Abstract
Objective:
To provide athletic trainers, physicians, and other health care professionals with best-practice guidelines for the management of sport-related concussions.
Background:
An estimated 3.8 million concussions occur each year in the United States as a result of sport and physical activity. Athletic trainers are commonly the first medical providers available onsite to identify and evaluate these injuries.
Recommendations:
The recommendations for concussion management provided here are based on the most current research and divided into sections on education and prevention, documentation and legal aspects, evaluation and return to play, and other considerations.
Key Words: mild traumatic brain injuries, pediatric concussions, education, assessment, evaluation, documentation
Despite a significant increase in research dedicated to identifying and managing sport-related concussion, it remains one of the most complex injuries sports medicine professionals face. Concussions occur from forces applied directly or indirectly to the skull that result in the rapid acceleration and deceleration of the brain. The sudden change in cerebral velocity elicits neuronal shearing, which produces changes in ionic balance1 and metabolism.2 When accompanied by clinical signs and symptoms, changes at the cellular level are commonly referred to as mild traumatic brain injury, or concussion. Concussions occur in males and females of all ages and in all sports, but are most common in contact and collision activities. Data collected from emergency department visits show a 62% increase (153 375 to 248 418) in nonfatal traumatic brain injuries between 2001 and 2009,3 with as many as 3.8 million reported and unreported sport- and recreation-related concussions occurring each year in the United States.4
As licensed medical professionals, athletic trainers (ATs) receive comprehensive didactic and clinical training in concussion management. They are typically the first providers to identify and evaluate injured persons and are integral in the postinjury management and return-to-play (RTP) decision-making process. Without exception, ATs should be present at all organized sporting events at all levels of play and should work closely with a physician or designate who has specific training and experience in concussion management to develop and implement a concussion-management plan based on the recommendations outlined here.
An update to the initial 2004 National Athletic Trainers' Association position statement on the management of sport-related concussion,5 this document contains recommendations on concussion management for practicing ATs based on the most recent scientific evidence. A review of the literature supporting these recommendations has also been included. The document covers the topics of “Education and Prevention,” “Documentation and Legal Aspects,” “Evaluation and RTP,” and “Other Considerations.”
INJURY DEFINITION
To best assemble the available concussion research and remain consistent with other medical groups, we sought to evaluate literature that defined concussion as a “trauma-induced alteration in mental status that may or may not involve loss of consciousness.”6 This definition was selected based on its broad application by medical organizations and widespread use within the literature from the time of the first National Athletic Trainers' Association position statement. We recognize the strength of the definition provided by the International Concussion in Sport Group and its subpoints as valid features that further define concussion.7 In evaluating and writing this document, we also included research defining concussive injuries in these terms. Notably absent from the literature and consistent with previous recommendations were the terms “ding,” “getting one's bell rung,” “clearing the cobwebs,” and other such phrases in reference to concussive injuries.5 These colloquial terms are antiquated, minimize injury severity, and should not be used to refer to concussion or mild traumatic brain injury.
RECOMMENDATIONS FOR CLINICAL PRACTICE
Education and Prevention
The clinical practice recommendations for each topic have been graded based on the Strength of Recommendation Taxonomy (SORT; Table 1).8
Table 1. .
Strength of Recommendation Taxonomy (SORT)a
| Strength of Recommendations |
Definition |
| A | Recommendation based on consistent and good quality experimental evidence (morbidity, mortality, exercise and cognitive performance, physiologic responses) |
| B | Recommendation based on inconsistent or limited quality experimental evidence |
| C | Recommendation based on consensus; usual practice; opinion; disease-oriented evidenceb; case series or studies of diagnosis, treatment, prevention, or screening; or extrapolations from quasi-experimental research |
Reprinted with permission from “Strength of Recommendation Taxonomy (SORT): A Patient-Centered Approach to Grading Evidence in the Medical Literature,” February 1, 2004, American Family Physician. Copyright © 2004 American Academy of Family Physicians. All Rights Reserved.
Patient-oriented evidence measures outcomes that matter to patients: morbidity, mortality, symptoms improvement, cost reduction, and quality of life. Disease-oriented evidence measures are intermediate, physiologic, or surrogate end points that may or may not reflect improvements in patient outcomes (eg, blood pressure, blood chemistry, physiologic function, pathologic findings).
1. The AT should use, and educate others in using, the proper terminology of concussion and mild traumatic brain injury as opposed to such colloquial terms as “ding” and “bell ringer.”9 Strength of Recommendation: B
2. The AT should work with the appropriate administrators to ensure that parents and coaches are educated on the following aspects of concussion: prevention, mechanism, recognition and referral, appropriate return to participation, physical and cognitive restrictions for concussed athletes, and ramifications of improper concussion management.10–12 Strength of Recommendation: B
3. The AT should be aware of and document potential modifying factors that could delay the RTP, and patients should be educated on the implications of these conditions as they affect recovery (Table 2).7 Strength of Recommendation: C
4. The AT should work to educate coaches, athletes, and parents about the limitations of protective equipment for concussion prevention. Strength of Recommendation: C
5. As part of educational efforts, ATs, athletes, coaches, and parents should read all warning labels associated with protective equipment. Strength of Recommendation: C
Table 2. .
Factors That May Modify the Risk of Concussion and Duration of Recovery7
| Risk |
Modifiers |
| Symptoms | Number |
| Duration (>10 d) | |
| Severity | |
| Signs | Prolonged loss of consciousness (>1 min), amnesia |
| Sequelae | Concussive convulsions |
| Temporal | Frequency: repeated concussions over time |
| Time: injuries close together in time | |
| Recency: recent concussion or traumatic brain injury | |
| Threshold | Repeated concussions occurring with progressively less impact, force, or slower recovery after each successive event |
| Age | Child or adolescent (<18 y) |
| Comorbidities and premorbidities | Migraine, depressions, or other mental health disorders; attention-deficit hyperactivity disorder; learning disabilities; sleep disorders |
| Medication | Psychoactive drugs, anticoagulants |
| Behavior | Dangerous style of play |
| Sport | High-risk activity, contact or collision sport, high sporting level |
Documentation and Legal Aspects
6. The AT should be aware of any and all relevant governing bodies (eg, state, athletic conference) and their policies and procedures regarding concussion management. Strength of Recommendation: C
7. The AT should document the athlete's (and when appropriate, the parent's) understanding of concussive signs and symptoms and his or her responsibility to report a concussion. Strength of Recommendation: C
8. The AT should communicate the status of concussed athletes to the managing physician on a regular basis. Strength of Recommendation: C
9. The AT should ensure proper documentation of the concussion evaluation, management, treatment, return-to-participation progression, and physician communications. Strength of Recommendation: C
Evaluation and RTP
10. Athletes at high risk of concussion (eg, those in contact or collision sports) should undergo baseline examinations before the competitive season.5,13,14 Strength of Recommendation: B
11. A new baseline examination should be completed annually for adolescent athletes, those with a recent concussion, and, when feasible, all athletes.15–17 Strength of Recommendation: B
12. The baseline examination should consist of a clinical history (including any symptoms), physical and neurologic evaluations, measures of motor control (eg, balance), and neurocognitive function.5,7,18–20 Strength of Recommendation: B
13. The baseline and postinjury examinations should be administered in similar environments that maximize the patient's abilities, and all baseline examinations should be reviewed for suboptimal performance.21 Strength of Recommendation: C
14. Any athlete suspected of sustaining a concussion should be immediately removed from participation and evaluated by a physician or designate (eg, AT). Strength of Recommendation: C
15. The concussion diagnosis is made through the clinical evaluation and supported by assessment tools.19 Strength of Recommendation: B
16. When the rapid assessment of concussion is necessary (eg, during competition), a brief concussion-evaluation tool (eg, Standardized Assessment of Concussion [SAC]20,22,23) should be used in conjunction with a motor-control evaluation and symptom assessment to support the physical and neurologic clinical evaluation. Strength of Recommendation: B
17. Once a concussion diagnosis has been made, the patient should undergo a daily focused examination to monitor the course of recovery. Strength of Recommendation: C
18. During the acute postconcussion recovery stage, daily testing of neurocognitive function and motor control is typically not needed until the patient is asymptomatic.24 Strength of Recommendation: C
19. A concussed athlete should not be returned to athletic participation on the day of injury.9 Strength of Recommendation: C
20. No concussed athlete should return to physical activity without being evaluated and cleared by a physician or designate (eg, AT) specifically trained and experienced in concussion evaluation and management. Strength of Recommendation: C
21. Young athletes with a past medical history that includes multiple concussions, a developmental disorder (eg, learning disabilities, attention-deficit hyperactivity disorder), or a psychiatric disorder (eg, anxiety, depression) may benefit from referral to a neuropsychologist to administer and interpret neurocognitive assessments and determine readiness to return to scholastic and athletic activities.7,25 Strength of Recommendation: C
22. A physical-exertion progression should begin only after the concussed athlete demonstrates a normal clinical examination, the resolution of concussion-related symptoms, and a return to preinjury scores on tests of motor control and neurocognitive function.7,26 Strength of Recommendation: C
23. Concussed athletes who do not show a typical progressive return to normal functioning after injury may benefit from other treatments or therapies. Strength of Recommendation: C
24. Concussion-grading scales should not be used to manage the injury. Instead, each patient should be evaluated and treated on an individual basis.7,9 Strength of Recommendation: B
25. After the injury has resolved, the concussion may be retrospectively graded for the purpose of medical record documentation. Strength of Recommendation: C
Other Considerations
Equipment
26. The AT should enforce the standard use of certified helmets while educating athletes, coaches, and parents that although such helmets help to prevent catastrophic head injuries (eg, skull fractures), they do not significantly reduce the risk of concussions.7,27–29 Strength of Recommendation: B
27. Helmet use in high-velocity sports (eg, alpine sports,30–32 cycling33–35) has been shown to protect against traumatic head and facial injury. Strength of Recommendation: A
28. Consistent evidence to support the use of mouthguards for concussion mitigation is not available. However, substantial evidence demonstrates that a properly fitted mouthguard reduces dental injuries.29 Strength of Recommendation: B
29. Research on the effectiveness of headgear in soccer players to reduce concussion is limited. The use of headgear is neither encouraged nor discouraged at this time. Strength of Recommendation: C
Pediatric Concussion
30. When working with children and adolescents, ATs should be aware that recovery may take longer than in adults and require a more prolonged RTP progression.7,36,37 Strength of Recommendation: B
31. Age-appropriate, validated concussion-assessment tools should be used in younger populations.7,25 Strength of Recommendation: C
32. Assessment of postconcussion symptoms in pediatric patients should include age-validated, standardized symptom scales and the formal input of a parent, teacher, or responsible adult.38–40 Strength of Recommendation: B
33. Pediatric athletes are undergoing continual brain and cognitive development and likely need more frequent updates to baseline assessments.16,41 Strength of Recommendation: B
34. Athletic trainers should work with school administrators and teachers to include appropriate academic accommodations in the concussion-management plan.7,39,42 Strength of Recommendation: C
Home Care
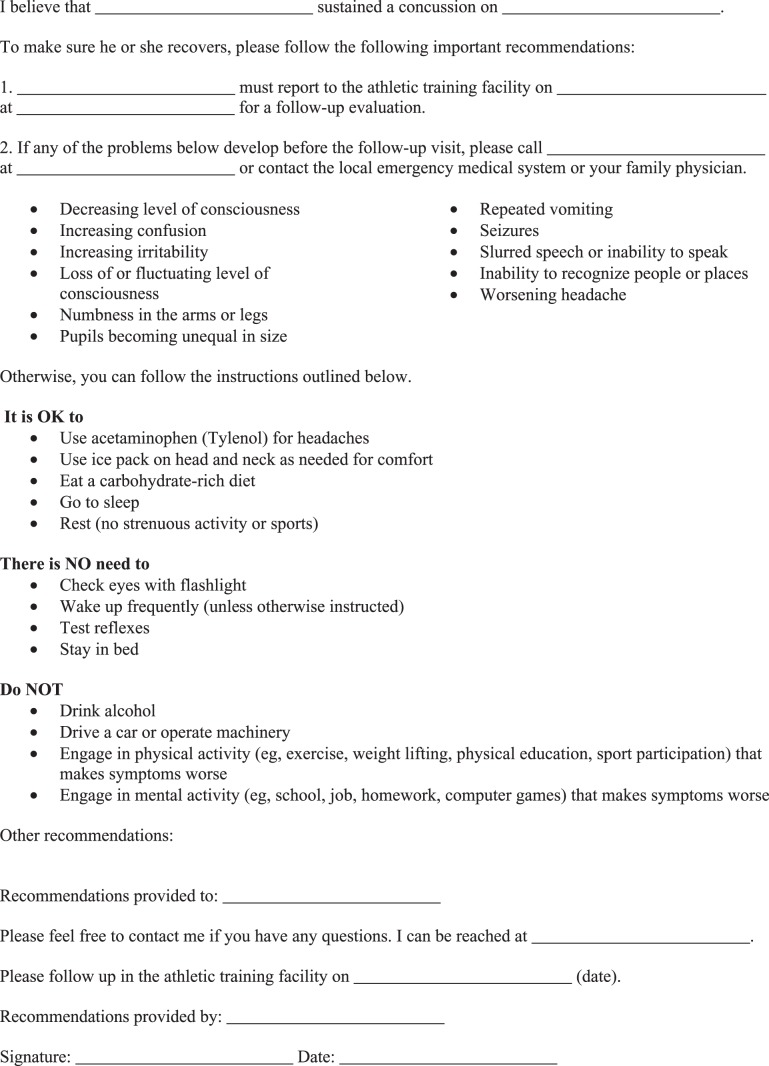
35. The AT and physician should agree on a standard concussion home-instruction form (eg, Appendix A) that is consistently used for all concussed patients, and a copy should be maintained in the medical record. Both oral and written instructions for home care should be given to the concussed athlete and to a responsible adult (eg, parent or roommate) who will observe and supervise the patient during the acute phase of the concussion.5,43 Strength of Recommendation: C
36. After a concussion diagnosis, the patient should be instructed to avoid medications other than acetaminophen. All current medications should be reviewed by the physician. 5,44,45 Strength of Recommendation: C
37. After a concussion diagnosis, the patient should be instructed to avoid ingesting alcohol, illicit drugs, or other substances that might interfere with cognitive function and neurologic recovery.5 Strength of Recommendation: C
38. After the initial monitoring period, rest is currently the best practice for concussion recovery. As such, there is typically no need to wake the patient during the night unless instructed by a physician.5 Strength of Recommendation: C
39. During the acute stage of injury, the patient should be instructed to avoid any physical or mental exertion that exacerbates symptoms.5,7,28,39,42 Strength of Recommendation: C
40. In addition to exclusion from physical activity related to team activities, concussed student-athletes should be excused from any activity requiring physical exertion (eg, physical education classes). Strength of Recommendation: C
41. School administrators, counselors, and instructors should be made aware of the patient's injury with a recommendation for academic accommodation during the recovery period.7,28,39,42 Strength of Recommendation: C
42. A patient with a concussion should be instructed to eat a well-balanced diet that is nutritious in quality and quantity and should drink fluids to stay hydrated.5 Strength of Recommendation: C
Multiple Concussions
43. For an athlete with a concussion history, the AT should adopt a more conservative RTP strategy.7,46,47 Strength of Recommendation: B
44. Referral to a physician or designate with concussion training and experience should be considered when an athlete with a history of multiple concussions sustains concussions with lessening forces, demonstrates increasing severity with each injury, or demonstrates objective or subjective changes in baseline brain function. Strength of Recommendation: C
45. The AT should recognize the potential for second-impact syndrome in young patients who sustain a second trauma to the brain prior to complete resolution of the first injury.1,48–50 Strength of Recommendation: C
46. The AT should be aware of the potential for long-term consequences of multiple subconcussive and concussive impacts.51–53 Strength of Recommendation: C
SUPPORTING LITERATURE REVIEW
Education and Prevention
When athletes, parents, coaches, administrators, and others discuss concussive injuries, they should use the appropriate medical terminology: concussion or mild traumatic brain injury. Use of such colloquial terms as “ding,” “bell ringer,” and “getting your bell rung” has a connotation that mitigates injury severity and should thus be avoided. For example, a noted decline in neurocognitive ability at 36 hours after injury was reported in patients labeled as “dinged” whose symptoms appeared to resolve within 15 minutes.9 This finding demonstrates a more serious effect of what was initially considered a minor injury.
Before the competitive season, the AT should review all concussion policies and procedures that outline injury definition, signs and symptoms, and the institution's policy on concussion management (see “Documentation and Legal Aspects” below regarding how state laws and organizational body regulations may influence institutional concussion policy). In many instances, the AT has access to the most up-to-date information on concussion diagnosis and management. This information should be disseminated to all of those involved in athlete health care as rapidly as possible and in an appropriate manner. These individuals include but are not limited to coaches, athletes, parents, administrators, and other medical professionals. In addition to these documents, agencies have developed educational information specific to coaches, athletes, and parents that has been shown to effectively educate the target audience.54–56
Athletes themselves have demonstrated limited knowledge regarding concussion symptoms; more than 50% of high school athletes57 and 70% of collegiate athletes58 did not report concussions sustained during football. One reason for nonreporting was that athletes were not aware of the signs and symptoms of concussion. Another study59 of high school rugby players demonstrated more knowledge of concussion signs and symptoms (61%); however, the athletes had limited knowledge of postinjury concussion-management guidelines. For example, 25% of the athletes believed loss of consciousness was required for the injury to be considered a concussion.59 Educational methods are effective in increasing athletes' awareness of concussion symptoms. Goodman et al60 found that exposure to a concussion-symptom video game improved symptom identification among youth ice hockey players.60 Similarly, Bramley et al61 noted that high school soccer players who received concussion education were more likely to report concussion symptoms to their coach.
Researchers57 have documented athletes' lack of willingness to report concussions to medical personnel, so parents of youth athletes should also be educated to recognize signs and symptoms of concussion. Parents (or guardians) typically have the most contact with young athletes and so are well positioned to report atypical behavior, but many parents are not properly educated on the topic of concussion.62 Sullivan et al63 reported that parents of male high school rugby athletes were knowledgeable about the signs and symptoms (83%) and the risks associated with continuing to play while injured (96%), yet only half were aware of the appropriate RTP guidelines after injury.
Even in the presence of an AT, coaches have the responsibility for recognizing the signs and symptoms of concussion in athletes. Several studies, however, have shown that coaches have limited knowledge and many misconceptions related to concussions. In a survey of youth sports coaches, 45% of respondents believed a concussion did not require immediate removal from a game or practice, and only 62% could correctly identify proper postconcussion management.10 In another investigation,64 high school coaches demonstrated greater overall knowledge of sport concussion (84%); they knew the most about injury recognition (92%) and the least about injury management (79%). Concussion-specific training is effective in improving injury knowledge: those attending a coaching education program10 or a coaches' workshop64 scored higher than nonattendees on their respective surveys. Sarmiento et al11 reported that 34% of high school coaches using the Centers for Disease Control and Prevention's “Heads Up” tool kit for concussion improved their concussion knowledge; specifically, they gained knowledge related to injury signs and symptoms. The coaches also noted that the tool kit changed their attitudes and behaviors related to concussion.11 Similarly, a short (15–20 minute), interactive, online, concussion-education program aimed at youth sports coaches resulted in improvements in symptom knowledge, general knowledge, injury misconceptions, self-efficacy, and behavioral intention.12 Collectively, these findings suggest that a brief training session on sport-concussion signs, symptoms, and injury management targeted at coaching staff can improve injury recognition. This type of training may ultimately benefit the AT by encouraging coaches to help identify concussed athletes and follow treatment plans.
After a concussive event, the AT should also educate the patient and any additional stakeholders (eg, parents and administrators) about the typical injury recovery. Although injury severity and a precise time to recover cannot be predicted immediately after injury, most concussed athletes return to their preinjury level of functioning within 2 weeks.65 However, several factors, including specific symptom patterns,7,66 age, and sex,67 may influence injury recovery and delay the return to participation (Table 2). Informing the patient about expected outcomes after injury may reduce anxiety about the injury and associated symptoms.7,68
Documentation and Legal Aspects
Certified ATs, team physicians, and other health care providers responsible for the management of patients with sport-related concussion should be aware of potential liabilities involved with delivering medical coverage and making RTP decisions for patients. Concussion management has medical and legal implications, and the threat of lawsuits is increasing for sports medicine professionals. Previous lawsuits against ATs and team physicians have addressed the premature clearing of patients and, surprisingly, withholding patients from play after concussion.69–73 Therefore, it is imperative for clinicians to manage these injuries in a systematic manner, using objective assessments, while documenting their daily findings. Certain legal principles are common to the laws of each state, but material differences exist in the decisions of the higher courts for each state and in state statutes.74 It is, however, the responsibility of the AT to follow the best-practice guidelines, recommendations, and practice limitations adopted by their respective work setting or oversight organization (eg, National Federation of State High School Associations, National Collegiate Athletic Association, National Football League) and the best practices for licensed ATs established, in part, by the position statements of the National Athletic Trainers' Association. In addition, ATs working in states with concussion-management legislation are bound to follow those laws in the event of a discrepancy with organizational guidelines or position statements.
To avoid litigation, ATs should understand the general elements of negligence and malpractice that typically govern claims for injury or death caused by improper treatment. A tort is a private wrong or injury suffered by a person as the result of another person's conduct. The law gives injured persons the right to be compensated through the recovery of damages. Torts may be intentional, meaning that the person intended to act, or unintentional, in that the person did not mentally intend to cause harm. A tort is committed when an AT fails to act as an ordinary and reasonably prudent person under similar circumstances and causes injury to another person.74,75
Negligence is an unintentional tort. Negligence law was founded on the principle that those who are harmed as the result of others' carelessness or failure to properly carry out responsibilities must be compensated. The person who was harmed has the burden of proving that the 4 legal elements of negligence are satisfied: a duty of care was owed as a result of a relationship that existed between the parties; the defendant breached the duty owed to the injured party; the breach of the duty is proved to be the cause of the harm to the plaintiff; and actual harm, not just the potential for harm, must have occurred. All 4 elements of negligence must be proven in order for the plaintiff to be compensated by the defendant for damages.75,76
Athletic trainers employed to treat and manage athletic injuries such as concussion owe a duty of reasonable care to their patients and have been the target of lawsuits alleging failures to meet the standard of care after sport-related injury, especially concussion. Allegations against ATs in cases of negligence after concussion most often include improper evaluation and testing of the patient, improper documentation, misunderstood communications with the patient, and a lack of education of the patient or the patient's family.77 For ATs to minimize the risk of becoming defendants and to better defend themselves should a case be filed, they must understand the standard of care for managing specific injuries based on the most recent scientific literature. The standard of care in athletic training is defined as a person's “legal duty to provide health care services consistent with what other health care practitioners of the same training, education, and credentialing would provide under the circumstances.”78 Athletic trainers can learn how the standard of care is applied to legal cases by examining specific cases and the firsthand experiences of those who have defended ATs during the litigation process.77
The athletic training profession must identify and adopt standard practice limitations and guidelines to establish the standard of care for managing concussions and other brain injuries. Ambiguity and the lack of a clear standard make it easier for plaintiffs' lawyers to construct theories of liability for lawsuits against ATs, alleging they breached the standard of care after a suspected concussion.77 Lawsuits against ATs often involve the evaluation or testing of the patient (or lack thereof), documentation of an injury, communications with the patient or with a physician about a patient, and education of the patient.
In a 2008 California case, an AT was found liable for failing to properly and promptly evaluate a patient who apparently had sustained a concussion only to later pass out, fall, and suffer a variety of physical injuries as a result of the AT's alleged failures.79 The court ordered the defendants to pay substantial damages to the injured patient. In another case, a University of Tennessee football player recovered hundreds of thousands of dollars when an AT allegedly failed to promptly report a patient's initial and ongoing symptoms to a physician. The patient subsequently sustained an acute subdural hematoma in connection with an injury incurred 1 month later.80 In another case, a high school football player alleged that his AT failed to properly evaluate him or take seriously his reported headaches and dizziness after a concussion and then prematurely returned him to play, which allegedly caused the patient to suffer second-impact syndrome after a second concussion 2 weeks later.81 In this case, although the jury awarded no damages to the injured player, the cost to the defendants was 3 years of litigation, substantial legal fees and expenses, and a month-long, stressful, high-profile trial.
Another possible allegation in the cases against ATs involves the lack of documentation in managing a sport-related concussion. For several years, ATs have been advised to document “all pertinent information” surrounding concussions.5 The documentation of information surrounding the evaluation and management of any suspected concussion should include but not be limited to (1) mechanism of injury; (2) initial signs and symptoms; (3) state of consciousness; (4) findings of the physical and neurologic examinations, symptoms, neurocognitive function, and motor control (noting any deficits compared with baseline); (5) instructions given to the patient or parent (or both); (6) recommendations provided by the physician; (7) graduated RTP progression, including dates and specific activities; and (8) relevant information on the patient's history of prior concussion and associated recovery pattern(s). Though lengthy, this level of detail can help prevent a premature return to participation, catastrophic brain injury such as second-impact syndrome, and legal liability. The expression “if it's not written, it didn't happen” is often used in legal situations. The question in these cases sometimes becomes whether certain information is or is not “pertinent.” For example, at some point during a concussed athlete's RTP progression, he or she will begin performing graduated exertional exercises (see “Evaluation and RTP” below). Daily documentation of the details surrounding this progression will help to avoid potential litigation in the event that the recovery or return to participation does not proceed as expected. For example, the dates on which the testing was performed, the witnesses to the testing, the actual maneuvers the patient performed, and the patient's description of any symptoms during or after activity should be documented. The value of this documentation may not be realized for some time, as legal trials generally occur years after the alleged improper conduct, when it is unlikely that anyone can accurately recall the details if they were not recorded at the time.
At the time of writing, all 50 states have enacted concussion laws. Nearly all of these laws include the components of (1) educating athletes, parents, and coaches; (2) instituting a concussion policy and emergency action plan; (3) removing the athlete from practice or play at the time of the suspected concussion; and (4) having a health care provider with training in concussion management perform medical evaluation and RTP clearance. The AT must know the laws of the state and recognize that failure to warn or educate the athlete can be the basis for another possible allegation. One simple way to educate athletes about the dangers of concussion and continuing to play while still symptomatic is to require them to read and sign a standard acknowledgment form indicating that they understand the signs and symptoms of concussion and their responsibility to report a concussion (Appendix B). Some legal experts even suggest that athletes should sign an acknowledgment that they understand the warning a manufacturer has placed on a helmet. For example, some football helmets carry warnings such as this:
Contact in football may result in concussion/brain injury, which no helmet can prevent. Symptoms include loss of consciousness or memory, dizziness, headache, nausea, or confusion. If you have symptoms, immediately stop and report them to your coach, [athletic] trainer, and parents. Do not return to a game or contact until all symptoms are gone and you receive medical clearance. Ignoring this warning may lead to another and more serious or fatal brain injury. No helmet system can protect you from serious brain and/or neck injuries, including paralysis or death. To avoid these risks, do not engage in the sport of football. (Reprinted with permission of Schutt Sports.)
In catastrophic cases where such an acknowledgment of understanding has not been secured by the AT, a “failure to warn” claim almost certainly will be made against the AT, especially when the plaintiff alleges that the patient never recovered from an earlier injury. Thus, before each season, at a minimum, the AT should require that each athlete read a concussion fact sheet, read the aforementioned warning on the helmet, and sign an acknowledgment that he or she read and understood both. Not only do these acknowledgments serve as a possible defense to a failure-to-warn claim, but under certain circumstances, they may also be used to establish that the patient is legally responsible for his or her own injuries (if, for example, the athlete reports symptoms to teammates but withholds the information from team personnel and continues to play). When a defendant asserts and can show that the plaintiff's injuries are a result of the plaintiff's own negligence, the defendant may prevail on a theory of contributory negligence or comparative negligence, which could bar the plaintiff from recovering any damages whatsoever.
The more education the AT provides to the patient (and parents of a patient who is a minor) concerning the risks of RTP before a complete recovery after a concussion (eg, the risk of playing while still symptomatic), the greater the likelihood of success the AT will have in defending against a failure-to-warn or failure-to-educate claim. More importantly, enhanced education to athletes should translate into more informed participants, which should lead to fewer catastrophic injuries.77 Finally, it is imperative that practicing ATs understand their individual state laws on concussion management because some states have made provisions for ATs to clear a concussed athlete to RTP. However, a physician with specific training and experience in concussion management should still be involved in the comprehensive approach to concussion management outlined in this position statement. A concussion-management policy outlining the roles and responsibilities of each member of the sports medicine team should be adopted.
Evaluation and RTP
Approach to Concussion Evaluation
The clinical presentation of concussion varies considerably both between individuals and between injuries in 1 individual. Additionally, the degree of brain dysfunction manifested by concussion often produces signs and symptoms that fall within the range of normal experiences in the population (eg, dehydration, fatigue, anxiety). For these reasons, a concussion-assessment model that uses objective baseline testing and careful postinjury testing is recommended. Although all athletes should ideally undergo a preseason baseline assessment, at a minimum, athletes who are at a high risk of concussion based on their sport67,82 should be included in any baseline testing program. Furthermore, athletes with a significant concussion history or other relevant comorbidity, such as attention-deficit hyperactivity disorder, should be considered for testing on an individual basis.
The intent of baseline testing is to aid the clinician in the postinjury management process by providing data that represent an athlete's brain function in an uninjured state. Objective baseline and postinjury information can be highly sensitive to concussive injuries,19 but the concussion diagnosis is made by clinically evaluating the injured athlete. In this way, postinjury retesting should not be considered a diagnostic tool for concussion, nor should it be used as a sole determinant of when it is safe to return to participation; rather, it is a supplement to support the clinical examination. These data are then best used as part of a comprehensive concussion- management approach that is communicated to the directing physician and other members of the sports medicine team with concussion training and experience.
Baseline Testing
The baseline evaluation of an athlete for the purpose of concussion management should include a documented neurologic history with symptoms and physical examination (Table 3). Baseline testing should also involve the objective evaluation of multiple spheres of brain function and, at minimum, assess neurocognitive performance and motor control. Obtaining premorbid self-report symptoms is also recommended for comparison with postinjury symptom presentations and for improved interpretation of other test data. Additionally, medication use should be carefully documented and made available for postinjury review.
Table 3. .
Suggested Domains of the Clinical History and Examination for Concussion Management
| Domain |
Features or Examples |
How to Assess?a |
| Previous concussions | Date(s) and circumstances; presence and duration of loss of consciousness, amnesia, and symptoms with each injury | Preparticipation examination |
| Concussion-related personal history | Mood disorder, learning disability, attention-deficit hyperactivity disorder, epilepsy or seizures, sleep apnea, skull fracture, migraine headaches | Preparticipation examination |
| Family history | Mood disorder, learning disability, attention-deficit hyperactivity disorder, dementia (eg, Alzheimer disease), migraine headaches, complications from concussions | Preparticipation examination |
| Symptoms | Current and recurrent | Symptom checklist or scale |
| Mental status | Level of consciousness, attention and concentration, orientation, memory | Standardized Assessment of Concussion |
| Eye examination | Eye movements with smooth pursuit (cranial nerves III, IV, VI), nystagmus (VIII), pupillary reflex (CN II, III) | Clinical examination |
| Muscle strength | Strength evaluation of deltoids, biceps, triceps, wrist and finger flexors and extensorsb; pronator drift | Clinical examination |
| Motor control | Balance assessment | Balance Error Scoring System |
| Cognitive function | Reaction time, working memory, delayed recall | Neurocognitive testing |
Assessment tools are indicated where available.
Notable deficits may be associated with nerve root injury or concussion.
Numerous testing methods are available for concussion management. When selecting specific tests and procedures for the concussion-assessment and concussion-management protocol, the AT should consult with members of the sports medicine team regarding the best tools for the clinical setting and secure written approval from the administration. When selecting specific assessment tools, the AT must also be aware of the limitations and requirements of the particular baseline test being considered. For example, the reliability of computer-based cognitive tests varies with the test-retest interval,83–87 and additional costs may be incurred to interpret test results.88,89
Once the tests are selected, care should be taken to provide each athlete with an environment that is designed to maximize test performance and be easily reproduced in the postinjury setting. Large-group administration of baseline tests is discouraged; small-group administration is preferable. Having a sufficient number of proctors and using standardized procedures are important.21 The AT should avoid conducting tests at unusual times of the day to ensure that athletes are reasonably rested and not physically or mentally fatigued after a practice or workout. Whenever possible, athletes should not undergo baseline testing when they are ill or injured in a manner that could influence test results. Lastly, if appropriate resources are available, the AT should conduct annual baseline tests on athletes. This is most crucial in adolescents, whose brains are continuing to develop,15–17 and in those who have sustained a concussion since their previous test.
Self-Report Symptom Assessment
Collecting subjective symptom information from a patient is a dynamic and complex process. Using symptom checklists (ie, yes/no) or scales (ie, graded and summed responses) that assess symptom duration or severity (or both) in a standardized manner90 is recommended. In general, symptom reports provide good sensitivity to concussive injuries,19,20 but the degree to which symptom reports can be a useful part of the neurologic history and examination in concussion management is potentially minimized by their limitations. Because of the nature and physical demands of athletics, an evaluation of concussion-related symptoms can yield low specificity compared with the reference standard of clinician-diagnosed concussion. That is, concussion-like symptoms are also commonly reported in athletes who are dehydrated91 and those who have performed strenuous activity92; the presence of these symptoms does not mean the athlete will demonstrate balance or neurocognitive impairments.93 In addition, for a variety of reasons, athletes may be motivated to underreport symptoms so they can continue activity after injury.57
Numerous concussion inventories are available for clinical use, including the Head Injury Scale,94 Graded Symptom Checklist,5 Concussion Symptom Inventory,7,95 and Sport Concussion Assessment Tool 3 (SCAT-3).7 The AT should choose a symptom-evaluation protocol that best suits his or her clinical practice and be consistent in its administration.
Motor Control
The diffuse effects of concussive injuries on brain function can often lead to deficits in motor control. Changes in motor control after injury have been documented in several areas, including gait,96,97 postural control,65,98–100 and hand movement101. As such, the assessment of 1 or more motor-control systems can provide useful information for concussion diagnosis and management. Perhaps the most common concussion-assessment tool is the evaluation of postural control. Overall balance deficits after injury have been attributed to failure to integrate sensory information arising from the vestibular and visual components of the balance mechanism.98–100 The Sensory Organization Test, although used successfully to quantify changes to the balance mechanism,19,102 is limited by cost and portability. In the initial days of injury, the Balance Error Scoring System (BESS) demonstrates similar injury sensitivity,20,65 is highly portable, and can be administered with minimal cost and training. As with other concussion-assessment tools, the AT should select the tools that best suit the clinical setting, be trained in their proper administration,103,104 understand their limitations,105–110 and use consistent methods in baseline and postinjury evaluations.
Mental-Status Testing
A change in mental status is the hallmark of concussion,6 yet concussed athletes rarely present with easily identifiable signs of injury. In fact, loss of consciousness is present in fewer than 10% of patients and posttraumatic amnesia in 25% of patients.46 In the absence of easily identifiable signs after concussion, an objective measure of mental status can significantly aid the AT in making the sideline diagnosis. Traditional questions of mental status involving questions of orientation about time (eg, what time is it?), location (eg, where are we?), and the person (eg, when is your birthday?) are ineffective in the sporting environment.111 The SAC was developed as a brief mental-status screening tool and is recommended for sideline use when comprehensive neurocognitive testing (see the next section) is not available or applicable. The SAC is a 5-minute test that evaluates the domains of orientation, immediate memory, concentration, and delayed recall.23 As a stand-alone measure used immediately after concussion, the SAC is highly sensitive to injury; its sensitivity is further increased when used with a symptom inventory and motor-control test.20 Sensitivity of the SAC to concussion declines 24 hours after injury; thus, use of the test to evaluate cognitive functioning is not recommended beyond this point.20
Neurocognitive Testing
Neurocognitive testing has historically been viewed as the cornerstone of the concussion-assessment process,112 yet when used in isolation, this technique does not provide clinically adequate sensitivity to concussion.19,20,113 Therefore, neurocognitive testing should never be used in isolation but rather in conjunction with symptom and motor-control assessments to support the clinical examination. Historically, pencil-and-paper tests, such as the Digit Span, Controlled Oral Word Association Test, and Hopkins Verbal Learning tests, have been used to evaluate concussive injuries. Several computer-based platforms are now available, including the Automated Neuropsychological Assessment Metrics (ANAM), Cogstate Axon, Concussion Vital Signs, Headminder Concussion Resolution Index (CRI), and Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT). The testing protocol should evaluate those domains known to be affected by concussion: information processing, planning memory, and switching mental set.112 Similar to other assessment methods, neurocognitive testing has limitations,114 and the AT should become familiar with the benefits and limitations of the testing methods selected.19,113,115,116
Regardless of the instrumentation, the emphasis should be on maximizing performance on the baseline and postinjury assessments. The test should be explained to the athlete before the assessment begins, and a distraction-free testing environment should be provided.21 After the baseline assessment, test scores should be reviewed using the manufacturer's validity criteria to ensure that the athletes gave maximal effort; those demonstrating suboptimal effort should retake the test.117 Once an athlete is injured, the AT and medical staff should limit the number of tests to time points that are critical to injury management to avoid performance improvements resulting from practice effects.118,119 Also, although some tests provide automated pass or fail scoring, these outputs may not accurately reflect the patient's injury status and are not recommended for clinical use.86 A neuropsychologist or physician with specific concussion training should interpret the postinjury data.89
Diagnosing Concussion
Concussion diagnosis in the athletic environment can be difficult given the pressures and time restrictions of competition. Some sports allow for unlimited injury- evaluation time, but others do not. Regardless of the time allotment, the AT and the medical staff should never feel pressured to complete a concussion assessment. At the time of suspected injury, the initial evaluation should assess acute trauma. If the athlete is unable to leave the field under his or her own power, the AT should perform a primary survey, including evaluation of airway, breathing, and circulation (ie, the ABCs). Whether the patient is conscious or not, the AT should suspect and, if possible, rule out a cervical spine injury and other more severe injuries. Once no life-threatening injuries are determined to be present, the concussion examination should begin.
Any athlete suspected of having a concussion should immediately be removed from participation and a systematic injury evaluation conducted. The intent of the concussion examination is to establish if the athlete should be removed from further participation. Regardless of the assessment measures used as part of the concussion-management protocol, the concussion diagnosis is made after a thorough clinical examination (Table 3). The clinical examination should include an injury history (including symptoms), observation of the patient, palpation for more severe orthopaedic or neurologic injury, and special tests for mental status and motor control (described earlier).120,121 Brief assessments that rely on the patient's response to such simple questions such “Are you OK?” or “Can you go?” are not supported and should not be used. The concussion assessment conducted by the AT should be implemented in a consistent fashion as part of a comprehensive neurologic evaluation. When a physician is not readily available, the AT should be more conservative when interpreting the clinical-examination results and making the injury diagnosis.
Transport to a medical facility for a concussion is not typically required but may be necessary if the patient is unconscious for a prolonged period of time (>1 minute), shows declining mental status during or after the injury evaluation, or demonstrates signs and symptoms of an injury more severe than a concussion. For a patient who is transported, the attending physician may recommend imaging to rule out injuries more severe than concussion, but computed tomography and magnetic resonance imaging add little to the concussion-evaluation process.7 Although other diagnostic techniques, such as functional magnetic resonance imaging,122 diffusion tensor imaging, magnetic resonance spectroscopy,2,123 serum biomarkers,124 and biomechanical techniques125,126 may be helpful in identifying and diagnosing concussion, their exclusive use as diagnostic tools has not been validated.
Postinjury Management
Once an athlete has been diagnosed with a concussion, he or she should be removed from the sport and not allowed to return to physical activity until cleared by a physician or designate, no sooner than the next day. The patient should not be left unattended on the sideline, and mental status should be regularly monitored. A notable decline in mental status may reflect more severe trauma and indicate that transport to a medical facility is necessary. In most instances, however, the patient can be sent home with appropriate postinjury instructions (see the “Home Care” section).
Once the concussion diagnosis has been made, a focused examination of the patient should be conducted daily to ensure a normal course of recovery. The magnitude of impact127,128 or postinjury decrements relative to preinjury testing should not be interpreted as a measure of injury severity or a predictor of how long the patient should be withheld from sport.129 Indeed, although the concept of grading injury severity based on such factors as the presence or absence of consciousness, symptom duration, and mental status has previously been supported,5 this is no longer the case. Each patient and each injury should be treated uniquely, focusing on cessation of symptoms and restoration of motor control, and neurocognitive test results should revert to preinjury levels before an RTP progression is implemented.
During the acute recovery period, the patient should be instructed to avoid physical activity (eg, workouts, conditioning, physical education) and limit cognitive activity (eg, academic work, video games, computer use) so as to not exacerbate concussion symptoms. Physical activity during the acute phase can have a detrimental effect on recovery,130 but the effect of cognitive stress on concussion recovery is less clear. As such, limiting cognitive activities to avoid worsening concussion symptoms is favored over complete isolation of the patient, which may result in the exacerbation of concussion-like symptoms unrelated to the injury.131
Once the patient no longer reports concussion-related symptoms and the clinical examination is normal, then objective assessments should be repeated and compared with baseline performance. The patient's reports of concussion-related symptoms are used as the primary measure to advance to the next stage in postconcussion management, so careful attention should be paid to steady resolution over time. In most instances, patients who no longer report concussion-related symptoms demonstrate preinjury performance levels on cognitive and motor control tests, but up to 40% of asymptomatic patients have continued cognitive declines.118,119 Therefore, the return-to-activity decision-making process should not begin until the patient no longer reports concussion-related symptoms, has a normal clinical examination, and performs at or above preinjury levels on measures of neurocognitive function and motor control. Although the duration of recovery demonstrated by individual patients on neurocognitive and motor-control tests varies, young adult males typically return to preinjury levels of functioning within 2 weeks.65 Female patients and younger patients may suffer from postinjury declines for 14 days or longer.36,132 Those reporting dizziness at the time of injury may have a protracted recovery,66 and those suffering from concussion symptoms beyond 30 days may be diagnosed with postconcussive syndrome.133 Some evidence suggests that normative data can be used for postinjury evaluations when baseline testing is not available.13 This scenario, however, is not ideal, and a more conservative injury-management strategy is warranted in these instances. During the recovery process, the AT should maintain regular contact with the directing physician to track the recovery and ensure that appropriate medical care is provided if recovery does not proceed normally.
Return-to-Play Decision Making
After an athlete is diagnosed with a concussion, the RTP progression should not start until he or she no longer reports concussion-related symptoms, has a normal clinical examination, and performs at or above preinjury levels of functioning on all objective concussion assessments. The exertion progression should follow the pattern outlined in Table 4; the typical time frame consists of 24 hours between levels.7 However, if activity at any stage results in a return of symptoms or a decline in test performance,134 then the activity should be immediately halted and restarted 24 hours later. The RTP timing is case dependent, but most patients diagnosed with a concussion can expect to be withheld from competition for at least 1 week. The AT can lengthen the sequence if symptoms return during recovery or the patient has other comorbidities that may affect recovery. The directing physician can shorten the timeline when appropriate. Regardless, no patient diagnosed with concussion should return to physical activity on the day of injury. An extended RTP progression may be necessary if the patient is held out for an extended amount of time and requires reconditioning for sport participation.
Table 4. .
Return-to-Play Progression
| Stagea |
Physical Activity |
| 1 | No activity |
| 2 | Light exercise: <70% age-predicted maximal heart rate |
| 3 | Sport-specific activities without the threat of contact from others |
| 4 | Noncontact training involving others, resistance training |
| 5 | Unrestricted training |
| 6 | Return to play |
Stages should be separated by at least 24 hours.7
Other Considerations
Equipment
It would seem natural that preventing concussion would include the appropriate use of protective equipment or other mechanisms. However, the literature to date does not support equipment as a means of concussion prevention. In a 2009 systematic review, Benson et al29 evaluated 51 studies of protective equipment (helmets, headgear, mouthguards, face shields) to determine if any form of protective equipment was useful in preventing sport-related concussion. Their results suggest that helmet use can reduce the risk of more serious head (eg, skull fracture) and brain (eg, subdural hematoma) injuries in recreational sports such as skiing, snowboarding, and bicycling. Yet the ability of these devices to prevent concussion was inconclusive.29 The authors also assessed the use of mouthguards and face shields and found no strong evidence to suggest that either device decreases concussion risk.29 Nonetheless, some published evidence in ice hockey indicates that, compared with a half-face shield, a full face shield offers a better fit and protection that may decrease the time lost from competition after a concussion.29
More specifically, no differences were noted in the incidence of concussion between American football players135,136 or Australian rules footballers137 wearing custom or noncustom mouthguards. No differences in concussion incidence were seen in rugby,138,139 ice hockey,140 or basketball141 players who did or did not wear mouthguards. In addition, researchers142 found no differences in neurocognitive impairment at the day-3 follow-up between athletes who reported wearing or not wearing a mouthguard at the time of concussion.
The use of protective headgear to decrease the risk of concussion in rugby is inconclusive. One group143 found a decrease in the risk of concussion among English premier rugby athletes who wore headgear; however, in 3 studies139,144,145 of youth or college rugby athletes, no association was noted between wearing headgear and decreased risk of concussion. Studies of headgear use in soccer have largely been laboratory based and focused on biomechanical variables.146–148 In 1 investigation,149 a small decrease in self-reported concussions was demonstrated in youth athletes wearing soccer headgear, but these results have not been replicated.
Pediatric Concussion
Sport-related concussion is a significant concern in the pediatric population. Data from the National Electronic Injury Surveillance System (NEISS) estimated that concussions in 8- to 19-year-olds resulted in more than 500 000 visits to the emergency department, with close to half (252 807 visits) resulting from a sport-related mechanism.150 Sport-related concussions –accounted for 58% of all emergency department visits in children (8–13 years old) and 46% of all concussions in adolescents (14–19 years old).150 Similarly, data from the National Hospital Ambulatory Medical Care Survey43 showed 144 000 emergency department visits for concussion in youth and adolescents (0–19 years old) over a 5-year period (2002–2006). Sport-related concussion was the most common mechanism, accounting for 30% of all concussions in persons between 5 and 19 years old.45 In high school athletes, Powell and Barber-Foss151 reported that AT-diagnosed concussions accounted for 5.5% of all sports injuries. More recently, data from High School Reporting Information Online (RIO) indicated that concussions in interscholastic athletes were responsible for 8.9% of all athletic injuries67 and that the overall concussion incidence rate according to RIO was 0.23 concussions per 1000 athlete exposures, with a game rate of 0.53 and a practice rate of 0.11 per 1000 athlete exposures.
Structural brain development occurs during childhood and adolescence with increased brain volume and connectivity, as reflected by increased white matter volume, which is apparent on magnetic resonance imaging.152,153 Younger athletes may be more vulnerable to concussion because of this structural immaturity, coupled with less myelination, thinner frontal and temporal bones, a greater head-to-body ratio, and weaker neck musculature.154–157 Furthermore, functional brain immaturity is present through early adulthood; the brain continues to mature in areas responsible for cognitive processing, such as attention and concentration, learning and memory, reasoning, and executive function.16,158 Thus, neurocognitive performance would be expected to change at least until the age of 20 years, requiring baseline levels of cognitive performance to be reassessed periodically, so that they can be compared with postinjury results.
The susceptibility of a child or adolescent to prolonged recovery after concussion may result from the fact that the developing functions of the immature brain are more vulnerable than established functions. Some have also postulated that injury to the brain might interfere with the complex biological processes needed for brain development.1,159–162 Concussed high school players took longer to recover from memory dysfunction than did concussed college players.36 Prolonged neurocognitive recovery has also been reported in other studies of high school athletes.163,164 Additionally, high school athletes with a history of 2 or more concussions demonstrated poorer cognitive recovery.163 However, to date, little evidence is available regarding postconcussion recovery in patients younger than high school age.
A primary concern of premature RTP among pediatric athletes is diffuse cerebral swelling with delayed catastrophic deterioration, commonly referred to as second-impact syndrome or malignant cerebral edema. The presence of second-impact syndrome has been debated,165,166 but in rare circumstances, cerebral swelling or edema can occur after injury to an immature brain.162,167,168 Although there may be controversy regarding the need for a second insult to cause the cerebral swelling, there is agreement that this diffuse cerebral swelling occurs more often in patients with immature brains.
The 2012 Zurich consensus statement on management of concussion in sport7 and the 2010 American Academy of Pediatrics' clinical report on sport-related concussion in children and adolescents169 recommended a multifaceted approach to concussion management in pediatric athletes. Yet, some special concerns are relevant to younger athletes. When assessing a concussed child or adolescent, it is important to obtain input from not only the patient but also from parents, health care providers, and teachers, as they may have additional information about the patient's preinjury and postinjury behavior that can be useful in the clinical evaluation and management plan.38
Assessing the patient's symptoms is advocated as a key aspect of concussion management. Numerous symptom checklists and scales have been developed for use in athletic populations,170 and children and adolescents can reliably report concussion-related symptoms.171–173 However, the Zurich consensus panel7 suggested that children younger than 10 years may report concussion symptoms differently from adults; therefore, age-appropriate symptom checklists may be needed to track symptoms after a suspected concussion. In light of this, the Health and Behavior Inventory –Child Version,174 was developed by the National Institutes of Health–National Institute of Neurological Disorders and Stroke to evaluate younger persons. The use of concussion-symptom scales is more appropriate for adolescents (ages 13–22 years) than for children (ages 5–12 years), and research has addressed validity as opposed to reliability.38 The addition of reliable and valid parental reports of postconcussion symptoms is an important adjunct to the report of the child or adolescent. However, in high school athletes, neurocognitive deficits may exist despite the resolution of self-report symptoms,36 suggesting that self-report symptoms should not be the only means of assessment.
Assessment of motor control and neurocognitive function is also important and may be useful in pediatric athletes.16,164,175 The method and timing of baseline assessments in children and adolescents require careful consideration because of the cognitive and neuromuscular maturation that occurs during this time.176–179 Hunt and Ferrara16 found that neurocognitive test scores differed between 9th- and 10th-grade students. Therefore, they recommended at least 2 baseline tests for high school athletes: the first as an incoming freshman and the second before sophomore year. A similar trend was noted with the Sport Concussion Assessment Tool-2 (SCAT-2): scores among 9th graders were lower than those among 11th and 12th graders.180 Lastly, improvements in neurocognitive performance were seen between the ages of 9 and 15 years, suggesting that baseline testing should be done every 6 months, or at least annually, until the age of 15.176 Although a person's own baseline measurements are the best values for postinjury comparisons, repeated baseline assessments may not be feasible because of administration time, cost, and effort. In these cases, using age-matched norms to supplement the clinical examination plus the patient's self-report and parental report of symptoms may be more cost effective.13
Despite the challenges of obtaining baseline neurocognitive or balance assessments in this younger age group, having baseline and postinjury neurocognitive scores can be valuable for managing potential school-related difficulties, such as focusing attention, learning and retaining new information, and managing multiple academic learning demands. The results of specific domain tests (eg, working memory, concentration, new learning and memory retention, and processing speed) can be useful in working with teachers and guidance counselors to develop strategies for successful academic outcomes. For example, temporary accommodations, including the use of written instructions, shorter assignments, and extended time for assignments, might be considered for students recovering from concussion.
Home Care
After a concussion diagnosis, a comprehensive medical management plan should be implemented that follows the institution's concussion policy and includes communication among all those involved. This plan should include the family (ie, patient and parents), school personnel (ie, teachers, administrators, counselors, coaches), school medical personnel (ie, AT, school nurse), and community referral sources (ie, team physician, other health care referral sources). Communication among all these groups is essential for appropriate management of a concussed athlete.
The home care plan should include frequent follow-up assessments and continued monitoring of concussion signs and symptoms.5,7 Patients and their parents or roommates should be provided with a list of signs and symptoms that would indicate a deteriorating condition and warrant immediate referral to the emergency department (Table 5). The patient, or a responsible person, should also be provided with a concussion instruction form (Appendix A) and instructed to follow up with the AT the next day he or she is at school.
Table 5. .
Observable Red-Flag Items That Warrant Immediate Referral to the Emergency Department via Emergency Medical Transport
| Decreasing level of consciousness |
| Increasing confusion |
| Increasing irritability |
| Loss of or fluctuating level of consciousness |
| Numbness in the arms or legs |
| Pupils becoming unequal in size |
| Repeated vomiting |
| Seizures |
| Slurred speech or inability to speak |
| Inability to recognize people or places |
| Worsening headache |
Medications and Diet
Limited evidence suggests that any medication is beneficial in accelerating the concussion-recovery process. All current medications should be reviewed by the physician, and concussed patients should avoid taking medications containing aspirin or nonsteroidal anti-inflammatory drugs. These medications are known to decrease platelet function and may increase intracranial bleeding, mask the severity and duration of symptoms, and possibly lead to a more severe injury. Acetaminophen may be used sparingly to ease headaches after concussion. During the acute stage of injury, the patient should avoid ingesting other substances that can affect central nervous system function, including alcohol and narcotics, and should be instructed to eat a well-balanced, nutritious diet.
During the subacute stage of recovery, the physician may prescribe medications to reduce specific symptoms, such as headache, sleep disturbances, or anxiety, or to improve symptom resolution.7,45 Additionally, medication may be prescribed if the symptoms are affecting broader aspects of the person's life such that the potential benefit of the medication is greater than the possible risks.45 Pharmacologic management of sport-related concussion should be directed only by those physicians with experience treating concussive injuries who are able to justify the benefit-to-risk ratio. One important consideration with respect to postconcussion medication use is that the patient should be asymptomatic when not on the medication before beginning an RTP progression.7
Rest
A concussed patient who returns home after the sport event should be monitored by a responsible adult and should have a good night's rest. In general, the patient does not need to be awakened during the night unless he or she experienced loss of consciousness, prolonged periods of amnesia, or significant symptoms before going to bed.5 Should the AT or physician prescribe nighttime waking, the responsible adult should be provided with instructions on when to wake the patient and what to observe during periods of waking.
During the acute recovery period, physical rest and cognitive rest are indicated while the patient is symptomatic.7,28,39,42 While symptomatic, the patient should avoid physical exertion, including physical education classes and recreational activities. Activities of daily living that do not exacerbate symptoms may be beneficial to the patient's recovery and should be allowed.130 When mental activities exacerbate symptoms, cognitive rest, including temporary academic accommodations (see the next paragraph), should be part of the concussion-management plan.7,28,39,42 Alterations in the amount of cognitive and physical rest should be made on an individual basis as the patient's symptom reports and adjunct assessment scores (ie, cognitive test scores) change during recovery.
The concept of cognitive rest was initially presented in the Prague consensus document181 and was reiterated in the Zurich consensus statement7 and the American Academy of Pediatrics Clinical Report.169 Cognitive rest refers to limiting academic and cognitive stressors in activities of daily living and school activities while the patient recovers from the concussion. Cognitive rest is part of a spectrum that ranges from very limited cognitive activity (ie, absent from school) to full cognitive activity (ie, full school attendance). The goal of cognitive rest is to keep the brain from engaging in mental challenges that will increase symptoms during the postconcussion stage.7,42,179 Most concussed patients require some amount of cognitive rest to ensure resolution of symptoms and recovery from the concussion. The type and amount of cognitive rest are individualized but may take the form of limiting mental exertion, including reading, writing, mathematical computation, and computer work. Limiting social activities requiring concentrated cognitive activity should also be considered, such as watching television, text messaging, playing video games, and listening to loud music. Communication among the medical providers, parents and patient, and school personnel (such as the school nurse, counselors, administrators, and teachers) is crucial to providing temporary accommodations that allow cognitive rest.42 To date, however, little empirical evidence supports the utility and efficacy of cognitive rest on recovery outcomes after concussion. Moderate levels of supervised exertion (eg, participating in school and light physical activity) during recovery were associated with better visual memory and reaction time outcomes and may be beneficial to recovery.130
Multiple Concussions
Similar to other types of injuries, the best predictor of subsequent concussion is a history of at least 1 concussion. Among collegiate football players, patients who self-reported 3 or more concussions were 3.5 times more likely to sustain a subsequent injury than players with no concussion history, whereas those with 2 concussions were 2.8 times more likely.46 An increased risk for subsequent concussions in high school athletes with a history of concussion has also been reported. In a prospective investigation,182 football players with a concussion history were nearly 3 times more likely to sustain another injury, whereas nonfootball players were 1.2 times more likely. Therefore, current recommendations7,47 suggest that modifying factors, including repeated concussions over time, multiple concussions within a short time frame, sustaining concussions with lessening force, or increasing severity of injury, should result in a more conservative management approach. Proper management of a concussion will reduce the risk of a repeat injury.183
Second-Impact Syndrome
A primary concern of premature RTP by pediatric athletes is second-impact syndrome, or malignant cerebral edema, which occurs after a second impact while the patient is still symptomatic from a previous injury to the head or body. The condition is characterized by diffuse cerebral swelling with catastrophic deterioration.1,48–50
Long-Term Consequences
The relationship between concussion and long-term cognitive health is not clear. A number of cross-sectional investigations184–186 have shown no chronic changes in neurocognitive functioning after concussion in a young adult population. Others, however, have shown changes to neurocognitive functioning,187,188 brain function,189–191 neuroelectrical activity,192–195 and motor control.196,197 Yet none of these authors reported an association between the declines and clinical impairment. Results of surveys51–53,198 of former professional athletes, however, have suggested the potential for cumulative concussive and subconcussive impacts over an athlete's playing career to be associated with late-life cognitive impairment, depression, and chronic traumatic encephalopathy. Indeed, retired professional football players with a self-reported history of 3 or more concussions were 3 times more likely and those with a history of 1 or 2 concussions were 1.5 times more likely to be diagnosed with depression than their peers who did not report concussions.51 Similarly, a preliminary report52 has associated retired professional football players who sustained 3 or more concussions with mild cognitive impairment and self-reported significant memory impairments. Others53,199,200 have speculated that exposure to concussive and subconcussive impacts may lead to chronic traumatic encephalopathy, a progressive neurodegenerative disorder that results in a buildup of tau proteins in the brain. In large part, persons reporting clinical impairments thought to be associated with concussion are former professional athletes with a uniquely high level of exposure to contact and collision sports that may have been moderated by a number of other intrinsic (eg, genetic profile) and extrinsic (eg, lifestyle) factors.201 In addition, longitudinal research that can directly associate concussive and subconcussive impacts with cognitive health, while controlling for normal age-related declines and other factors, has not been completed. As such, the relationship among concussion, subconcussive impacts, and long-term brain health is not clear. These studies are viewed as preliminary; additional research is needed to adequately address this association.
SUMMARY
This document is intended to provide clinical ATs with best-practice guidelines for concussion management based on recommendations derived from the most recent research. The best approach to concussion management involves the entire sports medicine team. The AT should spearhead the development of a detailed written plan outlining the concussion-management strategy and share it with administrators and coaches. The plan should include a baseline evaluation of athletes, including a neurologic history with symptoms and physical examination and objective measures of neurocognitive performance and motor control. Once the concussion diagnosis has been made, the patient should be immediately removed from further participation for at least 24 hours. Follow-up testing, using the same protocol as the baseline examination, can aid in determining when to start the return to physical activity after the patient is cleared by a physician or designate. Lastly, although most concussions resolve in a relatively short time frame, patients who are young, who have had multiple concussions, or who have premorbid factors may require additional attention. The AT should be familiar with these concerns, as well as the potential for long-term consequences, and account for them in the concussion-management plan.
ACKNOWLEDGMENTS
We gratefully acknowledge the efforts of Barry P. Boden, MD; Randall Cohen, DPT, ATC; Michael W. Collins, PhD; Ruben Echemendia, PhD: Michael S. Ferrara, PhD, ATC, FNATA; James S. Galloway, ATC; Margot Putukian, MD; and the Pronouncements Committee in the review of this document.
Appendix A. Sample Postconcussion Home Care Instructions
Appendix B. Sample Information for Patients, Parents, and Legal Custodians About Concussion
DISCLAIMER
The NATA and NATA Foundation publish position statements as a service to promote the awareness of certain issues to their members. The information contained in the position statement is neither exhaustive nor exclusive to all circumstances or individuals. Variables such as institutional human resource guidelines, state or federal statutes, rules, or regulations, as well as regional environmental conditions, may impact the relevance and implementation of these recommendations. The NATA and NATA Foundation advise members and others to carefully and independently consider each of the recommendations (including the applicability of same to any particular circumstance or individual). The position statement should not be relied upon as an independent basis for care but rather as a resource available to NATA members or others. Moreover, no opinion is expressed herein regarding the quality of care that adheres to or differs from the NATA and NATA Foundation position statements. The NATA and NATA Foundation reserve the right to rescind or modify its position statements at any time.
REFERENCES
- 1.Giza CC, Hovda DA. The neurometabolic cascade of concussion. J Athl Train. 2001;36(3):228–235. [PMC free article] [PubMed] [Google Scholar]
- 2.Vagnozzi R, Signoretti S, Cristofori L, et al. Assessment of metabolic brain damage and recovery following mild traumatic brain injury: a multicentre, proton magnetic resonance spectroscopic study in concussed patients. Brain. 2010;133(11):3232–3242. doi: 10.1093/brain/awq200. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤ 19 years, United States, 2001–2009. MMWR Morb Mortal Wkly Rep. 2011;60(39):1337–1342. [PubMed] [Google Scholar]
- 4.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–378. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Guskiewicz KM, Bruce SL, Cantu RC, et al. National Athletic Trainers' Association position statement: management of sport-related concussion. J Athl Train. 2004;39(3):280–297. [PMC free article] [PubMed] [Google Scholar]
- 6.American Academy of Neurology. Practice parameter: the management of concussion in sports (summary statement) Report of the Quality Standards Subcommittee. Neurology. 1997;48(3):581–585. doi: 10.1212/wnl.48.3.581. [DOI] [PubMed] [Google Scholar]
- 7.McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013;47(5):250–258. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- 8.Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. Am Fam Physician. 2004;69(3):548–556. [PubMed] [Google Scholar]
- 9.Lovell MR, Collins MW, Iverson GL, Johnston KM, Bradley JP. Grade 1 or “ding” concussions in high school athletes. Am J Sports Med. 2004;32(1):47–54. doi: 10.1177/0363546503260723. [DOI] [PubMed] [Google Scholar]
- 10.Valovich Mcleod TC, Schwartz C, Bay RC. Sport-related concussion misunderstandings among youth coaches. Clin J Sport Med. 2007;17(2):140–142. doi: 10.1097/JSM.0b013e31803212ae. [DOI] [PubMed] [Google Scholar]
- 11.Sarmiento K, Mitchko J, Klein C, Wong S. Evaluation of the Centers for Disease Control and Prevention's concussion initiative for high school coaches: “Heads Up: Concussion in High School Sports.”. J Sch Health. 2010;80(3):112–118. doi: 10.1111/j.1746-1561.2010.00491.x. [DOI] [PubMed] [Google Scholar]
- 12.Glang A, Koester MC, Beaver SV, Clay JE, McLaughlin KA. Online training in sports concussion for youth sports coaches. Int J Sports Sci Coach. 2010;5(1):1–12. doi: 10.1260/1747-9541.5.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmidt JD, Register-Mihalik JK, Mihalik JP, Kerr ZY, Guskiewicz KM. Identifying impairments after concussion: normative data versus individualized baselines. Med Sci Sports Exerc. 2012;44(9):1621–1628. doi: 10.1249/MSS.0b013e318258a9fb. [DOI] [PubMed] [Google Scholar]
- 14.Randolph C. Baseline neuropsychological testing in managing sport-related concussion: does it modify risk? Curr Sports Med Rep. 2011;10(1):21–26. doi: 10.1249/JSR.0b013e318207831d. [DOI] [PubMed] [Google Scholar]
- 15.Yakovlev PI, Lecours AR. The myelogenetic cycles of regional maturation of the brain. In: Minkowski A, editor. Regional Development of the Brain in Early Life. Philadelphia, PA: FA Davis;; 1967. pp. 3–70. In. ed. [Google Scholar]
- 16.Hunt TN, Ferrara MS. Age-related differences in neuropsychological testing among high school athletes. J Athl Train. 2009;44(4):405–409. doi: 10.4085/1062-6050-44.4.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fields RD. White matter in learning, cognition and psychiatric disorders. Trends Neurosci. 2008;31(7):361–370. doi: 10.1016/j.tins.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Broglio SP, Puetz TW. The effect of sport concussion on neurocognitive function, self-report symptoms, and postural control: a meta-analysis. Sports Med. 2008;38(1):53–67. doi: 10.2165/00007256-200838010-00005. [DOI] [PubMed] [Google Scholar]
- 19.Broglio SP, Macciocchi SN, Ferrara MS. Sensitivity of the concussion assessment battery. Neurosurgery. 2007;60(6):1050–1057. doi: 10.1227/01.NEU.0000255479.90999.C0. [DOI] [PubMed] [Google Scholar]
- 20.McCrea M, Barr WB, Guskiewicz K, et al. Standard regression-based methods for measuring recovery after sport-related concussion. J Int Neuropsychol Soc. 2005;11(1):58–69. doi: 10.1017/S1355617705050083. [DOI] [PubMed] [Google Scholar]
- 21.Moser RS, Schatz P, Neidzwski K, Ott SD. Group versus individual administration affects baseline neurocognitive test performance. Am J Sports Med. 2011;39(11):2325–2330. doi: 10.1177/0363546511417114. [DOI] [PubMed] [Google Scholar]
- 22.McCrea M. Standardized mental status testing on the sideline after sport-related concussion. J Athl Train. 2001;36(3):274–279. [PMC free article] [PubMed] [Google Scholar]
- 23.McCrea M. Standardized mental status assessment of sports concussion. Clin J Sport Med. 2001;11(3):176–181. doi: 10.1097/00042752-200107000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Ragan BG, Kang M. Measurement issues in concussion testing. Athl Ther Today. 2007;12(5):2–6. [Google Scholar]
- 25.Moser RS, Iverson GL, Echemendia RJ, et al. Neuropsychological evaluation in the diagnosis and management of sports-related concussion. Arch Clin Neuropsychol. 2007;22(8):909–916. doi: 10.1016/j.acn.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 26.Oliaro S, Anderson S, Hooker D. Management of cerebral concussion in sports: the athletic trainer's perspective. J Athl Train. 2001;36(3):257–262. [PMC free article] [PubMed] [Google Scholar]
- 27.Halstead DP. Performance testing updates in head, face, and eye protection. J Athl Train. 2001;36(3):322–327. [PMC free article] [PubMed] [Google Scholar]
- 28.Herring SA, Cantu RC, Guskiewicz KM, et al. American College of Sports Medicine. Concussion (mild traumatic brain injury) and the team physician: a consensus statement. Med Sci Sports Exerc. 2011;43(12):2412–2422. doi: 10.1249/MSS.0b013e3182342e64. 2011 update. [DOI] [PubMed] [Google Scholar]
- 29.Benson BW, Hamilton GM, Meeuwisse WH, McCrory P, Dvorak J. Is protective equipment useful in preventing concussion? A systematic review of the literature. Br J Sports Med. 2009;43(suppl 1):i56–i67. doi: 10.1136/bjsm.2009.058271. [DOI] [PubMed] [Google Scholar]
- 30.Hagel BE, Pless IB, Goulet C, Platt RW, Robitaille Y. Effectiveness of helmets in skiers and snowboarders: case-control and case crossover study. BMJ. 2005;330(7486):281. doi: 10.1136/bmj.38314.480035.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mueller BA, Cummings P, Rivara FP, Brooks MA, Terasaki RD. Injuries of the head, face, and neck in relation to ski helmet use. Epidemiology. 2008;19(2):270–276. doi: 10.1097/EDE.0b013e318163567c. [DOI] [PubMed] [Google Scholar]
- 32.Sulheim S, Holme I, Ekeland A, Bahr R. Helmet use and risk of head injuries in alpine skiers and snowboarders. JAMA. 2006;295(8):919–924. doi: 10.1001/jama.295.8.919. [DOI] [PubMed] [Google Scholar]
- 33.Curnow WJ. Bicycle helmets and public health in Australia. Health Promot J Austr. 2008;19(1):10–15. doi: 10.1071/he08010. [DOI] [PubMed] [Google Scholar]
- 34.Hewson PJ. Cycle helmets and road casualties in the UK. Traffic Inj Prev. 2005;6(2):127–134. doi: 10.1080/15389580590931590. [DOI] [PubMed] [Google Scholar]
- 35.Davidson JA. Epidemiology and outcome of bicycle injuries presenting to an emergency department in the United Kingdom. Eur J Emerg Med. 2005;12(1):24–29. doi: 10.1097/00063110-200502000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Field M, Collins MW, Lovell MR, Maroon J. Does age play a role in recovery from sports-related concussion? A comparison of high school and collegiate athletes. J Pediatr. 2003;142(5):546–553. doi: 10.1067/mpd.2003.190. [DOI] [PubMed] [Google Scholar]
- 37.Pellman EJ, Lovell MR, Viano DC, Casson IR. Concussion in professional football: recovery of NFL and high school athletes assessed by computerized neuropsychological testing—part 12. Neurosurgery. 2006;58(2):263–274. doi: 10.1227/01.NEU.0000200272.56192.62. [DOI] [PubMed] [Google Scholar]
- 38.Gioia GA, Schneider JC, Vaughan CG, Isquith PK. Which symptom assessments and approaches are uniquely appropriate for paediatric concussion? Br J Sports Med. 2009;43(suppl 1):i13–i22. doi: 10.1136/bjsm.2009.058255. [DOI] [PubMed] [Google Scholar]
- 39.Sady MD, Vaughan CG, Gioia GA. School and the concussed youth: recommendations for concussion education and management. Phys Med Rehabil Clin N Am. 2011;22(4):701–719. doi: 10.1016/j.pmr.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yeates KO, Kaizer E, Rusin J, et al. Reliable change in postconcussive symptoms and its functional consequences among children with mild traumatic brain injury. Arch Pediatr Adolesc Med. 2012;166(7):615–622. doi: 10.1001/archpediatrics.2011.1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Valovich-Mcleod TC, Bay RC, Lam KC, Chhabra A. Representative baseline values on the Sport Concussion Assessment Tool 2 (SCAT2) in adolescent athletes vary by gender, grade, and concussion history. Am J Sports Med. 2012;40(4):927–933. doi: 10.1177/0363546511431573. [DOI] [PubMed] [Google Scholar]
- 42.Valovich McLeod TC, Gioia GA. Cognitive rest: the often neglected aspect of concussion management. Athl Ther Today. 2010;15(2):1–3. [Google Scholar]
- 43.Casa DJ, Guskiewicz KM, Anderson SA, et al. National Athletic Trainers' Association position statement: preventing sudden death in sports. J Athl Train. 2012;47(1):96–118. doi: 10.4085/1062-6050-47.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McCrory P. Should we treat concussion pharmacologically? The need for evidence based pharmacological treatment for the concussed athlete. Br J Sports Med. 2002;36(1):3–5. doi: 10.1136/bjsm.36.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 45.Meehan WP. Medical therapies for concussion. Clin Sports Med. 2011;30(1):115–124. doi: 10.1016/j.csm.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA concussion study. JAMA. 2003;290(19):2549–2555. doi: 10.1001/jama.290.19.2549. [DOI] [PubMed] [Google Scholar]
- 47.Herring SA, Cantu RC, Guskiewicz KM, et al. American College of Sports Medicine. Concussion (mild traumatic brain injury) and the team physician: a consensus statement—2011 update. Med Sci Sports Exerc. 2011;43(12):2412–2422. doi: 10.1249/MSS.0b013e3182342e64. [DOI] [PubMed] [Google Scholar]
- 48.Saunders RL, Harbaugh RE. The second impact in catastrophic contact-sports head trauma. JAMA. 1984;252(4):538–539. [PubMed] [Google Scholar]
- 49.Cantu RC, Voy R. Second impact syndrome: a risk in any contact sport. Phys Sportsmed. 1995;23(6):27–28. doi: 10.1080/00913847.1995.11947799. 31. [DOI] [PubMed] [Google Scholar]
- 50.Bruce DA, Alavi A, Bilaniuk L, Dolinskas C, Obrist W, Uzzell B. Diffuse cerebral swelling following head injuries in children: the syndrome of “malignant brain edema.”. J Neurosurg. 1981;54(2):170–178. doi: 10.3171/jns.1981.54.2.0170. [DOI] [PubMed] [Google Scholar]
- 51.Guskiewicz KM, Marshall SW, Bailes J, et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. 2007;39(6):903–909. doi: 10.1249/mss.0b013e3180383da5. [DOI] [PubMed] [Google Scholar]
- 52.Guskiewicz KM, Marshall SW, Bailes J, et al. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery. 2005;57(4):719–726. doi: 10.1093/neurosurgery/57.4.719. [DOI] [PubMed] [Google Scholar]
- 53.McKee AC, Cantu RC, Nowinski CJ, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68(7):709–735. doi: 10.1097/NEN.0b013e3181a9d503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Covassin T, Elbin RJ, Sarmiento K. Educating coaches about concussion in sports: evaluation of the CDC's “Heads Up: Concussion in Youth Sports” initiative. J Sch Health. 2012;82(5):233–238. doi: 10.1111/j.1746-1561.2012.00692.x. [DOI] [PubMed] [Google Scholar]
- 55.Chrisman SP, Schiff MA, Rivara FP. Physician concussion knowledge and the effect of mailing the CDC's “Heads Up” toolkit. Clin Pediatr (Phila) 2011;50(11):1031–1039. doi: 10.1177/0009922811410970. [DOI] [PubMed] [Google Scholar]
- 56.Sawyer RJ, Hamdallah M, White D, Pruzan M, Mitchko J, Huitric M. High school coaches' assessments, intentions to use, and use of a concussion prevention toolkit: Centers for Disease Control and Prevention's “Heads Up: Concussion In High School Sports.”. Health Promot Pract. 2010;11(1):34–43. doi: 10.1177/1524839907309377. [DOI] [PubMed] [Google Scholar]
- 57.McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004;14(1):13–17. doi: 10.1097/00042752-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 58.Sefton JM, Pirog K, Capitao A, Harackiewicz D, Cordova ML. An examination of factors that influence knowledge and reporting of mild brain injuries in collegiate football. J Athl Train. 2004;39(suppl):S52–S53. [Google Scholar]
- 59.Sye G, Sullivan SJ, McCrory P. High school rugby players' understanding of concussion and return to play guidelines. Br J Sports Med. 2006;40(12):1003–1005. doi: 10.1136/bjsm.2005.020511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Goodman D, Bradley NL, Paras B, Williamson IJ, Bizzochi J. Video gaming promotes concussion knowledge acquisition in youth hockey players. J Adolesc. 2006;29(3):351–360. doi: 10.1016/j.adolescence.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 61.Bramley H, Patrick K, Lehman E, Silvis M. High school soccer players with concussion education are more likely to notify their coach of a suspected concussion. Clin Pediatr (Phila) 2012;51(4):332–336. doi: 10.1177/0009922811425233. [DOI] [PubMed] [Google Scholar]
- 62.Coghlin CJ, Myles BD, Howitt SD. The ability of parents to accurately report concussion occurrence in their bantam-aged minor hockey league children. J Can Chiropr Assoc. 2009;53(4):233–250. [PMC free article] [PubMed] [Google Scholar]
- 63.Sullivan SJ, Bourne L, Choie S, et al. Understanding of sport concussion by the parents of young rugby players: a pilot study. Clin J Sport Med. 2009;19(3):228–230. doi: 10.1097/JSM.0b013e3181a41e43. [DOI] [PubMed] [Google Scholar]
- 64.O'Donoghue EM, Onate JA, Van Lunen B, Peterson CL. Assessment of high school coaches' knowledge of sport-related concussions. Athl Train Sports Health. 2009;1(3):120–132. [Google Scholar]
- 65.McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA concussion study. JAMA. 2003;290(19):2556–2563. doi: 10.1001/jama.290.19.2556. [DOI] [PubMed] [Google Scholar]
- 66.Lau BC, Kontos AP, Collins MW, Mucha A, Lovell MR. Which on-field signs/symptoms predict protracted recovery from sport-related concussion among high school football players. Am J Sports Med. 2011;39(11):2311–2318. doi: 10.1177/0363546511410655. [DOI] [PubMed] [Google Scholar]
- 67.Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42(4):495–503. [PMC free article] [PubMed] [Google Scholar]
- 68.Wood RL, McCabe M, Dawkins J. The role of anxiety sensitivity in symptom perception after minor head injury: an exploratory study. Brain Inj. 2011;25(13–14):1296–1299. doi: 10.3109/02699052.2011.624569. [DOI] [PubMed] [Google Scholar]
- 69.Plevretes v La Salle University. 2007):07–5186. (ED PA. [Google Scholar]
- 70.Kampmeier v Nyquist. 1997) 553 F2d 296 (2nd Cir. [Google Scholar]
- 71.Grube v Bethlehem Area School District. 1982) 550 F Supp 418 (ED PA. [Google Scholar]
- 72.Wright v Columbia University. 1981) 520 F Supp 789 (ED PA. [Google Scholar]
- 73.Poole v South Plainfield Board of Education. 1980) 490 F Supp 948 (D NJ. [Google Scholar]
- 74.Quandt EF, Mitten MJ, Black JS. Legal liability in covering athletic events. Sports Health. 2009;1(1):84–90. doi: 10.1177/1941738108327530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Osborne B. Principles of liability for athletic trainers: managing sport-related concussion. J Athl Train. 2001;36(3):316–321. [PMC free article] [PubMed] [Google Scholar]
- 76.Dobbs DB. Torts and Compensation. 2nd ed. St Paul, MN: West Publishing Co;; 1993. [Google Scholar]
- 77.Guskiewicz KM, Pachman SE. Management of sport-related brain injuries: preventing poor outcomes and minimizing the risk for legal liabilities. Athl Train Sports Health. 2010;2(6):248–252. [Google Scholar]
- 78.Ray R. Management Strategies in Athletic Training. 3rd ed. Champaign, IL: Human Kinetics;; 2005. [Google Scholar]
- 79.Gill v Tamalpais Union High School District. 2008 A112705. (Cal Ct App) [Google Scholar]
- 80.Pinson v Tennessee. 1995 WL 739820. (Tenn Ct App) [Google Scholar]
- 81.Melka v Orthopaedic Associates of Wisconsin. 2008) 06CV2136 (Wisc Cir Ct. [Google Scholar]
- 82.National Collegiate Athletic Association Injury Surveillance Summary for 15 sports: 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):165–319. [Google Scholar]
- 83.Elbin RJ, Schatz P, Covassin T. One-year test-retest reliability of the online version of ImPACT in high school athletes. Am J Sports Med. 2011;39(11):2319–2324. doi: 10.1177/0363546511417173. [DOI] [PubMed] [Google Scholar]
- 84.Collie A, Maruff P, Makdissi M, McCrory P, McStephen M, Darby D. CogSport: reliability and correlation with conventional cognitive tests used in postconcussion medical evaluations. Clin J Sport Med. 2003;13(1):28–32. doi: 10.1097/00042752-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 85.Iverson GL, Lovell MR, Podell K, Collins MW. Paper presented at: 31st Annual Conference of the International Neuropsychological Society; February 5–8. Honolulu, HI: 2003. Reliability and validity of ImPACT. [Google Scholar]
- 86.Broglio SP, Ferrara MS, Macciocchi SN, Baumgartner TA, Elliott R. Test-retest reliability of computerized concussion assessment programs. J Athl Train. 2007;42(4):509–514. [PMC free article] [PubMed] [Google Scholar]
- 87.Schatz P. Long-term test-retest reliability of baseline cognitive assessments using ImPACT. Am J Sports Med. 2009;38(1):47–53. doi: 10.1177/0363546509343805. [DOI] [PubMed] [Google Scholar]
- 88.Grindel SH. The use, abuse, and future of neuropsychologic testing in mild traumatic brain injury. Curr Sports Med Rep. 2006;5(1):9–14. doi: 10.1097/01.csmr.0000306513.79430.03. [DOI] [PubMed] [Google Scholar]
- 89.Echemendia RJ, Herring S, Bailes J. Who should conduct and interpret the neuropsychological assessment in sports-related concussion? Br J Sports Med. 2009;43(suppl 1):i32–i35. doi: 10.1136/bjsm.2009.058164. [DOI] [PubMed] [Google Scholar]
- 90.Iverson GL, Brooks BL, Ashton VL, Lange RT. Interview versus questionnaire symptom reporting in people with the postconcussion syndrome. J Head Trauma Rehabil. 2010;25(1):23–30. doi: 10.1097/HTR.0b013e3181b4b6ab. [DOI] [PubMed] [Google Scholar]
- 91.Patel AV, Mihalik JP, Notebaert AJ, Guskiewicz KM, Prentice WE. Neuropsychological performance, postural stability, and symptoms after dehydration. J Athl Train. 2007;42(1):66–75. [PMC free article] [PubMed] [Google Scholar]
- 92.Williams SJ, Nukada H. Sport and exercise headache, part 2: diagnosis and classification. Br J Sports Med. 1994;28(2):96–100. doi: 10.1136/bjsm.28.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sabin MJ, Van Boxtel BA, Nohren MW, Broglio SP. Presence of headache does not influence sideline neurostatus or balance in high school football athletes. Clin J Sport Med. 2011;21(5):411–415. doi: 10.1097/JSM.0b013e318223f3a4. [DOI] [PubMed] [Google Scholar]
- 94.Piland SG, Motl RW, Ferrara MS, Peterson CL. Evidence for the factorial and construct validity of a self-report concussion symptoms scale. J Athl Train. 2003;38(2):104–112. [PMC free article] [PubMed] [Google Scholar]
- 95.Randolph C, Millis S, Barr WB, et al. Concussion symptom inventory: an empirically derived scale for monitoring resolution of symptoms following sport-related concussion. Arch Clin Neuropsychol. 2009;24(3):219–229. doi: 10.1093/arclin/acp025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Catena RD, Van Donkelaar P, Chou LS. Cognitive task effects on gait stability following concussion. Exp Brain Res. 2007;176(1):23–31. doi: 10.1007/s00221-006-0596-2. [DOI] [PubMed] [Google Scholar]
- 97.Parker TM, Osternig LR, Van Donkelaar P, Chou LS. Gait stability following concussion. Med Sci Sports Exerc. 2006;38(6):1032–1040. doi: 10.1249/01.mss.0000222828.56982.a4. [DOI] [PubMed] [Google Scholar]
- 98.Guskiewicz KM, Riemann BL, Perrin DH, Nashner LM. Alternative approaches to the assessment of mild head injury in athletes. Med Sci Sports Exerc. 1997;29(suppl 7):S213–S221. doi: 10.1097/00005768-199707001-00003. [DOI] [PubMed] [Google Scholar]
- 99.Peterson CL, Ferrara MS, Mrazik M, Piland S, Elliot R. Evaluation of neuropsychological domain scores and postural stability following cerebral concussion in sports. Clin J Sport Med. 2003;13(4):230–237. doi: 10.1097/00042752-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 100.Guskiewicz KM, Ross SE, Marshall SW. Postural stability and neuropsychological deficits after concussion in collegiate athletes. J Athl Train. 2001;36(3):263–273. [PMC free article] [PubMed] [Google Scholar]
- 101.De Monte VE, Geffen GM, May CR, McFarland K, Heath P, Neralic M. The acute effects of mild traumatic brain injury on finger tapping with and without word repetition. J Clin Exp Neuropsychol. 2005;27(2):224–239. doi: 10.1080/13803390490515766. [DOI] [PubMed] [Google Scholar]
- 102.Broglio SP, Ferrara MS, Sopiarz K, Kelly MS. Reliable change of the sensory organization test. Clin J Sport Med. 2008;18(2):148–154. doi: 10.1097/JSM.0b013e318164f42a. [DOI] [PubMed] [Google Scholar]
- 103.Riemann BL, Guskiewicz KM. Effects of mild head injury on postural stability as measured through clinical balance testing. J Athl Train. 2000;35(1):19–25. [PMC free article] [PubMed] [Google Scholar]
- 104.Riemann BL, Guskiewicz KM, Shields EW. Relationship between clinical and forceplate measures of postural stability. J Sport Rehabil. 1999;8(2):71–82. [Google Scholar]
- 105.Broglio SP, Zhu W, Sopiarz K, Park Y. Generalizability theory analysis of balance error scoring system reliability in healthy young adults. J Athl Train. 2009;44(5):497–502. doi: 10.4085/1062-6050-44.5.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Valovich TC, Perrin DH, Gansneder BM. Repeat administration elicits a practice effect with the Balance Error Scoring System but not with the Standardized Assessment of Concussion in high school athletes. J Athl Train. 2003;38(1):51–56. [PMC free article] [PubMed] [Google Scholar]
- 107.Fox ZG, Mihalik JP, Blackburn JT, Battaglini CL, Guskiewicz KM. Return of postural control to baseline after anaerobic and aerobic exercise protocols. J Athl Train. 2008;43(5):456–463. doi: 10.4085/1062-6050-43.5.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Broglio SP, Monk A, Sopiarz K, Cooper ER. The influence of ankle support on postural control. J Sci Med Sport. 2009;12(3):388–392. doi: 10.1016/j.jsams.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 109.Susco TM. Valovich McLeod TC, Gansneder BM, Shultz SJ. Balance recovers within 20 minutes after exertion as measured by the Balance Error Scoring System. J Athl Train. 2004;39(3):241–246. [PMC free article] [PubMed] [Google Scholar]
- 110.Wilkins JC. Valovich McLeod TC, Perrin DH, Gansneder BM. Performance on the Balance Error Scoring System decreases after fatigue. J Athl Train. 2004;39(2):156–161. [PMC free article] [PubMed] [Google Scholar]
- 111.Maddocks DL, Dicker GD, Saling MM. The assessment of orientation following concussion in athletes. Clin J Sport Med. 1995;5(1):32–35. doi: 10.1097/00042752-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 112.Aubry M, Cantu R, Dvorak J, et al. Summary and agreement statement of the first International Conference on Concussion in Sport, Vienna 2001: recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br J Sports Med. 2002;36(1):6–10. doi: 10.1136/bjsm.36.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Schatz P, Pardini JE, Lovell MR, Collins MW, Podell K. Sensitivity and specificity of the ImPACT test battery for concussion in athletes. Arch Clin Neuropsychol. 2006;21(1):91–99. doi: 10.1016/j.acn.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 114.Randolph C, McCrea M, Barr WB. Is neuropsychological testing useful in the management of sport-related concussion? J Athl Train. 2005;40(3):139–152. [PMC free article] [PubMed] [Google Scholar]
- 115.Van Kampen DA, Lovell MR, Pardini JE, Collins MW, Fu FH. The “value added” of neurocognitive testing after sports-related concussion. Am J Sports Med. 2006;34(10):1630–1635. doi: 10.1177/0363546506288677. [DOI] [PubMed] [Google Scholar]
- 116.Maruff P, Thomas E, Cysique L, et al. Validity of the CogState brief battery: relationship to standardized tests and sensitivity to cognitive impairment in mild traumatic brain injury, schizophrenia, and AIDS dementia complex. Arch Clin Neuropsychol. 2009;24(2):165–178. doi: 10.1093/arclin/acp010. [DOI] [PubMed] [Google Scholar]
- 117.Schatz P, Moser RS, Solomon GS, Ott SD, Karpf R. Prevalence of invalid computerized baseline neurocognitive test results in high school and collegiate athletes. J Athl Train. 2012;47(3):289–296. doi: 10.4085/1062-6050-47.3.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Broglio SP, Macciocchi SN, Ferrara MS. Neurocognitive performance of concussed athletes when symptom free. J Athl Train. 2007;42(4):504–508. [PMC free article] [PubMed] [Google Scholar]
- 119.Fazio VC, Lovell MR, Pardini JE, Collins MW. The relation between post concussion symptoms and neurocognitive performance in concussed athletes. NeuroRehabilitation. 2007;22(3):207–216. [PubMed] [Google Scholar]
- 120.Broglio SP, Guskiewicz KM. Concussion in sports: the sideline assessment. Sports Health. 2009;1(5):361–369. doi: 10.1177/1941738109343158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Guskiewicz KM, Broglio SP. Sport-related concussion: on-field and sideline assessment. Phys Med Rehabil Clin N Am. 2011;22(4):603–617. doi: 10.1016/j.pmr.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 122.Gonzalez PG, Walker MT. Imaging modalities in mild traumatic brain injury and sports concussion. PM R. 2011;3(10 suppl 2):S413–S424. doi: 10.1016/j.pmrj.2011.08.536. [DOI] [PubMed] [Google Scholar]
- 123.Vagnozzi R, Signoretti S, Tavazzi B, et al. Temporal window of metabolic brain vulnerability to concussion: a pilot 1H-magnetic resonance spectroscopy study in concussed athletes, part III. Neurosurgery. 2008;62(6):1286–1295. doi: 10.1227/01.neu.0000333300.34189.74. [DOI] [PubMed] [Google Scholar]
- 124.Undén J, Romner B. Can low serum levels of S100B predict normal CT findings after minor head injury in adults? An evidence-based review and meta-analysis. J Head Trauma Rehabil. 2010;25(4):228–240. doi: 10.1097/HTR.0b013e3181e57e22. [DOI] [PubMed] [Google Scholar]
- 125.Greenwald RM, Gwin JT, Chu JJ, Crisco JJ. Head impact severity measures for evaluating mild traumatic brain injury risk exposure. Neurosurgery. 2008;62(4):789–798. doi: 10.1227/01.neu.0000318162.67472.ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Broglio SP, Schnebel B, Sosnoff JJ, et al. Biomechanical properties of concussions in high school football. Med Sci Sports Exerc. 2010;42(11):2064–2071. doi: 10.1249/MSS.0b013e3181dd9156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Guskiewicz KM, Mihalik JP, Shankar V, et al. Measurement of head impacts in collegiate football players: relationship between head impact biomechanics and acute clinical outcome after concussion. Neurosurgery. 2007;61(6):1244–1252. doi: 10.1227/01.neu.0000306103.68635.1a. [DOI] [PubMed] [Google Scholar]
- 128.Broglio SP, Eckner JT, Surma T, Kutcher JS. Post-concussion cognitive declines and symptomatology are not related to concussion biomechanics in high school football players. J Neurotrauma. 2011;28(10):2061–2068. doi: 10.1089/neu.2011.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hinton-Bayre AD, Geffen G. Severity of sports-related concussion and neuropsychological test performance. Neurology. 2002;59(7):1068–1070. doi: 10.1212/wnl.59.7.1068. [DOI] [PubMed] [Google Scholar]
- 130.Majerske CW, Mihalik JP, Ren D, et al. Concussion in sports: postconcussive activity levels, symptoms, and neurocognitive performance. J Athl Train. 2008;43(3):265–274. doi: 10.4085/1062-6050-43.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Silverberg ND, Iverson GL. Is rest after concussion “the best medicine”?: recommendations for activity resumption following concussion in athletes, civilians, and military service members. J Head Trauma Rehabil. 2013;28(4):250–259. doi: 10.1097/HTR.0b013e31825ad658. [DOI] [PubMed] [Google Scholar]
- 132.Covassin T, Elbin RJ, Harris W, Parker T, Kontos A. The role of age and sex in symptoms, neurocognitive performance, and postural stability in athletes after concussion. Am J Sports Med. 2012;40(6):1303–1312. doi: 10.1177/0363546512444554. [DOI] [PubMed] [Google Scholar]
- 133.World Health Organisation. ICD-10 classifications of mental and behavioural disorder: clinical descriptions and diagnostic guidelines. http://www.who.int/classifications/icd/en/bluebook.pdf. Published January 1992. Accessed August 29, 2013. [Google Scholar]
- 134.McGrath N, Dinn WM, Collins MW, Lovell MR, Elbin RJ, Kontos AP. Post-exertion neurocognitive test failure among student-athletes following concussion. Brain Inj. 2013;27(1):103–113. doi: 10.3109/02699052.2012.729282. [DOI] [PubMed] [Google Scholar]
- 135.Wisniewski JF, Guskiewicz KM, Trope M, Sigurdsson A. Incidence of cerebral concussions associated with type of mouthguard used in college football. Dent Traumatol. 2004;20(3):143–149. doi: 10.1111/j.1600-4469.2004.00259.x. [DOI] [PubMed] [Google Scholar]
- 136.Barbic D, Pater J, Brison RJ. Comparison of mouth guard designs and concussion prevention in contact sports: a multicenter randomized controlled trial. Clin J Sport Med. 2005;15(5):294–298. doi: 10.1097/01.jsm.0000171883.74056.21. [DOI] [PubMed] [Google Scholar]
- 137.Finch C, Braham R, McIntosh A, McCrory P, Wolfe R. Should football players wear custom fitted mouthguards? Results from a group randomised controlled trial. Inj Prev. 2005;11(4):242–246. doi: 10.1136/ip.2004.006882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Blignaut JB, Carstens IL, Lombard CJ. Injuries sustained in rugby by wearers and non-wearers of mouthguards. Br J Sports Med. 1987;21(2):5–7. doi: 10.1136/bjsm.21.2.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Marshall SW, Loomis DP, Waller AE, et al. Evaluation of protective equipment for prevention of injuries in rugby union. Int J Epidemiol. 2005;34(1):113–118. doi: 10.1093/ije/dyh346. [DOI] [PubMed] [Google Scholar]
- 140.Benson BW, Meeuwisse WH. Ice hockey injuries. Med Sport Sci. 2005;49:86–119. doi: 10.1159/000085393. [DOI] [PubMed] [Google Scholar]
- 141.Labella CR, Smith BW, Sigurdsson A. Effect of mouthguards on dental injuries and concussions in college basketball. Med Sci Sports Exerc. 2002;34(1):41–44. doi: 10.1097/00005768-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 142.Mihalik JP, McCaffrey MA, Rivera EM, et al. Effectiveness of mouthguards in reducing neurocognitive deficits following sports-related cerebral concussion. Dent Traumatol. 2007;23(1):14–20. doi: 10.1111/j.1600-9657.2006.00488.x. [DOI] [PubMed] [Google Scholar]
- 143.Kemp SP, Hudson Z, Brooks JH, Fuller CW. The epidemiology of head injuries in English professional rugby union. Clin J Sport Med. 2008;18(3):227–234. doi: 10.1097/JSM.0b013e31816a1c9a. [DOI] [PubMed] [Google Scholar]
- 144.McIntosh AS, McCrory P. Effectiveness of headgear in a pilot study of under 15 rugby union football. Br J Sports Med. 2001;35(3):167–169. doi: 10.1136/bjsm.35.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kahanov L, Dusa MJ, Wilkinson S, Roberts J. Self-reported headgear use and concussions among collegiate men's rugby union players. Res Sports Med. 2005;13(2):77–89. doi: 10.1080/15438620590956025. [DOI] [PubMed] [Google Scholar]
- 146.Broglio SP, Ju YY, Broglio MD, Sell TC. The efficacy of soccer headgear. J Athl Train. 2003;38(3):220–224. [PMC free article] [PubMed] [Google Scholar]
- 147.Withnall C, Shewchenko N, Wonnacott M, Dvorak J. Effectiveness of headgear in football. Br J Sports Med. 2005;39(suppl 1):i40–i48. doi: 10.1136/bjsm.2005.019174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Hrysomallis C. Impact energy attentuation of protective football headgear against a yielding surface. J Sci Med Sport. 2004;7(2):156–164. doi: 10.1016/s1440-2440(04)80005-7. [DOI] [PubMed] [Google Scholar]
- 149.Delaney JS, Al-Kashmiri A, Drummond R, Correa JA. The effect of protective headgear on head injuries and concussions in adolescent football (soccer) players. Br J Sports Med. 2008;42(2):110–115. doi: 10.1136/bjsm.2007.037689. [DOI] [PubMed] [Google Scholar]
- 150.Bakhos LL, Lockhart GR, Myers R, Linakis JG. Emergency department visits for concussion in young child athletes. Pediatrics. 2010;126(3):e550–e556. doi: 10.1542/peds.2009-3101. [DOI] [PubMed] [Google Scholar]
- 151.Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA. 1999;282(10):958–963. doi: 10.1001/jama.282.10.958. [DOI] [PubMed] [Google Scholar]
- 152.Giedd JN. The teen brain: insights from neuroimaging. J Adolesc Health. 2008;42(4):335–343. doi: 10.1016/j.jadohealth.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 153.Giedd JN, Blumenthal J, Jefferies NO, et al. Brain development during childhood and adolescence: a longitudinal MRI study. Nat Neurosci. 1999;2(10):861–863. doi: 10.1038/13158. [DOI] [PubMed] [Google Scholar]
- 154.Webbe FM, Barth JT. Short-term and long-term outcome of athletic closed head injuries. Clin Sports Med. 2003;22(3):577–592. doi: 10.1016/s0278-5919(02)00103-5. [DOI] [PubMed] [Google Scholar]
- 155.McKeever CK, Schatz P. Current issues in the identification, assessment, and management of concussions in sports-related injuries. Appl Neuropsychol. 2003;10(1):4–11. doi: 10.1207/S15324826AN1001_2. [DOI] [PubMed] [Google Scholar]
- 156.Buzzini SR, Guskiewicz KM. Sport-related concussion in the young athlete. Curr Opin Pediatr. 2006;18(4):376–382. doi: 10.1097/01.mop.0000236385.26284.ec. [DOI] [PubMed] [Google Scholar]
- 157.Shaw NA. The neurophysiology of concussion. Prog Neurobiol. 2002;67(4):281–344. doi: 10.1016/s0301-0082(02)00018-7. [DOI] [PubMed] [Google Scholar]
- 158.Fischer KW, Rose SP. Dynamic growth cycles of brain and cognitive development. In: RW Thatcher, GR Lyon, Rumsey J, Krasnegor N., editors. Developmental Neuroimaging: Mapping the Development of Brain and Behavior. New York, NY: Academic Press;; 1996. pp. 263–279. In. eds. [Google Scholar]
- 159.Thomas R, Taylor K. Assessing head injuries in children. MCN Am J Matern Child Nurs. 1997;22(4):198–202. doi: 10.1097/00005721-199707000-00008. [DOI] [PubMed] [Google Scholar]
- 160.Levin HS. Neuroplasticity following non-penetrating traumatic brain injury. Brain Inj. 2003;17(8):665–674. doi: 10.1080/0269905031000107151. [DOI] [PubMed] [Google Scholar]
- 161.Ewing-Cobbs L, Barnes MA, Fletcher JM. Early brain injury in children: development and reorganization of cognitive function. Dev Neuropsychol. 2003;24(2–3):669–704. doi: 10.1080/87565641.2003.9651915. [DOI] [PubMed] [Google Scholar]
- 162.Kirkwood MW, Yeates KO, Wilson PE. Pediatric sport-related concussion: a review of the clinical management of an oft-neglected population. Pediatrics. 2006;117(4):1359–1371. doi: 10.1542/peds.2005-0994. [DOI] [PubMed] [Google Scholar]
- 163.Moser RS, Schatz P, Jordan BD. Prolonged effects of concussion in high school athletes. Neurosurgery. 2005;57(2):300–306. doi: 10.1227/01.neu.0000166663.98616.e4. [DOI] [PubMed] [Google Scholar]
- 164.Sim A, Terrberry-Spohr L, Wilson KR. Prolonged recovery of memory functioning after mild traumatic brain injury in adolescent athletes. J Neurosurg. 2008;108(3):511–516. doi: 10.3171/JNS/2008/108/3/0511. [DOI] [PubMed] [Google Scholar]
- 165.McCrory PR. Does second impact syndrome exist? Clin J Sport Med. 2001;11(3):144–149. doi: 10.1097/00042752-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 166.Cassidy JD, Carroll LJ, Peloso PM, et al. WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Incidence, risk factors, and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004;(suppl 43):28–60. doi: 10.1080/16501960410023732. [DOI] [PubMed] [Google Scholar]
- 167.Bruce DA. Delayed deterioration of consciousness after trivial head injury in childhood. Br Med J (Clin Res Ed) 1984;289(6447):715–716. doi: 10.1136/bmj.289.6447.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Snoek JW, Minderhound JM, Wilmink JT. Delayed deterioration following mild head injury in children. Brain. 1984;107(pt 1):15–36. doi: 10.1093/brain/107.1.15. [DOI] [PubMed] [Google Scholar]
- 169.Halstead ME, Walter KD. Council on Sports Medicine and Fitness, American Academy of Pediatrics. Clinical report: sport-related concussion in children and adolescents. Pediactrics. 2010;126(3):597–615. doi: 10.1542/peds.2010-2005. [DOI] [PubMed] [Google Scholar]
- 170.Alla S, Sullivan SJ, Hale L, McCrory PR. Self-report scales/checklists for the measurement of concussion symptoms: a systematic review. Br J Sports Med. 2009;43(suppl 1):i3–i12. doi: 10.1136/bjsm.2009.058339. [DOI] [PubMed] [Google Scholar]
- 171.Mailer BJ, Valovich-Mcleod TC, Bay RC. Healthy youth are reliable in reporting symptoms on a graded symptom scale. J Sport Rehabil. 2008;17(1):11–20. doi: 10.1123/jsr.17.1.11. [DOI] [PubMed] [Google Scholar]
- 172.Gioia GA, Collins MW, Isquith PK. Improving identification and diagnosis of mild traumatic brain injury with evidence: psychometric support for the acute concussion evaluation. J Head Trauma Rehabil. 2008;23(4):230–242. doi: 10.1097/01.HTR.0000327255.38881.ca. [DOI] [PubMed] [Google Scholar]
- 173.Lovell MR, Iverson GL, Collins MW, et al. Measurement of symptoms following sports-related concussion: reliability and normative data for the post-concussion scale. Appl Neuropsychol. 2006;13(3):166–174. doi: 10.1207/s15324826an1303_4. [DOI] [PubMed] [Google Scholar]
- 174.Yeates KO, Luria J, Bartkowski H, Rusin J, Martin L, Bigler ED. Postconcussive symptoms in children with mild closed head injuries. J Head Trauma Rehabil. 1999;14(4):337–350. doi: 10.1097/00001199-199908000-00003. [DOI] [PubMed] [Google Scholar]
- 175.Valovich McLeod TC, Barr WB, McCrea M, Guskiewicz KM. Psychometric and measurement properties of concussion assessment tools in youth sports. J Athl Train. 2006;41(4):399–408. [PMC free article] [PubMed] [Google Scholar]
- 176.McCrory PR, Collie A, Anderson V, Davis G. Can we manage sport related concussion in children the same as in adults? Br J Sports Med. 2004;38(5):516–519. doi: 10.1136/bjsm.2004.014811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Kirkwood MW, Randolph C, Yeates KO. Returning pediatric athletes to play after concussion: the evidence (or lack thereof) behind baseline neuropsychological testing. Acta Paediatr. 2009;98(9):1409–1411. doi: 10.1111/j.1651-2227.2009.01448.x. [DOI] [PubMed] [Google Scholar]
- 178.Canadian Paediatric Society. Identification and management of children with sport-related concussion. Paediatr Child Health. 2006;11(7):420–428. [Google Scholar]
- 179.Purcell L. What are the most appropriate return-to-play guidelines for concussed child athletes? Br J Sports Med. 2009;43(suppl 1):i51–i55. doi: 10.1136/bjsm.2009.058214. [DOI] [PubMed] [Google Scholar]
- 180.Valovich-Mcleod TC, Bay RC, Lam KC, Chhabra A. Representative baseline values on the Sport Concussion Assessment Tool 2 (SCAT2) in adolescent athletes vary by gender, grade, and concussion history. Am J Sports Med. 2012;40(4):927–933. doi: 10.1177/0363546511431573. [DOI] [PubMed] [Google Scholar]
- 181.McCrory P, Johnston K, Meeuwisse W, et al. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Br J Sports Med. 2005;39(4):196–204. doi: 10.1136/bjsm.2005.018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Schulz MR, Marshall SW, Mueller FO, et al. Incidence and risk factors for concussion in high school athletes, North Carolina, 1996–1999. Am J Epidemiol. 2004;160(10):937–944. doi: 10.1093/aje/kwh304. [DOI] [PubMed] [Google Scholar]
- 183.Cantu RC, Register-Mihalik JK. Considerations for return-to-play and retirement decisions after concussion. PM R. 2011;3(10 suppl 2):S440–S444. doi: 10.1016/j.pmrj.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 184.Broglio SP, Ferrara MS, Piland SG, Anderson RB, Collie A. Concussion history is not a predictor of computerized neurocognitive performance. Br J Sports Med. 2006;40(9):802–805. doi: 10.1136/bjsm.2006.028019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Collie A, McCrory P, Makdissi M. Does history of concussion affect current cognitive status? Br J Sports Med. 2006;40(6):550–551. doi: 10.1136/bjsm.2005.019802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Iverson GL, Brooks BL, Lovell MR, Collins MW. No cumulative effects for one or two previous concussions. Br J Sports Med. 2006;40(1):72–75. doi: 10.1136/bjsm.2005.020651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.De Beaumont L, Theoret H, Mongeon D, et al. Brain function decline in healthy retired athletes who sustained their last sports concussion in early adulthood. Brain. 2009;132(pt 3):695–708. doi: 10.1093/brain/awn347. [DOI] [PubMed] [Google Scholar]
- 188.Ellemberg D, Leclerc S, Couture S, Daigle C. Prolonged neuropsychological impairments following a first concussion in female university soccer athletes. Clin J Sport Med. 2007;17(5):369–374. doi: 10.1097/JSM.0b013e31814c3e3e. [DOI] [PubMed] [Google Scholar]
- 189.Breedlove EL, Robinson M, Talavage TM, et al. Biomechanical correlates of symptomatic and asymptomatic neurophysiological impairment in high school football. J Biomech. 2012;45(7):1265–1272. doi: 10.1016/j.jbiomech.2012.01.034. [DOI] [PubMed] [Google Scholar]
- 190.Talavage TM, Nauman E, Breedlove EL, et al. Functionally-detected cognitive impairment in high school football players without clinically-diagnosed concussion. J Neurotrauma. doi: 10.1089/neu.2010.1512. http://online.liebertpub.com/doi/full/10.1089/neu.2010.1512. Published online ahead of print April 11, 2013. Accessed August 30, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Bazarian JJ, Zhu T, Blyth B, Borrino A, Zhong J. Subject-specific changes in brain white matter on diffusion tensor imaging after sports-related concussion. Magn Reson Imaging. 2012;30(2):171–180. doi: 10.1016/j.mri.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Broglio SP, Pontifex MB, O'Connor P, Hillman CH. The persistent effects of concussion on neuroelectic indices of attention. J Neurotrauma. 2009;26(9):1463–1470. doi: 10.1089/neu.2008.0766. [DOI] [PubMed] [Google Scholar]
- 193.Pontifex MB, O'Connor PM, Broglio SP, Hillman CH. The association between mild traumatic brain injury history and cognitive control. Neuropsychologia. 2009;47(14):3210–3216. doi: 10.1016/j.neuropsychologia.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 194.Gaetz M, Goodman D, Weinberg H. Electrophysiological evidence for the cumulative effects of concussion. Brain Inj. 2000;14(12):1077–1088. doi: 10.1080/02699050050203577. [DOI] [PubMed] [Google Scholar]
- 195.Dupuis F, Johnston KM, Lavoie M, Lepore F, Lassonde M. Concussion in athletes produce brain dysfunction as revealed by event-related potentials. Neuroreport. 2000;11(18):4087–4092. doi: 10.1097/00001756-200012180-00035. [DOI] [PubMed] [Google Scholar]
- 196.Sosnoff JJ, Broglio SP, Shin S, Ferrara MS. Previous mild traumatic brain injury and postural control dynamics. J Athl Train. 2011;46(1):85–91. doi: 10.4085/1062-6050-46.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Martini DN, Sabin MJ, DePesa SA, et al. The chronic effects of concussion on gait. Arch Phys Med Rehabil. 2011;92(4):585–589. doi: 10.1016/j.apmr.2010.11.029. [DOI] [PubMed] [Google Scholar]
- 198.Gavett BE, Stern RA, McKee AC. Chronic traumatic encephalopathy: a potential late effect of sport-related concussive and subconcussive head trauma. Clin Sports Med. 2011;30(1):179–188. doi: 10.1016/j.csm.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Omalu BI, DeKosky ST, Hamilton RL, et al. Chronic traumatic encephalopathy in a National Football League player, part II. Neurosurgery. 2006;59(5):1086–1092. doi: 10.1227/01.NEU.0000245601.69451.27. [DOI] [PubMed] [Google Scholar]
- 200.Omalu BI, DeKosky ST, Minster RL, Kamboh MI, Hamilton RL, Wecht CH. Chronic traumatic encephalopathy in a National Football League player. Neurosurgery. 2005;57(1):128–134. doi: 10.1227/01.neu.0000163407.92769.ed. [DOI] [PubMed] [Google Scholar]
- 201.Broglio SP, Eckner JT, Paulson H, Kutcher JS. Cognitive decline and aging: the role of concussive and sub-concussive impacts. Exerc Sport Sci Rev. 2012;40(3):138–144. doi: 10.1097/JES.0b013e3182524273. [DOI] [PMC free article] [PubMed] [Google Scholar]