Abstract
Diverticulitis is a debilitating complication of diverticular disease that affects approximately 2.5 million individuals in the United States. Compared to many other gastrointestinal conditions, diverticular disease is poorly understood in terms of its burden on patients and healthcare systems. This review examines the existing literature and discusses the current knowledge of the burden of diverticular disease. Literature confirmed that bothersome symptoms (such as abdominal pain and bloating) and potentially serious, disease-related complications (such as diverticulitis and diverticular bleeding) place a significant burden on patients. Broad-spectrum antibiotic therapy and surgery are the generally accepted mainstays of treatment for acute complications of diverticular disease. Despite these options, patients frequently experience substantially reduced quality of life (particularly in terms of social and emotional functioning) and increased mortality (predominantly due to disease-related complications) compared to healthy controls. Furthermore, diverticular disease accounted for 254,179 inpatient discharges and 1,493,865 outpatient clinic visits in the United States in 2002, at an estimated cost per hospitalization of $9,742-$11,729. Enhancing the quality of life of patients with diverticular disease and reducing disease exacerbations and complications will substantially benefit patients and healthcare systems. However, long-established treatment algorithms fall short of these therapeutic goals. Research into new treatment options for patients with diverticular disease should therefore be pursued.
Keywords: Diverticular disease, quality of life, disease burden, healthcare costs
Colonic diverticulosis is an age-related disease that affects approximately one fourth of the population in developed countries.1 Diverticulosis is characterized by asymptomatic saclike protrusions (diverticula) in the colonic wall that form when the mucosa herniates at weak points in the muscularis propria; these weak points occur where blood vessels enter to supply the colonic wall.2 Although most patients with pathologic evidence of colonic diverticula are asymptomatic, some patients develop symptoms such as abdominal discomfort and altered bowel habits.
These patients are said to have symptomatic diverticular disease. Clinical symptoms develop in up to 25% of patients with diverticular disease.3,4 When infection and/or inflammation develop in the diverticula, the condition is generally known as diverticulitis; despite the general acceptance of this definition, a separate classification of the disease has yet to be defined.5 Medical treatment consisting of broad-spectrum antibiotics and bowel rest is usually indicated to resolve the initial symptoms of acute diverticular disease, although surgery may be necessary in the event of a life-threatening complication such as a perforation, obstruction, abscess, or fistula.6-8 For patients who experience recurrent episodes of diverticulitis despite conservative treatment, surgical intervention is frequently recommended; however, surgery is not guaranteed to prevent a recurrence of diverticular disease elsewhere in the colon.4-10 As a relatively common gastrointestinal condition with complications that can require substantial medical attention to treat and stabilize, diverticular disease would be expected to place a considerable burden on both patients and healthcare resources. However, research in this area is still relatively immature compared to research on the burden of other gastrointestinal diseases. This article reviews the available evidence regarding the impact of diverticular disease on patients in terms of quality of life and mortality, and it explores the burden of the disease on healthcare utilization and resources. In constructing this review, a search of the PubMed database for the period 1995—2010 was performed using “diverticular disease” and “diverticulitis” as constant search terms and including additional terms—such as “healthcare,” “utilization,” “burden,” “cost,” “economics,” “quality of life,” and “mortality”—in each section. Additional supporting references known to the authors were reviewed and included as relevant.
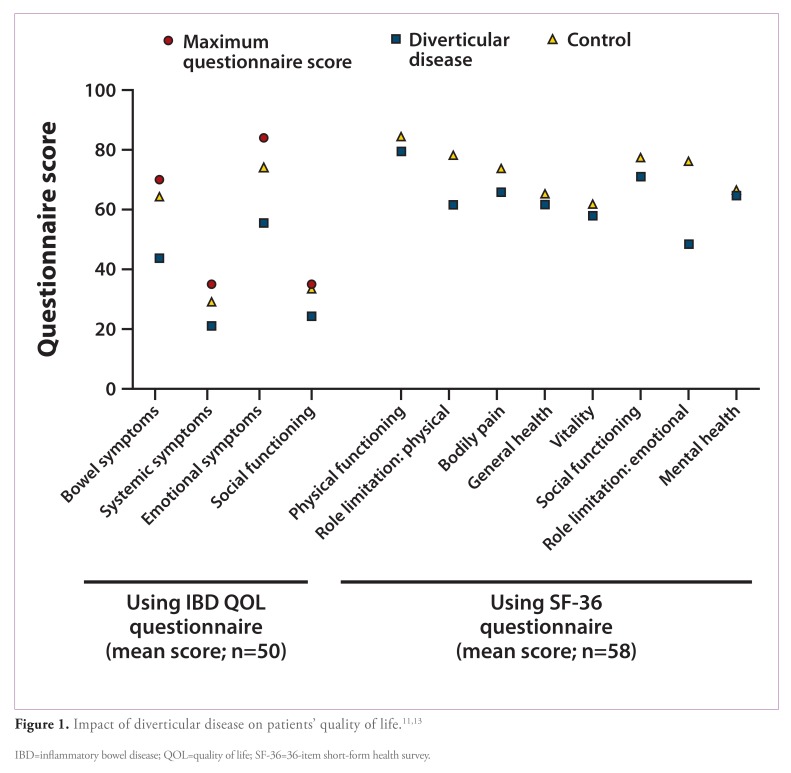
Impact on Quality of Life and Daily Activities
In contrast to the many studies on other chronic digestive diseases, very few studies have examined the effect of diverticular disease on patients’ quality of life, and current research in this area lacks a validated, disease-specific questionnaire. Although few studies have examined how quality of life relates to the disease state (as opposed to how surgical intervention affects quality of life), preliminary evidence for a deterioration in quality of life in patients with diverticular disease comes from 3 small, uncontrolled studies, 2 of which are depicted in Figure 1.11-13 In the first of these studies, 50 patients with symptomatic diverticular disease as their primary diagnosis were retrospectively identified from medical records and were shown to have significantly lower quality-of-life scores in all 4 domains of a structured, nonvalidated questionnaire (bowel symptoms, systemic symptoms, emotional symptoms, and social functioning) compared to 50 matched healthy control subjects (P<.003 for all areas).11 Diverticular disease particularly affected scores for bowel symptoms and emotional symptoms. In this study, no distinction was made between patients with diverticular disease, diverticulitis, or other complications. In a separate study, researchers noted an overall negative impact on all domains of the generic, 36-item short-form health survey (SF-36) questionnaire in 38 patients (age <50 years) with diverticular disease and/or diverticulitis who were identified from a hospital medical database. Although this study had a small number of patients, it found no significant difference in mean SF-36 domain scores between patients treated with either medical therapy (n=33) or surgical intervention (n=5).12 Similarly, in a third study, SF-36 domain scores were shown to be adversely affected (compared to the population norm) in 58 outpatients with uncomplicated, symptomatic diverticular disease.13 Notably, 6 months of randomized treatment (given on a cyclic basis) with the broad-spectrum antibiotic rifaximin (Xifaxan, Salix Pharmaceuticals) or oral 5-aminosalicylic acid (5-ASA) significantly improved mean SF-36 domain scores and global symptom scores from baseline in both treatment groups. However, the greatest improvement was seen in the 5-ASA group. Despite the limited data specifically examining quality of life, the results of these 3 studies suggest a clear burden of diverticular disease on the lives of patients. Other studies assessing quality of life in patients with diverticular disease have utilized this outcome measure to compare different surgical techniques. In 1 study, quality of life (assessed using the SF-36 questionnaire) was shown to be similar after long-term follow-up (minimum, 2 years; mean, 62.2 months) in 45 matched pairs of patients who had undergone either open or lapa- roscopic surgery for acute diverticulitis.14 In this study, SF-36 scores for both groups were high and only slightly below that expected for the general population. Similar quality-of-life scores (also measured using the SF-36 questionnaire) were observed in 99 patients who had undergone either laparoscopic or open colectomy for benign polyps or uncomplicated diverticular disease.15 The occurrence of postoperative complications (hernia or small bowel obstruction) predicted lower SF-36 scores in both groups. In a third study, no significant difference in long-term quality of life (measured using the SF-36 questionnaire) was noted in 188 patients who had undergone single-stage or staged resection for complicated diverticular disease; patients in this study were treated up to 22 years prior to administration of the survey, and those patients who had undergone stagedresection were surveyed following reversal.16 However, social functioning and general health were substantially worse in both groups compared to the general US population. Age and postoperative complications also had a significant impact on physical domain scores. Despite the lack of a disease-specific assessment instrument, these studies suggest a substantial impact of diverticular disease—related symptoms on patients’ quality of life. Statistics show that there are 86,000 patients with diverticular disease in the United States who are registered as disabled (out of a total disease population of 2.5 million), indicating that the disease has a substantial impact on patients’ daily lives.17-19 For patients who are candidates for medical therapy, new treatment options are required to reduce the impact of the disease on patients’ lives. When patients require surgery, the type of surgical intervention appears to have little influence on patients’ quality of life; however, the development of postoperative, disease-related complications can have a major impact on quality of life.
Mortality Associated with Diverticular Disease
Most deaths in patients with diverticular disease tend to be related to severe disease complications (Table 1). In 1998, a total of 3,414 deaths were attributed to diverticular disease in the United States (70% of which occurred in women), yielding an overall mortality rate of 2.5 deaths per 100,000 individuals.20 At that time, diverticular disease ranked sixth overall in terms of gastrointestinal mortality. The latest figures showed that, out of a total of 2,397,615 deaths in the United States in 2004, diverticular disease accounted for 3,372 deaths (0.14%).21,22 The prevalence and annual incidence of diverticular disease in the United States are thus approximately 2.5 million and 300,000, respectively.19 Similar trends are seen in Europe, where the most recent estimates indicate that 23,605 deaths are due to diver-ticular disease each year, with an inpatient mortality rate of 3%.1 Unsurprisingly, in-hospital mortality is generally lower among patients who can be treated medically compared to patients who require surgical intervention.23 Indeed, the highest mortality rate is observed among patients who undergo emergency surgery for complicated diverticular disease, with current estimates reporting that 12—36% of patients die following surgery.3 Peritonitis, in particular, is associated with a high mortality rate (approximately 6% if purulent and 35% if feculent).24 In a meta-analysis of surgical procedures, postoperative mortality was approximately 14% following surgery for acute diverticulitis with generalized peritonitis.25 In 2 further studies, the Mannheim Peritonitis Index score was shown to predict mortality in elderly patients with perforated diverticulitis.26,27 Additionally, different operative procedures appear to be associated with different mortality rates. In a recent meta-analysis of 15 studies (which were mainly retrospective), primary resection with anastomosis was compared to the conventional Hartmann procedure in 963 patients with acute colonic diverticulitis; postoperative mortality rates were shown to be 4.9% and 15.1%, respectively.25 In the emergency setting, postoperative mortality rates were 7.4% with primary resection plus anastomosis and 15.6% with the Hartmann procedure. These results may reflect real differences between the 2 procedures, or they may be due to differences in patient-related, hospital-related, and/or study-related factors. Further prospective studies are required to explain the observed differences in mortality. Population mortality rates due to diverticular disease have remained relatively stable over recent years.20,28-30 A reduction in mortality rates might have been expected as a result of improvements in treatment and patient care; however, any improvements in care must be balanced against the increasing prevalence of the disease and advances in diagnosis and disease classification. Therefore, continuing to improve our understanding of this disease and its treatment options is essential in order to combat the increasing caseload of this disease.
Healthcare Utilization
Diverticular disease is responsible for large numbers of gastrointestinal admissions and clinic visits, and it places a significant burden on emergency and surgical resources. Furthermore, this burden is increasing with the rising caseload of diverticular disease in the United States. In 2002, diverticular disease accounted for 254,179 inpatient discharges in the United States and an estimated 1,493,865 outpatient clinic visits.30 For admitted patients, the median length of stay in the hospital was estimated to be 3 or 4 days (for patients with or without hemorrhage, respectively).30 The shorter hospital stay in patients with hemorrhage is likely due to the self-limiting nature of diverticular bleeding in most patients. The most recent data indicate that a total of 815,000 patients required hospitalization for diverticular disease in 2004, with 3.2 million patients receiving outpatient care for this condition.30 In total, this care resulted in $2.8 million in prescription costs alone. Some evidence suggests that pain related to diverticular disease is one of the leading causes of emergency room visits due to nontraumatic abdominal pain, at least among the elderly.31 Among patients with diverticular disease, the most common reasons for emergency admissions appear to be acute diverticulitis and diverticular hemorrhage.32 Emergency admissions requiring immediate surgery are associated with prolonged hospital stays, higher morbidity, and higher postoperative mortality than emergency admissions that do not require surgical intervention.32 Prior recurrent admissions and younger age are factors associated with an elevated risk of emergency surgery.29,32-34 Few studies have analyzed changes in hospital admis- sion patterns; however, evidence suggests that admissions due to diverticular disease are increasing. Nationwide inpatient samples of 267,000 patients in the United States showed that diverticular disease accounted for 120,500 admissions in 1998 and 151,900 admissions in 2005 (26% increase).35 Over this 8-year period, the age-adjusted rate of diverticulitis increased from 61.9 cases per 100,000 patients to 75.6 cases per 100,000 patients, with admission rates increasing most rapidly among patients 44 years of age or younger; specifically, the data showed a 150% increase in patients 15—24 years of age, a 70% increase in patients 25-44 years of age, and a 28% increase in patients 45—64 years of age.36 Similar results have been observed in England, where examination of patients’ admission criteria between 1996 and 2006 revealed 560,281 admissions with a primary diagnosis of diverticular disease. Over the study period, the national admission rate increased from 0.56 admissions per 1,000 individuals per year to 1.20 admissions per 1,000 individuals per year.37 Among both studies in the United States and England, a similar time trend was reported for both outpatients and admissions requiring surgery.
Economic Impact of Diverticular Disease
Various studies have shown that diverticular disease places a significant burden on healthcare resources.38 In 1998, when 2.2 million cases of diverticular disease occurred in the United States, total direct healthcare costs attributed to the disease were $2.358 billion (Table 2).20 At this time, indirect costs associated with the disease amounted to $141 million, resulting in a total cost due to diverticular disease of $2.499 billion. Thus, diverticular disease was the fifth most important gastrointestinal disease in the United States from an eco-nomic perspective. The most recent data available, from 2008, estimate the mean cost per patient discharge to be $9,594, resulting in an aggregate cost of $3.066 billion throughout the United States.39 The costs associated with diverticular disease include those related to hospitalizations (including stays in intensive care units and/or high dependency units), surgery, investigations (eg, colonoscopies, flexible sigmoidoscopies, barium enemas, computed tomography scans, and ultrasound scans), clinic visits (including emergency room, outpatient, and physician office visits), and medications.20,38,40 However, the main cost driver is the use of hospital facilities (bed days), which accounts for 65—70% of the total healthcare costs associated with diverticular disease.20,38 In this regard, 2002 data showed a median number of 3—4 bed days per admission in the United States and 6 bed days per admission in England.30,41 Given these data, strategies to reduce the number of hospital admissions and bed days may have clear benefits for patients and could result in cost savings for healthcare providers. Recent evidence suggests that delaying elective surgery for patients with recurrent, uncomplicated diverticular disease is the optimal treatment strategy from both an economic perspective and a clinical perspective, as this approach results in a reduced symptom burden, fewer admissions, less additional treatment, lower rates of mortality and colostomy, an increase in quality-adjusted life-years, and significant cost savings.42-45 In patients for whom surgery is indicated, a recent meta-analysis showed that laparoscopic surgery for diverticular disease was associated with a significantly reduced length of stay (a reduction of nearly 4 days) and fewer complications compared to open surgery, which translates into lower overall costs.46-51 Considering the care that patients receive during treatment, growing evidence suggests that the type of healthcare provider present at each visit can play an important role in reducing costs. One study showed that provision of care by an integrated, multidisciplinary, digestive health service can significantly reduce overall costs (P=.0497) and the length of the hospital stay (P=.0017) in patients admitted for diverticulitis compared to care provided by nonintegrated inpatient services.52 This finding suggests that cost savings can be achieved by providing dedicated, multidisciplinary, gastrointestinal healthcare. In another study, gastroenterologistled inpatient treatment of patients with acute diverticulitis was shown to be associated with reduced costs (resulting from shorter hospital stays and a lower risk of future readmission) compared to treatment led by family practitioners or internists.53 Similarly, a recent systematic review showed that care for gastrointestinal bleeding and diverticulitis provided by gastroenterologists was associated with a significantly shorter length of stay compared to care provided by general physicians (internists, family physicians, and/or general surgeons).54 Readers should note that the aforementioned results are all from retrospective studies and thus may have been prone to selection bias. However, these findings suggest that gastroenterologists and colorectal surgeons may provide more effective and efficient care when managing patients with diverticular disease.
Conclusion
Diverticular disease is a very common gastrointestinal condition that places a significant burden on patients (in terms of symptoms, quality of life, and mortality) and is associated with significant healthcare resource utilization and costs. Medical therapy may potentially help improve troublesome symptoms and quality of life in some patients, but other patients may develop recurrent or severe disease and/or serious complications that necessitate hospitalization and surgery. In addition to impacting healthcare utilization and the overall cost of care, complications of diverticular disease are associated with a high mortality rate. Future research therefore needs to assess strategies for reducing both the morbidity of diverticulitis and the healthcare costs associated with its complications. Specifically, studies should consider the level of care provided by gastroenterology specialists, whether delaying elective surgery for specific patients is appropriate, and how diagnosis and patient management is provided by physicians. In this regard, researchers need to move away from the retrospective studies that have traditionally been conducted in this area and instead concentrate on prospective trials, as high- quality data are needed to improve treatment practice and optimize management of diverticular disease.
Dr. Reddy has no conflicts of interest to disclose. Dr. Longo has received consulting fees/honoraria and support for travel to meetings from Shire, but he has not received any funding in connection with this manuscript. Shire Development LLC provided funding to GeoMed and MedErgy for support in writing and editing this manuscript. Mark Richardson (contract writer), Sarah Wright (GeoMed), and Jason McDonough (MedErgy) provided writing assistance for this publication under the direction of the authors. GeoMed and MedErgy also provided editorial assistance in formatting, proofreading, copyediting, and fact checking. Representatives from Shire Development LLC reviewed and edited the manuscript for scientific accuracy. Although Shire Development LLC was involved in the topic concept and fact checking of information, the authors independently controlled the content of this manuscript, the ultimate interpretation, and the decision to submit it for publication.
References
- 1.Delvaux M. Diverticular disease of the colon in Europe: epidemiology, impact on citizen health and prevention. Aliment Pharmacol Ther. 2003;18(suppl 3):71–74. doi: 10.1046/j.0953-0673.2003.01720.x. [DOI] [PubMed] [Google Scholar]
- 2.Comparato G, Pilotto A, Franze A, Franceschi M, Di Mario F. Diverticular disease in the elderly. Dig Dis. 2007;25:151–159. doi: 10.1159/000099480. [DOI] [PubMed] [Google Scholar]
- 3.Janes SE, Meagher A, Frizelle FA. Management of diverticulitis. BMJ. 2006;332:271–275. doi: 10.1136/bmj.332.7536.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stollman N, Raskin JB. Diverticular disease of the colon. Lancet. 2004;363:631–639. doi: 10.1016/S0140-6736(04)15597-9. [DOI] [PubMed] [Google Scholar]
- 5.Tursi A. New physio pathological and therapeutic approaches to diverticular disease of the colon. Expert Opin Pharmacother. 2007;8:299–307. doi: 10.1517/14656566.8.3.299. [DOI] [PubMed] [Google Scholar]
- 6.Rafferty J, Shellito P, Hyman NH, Buie WD. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939–944. doi: 10.1007/s10350-006-0578-2. [DOI] [PubMed] [Google Scholar]
- 7.Stollman NH, Raskin JB. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110–3121. doi: 10.1111/j.1572-0241.1999.01501.x. [DOI] [PubMed] [Google Scholar]
- 8.Murphy T, Hunt RH, Fried M, Krabshuis JH. World Gastroenterology Organisation (WGO) practice guidelines: diverticular disease. www.orldgastroenterology.org/assets/downloads/en/pdf/guidelines/07_diverticular_disease.pdf
- 9.Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133–142. doi: 10.1002/bjs.4873. [DOI] [PubMed] [Google Scholar]
- 10.Andeweg C, Peters J, Bleichrodt R, van Goor H. Incidence and risk factors of recurrence after surgery for pathology-proven diverticular disease. World J Surg. 2008;32:1501–1506. doi: 10.1007/s00268-008-9530-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bolster LT, Papagrigoriadis S. Diverticular disease has an impact on quality of life—results of a preliminary study. Colorectal Dis. 2003;5:320–323. doi: 10.1046/j.1463-1318.2003.00458.x. [DOI] [PubMed] [Google Scholar]
- 12.Koo V, Strange J, Lam CY, Epanomeritakis M. Young patients with diverticular disease: a preliminary quality of life study. Int J Surg. 2007;5:244–249. doi: 10.1016/j.ijsu.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 13.Comparato G, Fanigliulo L, Aragona G, et al. Quality of life in uncomplicated symptomatic diverticular disease: is it another good reason for treatment? Dig Dis. 2007;25:252–259. doi: 10.1159/000103896. [DOI] [PubMed] [Google Scholar]
- 14.Roblick UJ, Massmann A, Schwandner O, et al. Quality of life assessment after surgery for diverticulitis—a follow-up study. Zentralbl Chir. 2002;127:31–35. doi: 10.1055/s-2002-20231. [DOI] [PubMed] [Google Scholar]
- 15.Thaler K, Dinnewitzer A, Mascha E, et al. Long-term outcome and health-related quality of life after laparoscopic and open colectomy for benign disease. Surg Endosc. 2003;17:1404–1408. doi: 10.1007/s00464-002-8855-1. [DOI] [PubMed] [Google Scholar]
- 16.Constantinides VA, Aydin HN, Tekkis PP, Fazio VW, Heriot AG, Remzi FH. Long-term, health-related, quality of life comparison in patients undergoing single stage vs staged resection for complicated diverticular disease. Colorectal Dis. 2006;8:663–671. doi: 10.1111/j.1463-1318.2006.00961.x. [DOI] [PubMed] [Google Scholar]
- 17.Adams PF, Hendershot GE, Marano MA. Current estimates from the National Health Interview Survey, 1996. Vital Health Stat 10. 1999;l-203. [PubMed]
- 18.Collins JG. Prevalence of selected chronic conditions: United States, 1990— 1992. Vital Health Stat 10. 1997:1–89. [PubMed] [Google Scholar]
- 19.http://articles.directorym.com/Diverticular_Dis-ease-a852916.html#8056922 Natural Health Information On Demand. Diverticular disease: what should I know about diverticular disease?
- 20.Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500–1511. doi: 10.1053/gast.2002.32978. [DOI] [PubMed] [Google Scholar]
- 21.Minino AM, Heron MP, Murphy SL, Kochanek KD. Hyattsville, Md: National Center for Health Statistics; 2007. Deaths: final data for 2004. National Vital Statistics Reports. [PubMed] [Google Scholar]
- 22.http://digestive.niddk.nih.gov/statistics/statistics.aspx National Digestive Diseases Information Clearinghouse (NIDDC). Digestive disease statistics for the United States.
- 23.Peppas G, Bliziotis IA, Oikonomaki D, Falagas ME. Outcomes after medical and surgical treatment of diverticulitis: a systematic review of the available evidence. J Gastroenterol Hepatol. 2007;22:1360–1368. doi: 10.1111/j.1440-1746.2007.05118.x. [DOI] [PubMed] [Google Scholar]
- 24.Bogardus ST., Jr. What do we know about diverticular disease? A brief overview. J Clin Gastroenterol. 2006;40(suppl 3):S108–S111. doi: 10.1097/01.mcg.0000212603.28595.5c. [DOI] [PubMed] [Google Scholar]
- 25.Constantinides VA, Tekkis PP, Athanasiou T, et al. Primary resection with anastomosis vs. Hartmann’s procedure in nonelective surgery for acute colonic diverticulitis: a systematic review. Dis Colon Rectum. 2006;49:966–981. doi: 10.1007/s10350-006-0547-9. [DOI] [PubMed] [Google Scholar]
- 26.Makela JT, Kiviniemi H, Laitinen S. Prognostic factors of perforated sigmoid diverticulitis in the elderly. Dig Surg. 2005;22:100–106. doi: 10.1159/000085472. [DOI] [PubMed] [Google Scholar]
- 27.Pisanu A, Cois A, Uccheddu A. Surgical treatment of perforated diverticular disease: evaluation of factors predicting prognosis in the elderly. Int Surg. 2004;89:35–38. [PubMed] [Google Scholar]
- 28.Goldacre M, Duncan M, Cook-Mozaffari P, Davidson M, McGuiness H, Meddings D. http://www.uhce.ox.ac.uk/Atlases/Trends/England/Diverticular%20disease_Eng-land.pdf Diverticular disease in England 1996 to 2004: mortality trends.
- 29.Kang JY, Hoare J, Tinto A, et al. Diverticular disease of the colon—on the rise: a study of hospital admissions in England between 1989/1990 and 1999/2000. Aliment Pharmacol Ther. 2003;17:1189–1195. doi: 10.1046/j.1365-2036.2003.01551.x. [DOI] [PubMed] [Google Scholar]
- 30.Shaheen NJ, Hansen RA, Morgan DR, et al. The burden of gastrointestinal and liver diseases, 2006. Am J Gastroenterol. 2006;101:2128–2138. doi: 10.1111/j.1572-0241.2006.00723.x. [DOI] [PubMed] [Google Scholar]
- 31.Lewis LM, Banet GA, Blanda M, Hustey FM, Meldon SW. Gerson LW Etiology and clinical course of abdominal pain in senior patients: a prospective, multicenter study. J Gerontol A Biol Sci Med Sci. 2005;60:1071–1076. doi: 10.1093/gerona/60.8.1071. [DOI] [PubMed] [Google Scholar]
- 32.John SK, Teo NB, Forster AL. A prospective study of acute admissions in a surgical unit due to diverticular disease. Dig Surg. 2007;24:186–190. doi: 10.1159/000102897. [DOI] [PubMed] [Google Scholar]
- 33.Anaya DA, Flum DR. Risk of emergency colectomy and colostomy in patients with diverticular disease. Arch Surg. 2005;140:681–685. doi: 10.1001/archsurg.140.7.681. [DOI] [PubMed] [Google Scholar]
- 34.Pautrat K, Bretagnol F, Huten N, de Calan L. Acute diverticulitis in very young patients: a frequent surgical management. Dis Colon Rectum. 2007;50:472–477. doi: 10.1007/s10350-006-0787-8. [DOI] [PubMed] [Google Scholar]
- 35.Etzioni DA, Mack TM, Beart RW, Jr, Kaiser AM. Diverticulitis in the United States: 1998—2005: changing patterns of disease and treatment. Ann Surg. 2009;249:210–217. doi: 10.1097/SLA.0b013e3181952888. [DOI] [PubMed] [Google Scholar]
- 36.Nguyen GC, Sam JJ. Nationwide trends in hospital admissions for diverticulitis: a rising health burden among those under age 65 in the United States. Gastroenterology. 2011;136:A126. Abstract 833.
- 37.Jeyarajah S, Faiz O, Bottle A, et al. Diverticular disease hospital admissions are increasing, with poor outcomes in the elderly and emergency admissions. Aliment Pharmacol Ther. 2009;30:1171–1182. doi: 10.1111/j.1365-2036.2009.04098.x. [DOI] [PubMed] [Google Scholar]
- 38.Papagrigoriadis S, Debrah S, Koreli A, Husain A. Impact of diverticular disease on hospital costs and activity. Colorectal Dis. 2004;6:81–84. doi: 10.1111/j.1463-1318.2004.00532.x. [DOI] [PubMed] [Google Scholar]
- 39.Healthcare cost utilization project. US Department of Health and Human Services Agency for Healthcare Research and Quality. http://hcupnet.ahrq.gov
- 40.Burt CW, Schappert SM. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 1999—2000. Vital Health Stat 13- 2004;l-70. [PubMed]
- 41.Hospital episode statistics, Department of Health, England, 2002-03. http://www.rightdiagnosis.com/d/diverticular_diseases/stats.htm
- 42.Makela J, Vuolio S, Kiviniemi H, Laitinen S. Natural history of diverticular disease: when to operate? Dis Colon Rectum. 1998;41:1523–1528. doi: 10.1007/BF02237300. [DOI] [PubMed] [Google Scholar]
- 43.Makela JT, Kiviniemi HO, Laitinen ST. Elective surgery for recurrent diverticulitis. Hepatogastroenterology. 2007;54:1412–1416. [PubMed] [Google Scholar]
- 44.Richards RJ, Hammitt JK. Timing of prophylactic surgery in prevention of diverticulitis recurrence: a cost-effectiveness analysis. Dig Dis Sci. 2002;47:1903–1908. doi: 10.1023/a:1019624101225. [DOI] [PubMed] [Google Scholar]
- 45.Salem L, Veenstra DL, Sullivan SD, Flum DR. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg. 2004;199:904–912. doi: 10.1016/j.jamcollsurg.2004.07.029. [DOI] [PubMed] [Google Scholar]
- 46.Purkayastha S, Constantinides VA, Tekkis PP, et al. Laparoscopic vs. open surgery for diverticular disease: a meta-analysis of nonrandomized studies. Dis Colon Rectum. 2006;49:446–463. doi: 10.1007/s10350-005-0316-1. [DOI] [PubMed] [Google Scholar]
- 47.Alves A, Panis Y, Slim K, Heyd B, Kwiatkowski F, Mantion G. French multicentre prospective observational study of laparoscopic versus open colectomy for sigmoid diverticular disease. Br J Surg. 2005;92:1520–1525. doi: 10.1002/bjs.5148. [DOI] [PubMed] [Google Scholar]
- 48.Dwivedi A, Chahin F, Agrawal S, et al. Laparoscopic colectomy vs. open colectomy for sigmoid diverticular disease. Dis Colon Rectum. 2002;45:1309–1314. doi: 10.1007/s10350-004-6415-6. [DOI] [PubMed] [Google Scholar]
- 49.Liberman MA, Phillips EH, Carroll BJ, Fallas M, Rosenthal R. Laparoscopic colectomy vs traditional colectomy for diverticulitis. Outcome and costs. Surg Endosc. 1996;10:15–18. doi: 10.1007/s004649910002. [DOI] [PubMed] [Google Scholar]
- 50.Senagore AJ, Duepree HJ, Delaney CP, Dissanaike S, Brady KM, Fazio VW. Cost structure of laparoscopic and open sigmoid colectomy for diverticular disease: similarities and differences. Dis Colon Rectum. 2002;45:485–490. doi: 10.1007/s10350-004-6225-x. [DOI] [PubMed] [Google Scholar]
- 51.Kohler L, Risen D, Troidl H. Laparoscopic colorectal resection for diverticulitis. Int J Colorectal Dis. 1998;13:43–47. doi: 10.1007/s003840050130. [DOI] [PubMed] [Google Scholar]
- 52.Arseneau KO, Yeaton P, Kahaleh M, Cominelli F. Effect of digestive health care services integration on resource use and outcomes in patients with digestive disorders. Clin Gastroenterol Hepatol. 2003;1:145–151. doi: 10.1053/cgh.2003.50020. [DOI] [PubMed] [Google Scholar]
- 53.Zarling EJ, Piontek F, Klemka-Walden L, Inczauskis D. The effect of gastroenterology training on the efficiency and cost of care provided to patients with diverticulitis. Gastroenterology. 1997;112:1859–1862. doi: 10.1053/gast.1997.v112.pm9178677. [DOI] [PubMed] [Google Scholar]
- 54.Provenzale D, Ofman J, Gralnek I, Rabeneck L, Koff R, McCrory D. Gastroenterologist specialist care and care provided by generalists—an evaluation of effectiveness and efficiency. Am J Gastroenterol. 2003;98:21–28. doi: 10.1111/j.1572-0241.2003.07208.x. [DOI] [PubMed] [Google Scholar]