw fit. Coding multiple transcripts at this stage allowed the researchers to gain a clearer sense of the content that would represent each domain.18 When the data had been placed in domains, the next stage of data analysis involved constructing core ideas from each domain. This process often is called abstracting15 and essentially involved more concisely summarizing what the participant said in each domain to develop a codebook.18 Finally, we cross-analyzed multiple participant interviews. During this phase, the researchers looked for relationships, similarities, and differences that emerged from the interviews when they were examined together. Cross-analysis enabled the researchers to distinguish categories in which the core ideas could be placed.18 These categories emerged from the data provided and were not established from the literature or preconceived ideas.18,22 Additionally, categories often were modified as the researchers became more familiar with the data. When cross-analysis was completed, we also needed to characterize the frequency of occurrence for all categories. More specifically, frequency counting enabled the research team to determine how often each category was applied across the whole sample, providing a sense of the representativeness of the entire sample.18 Frequency of the categories was divided into 4 components: (1) general, (2) typical, (3) variant, or (4) rare. For this investigation, a category was considered general if it applied to all or all but one case, typical if it applied to more than half of the cases, variant if it applied to less than half of the cases, or rare if the data related to only 2 to 3 cases.18
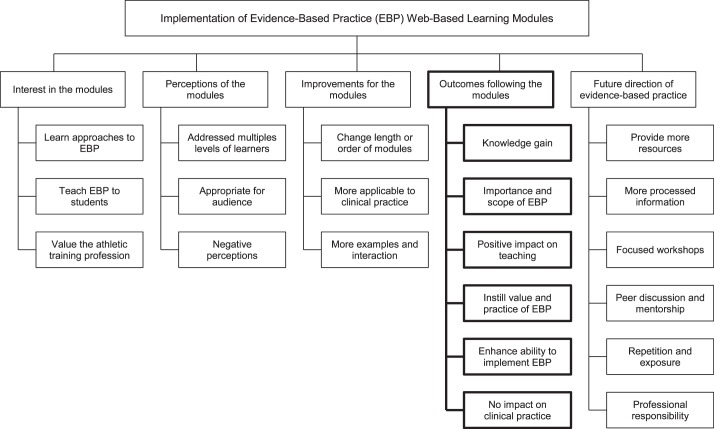
Before the start of data collection for this study, research team members and auditors were trained on the CQR data-analysis process. Training suggestions from Hill et al18 were applied to ensure all members had the same understanding of how the process would occur throughout the investigation. The primary researcher (C.E.W.) conducted additional training sessions with the novice qualitative researcher (A.L.W.). Inclusion of the novice researcher was deemed advantageous to data analysis; she could provide a fresh perspective and interpretation of the results because her biases at that point were limited. Involvement of the research team and auditors varied throughout the data-analysis process (Figure 1).
Figure 1. .
Research team involvement during consensual qualitative research data analysis.
To enhance the trustworthiness of the results from this qualitative study, we implemented several strategies. The CQR approach inherently guaranteed that triangulation and peer debriefing occurred. By including multiple researchers in the data analysis of this investigation, we were able to continually triangulate the data (ie, multiple-analyst triangulation) and diminish researcher bias by ensuring that at least 2 researchers were involved in each phase of analysis. Additionally, the inclusion of 2 auditors enhanced the realm of additional perspectives to ensure that multiple avenues had been considered.18 Another strategy used within the investigation to ensure trustworthiness was member checks.19 We used member checking to ensure coherence between the intended purpose and the methods of the study. This strategy was used in various forms throughout the data-collection process. First, the primary researcher used probing questions during the individual interviews to confirm participant responses and further explore concepts. Second, participants could review the transcripts of their interviews to confirm the accuracy and representativeness of their responses.
RESULTS
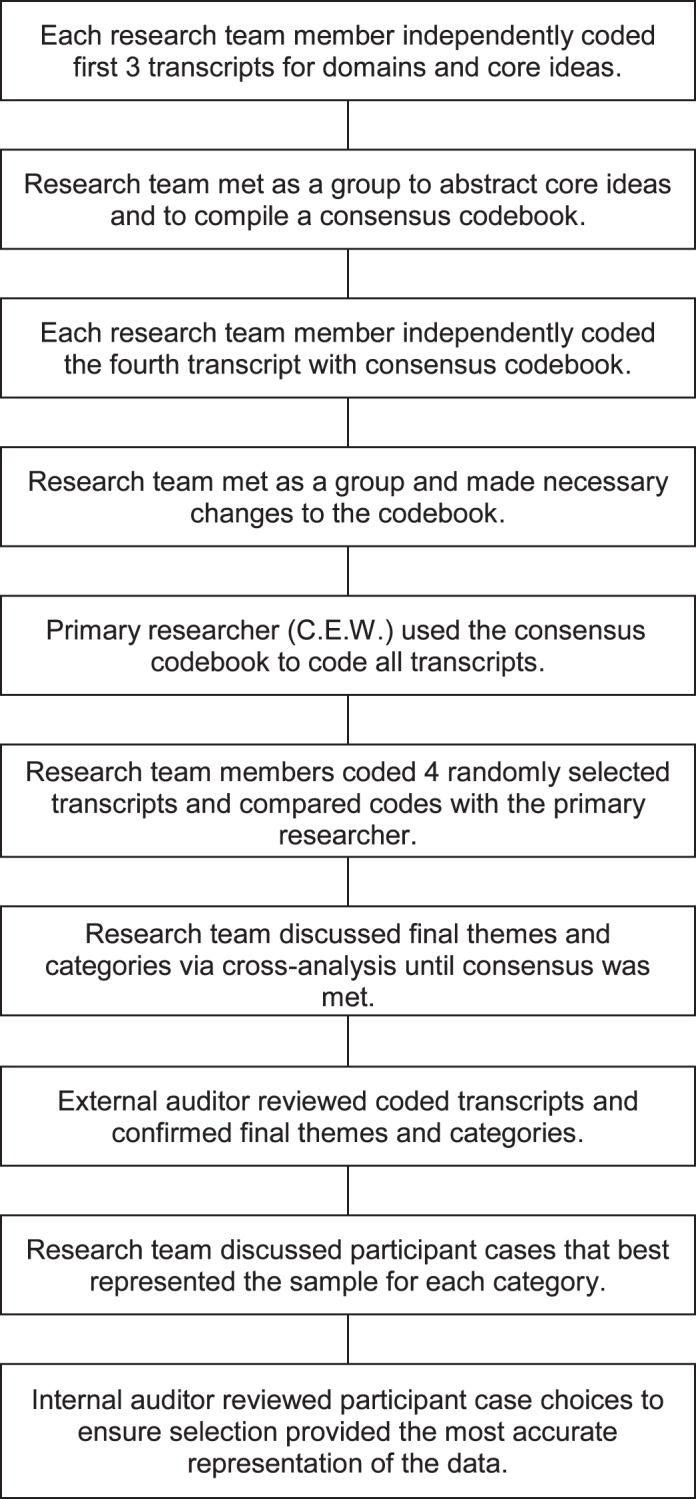
The CQR emergent design revealed 5 themes relating to the EBP Web-based modules, and the conceptual framework of themes is displayed in Figure 2. For the purposes of this article, we solely focused on educators' and clinicians' perceptions of the outcomes achieved within the 6 months after the implementation of the Web-based modules.
Figure 2. .
Conceptual framework of themes and categories. We focused solely on the theme of outcomes after the modules.
During the interviews, ATs generally perceived the EBP Web-based modules to produce various types of outcomes regarding athletic training education or clinical practice. Data analyzed from this theme were reduced to 6 pertinent categories: knowledge gain, importance and scope of EBP, positive impact on didactic teaching, instill value and practice of EBP among students, enhance ability to implement EBP within clinical practice, and no current impact on clinical practice. The frequency of participant cases per category is displayed in Table 4.
Table 4. .
Participant Cases By Category
| Category |
Frequency |
No. of Participant Cases |
| Knowledge gaina | General | 24 |
| Importance and scope of evidence-based practicea | Typical | 16 |
| Positive impact on didactic teachingb | General | 11 |
| Instill value and practice of evidence-based practice among studentsb | General | 11 |
| Enhance ability to implement evidence-based practice within clinical practicec | Typical | 7 |
| No current impact on clinical practicec | Typical | 10 |
Indicates clinicians and educators (n = 25).
Indicates educators only (n = 12).
Indicates clinicians only (n = 13).
Knowledge Gain
Generally, athletic training educators and clinicians described the Web-based modules as a beneficial educational medium to promote knowledge enhancement of the various EBP concepts. Dr Fosgate noted,
I thought I knew what [EBP] was until after going through these modules; I learned so much more about it... I definitely feel more comfortable talking about that information. I still think I have a ways to grow with it, but after doing the modules and taking the posttest I felt so much better; I was like “wow, I feel like I've actually learned something.”
Homier stated,
It definitely gave a better understanding [of] exactly what [EBP] is. I have been able to read [the literature] a little bit more concisely and find a little bit more material from it, and I know what is good and what is not good from reading the articles.
According to Dr Dominique,
That's really when I was realizing, okay, this isn't that intimidating; this really does relate to what we already do. For example, as I was going through the PICO [patient, intervention, comparison, outcome] format, that's where I was like “okay, I already do this, I'm just going to restructure how I approach it based on what I'm learning here.” So, it seemed more manageable, and it helped me break down the big umbrellas of EBP into how I could approach it and then also how I could teach students.
Moran commented,
I got a much better understanding of the process and why the evidence-based practice is a tool that we could use. I didn't really know anything about it beforehand, so it gave me a much better understanding of the use of it. I feel like this is something that I will be able to use.
Importance and Scope of EBP
Along with the ability to enhance knowledge, participants typically expressed that the modules enriched their perceptions of EBP and highlighted why this approach to clinical practice is an important shift for the athletic training profession. According to Dr Cavins, “It made me realize I have a long way to go but that this is really important and that we need to get on it.” Rose said,
I think it gave me a little bit different perspective on being more conscientious about best-practice procedures; a little sort of reminder of the importance of following best practices. I mean just the concept and importance of following best-practice procedures and realizing the importance of that in the progression of our profession.
Varner noted, “I definitely have a better understanding of why it's important; I definitely have a higher opinion of evidence-based practice after doing these modules.” Wilson said, “I think that it reinforced the fact that we need that evidence-based practice in our profession, but I had a firm belief already that we needed that.”
Positive Impact on Didactic Teaching
The 12 educators generally described the Web-based modules as having a positive effect on their abilities to implement the teaching of EBP throughout their athletic training curricula. Dr Birch said,
I think it definitely had a positive outcome on the way I approach the classroom because a lot of times it's easy for somebody that's in academia, especially doing research, to take a lot of these concepts for granted. But you just can't assume that people know this stuff, and it's easy to kind of just brush over the details with these, especially because I work with these concepts all of the time. I paid really good attention to the examples that the modules provided and the way the material was presented because it was meant to be presented as an introduction to evidence-based practice. And, that's what I'm giving to my students. I think for a lot of these concepts you really need to have examples and make the students apply these concepts to those examples until they've done enough repetitions to understand it.
Carpenter remarked,
The modules really allowed me to go ahead and use some of the language to explain to students in better words than I could come up with. In the past, I would just go up there and talk to students about [EBP concepts], and my guess is that I was talking to them probably at a level that some of them just didn't understand. So, I was able to use quite a bit of it in my teachings and will continue to do so. I think that's important, so it's really changed how I talk to my students about how they do what they do and why they do what they do.
Dr Fosgate explained,
The modules gave me a very good basis to have discussions about it, to implement assignments about it, and to just field questions from students as we talk about evidence-based practice in athletic training. So, I think it gave me a good basis of information for all of that. I guess I'm starting to incorporate it more so, and I think for me talking to our clinicians and asking what questions they have or what answers they want and kind of taking a look at that and coming up with clinical questions based on that.
Lavoy noted,
It changed my confidence in talking about it and teaching it. I think they had a positive impact for sure. The modules gave me more confidence because they gave me more information and so it became something I was thinking about all the time because it made more sense in my head, so it was something I was willing to start talking about in class and start really using the information that we were given, and I really started trying to look now as I am teaching and ask what the evidence says about this. So, I think having that EBP in the back of my head now because I feel like I know so much more about it. It makes me look for that as I am teaching.
Instill Value and Practice of EBP Among Students
Along with an enhanced ability to instruct students on the concepts of EBP in the classroom, the educators generally indicated specific techniques they have begun to use to incorporate EBP within their daily teaching practices. Educators most often discussed how they have begun to incorporate the patient, intervention, comparison, and outcome format and literature searching or use with their students. They also discussed several other implementation strategies. Dr Dominique observed,
I'm bringing in research articles as much as I can as we're talking about the topic to help them understand how it relates and just making sure that they don't just associate research and informed practice in their statistics class and in their research methods class; it really does have a role in all parts of athletic training. So, hopefully they realize that it's a part of everything that we do. I would say the most is just getting associated with the literature and the process of how do you go about it if you have a question or if you're making a decision. You don't just do what your [clinical preceptor] does.
Dr Birch said,
I really try to get our students to draw back to the evidence-based practice model regularly to see where different pieces of evidence fit when we're talking about some kind of clinical problem in class. If we first ask ourselves what we know about the problem, a lot of times we draw to our clinical experience and what we think our patients find meaningful, and then we go to the research experience. I think whenever you start with your theoretical model, which in this case is our evidence-based practice model, it gets students in the habit of going to the 3 sources of evidence to begin to make a decision versus just automatically saying, “Well, this is what I've done before, or this is what the research says we have to do.”
Dr Fosgate remarked,
I actually had my students do a critically appraised topic paper and also presented that to the [clinical preceptors] to say, “This tells you how clinically applicable this is without having to read that whole article.” So, trying to incorporate some assignments for them to get that practice of doing this to have a better understanding of some of this information.
Additionally, educators typically discussed how the Web-based modules inspired them to change assignments within the classroom to incorporate more EBP concepts. Dr Dominique explained,
In the past, we have had our seniors do an actual research project, but now what we're trying to do is get them to be more users of the evidence. So, they're going to be doing a critically appraised topic where, you know, they have an advanced clinical question, and then they're trying to really thoroughly review the literature. And then be able to turn around and write that in a paper and then present it to [clinical preceptors] and other students.
DiLorenzo noted,
This year, I completely changed this assignment that I've been doing in my classroom for years. This experience was the impetus for me to say, “You know it's time to do something different, it's time to do something more applicable, and this is where our students need to get some practice and some experience.” So, instead of doing an article review they're now doing this evidence-based assignment where they have to develop a clinical question using the PICO format and then they have to do a map of their search.
Lavoy observed,
I have actually changed the way I had them create and develop their project for that class—more based on evidence-based practice and you know, doing some hierarchy as far as diagnostic techniques and comparing and contrasting rehab[ilitation] programs and what the evidence says about each one of those. I really tried to use more of the principles of EBP in that class more for them to go out and find their own evidence, so they've had to develop a clinical question and really use the concept of evidence-based practice to develop a paper.
Enhance Ability to Implement EBP Within Clinical Practice
Athletic training clinicians typically described how the Web-based modules have enhanced the skills that will allow them to incorporate EBP into their daily clinical practices.
Moran commented,
As far as in my practice, I've actually used more research databases than I used to [to] try and figure out different solutions to different injuries that I've been having. I think it's just something that you have to practice using, I guess, and get used to how it works in your everyday work. So, it's just kind of getting used to and using it regularly, I guess.
According to Parker,
It just gave me some better strategies to access some things. I don't find it easy necessarily to go digging through the literature, but it did give me some places to go and strategies to use, so I think it's definitely had a positive impact on how I can actually search some literature. Some of the stuff in the later modules like processing the evidence and defining evidence, I find that information gave me a broader sense of understanding some of the literature. It puts it into context of how the rest of the medical world sees things. I think the things I took immediately were some of the search engine uses, what databases to look through, how to process some searches. How to use PubMed a little better, how to access some of the databases, how to actually find those databases and use them, that helped immediately, which I was able to dig into.
Varner said,
It got me more interested in reading more of the research articles and taking the time to understand the statistics and not just read the conclusions, but reading the methods and the results too. I'm just going a little bit more in depth with it and deciding for myself, “Okay, how do I think this will work with my patients in this setting?”
No Current Impact on Clinical Practice
Although clinicians typically perceived EBP to be an important concept for the athletic training profession after the implementation of the Web-based modules, they generally described that the modules did not have a current effect on their clinical decision-making process. Boyce explained,
I wouldn't really say they had that much of an impact—nothing new and exciting came up. I've got 30 years of experience under my belt now, so most of the stuff I see is something I've seen before. If something new and different had come up, it might have been fun because then I could have tied it all together, but nothing new and exciting came up.
Decker remarked,
I think just a lack of actually putting what I learned into practice; I think it might not have had an effect. I'm just still not looking at a research article and determining what the level of evidence is, you know? Maybe I have a wrong perception of my clinical skills, but I feel like where I'm at and how I'm getting my information and how I'm dictating my practice has worked thus far... I just don't think I'm motivated enough to do it. I would need to kind of take a look and say, “Well, why am I doing this,” but I don't think I've hit that point yet.
Wilson commented,
Probably not a real impact; working in the high school environment, I am not actually doing research and stuff. Not really an impact on how I work other than the fact of the reinforcement, the need that—yeah, I do need to keep current, and we need to ask questions about why we're doing that. But I am not sure if I could directly point [to] something where it changed my view or my treatment pattern. I am not sure if I actually took anything in particular from the subject matter and it went directly towards the kids. But since I am not doing research and I am not teaching, I generally don't have to use terms like that; that's kind of outside the scope of my day-to-day practice. But if I decide to teach or have a sports medicine class, I feel comfortable that with some of that stuff, I can add it in and talk about it.
In rare cases, clinicians described the Web-based modules as providing more academic information than components that could be implemented directly in their specific clinical practices. Therefore, they reported the modules had no effect on their clinical practice. Rose stated,
It was involved enough that it didn't really provide a learning experience for me as much as it was an exposure. It was way too much for me to swallow personally; I don't know that it really had any effect on my clinical practice.
Schaffer told us,
It hasn't been something that I use other than when I am reading the journal or reading other publications, to just be aware whether this research is something I should trust or not trust. The impact has been pretty negligible other than paying attention to the article and the research that's coming out. Nothing applicable because I don't feel that the modules led to anything clinically; they were academic as far as how to do a literature search and that type of thing.
DISCUSSION
This qualitative inquiry established that the implementation of 10 EBP Web-based modules did have some perceived positive effects on both educators and clinicians. Knowledge gain and enforcing the importance and scope of EBP were 2 principle benefits athletic training educators and clinicians identified from the implementation of the modules. Educators indicated that this educational intervention had an immediate positive effect on how they approach EBP in the classroom and discussed several examples of how they have begun to instill the value and practice of EBP in their students throughout the curriculum. Clinicians suggested that the Web-based modules enhanced their abilities to implement EBP within their clinical practices, yet they had not made specific changes to how they approach patient care. To effectively incorporate EBP within all realms of athletic training (ie, clinical practice, education, research), it is crucial not only to distinguish how to increase knowledge of the various concepts involved but also to focus on identifying the most successful ways to translate knowledge to clinical practice. To do so, we must focus on integrating educational teachings alongside best evidence that practicing clinicians can use to affect patient care.
Knowledge Gain and Knowledge Translation of EBP
Several researchers14,23–26 have examined the effect of educational interventions in enhancing the immediate knowledge of EBP concepts among health care professionals and have reported successful outcomes. In a review focusing on Web-based educational interventions, Chumley-Jones et al23 determined that Web-based learning effectively enhanced health care professionals' knowledge of a topic and was a comparable method to other educational interventions. Kerfoot et al25 also reported increases in urology test scores of medical students after they accessed a series of Web-based tutorials when compared with a control group. Specific to athletic training, Welch et al9 reported short-term knowledge increases among their participants, but it is unclear whether those improvements remained 6 months after the initial implementation of the educational intervention.
Assessment of knowledge retention of the EBP concepts after an educational intervention may be an important component to effectively integrate EBP into athletic training education and clinical practice. However, we must look beyond knowledge retention and begin to focus on knowledge translation. Knowledge translation is most accurately described as “a dynamic and iterative process that includes synthesis, dissemination, exchange and ethically-sound application of knowledge to improve the health of patients, provide more effective health services and products and strengthen the health care system.”27 More directly, knowledge translation focuses on methods that will ensure the transfer of clinicians' knowledge to practice to improve patient care and health care outcomes. Clinical experience may be the avenue clinicians use most when answering a clinical question. Although considering clinical expertise still is important during the clinical decision-making process, knowledge-translation models may help to diminish the EBP knowledge-behavior gap,28 allowing clinicians to more effectively incorporate research evidence alongside clinical experience. Although the examination of knowledge translation is fairly new to health care professions, the infusion of EBP across medicine and health care has ignited the need to determine the most effective manner of converting knowledge attained into knowledge used in practice. Several theories and models have been proposed for knowledge translation (eg, predisposing, reinforcing and enabling constructs in educational diagnosis and evaluation–policy, regulatory, and organizational constructs in educational and environmental development [PRECEDE-PROCEED] model, the Ottawa Model of Research Use)29–32; however, research on which model is most successful for EBP in health care is limited.
One model that commonly is discussed across health care disciplines is the PRECEDE-PROCEED Model of Health Program Planning and Evaluation.33 The foundation of this model outlines 3 essential steps that could help move the athletic training profession toward an EBP culture. First, ATs must be predisposed to change by increasing knowledge of EBP concepts.33,34 Strides have been taken over the past 5 years to accomplish this goal among various groups of ATs.2,7,9,35 Second, change must be enabled by promoting ideal conditions in both the educational and practice settings. Third, after the EBP paradigm shift occurs for athletic training, ATs must continue to reinforce it.33,34 The PRECEDE-PROCEED model33 has been incorporated in other health professions, such as medicine and nursing, and researchers36–38 have been encouraged that it is successful at achieving the desired goal of improving patient care. Thus, as ATs begin to determine the best mechanisms to promote knowledge translation of EBP concepts into practice, the profession should consider adopting a knowledge-translation model, such as PRECEDE-PROCEED, used in other health care professions. This model may be an effective mechanism to help clinicians incorporate new knowledge along with previous clinical experience when making sound clinical decisions, which in turn may help improve the overall care provided to patients.
Positive Impact on Athletic Training Educators
Participants in our investigation reported that the EBP Web-based modules had a positive effect on their instruction mode and encouraged positive changes in how they approach EBP in the classroom. This is an important step forward in removing the lack-of-knowledge barrier that athletic training educators have expressed in the literature.3,8 In addition, many participants discussed the integration of EBP throughout the curriculum and a holistic approach to implementation of these concepts rather than just the addition of an independent EBP class. This finding supports strategies suggested by athletic training educators3 and clinical preceptors.1 The EBP concepts can be incorporated throughout didactic curricula in several ways because there is no set place where a concept must be discussed and no single strategy to effectively discuss it. As professional athletic training programs continue to develop the curricula to align with the fifth edition of the NATA's Athletic Training Education Competencies,35 they should focus on implementation techniques that work best for the faculty and clinical staff at specific institutions. However, given that the EBP concepts are foundational to clinical practice and may affect how a student chooses to make effective clinical decisions based on evidence, educators should aim to introduce the EBP concepts to athletic training students early and often. Students not only must learn the foundations of EBP but also must learn how to routinely incorporate the EBP paradigm into their decision-making process in the clinical setting.
As educators make changes to align their didactic curricula with the new EBP competencies, they must determine their own views on incorporating the EBP paradigm. Educators must ensure that the material included in their courses not only meets the needs of the athletic training competencies but also provides real-life examples that will resonate with the students. Classroom instruction may reach students on an academic level, yet unless it has relevance to clinical practice, students will be unlikely to transfer that information into practice.39 For students to truly embrace EBP and carry it with them throughout their careers, they must understand, respect, and foster the blend of research evidence, clinical expertise, and patient preferences for optimal patient care.40 Therefore, students must learn early in their academic careers that incorporating evidence into clinical practice requires active inquiry.41 Current techniques and strategies to apply best practices to patient care also must be questioned continually to determine whether they are the best mechanisms for any given patient.
Influence on Athletic Training Clinicians
Clinicians in our investigation indicated the Web-based modules elicited small changes in their perceived abilities to implement EBP within practice. They remarked that the Web-based modules provided them with tools and strategies to more effectively search for literature and have a more comprehensive understanding of what they read. Our findings also indicated that the Web-based modules enhanced their confidence with the concepts of EBP. Hankemeier and Van Lunen2 assessed confidence among ATs in their knowledge of EBP concepts. A weak positive relationship was found between their knowledge of EBP and confidence, indicating that individuals with higher knowledge scores also perceived themselves to be more confident in their knowledge of EBP. Therefore, although our participants composed only a small sample of athletic training clinicians and educators, we can hypothesize that the increased confidence of ATs in this investigation may be due to increased knowledge of EBP concepts after the implementation of the Web-based modules.
Even though clinicians reported an enhanced ability to implement EBP concepts within their practices, they also indicated that they had not changed their daily practices or clinical decision making. Our results were similar to those of other authors11,13 investigating outcomes after an educational intervention. Whereas multiple researchers have found mixed results in behavioral changes after an educational intervention, the most common types of interventions that promote positive changes in clinical practice and improved patient care are interactive interventions and strategies that are multifaceted (eg, didactic lecture combined with interactive discussion).42–44 Single-strategy educational interventions (eg, lecture format only) designed to translate evidence into practice have been shown to have a poor effect on sustained practice changes.45 Similarly, purely didactic interventions have not produced behavioral changes in health care professionals.42 These findings imply that future educational interventions targeted at altering the clinical behaviors of ATs should focus on mixed modes of delivery and interactive strategies.
Kent et al28 suggested that multiple approaches should be initiated and that each approach should be alternative and proactive. Incorporating reminders, educational outreach visits, and mechanisms that provide evaluation and feedback have been identified as suitable hands-on approaches that allow individuals to be proactive in the learning process.28,45 Investigators need to identify strategies to help clinicians understand and implement the concepts of EBP and overcome barriers that may prevent them from translating new knowledge into clinical practice. Additionally, new strategies also should highlight the direct clinical benefits of incorporating EBP to improve patient care. Athletic training educational mediums supported with evidence (eg, practice briefs, clinical bottom lines, NATA Foundation alerts, conference presentations) need to be provided continually throughout continuing education opportunities.
Athletic trainers are expected to be active decision makers daily, and the EBP process aligns with the active decision-making process of athletic training. They must recognize that being informed about evidence is not the only factor that is vital to actually practicing in an evidence-based manner, and they must embrace the various sources of evidence that may contribute to their bodies of knowledge. Contrary to what clinicians may perceive, evidence can come in forms other than laboratory research. Whereas strictly controlled research is widely regarded as the primary form of evidence, it must be conducted in a manner that ensures both internal validity and clinical applicability. In some instances, research literature that is considered to be lower-level evidence (eg, case reports, case series) may be warranted depending on the type of clinical question (eg, prognosis, diagnosis, intervention) being asked. Furthermore, evidence that may be of use to clinicians also can be generated via peer and expert dialogue, as well as clinical outcomes. According to Ciliska et al,46 EBP mentors can help clinicians guide their own EBP by acting as facilitators in evidence consumption. Thompson et al47 determined that nurses use human resources as the primary means of gathering evidence in uncertain situations. The most common resources they used were experts (ie, clinical nurse specialists, experienced colleagues) and peer dialogue (ie, primary and secondary care colleagues). They also consulted other health care professionals when the situation was outside of their primary expertise (ie, pharmacists). To facilitate the incorporation of EBP within athletic training, practicing clinicians should identify appropriate mentors and contact other ATs who are experts in EBP implementation.
Athletic trainers should be comfortable using expert and peer sources of information in situations where they are uncertain, especially when research evidence in a particular topic area is unavailable. Expert and peer dialog should not be limited strictly to ATs but should include an interprofessional collaboration with other health care professionals who may be experts in EBP implementation.47 Individuals must be motivated to pursue EBP from a patient-centered care perspective. Athletic trainers should be inspired to integrate research evidence and their patients' goals and values with their clinical expertise to optimize individual patient outcomes.
Changing the Use of Evidence in Daily Practice
To stay in line with other health care professions and truly become an evidence-based profession, athletic training needs to embrace cognitive and behavioral changes from both local and global perspectives.4,48 Athletic trainers need to develop a mutually beneficial model of enhancing EBPs within all realms of the profession. Although ensuring that individual ATs enhance their practices through the use of multiple evidence sources is important, change also must occur at an organizational level. The need for a paradigm shift in athletic training is not a new concept,48 and researchers1,8 have confirmed that ATs perceive the incorporation of EBP as a necessary cultural shift to enhance the profession. As with any transformation, the shift from clinical decisions based in tradition and authority to decisions supported by evidence will require an organizational change.1 The nursing profession has outlined several EBP models that facilitate organizational change to foster the incorporation of EBP into practice.39 Of particular interest is the advancing research and clinical practice through close collaboration (ARCC) model. This model is designed to aid professionwide application and sustainability of EBP to enhance quality health care outcomes.39 The primary strategy of this model is the incorporation of EBP mentors who work directly with clinicians to develop strategies that diminish the barriers commonly reported for EBP implementation (eg, inadequate time, lack of available resources, knowledge).39 The ARCC model's premise is that if the barriers to EBP diminish, clinicians will be more likely to adopt EBP and make changes to their daily practices.39 Thus, by providing EBP mentors to help clinicians reduce implementation barriers, the ARCC model is promoting an avenue for organizational change and a paradigm shift toward an EBP culture.
Athletic training educators must accept a pivotal role in the translation of evidence into practice. Because they facilitate the professional development, professional learning, and personal growth of students each day,34 educators are the fundamental first step in helping students become familiar and comfortable with accessing, appraising, translating, and when applicable, applying research evidence into clinical practice.28 Therefore, educators must realize that they are the foundation of knowledge translation to future generations of ATs and that they serve as the link between the researchers who produce evidence and the clinicians who are being instructed to apply the evidence.49 Results50 from a systematic review have suggested that nursing educators are the ideal individuals to facilitate knowledge translation in nursing because they are familiar with nursing practices and have strong backgrounds in the field. Thus, given that large numbers of athletic training educators also are involved in clinical education components, they are well suited to facilitate knowledge translation. Additionally, clinical preceptors are well versed in athletic training practices and can draw from their own experiences as clinicians to help students progress.
Specific mechanisms for change at an organizational level need to include constant revisions of the NATA's educational competencies to include new and developing health care reforms and to eliminate required competency in skills that are not supported by EBP. By continuing to teach these unsupported ideas and skills, the perpetual cycle of practice based on tradition will not be broken. In addition, a reform of continuing education that requires more active participation in continuing education units may enhance the shift to EBP. Organizational change also can be facilitated with frequently updated position statements and guidelines. The NATA occasionally releases position statements that give overviews of the suggested plans of care for various conditions and situations that ATs may encounter. However, position statements generally are compiled only on topics that may be associated with profound legal concerns. If more position statements or practice guidelines focusing on conditions, treatments, and situations that ATs encounter daily were made available, the way clinicians approach situations might be more consistently in line with the best research evidence. Whereas research has been divided on the effectiveness of dissemination of clinical practice guidelines, many investigators have concluded that clinicians prefer information that is easy to apply and sources of evidence that do not require active search and appraisal of the literature. Thompson et al47 interviewed nurses who communicated they preferred sources of information that were quick to access, easy to understand, and grounded in clinical usefulness. Similarly, in their review, Grol and Grimshaw51 found that clinical guidelines offering a more concrete description of a desired clinical application were associated with better compliance with the recommendations.
A cultural shift from the current model of athletic training practice to EBP will require dedication from every facet of the profession. Clinicians, educators, researchers, and students need to be willing to embrace this change. In addition, leaders in the profession need to continue to facilitate this shift at the organizational level. By embracing the integration of patient values, clinical expertise, and the best available research evidence to improve patient care and health care outcomes, the profession of athletic training can gain recognition as an integral part of the health care community.
Limitations
We selected our participants from a specific group of ATs who took part in a study to assess the effect of Web-based modules to enhance knowledge of EBP concepts and, therefore, were from a nonrandomized sample of the population. Their perceptions and experiences with the Web-based modules themselves may have influenced whether they had successful or unsuccessful outcomes when implementing EBP within their teaching or clinical practices. The Web-based modules that were used in the previous investigation were not designed in a way that would appeal to all types of learners. If participants in this investigation did not respond well to Web-based learning, their responses for this study may have been affected. Although we assumed all participants spoke truthfully about their experiences with the Web-based modules, the self-report nature of the educators' and clinicians' implementation of EBP within practice also may be a limitation. During this investigation, we did not compare the responses of participants with their quantitative knowledge scores of the EBP concepts involved in the Web-based modules. Therefore, their perceptions of knowledge gain and actual knowledge retention cannot be justified. Further research is necessary to determine whether the short-term knowledge gained immediately after the educational intervention was retained after a 6-month period.
CONCLUSIONS
As athletic training continues to shift toward becoming an evidence-based profession, substantial focus needs to be given to diminishing the gap between evidence and practice. Strategies to bridge this gap should target individual ATs and should change at an organizational level. This investigation sheds light on the outcomes sustained from an educational intervention to enhance knowledge of EBP concepts among ATs. Participants perceived that the Web-based modules enhanced their knowledge and the importance of EBP, and educators indicated a positive effect on didactic instruction patterns, as well as on instilling value and practice of EBP in students. Additionally, although some clinicians reported the Web-based modules had no effect on their clinical practices, others perceived an enhanced ability to implement EBP within clinical practice.
Whereas having a mechanism to increase knowledge of EBP within athletic training is a step in the right direction, the ultimate goal is to change clinical practice in a manner that enhances patient outcomes. Based on a multitude of research in other health care professions, we suggest that future strategies should be focused on multiple approaches and continual follow-up. Investigators should aim to identify successful strategies to aid ATs in effectively implementing EBP into education and clinical practice. Studies in which researchers investigate the perceptions of clinical preceptors regarding strategies for EBP also would be beneficial because these individuals most often are involved in both didactic and clinical portions of the education of athletic training students. Additionally, researchers should assess which approaches and educational interventions effectively increase translating knowledge into practice. Further consideration also should be given to the adoption of a knowledge translation model to assist the athletic training profession in the paradigm shift to fostering an EBP culture.
ACKNOWLEDGMENTS
The Mid-Atlantic Athletic Trainers' Association provided financial support for this investigation. We thank Dr Sarah Manspeaker for her support of this qualitative inquiry.
REFERENCES
- 1.Hankemeier DA, Van Lunen BL. Approved Clinical Instructors' perspectives on evidence-based practice implementation strategies for students. J Athl Train. 2011;46(6):655–664. doi: 10.4085/1062-6050-46.6.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hankemeier DA, Van Lunen BL, McCarty CW, et al. Use of evidence-based practice among athletic training educators, clinicians, and students, part 1: perceived importance, knowledge, and confidence. J Athl Train. 2013;48(3):394–404. doi: 10.4085/1062-6050-48.2.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manspeaker S, Van Lunen B. Overcoming barriers to implementation of evidence-based practice concepts in athletic training education: perceptions of select educators. J Athl Train. 2011;46(5):514–522. doi: 10.4085/1062-6050-46.5.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Welch CE, Van Lunen BL, Walker SE, et al. Athletic training educators' knowledge, comfort, and perceived importance of evidence-based practice. Athl Train Educ J. 2011;6(1):5–14. [Google Scholar]
- 5.Welch CE, Van Lunen BL, Walker SE, et al. Effectiveness of a single-day evidence-based concepts pilot workshop for athletic training educators [abstract] Athl Train Educ J. 2011;6(1):S28–S29. (suppl): [Google Scholar]
- 6.Hankemeier DA, Van Lunen BL. Perceptions of approved clinical instructors: strategies for overcoming barriers in the implementation of evidence-based practice [abstract] J Athl Train. 2011;46(3):S37–S38. doi: 10.4085/1062-6050-48.1.18. (suppl) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manspeaker SA, Van Lunen BL, Turocy P, Pribesh S, Hankemeier DA. Student knowledge, attitudes and use of evidence-based concepts following an educational intervention. Athl Train Educ J. 2011;6(2):88–98. [Google Scholar]
- 8.McCarty CW, Hankemeier DA, Walter JM, Newton EJ, Van Lunen BL. Use of evidence-based practice among athletic training educators, clinicians, and students, part 2: attitudes, beliefs, accessibility, and barriers. J Athl Train. 2013;48(3):405–415. doi: 10.4085/1062-6050-48.2.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Welch CE, Van Lunen BL, Hankemeier DA. An evidence-based practice educational intervention for athletic trainers: a randomized controlled trial. J Athl Train. 2014;49(2):210–219. doi: 10.4085/1062-6050-49.2.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ciliska D. Evidence-based nursing: how far have we come? What's next? Evid Based Nurs. 2006;9(2):38–40. doi: 10.1136/ebn.9.2.38. [DOI] [PubMed] [Google Scholar]
- 11.Cameron C, Naylor CD. No impact from active dissemination of the Ottawa Ankle Rules: further evidence of the need for local implementation of practice guidelines. CMAJ. 1999;160(8):1165–1168. [PMC free article] [PubMed] [Google Scholar]
- 12.Fritsche L, Greenhalgh T, Falck-Ytter Y, Neumayer H, Kunz R. Do short courses in evidence based medicine improve knowledge and skills? Validation of Berlin questionnaire and before and after study of courses in evidence based medicine. BMJ. 2002;325(7376):1338–1341. doi: 10.1136/bmj.325.7376.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennedy T, Regehr G, Rosenfeld J, Roberts SW, Lingard L. Exploring the gap between knowledge and behavior: a qualitative study of clinician action following an educational intervention. Acad Med. 2004;79(5):386–393. doi: 10.1097/00001888-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Nicholson LJ, Warde CM, Boker JR. Faculty training in evidence-based medicine: improving evidence acquisition and critical appraisal. J Contin Educ Health Prof. 2007;27(1):28–33. doi: 10.1002/chp.90. [DOI] [PubMed] [Google Scholar]
- 15.Corbin J, Strauss A. Basics of Qualitative Research. 3rd ed. Los Angeles, CA: Sage Publications Inc;; 2008. [Google Scholar]
- 16.Giorgi A. Sketch of a psychological phenomenological method. In: Giorgi A, editor. Phenomenology and Psychological Research. Pittsburgh, PA: Duquesne University Press;; 1985. pp. 8–22. In. ed. [Google Scholar]
- 17.Elliott R. Comprehensive process analysis: understanding the change process in significant therapy events. In: MJ Parker, Addison RB., editors. Entering the Circle: Hermaneutic Investigations in Psychology. Albany, NY: State University of New York Press;; 1985. pp. 165–184. In. eds. [Google Scholar]
- 18.Hill CE, Knox S, Thompson BJ, Nutt-Williams E, Hess SA, Ladany N. Consensual qualitative research: an update. J Couns Psychol. 2005;52(2):196–205. [Google Scholar]
- 19.Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed. Thousand Oaks, CA: Sage Publications Inc;; 2002. [Google Scholar]
- 20.Goetz JP, LeCompte MD. Ethnography and Qualitative Design in Educational Research. New York, NY: Academic Press;; 1984. [Google Scholar]
- 21.Lincoln YS, Guba EG. Naturalistic Inquiry. Beverly Hills, CA: Sage Publications Inc;; 1985. [Google Scholar]
- 22.Mahrer AR. Discovery-oriented psychotherapy: rationale, aims, and methods. Am Psychol. 1988;43(9):694–702. doi: 10.1037//0003-066x.43.9.694. [DOI] [PubMed] [Google Scholar]
- 23.Chumley-Jones HS, Dobbie A, Alford CL. Web-based learning: sound educational method or hype: a review of the evaluation literature. Acad Med. 2002;77(10 suppl):S86–S93. doi: 10.1097/00001888-200210001-00028. [DOI] [PubMed] [Google Scholar]
- 24.Greenhalgh T. Computer assisted learning in undergraduate medical education. BMJ. 2001;322(7277):40–44. doi: 10.1136/bmj.322.7277.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kerfoot BP, Baker H, Jackson TL, et al. A multi-institutional randomized controlled trial of adjuvant web-based teaching to medical students. Acad Med. 2006;81(3):224–230. doi: 10.1097/00001888-200603000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Letterie GS. Medical education as a science: the quality of evidence for computer-assisted instruction. Am J Obstet Gynecol. 2003;188(3):849–853. doi: 10.1067/mob.2003.168. [DOI] [PubMed] [Google Scholar]
- 27.About knowledge translation & commercialization. Canadian Institutes of Health Research Web site. http://www.cihr-irsc.gc.ca/e/29418.html. Published 2009. Modified May 15, 2013. Accessed October 2, 2013. [Google Scholar]
- 28.Kent B, Hutchinson AM, Fineout-Overholt E. Getting evidence into practice-understanding knowledge translation to practice change. Worldviews Evid Based Nurs. 2009;6(3):183–185. doi: 10.1111/j.1741-6787.2009.00165.x. [DOI] [PubMed] [Google Scholar]
- 29.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall;; 1986. [Google Scholar]
- 30.Fox RD, Mazmanian PE, Putnam RW. Changing and Learning in the Lives of Physicians. New York, NY: Praeger Publications;; 1989. [Google Scholar]
- 31.Pathman DE, Konrad TR, Freed GL, Freeman VA, Koch GG. The awareness-to-adherence model of the steps to clinical guidelines compliance: the case of pediatric vaccine recommendations. Med Care. 1996;34(9):873–889. doi: 10.1097/00005650-199609000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Tyler RW. Basic Principles of Curriculum and Instruction. Chicago, IL: University of Chicago Press;; 1949. [Google Scholar]
- 33.Green LW, Kreuter M, Deeds S, Partridge K. Health Education Planning: A Diagnostic Approach. Palo Alto, CA: Mayfield Press;; 1980. [Google Scholar]
- 34.Davis D, Evans M, Jadad A, et al. The case for knowledge translation: shortening the journey from evidence to effect. BMJ. 2003;327(7405):33–35. doi: 10.1136/bmj.327.7405.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Athletic Trainers' Association. Athletic Training Education Competencies. 5th ed. Dallas, TX: National Athletic Trainers' Association;; 2011. pp. 1–32. [Google Scholar]
- 36.Chiang LC, Huang JL, Yeh KW, Lu CM. Effects of a self-management asthma educational program in Taiwan based on PRECEDE-PROCEED model for parents with asthmatic children. J Asthma. 2004;41(2):205–215. doi: 10.1081/jas-120026078. [DOI] [PubMed] [Google Scholar]
- 37.Mirtz TA, Thompson MA, Greene L, Wyatt LA, Akagi CG. Adolescent idiopathic scoliosis screening for school, community, and clinical health promotion practice utilizing the PRECEDE-PROCEED model. Chiropr Osteopat. 2005;13:25. doi: 10.1186/1746-1340-13-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tu K, Mamdani MM, Jacka RM, Forde NJ, Rothwell DM, Tu JV. The striking effect of the Heart Outcomes Prevention Evaluation (HOPE) on ramipril prescribing in Ontario. CMAJ. 2003;168(5):553–557. [PMC free article] [PubMed] [Google Scholar]
- 39.Fineout-Overholt E, Williamson KM, Kent B, Hutchinson AM. Teaching EBP: strategies for achieving sustainable organizational change toward evidence-based practice. Worldviews Evid Based Nurs. 2010;7(1):51–53. doi: 10.1111/j.1741-6787.2010.00185.x. [DOI] [PubMed] [Google Scholar]
- 40.Melnyk B, Fineout-Overholt E, Stillwell S, Williamson K. Transforming healthcare quality through innovations in evidence-based practice. In: Porter-O'Grady T, Malloch K, editors. Innovation Leadership. Boston, MA: Jones & Bartlett;; 2010. In. eds. [Google Scholar]
- 41.Doanes GH, Varcoe C. Knowledge translation in everyday nursing: from evidence-based inquiry to inquiry-based practice. ANS Adv Nurs Sci. 2008;31(4):283–295. doi: 10.1097/01.ANS.0000341409.17424.7f. [DOI] [PubMed] [Google Scholar]
- 42.Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. The Cochrane Effective Practice and Organization of Care Review Group. BMJ. 1998;317(7156):465–468. doi: 10.1136/bmj.317.7156.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Davis DA, O'Brien MA. Freemantle, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282(9):867–874. doi: 10.1001/jama.282.9.867. [DOI] [PubMed] [Google Scholar]
- 44.Wensing M, van der Weijden T, Grol R. Implementation guidelines and innovations in general practice: which interventions are effective? Br J Gen Pract. 1998;48(427):991–997. [PMC free article] [PubMed] [Google Scholar]
- 45.Grimshaw JM, Thomas RE, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Asses. 2004;8(6):iii–iv. doi: 10.3310/hta8060. 1–72. [DOI] [PubMed] [Google Scholar]
- 46.Ciliska D, DiCenso A, Melnyk B, Stetler C. Using models and strategies for evidence-based practice. In: Melnyk BM, Fineout-Overholt E, editors. Evidence-Based Practice in Nursing and Healthcare: A Guide to Best Practice. Philadelphia, PA: Lippincott Williams & Wilkins;; 2005. In. eds. [Google Scholar]
- 47.Thompson C, Kinmonth AL, Stevens L, et al. Effects of a clinical-practice guideline and practice-based education on detection and outcome of depression in primary care: Hampshire Depression Project randomized controlled trial. Lancet. 2000;355(9199):185–191. doi: 10.1016/s0140-6736(99)03171-2. [DOI] [PubMed] [Google Scholar]
- 48.Winterstein A. A changing paradigm. Athl Ther Today. 2006;11(1):22–24. [Google Scholar]
- 49.Dobbins M, Robeson P, Ciliska D, et al. A description of a knowledge broker role implemented as part of a randomized control trial evaluating three knowledge translation strategies. Implement Sci. 2009;4:23. doi: 10.1186/1748-5908-4-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Milner M, Estabrooks CA, Myrick F. Research utilization and clinical nurse educators: a systematic review. J Eval Clin Pract. 2006;12(6):639–655. doi: 10.1111/j.1365-2753.2006.00632.x. [DOI] [PubMed] [Google Scholar]
- 51.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003;362(9391):1225–1230. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]