Abstract
Background.
We examined the effects of hip fracture on mortality, entry into long-term institutional care, and new evidence of poverty. We estimate of the proportion of hip fracture patients who require not just short-term rehabilitation but who become dependent on long-term institutional care, and the risk of becoming newly dependent on Medicaid or eligible for low-income subsidies following hip fracture.
Methods.
We used data from 2005 through 2010 for a random 5% sample of Medicare beneficiaries (N = 3.1 million) to conduct a retrospective matched cohort study. We used high-dimensional propensity score matching to compare outcomes for patients who experienced a hip fracture with subjects who did not, but had similar propensity for suffering a hip fracture. We then compared the 1-year risk of death, debility, and destitution between groups.
Results.
We matched 43,210 hip fracture patients to comparators without a hip fracture. Hip fractures were associated with more than a twofold increase in likelihood of mortality (incidence proportion ratio [IPR] of 2.27, 95% CI, 2.20–2.34), a fourfold increase in likelihood of requiring long-term nursing facility care (IPR, 3.96; 95% CI, 3.77–4.16), and a twofold increase in the probability of entering into low-income status (IPR, 2.14; 95% CI 1.99–2.31) within 1 year following hip fracture compared with subjects without a hip fracture.
Conclusions.
Hip fracture in elderly patients resulted in increased death, debility, and destitution. Initiatives that lead to improved treatment of osteoporosis could result in a decrease in incidence of fractures, subsequent death, debility, and destitution for older adults.
Key Words: Hip fracture, High-dimensional propensity score, Mortality, Osteoporosis.
Hip fractures in older adults are associated with increased mortality (1,2), morbidity (1), risk of second fracture (2), and decreased ability to perform activities of daily living (3–5). One-year mortality risk following hip fracture in patients aged 65 and over has been estimated between 12% and 37% (6,7), and 5-year mortality risk can reach upwards of 60% in some elderly populations (2,8–10). Among hip fracture survivors, half do not regain their pre-fracture functionality, and approximately, 20% require some type of long-term care (3,11).
Becoming dependent on institutional long-term care is an undesirable outcome that can itself result in lower quality of life. Moreover, long-term care is expensive. Estimates of private long-term care costs range between $60,000 and $72,000 per year (12). Long-term care insurance is available, but only about 2.3% of the U.S. population and 12.4% of individuals aged 65 and over have this type of insurance (13,14). Thus, many people who experience a hip fracture run the risk of exhausting their financial resources paying for care and can subsequently become eligible for Medicaid, adding to the social costs. Medicaid pays approximately $109 billion a year for long-term care of the elderly adults (15).
As many as 50% of hip fractures may be preventable (16,17): so some of the adverse outcomes and the financial burden associated with hip fractures can potentially be avoided. This article examines the effects of hip fracture on death, debility (new dependence long-term institutional care), and destitution (entry into Medicaid or eligibility for low-income drug subsidies). A unique contribution of this study is its estimation of the proportion of hip fracture patients who require not just short-term rehabilitation in a nursing facility, but who become dependent on long-term institutional care within 1 year after hip fracture. Another unique feature of this study is its determination of the risk of becoming newly impoverished following hip fracture within 1 year.
Methods
Data Source and Eligibility
We conducted a retrospective matched cohort study. We used administrative claims data from 2005 through 2010 for a random 5% sample of Medicare beneficiaries from the Chronic Condition Data Warehouse (18). The Chronic Condition Data Warehouse was created by the Centers for Medicare and Medicaid Services in order to provide researchers with easier to use, de-identified Medicare and Medicaid claims, assessment, and Part D Prescription Drug Event data that has already been merged and linked across the continuum of care (18). Use of these data was approved by Centers for Medicare and Medicaid Services and by the University of Alabama at Birmingham Institutional Review Board.
Individuals were eligible for analysis if they had continuous traditional fee-for-service Medicare coverage (Parts A and B, not enrolled in Medicare Advantage) for 12 consecutive months before their entry into this study and for 12 months after entry or up to the month in which they died. We excluded individuals enrolled in Medicare Advantage because they typically have incomplete claims data. Additionally, individuals had to be 65 years or older and residents of the 50 states or the District of Columbia. We excluded beneficiaries with problematic data (aged more than 110 years, migrated in or out of the 5% Medicare sample, multiple genders, birth dates, or death dates).
Hip fractures were identified using primary or non-primary inpatient hospital diagnosis codes for closed hip fracture or by outpatient diagnosis codes paired with procedure codes specific to hip fracture repair (19,20). We define the index date for hip fracture patients as the date of the first case-qualifying hip fracture claim (ie, admission date for hospitalization or date of service for outpatient claims). Individuals who suffered a second hip fracture during the 12-month follow-up period were excluded.
Outcomes of Interest
The outcomes of interest were death, debility, and destitution. Mortality was ascertained from Medicare enrollment data. We operationalize debility as new long-term nursing home placement among previously community-dwelling beneficiaries, therefore, individuals who were living in long-term nursing facilities at baseline were excluded from our debility analysis. Long-term nursing home placement was ascertained using physician claims for providing nursing home care. The precise algorithm was developed, described, and validated by Yun and colleagues (21). We operationalize destitution as becoming newly eligible for Medicaid or as being eligible for low-income subsidy under Medicare Part D, therefore, individuals who were Medicaid and low-income status eligible at baseline were excluded from our destitution analysis. We determined Medicaid enrollment from the Medicaid Buy-in (payment of Medicare premiums) variable in the Medicare data, and we determined low-income eligibility using receipt of low-income subsidies under Medicare part D as a marker of poverty. All outcomes were assessed within 365 days following the index date.
High-Dimensional Propensity Score Matching
Our study used high-dimensional propensity score (HDPS) matching to control for confounding. This method was developed by Schneeweiss and colleagues (22) and made publicly available for use (http://www.hdpharmacoepi.org/). HDPS procedures identify those factors, from the thousands of potential variables (eg, diagnoses and procedure codes), which are likely confounders in that they are strongly associated with exposures and outcomes of interest. Once these covariates have been identified, a propensity score for the likelihood of an exposure is generated for each subject in the data. For the development of our HDPSs, we used hip fracture as the exposure of interest and mortality as the outcome.
We calculated propensity scores in a time-varying manner for each subject as follows. For each beneficiary, we calculated the HDPS at the beginning of each 6-month interval (semester) from their first month of eligibility between January 1, 2006 through December 31, 2009 (eight semesters), using covariate data measured in the 365-day period preceding the start of the semester. We matched each beneficiary who experienced a hip fracture in a particular semester with a comparison subject who had a similar propensity score in the same semester but did not experience a hip fracture within that semester. Subjects were considered eligible for matching if they met inclusion criteria at the time of index fracture and had no fracture in the semester or in any preceding semester. In addition to being matched on propensity score, in order to further isolate the effect of hip fractures on our outcomes of interest and adjust for confounding, comparators had to have the same baseline residency status (long-term care facility versus community) and have the same income status (low versus not low income). We employed a greedy matching algorithm such that beneficiaries with hip fractures were matched to the closest comparators based on the fracture propensity score (23). Fracture and/or comparator pairs had to match with at least three decimal places of precision on the estimated propensity score.
Data Analysis
All data management and analyses were conducted using SAS 9.1 (SAS Institute, Cary, NC). We assessed the balance of observable baseline characteristics between the hip fracture cohort and all eligible comparators, and then between the fracture cohort and matched comparators. These characteristics included demographic factors that were explicitly part of the matching criteria: age, gender, race, residency status, personal income status, area (census tract) median income, geographic area, and rural area residency. We also examined the balance on a variety of health services utilization measures and comorbid conditions that were not explicitly specified in the HDPS algorithm. The utilization measures included total health care expenditures during the baseline period, hospital stays and inpatient days, number of physician visits, and use of skilled nursing facility or home health services. Comorbidities were assessed using Charlson comorbidity scores (derived from International Classification of Diseases-9 codes from both inpatient and outpatient claims using the method specified in Deyo and colleagues [24] and Kilgore and colleagues [25]), along with specific fracture risk factors: any osteoporosis diagnosis or fracture during baseline, conditions treated with glucocorticoids, and conditions that are associated with increased fall risk (26,27).
We used standardized differences (the absolute difference in means or proportions, divided by the pooled standard errors), as this method assesses balance between variables without respect to sample size (28). In general, standardized differences in excess of 20 are considered to represent serious imbalance between cohorts (29,30). For each outcome, and separately for the hip fracture and comparator cohorts, we computed the incidence proportion as the number of subjects experiencing the outcome, divided by the total number of beneficiaries in the cohort. We then calculated the incidence proportion ratios (IPR) and estimated the 95% CIs using log binomial regression models.
Results
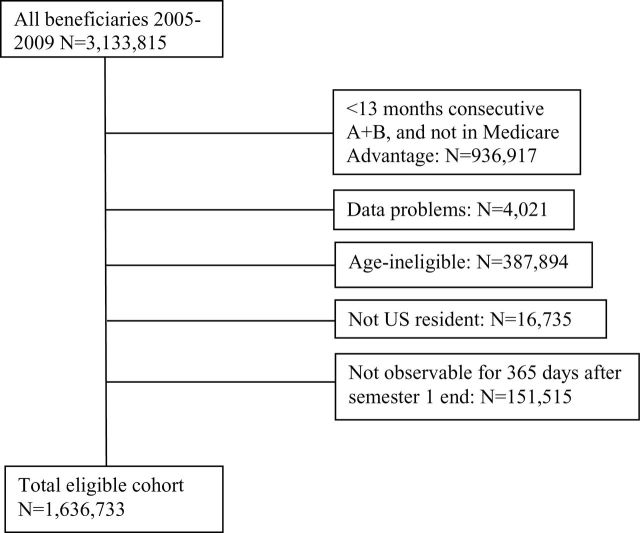
Figure 1 shows the selection of subjects eligible for inclusion in the study before HDPS matching. We began with 3.1 million Medicare beneficiaries.
Figure 1.
Construction of eligible cohort and results of exclusion criteria.
After removing individuals who did not meet eligibility criteria, we were left with 1.6 million eligible subjects. Of these, 46,730 experienced an incident hip fracture between 2006 and 2009. There were 1,550 hip fracture patients who could not be matched based on the predefined criteria (baseline residency status, income status, age, and gender), 1,282 patients who were matched on less than three propensity score decimal places, 1 patient who was out of HDPS matching range, and 565 matched pairs who were excluded because the matched comparator had a hip fracture within the year of follow up. That left 43,332 hip fracture cohort subjects matched to comparators without a hip fracture.
Table 1 compares demographic variables for the hip fracture cohort, the full group of potential comparators, and cohort of matched comparators who did not experience hip fractures. Individuals experiencing hip fractures were older and of lower socioeconomic status than those who did not have a fracture. The HDPS matching procedure resulted in much improved balance among these factors, both for the first semester and the overall sample. None of our standardized differences were more than 3.31 and most differences were less than 1.
Table 1.
Distribution (%) of Demographic Characteristics
| Baseline Characteristics | Hip Fractures | All Eligible Comparators | Standardized Differences | Matched Fractures | Matched Comparators | Standardized Differences |
|---|---|---|---|---|---|---|
| (N = 43,332) | (N = 1,629,920) | (N = 43,332) | (N = 43,332) | |||
| Age group (%) | ||||||
| 65–74 | 18.0 | 52.1 | 76.5 | 18.0 | 18.0 | 0.00 |
| 75–84 | 45.8 | 34.0 | 24.4 | 45.8 | 45.8 | 0.02 |
| ≥85 | 36.3 | 14.0 | 53.2 | 36.3 | 36.2 | 0.12 |
| Gender (%) | ||||||
| Female | 78.0 | 62.1 | 35.1 | 78.0 | 78.0 | 0.00 |
| Race (%) | ||||||
| White | 93.7 | 88.2 | 19.3 | 93.7 | 93.7 | 0.00 |
| Black | 3.4 | 7.3 | 17.4 | 3.4 | 3.4 | 0.22 |
| Hispanic | 1.1 | 1.5 | 2.9 | 1.1 | 1.2 | 0.56 |
| Other | 1.8 | 3.1 | 8.4 | 1.8 | 1.7 | 0.76 |
| Residency status (%) | ||||||
| Nursing home | 19.5 | 5.4 | 43.6 | 19.5 | 19.5 | 0.00 |
| Personal income status (%) | ||||||
| Low income | 22.8 | 12.8 | 26.4 | 22.8 | 22.8 | 0.00 |
| Area median income | ||||||
| <$30,000 | 20.4 | 19.1 | 3.4 | 20.4 | 20.0 | 1.10 |
| $30,000–$44,999 | 38.2 | 37.4 | 1.6 | 38.2 | 38.6 | 0.80 |
| $45,000–$59,999 | 21.8 | 22.2 | 1.0 | 21.8 | 21.6 | 0.41 |
| $60,000–$74,999 | 10.7 | 11.4 | 2.3 | 10.7 | 10.8 | 0.52 |
| $75,000+ | 9.0 | 10.0 | 3.4 | 9.0 | 9.1 | 0.24 |
| Year of fracture (%) | ||||||
| 2006 | 28.4 | NA | 28.4 | NA | ||
| 2007 | 26.0 | NA | 26.0 | NA | ||
| 2008 | 23.5 | NA | 23.5 | NA | ||
| 2009 | 22.1 | NA | 22.1 | NA | ||
| Geographic region (%) | ||||||
| Pacific | 9.7 | 11.0 | 4.1 | 9.7 | 9.7 | 0.17 |
| Mountain | 5.2 | 5.5 | 1.3 | 5.2 | 5.2 | 0.13 |
| West North Central | 8.4 | 7.7 | 2.5 | 8.4 | 8.7 | 1.07 |
| East North Central | 17.2 | 17.6 | 0.9 | 17.2 | 17.2 | 0.00 |
| West South Central | 11.3 | 10.8 | 1.4 | 11.3 | 11.5 | 0.72 |
| East South Central | 7.4 | 6.8 | 2.3 | 7.4 | 7.3 | 0.27 |
| South Atlantic | 21.2 | 21.2 | 0.1 | 21.2 | 20.8 | 0.81 |
| Middle Atlantic | 13.9 | 13.7 | 0.6 | 13.9 | 14.1 | 0.43 |
| New England | 5.6 | 5.6 | 0.0 | 5.6 | 5.4 | 0.88 |
| Rural area (%) | 27.5 | 26.5 | 2.3 | 27.5 | 27.1 | 0.81 |
Note: NA = not applicable.
Table 2 shows the differences in health care expenditures, health services utilization, skilled nursing facility residence, comorbidities, and fracture risk between fracture cases and comparators (please see Supplementary Appendix A for more details), before and after matching. The matching procedure produced good balance between groups even though none of the factors in Table 2 were explicitly included in the HDPS algorithm.
Table 2.
Health Services Utilization and Comorbidities
| Baseline Characteristics | Hip Fractures | All Eligible Controls | Standardized Differences | Matched Fractures | Matched Comparators | Standardized Differences |
|---|---|---|---|---|---|---|
| (N = 43,332) | (N = 1,629,920) | (N = 43,332) | (N = 43,332) | |||
| Health care expenditures ($) | ||||||
| Mean | 8,707 | 6,742 | 13.0 | 8,707 | 8,424 | 1.9 |
| Standard deviation | 15,431 | 14,848 | 15,431 | 14,498 | ||
| Any hospitalization (%) | 28.4 | 19.1 | 22.2 | 28.4 | 27.6 | 1.78 |
| Hospital days | ||||||
| Mean | 3.3 | 2.1 | 14.8 | 3.3 | 3.2 | 1.45 |
| Standard deviation | 9.0 | 7.5 | 9.0 | 9.0 | ||
| Number of physician visits | ||||||
| Mean | 28.5 | 23.1 | 21.0 | 28.5 | 28.3 | 0.93 |
| Standard deviation | 27.0 | 24.5 | 27.0 | 26.8 | ||
| SNF stay (%) | 14.5 | 4.6 | 34.2 | 14.5 | 15.3 | 2.22 |
| Home health care (%) | 15.9 | 8.2 | 23.8 | 15.9 | 14.4 | 4.02 |
| Charlson comorbidity scores (%) | ||||||
| 0 | 39.3 | 50.8 | 23.2 | 39.3 | 40.1 | 1.53 |
| 1-2 | 27.3 | 26.5 | 1.7 | 27.3 | 27.6 | 0.76 |
| 3+ | 33.5 | 22.7 | 24.0 | 33.5 | 32.4 | 2.32 |
| Fracture risk factors (%) | ||||||
| OP diagnosis | 17.2 | 9.6 | 22.3 | 17.2 | 14.6 | 7.15 |
| Fracture | 6.5 | 2.3 | 20.4 | 6.5 | 4.7 | 7.96 |
| Conditions treated with glucocorticoids | 22.4 | 17.9 | 11.3 | 22.4 | 22.2 | 0.55 |
| Falls or fall risk | 37.2 | 22.9 | 31.5 | 37.2 | 34.9 | 4.73 |
Table 3 shows 1-year risks of death, debility, and destitution among beneficiaries who experienced hip fractures and their matched comparators. Hip fractures were associated with a 16% absolute increase in 1-year mortality for all matched pairs in our sample (an IPR of 2.27, 95% CI, 2.20–2.34). Hip fractures were associated with a 17% absolute increase in 1-year mortality (an IPR of 1.67, 95% CI, 1.60–1.75) among nursing home residents, and a 15.8% absolute increase in 1-year mortality (IPR of 2.65, 95% CI, 2.56–2.75) among community-dwelling individuals. It is noteworthy that more than 18% of hip fractures occurred among nursing home residents although these individuals make up only 5% of all beneficiaries. Similarly, hip fractures were associated with a fourfold increase in the likelihood of requiring long-term nursing facility care (IPR, 3.96; 95% CI, 3.77–4.16) and a twofold increase in the probability of entering into low-income status (IPR, 2.14; 95% CI 1.99–2.31).
Table 3.
Death, Debility, and Destitution Following Hip Fracture and Among Matched Comparators
| Outcome Event and Subject Group | N Pairs* | Hip Fractures | Comparators | IPRs‡ | 95% CI§ | ||
|---|---|---|---|---|---|---|---|
| N Events | (%)† | N Events | (%) | ||||
| 1-y mortality | |||||||
| All subjects | 43,332 | 12,413 | (28.6) | 5,470 | (12.6) | 2.27 | 2.20–2.34 |
| Long-term care resident | 8,438 | 3,581 | (42.4) | 2,141 | (25.4) | 1.67 | 1.60–1.75 |
| Community dwelling | 34,894 | 8,832 | (25.3) | 3,329 | (9.5) | 2.65 | 2.56–2.75 |
| Low income | 9,866 | 3,265 | (33.1) | 1,716 | (17.4) | 1.91 | 1.81–2.01 |
| Not low income | 33,466 | 9,148 | (27.3) | 3,754 | (11.2) | 2.44 | 2.35–2.52 |
| Debility (long-term care residency) | |||||||
| Community dwelling | 34,894 | 7,022 | (20.1) | 1,773 | (5.1) | 3.96 | 3.77–4.16 |
| Destitution (newly low income) | |||||||
| Not low income | 33,466 | 2,213 | (6.6) | 1,032 | (3.1) | 2.14 | 1.99–2.31 |
Notes : IPR = incidence proportion ratios.
*Number of hip fracture and comparator matched pairs included in the analysis.
†Percent experiencing each outcome among total hip fractures or comparators in the subject group being analyzed.
‡IPR for the event of interest in hip fracture patients versus comparators.
§95% CI of the IPRs.
Table 4 refers only to hip fracture cases, excluding those either in long-term institutional care (debilitated) or in low-income status (destitute) prior to the fracture. Among this group (N = 28,890), 22,743 (79%) experienced neither debility nor destitution. Table 4 shows the rate of destitution (80%) among those who became debilitated and the rate of debility (60%) among those who became destitute.
Table 4.
Destitution Among Individuals Who Became Debilitated and Debility Among Hip Fracture Patients Who Became Destitute Within 1 Year Following Hip Fracture
| Destitution, N (%) | ||
| Debility | Yes | No |
| 4,343 (80%) | 1,093 (20%) | |
| Debility, N (%) | ||
| Destitution | Yes | No |
| 1,093 (61%) | 711 (39%) | |
Discussion
Hip fractures are followed by elevated risks of death, debility, and destitution. The 1-year absolute risk of mortality was higher for individuals who suffered hip fractures (28.6%), compared with comparator patients who did not suffer a hip fracture (12.6%); excess mortality was 16%, and IPR was 2.27. Similar to our own excess mortality findings, Katelaris and Cumming (9) have estimated 1-year excess mortality to be 17% higher among hip fracture patients compared with people without hip fracture using various analytical methods. However, they found a three to fourfold hazard ratio for the comparators used. A meta-analysis by Haentjens and colleagues (31) reported hazard ratios of 2.87 for women and 3.70 for men, with excess mortality ranging from 2% to 40%, depending on age and gender. These findings were higher than ours in terms of relative risk. Part of this difference could be the differing time frames for the studies. However, some of the difference may arise from differing analytic approaches. The Haentjens and colleagues (31) meta-analysis criticized a number of studies for failure to adequately address confounding. We addressed confounding using a HDPS matching analysis method and were able to show excellent balance in measured covariates that might otherwise contribute to confounding. We know of no other study addressing this topic that uses this technique to minimize confounding in their analysis.
To our knowledge, this study represents the first attempt to use HDPS matching to estimate the proportion of individuals experiencing a hip fracture who actually transition from being community dwelling to living in long-term care following hip fracture. In this study, about 20% of hip fracture patients who were community dwelling at the time of their fracture became debilitated, entering long-term care within 1 year—an absolute excess of 15% and a fourfold relative increase over the risk of comparators, and twice as many individuals who experienced hip fracture became newly eligible for Medicaid or low-income subsidies as did the matched comparators. In addition, we find that hip fracture patients who ended up Medicaid dependent were four times more likely to be admitted to long-term nursing care prior to dependence than hip fracture patients who did not become Medicaid dependent. Although we cannot claim a causal pathway between hip fracture, long-term nursing facility care, and eventual Medicaid dependence, these findings suggest a relationship between long-term care use and eventual Medicaid dependence.
Thus, a hip fracture in the Medicare aged population is a life-changing event. These results are particularly disquieting for several reasons. The older adult and elderly population, those most vulnerable to hip fractures, is projected to grow by 60% by 2025 (32). Also, rates of osteoporosis are projected to rise over the next decade (33). An aging population and increased rates of osteoporosis could lead to an increase in fractures, potentially leading to increases in direct medical expenditure, societal burden, death, debility, destitution, and a decrease in quality of life for this population if initiatives to improve the treatment of osteoporosis and the prevention of fractures are not implemented.
Although we know of no other studies that use HDPS matching to estimate the proportion of patients who remain residents of a long-term care facility a year after hip fracture incidence, a study by Brown and colleagues (34) on long-term care dependence following stroke has findings similar to those of our own study (34). We attempted to identify a similar study in stroke patients for several reasons. Strokes, like hip fractures, affect a large number of people over the age of 65 years (35,36), they are both devastating events with similar mortality outcomes (approximately 25% 1-year mortality and 50% 5-year mortality) (2,34); they both can lead to long-term care admission (5,34), and they are both preventable (2,37). Brown and colleagues (34) found that 18% of individuals who experienced a stroke while not residing in a nursing home were admitted and remained in long-term care a year after the event, whereas we find that approximately 20% of surviving hip fracture patients remained in long-term care 1-year post event. These findings may have policy implications and are important not only because of the increased rate of long-term care dependence we find after hip fracture compared to stroke but also because of the higher degree of hip fracture prevention, up to 50%, provided by pharmacological interventions (2,17,38).
We included individuals who were residing in nursing home facilities and who were receiving low income in our calculation of 1-year absolute risk of mortality. As expected, rates of mortality were higher for these groups. The absolute increase in 1-year mortality for nursing facility residents following hip fracture was only slightly larger than the absolute increase in 1-year mortality for community-dwelling individuals. However, the IPRs of mortality following hip fracture were higher for community-dwelling individuals than for nursing facility residents. This suggests that suffering a hip fracture as a community-dwelling individual as opposed to a nursing facility resident is a relatively worse event in terms of additional mortality risk.
Although we used HDPS matching to control for confounding in this study and were able to achieve very good balance of sociodemographic as well as other measured health-related characteristics between our hip fracture and non-hip fracture cohort using this study design, this study is ultimately observational. In addition, although HDPS has the added benefit of controlling for a relatively larger number of patient characteristics than other observational methods, we still may not have accounted for all observable and unobservable characteristics of patients. Therefore, although we found a strong relationship between hip fracture and death, debility, and destitution, our results could still be subject to some degree of omitted variable bias. In addition, a recent publication by Koroukian and colleagues (39) suggests that our use of the state buy-in variable to estimate newly eligible Medicaid recipients (destitution) may be biased between 5% and 11%.
We used Medicare data to conduct this study and were able to compare outcomes of a large number of patients who suffered a hip fracture with a large number of patients who did not suffer hip fracture. The data we used are also nationally representative of race, gender, and other sociodemographic characteristics. However, because we relied on Medicare data and because of our exclusion criteria, we were only able to explore the effects of hip fracture on individuals who were 65 years of age and older. Although this age cohort is the most likely to experience hip fracture, this study results and the potential policy and treatment implications of those results are perhaps not generalizable to other important groups likely to suffer hip fracture such as younger postmenopausal women.
Conclusions
A substantial body of evidence indicates that nearly 50% of hip fractures can be prevented through the use of antiosteoporosis medication (2,17,38), a substantially larger percent reduction than the 17% reduction in stroke associated with the use of pharmaceutical interventions (37,40). In light of these differences, we do not advocate for a decrease in attention to stroke prevention, but rather an increase in attention to hip fracture prevention. This information and our findings could potentially allow policy makers, clinicians, and public health researchers and decision makers to estimate the potential health and economic benefits of interventions to reduce hip fracture rates. Additionally, admission into long-term care residence and loss of independence as a result of hip fracture are an undesirable outcome for the elderly population with some studies reporting a majority of older women preferring death to nursing home admission (41). Given the increased probability of death and debility following hip fracture, the increased financial burden and loss of quality of life for individuals and families as a result of long-term care residence, and the costs to the Medicare and Medicaid programs, much greater effort at promoting prevention, particularly among high-risk individuals is warranted.
Supplementary Material
Supplementary material can be found at: http://biomedgerontology.oxfordjournals.org/
Funding
This research was supported by a contract between University of Alabama at Birmingham and Amgen Inc. Only the authors from University of Alabama at Birmingham had access to the Medicare data used. The analysis, presentation, and interpretation of the results were solely the responsibility of the authors. J.R.C. is supported by the National Institutes of Health (AR053351).
References
- 1. Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51:364–370 [DOI] [PubMed] [Google Scholar]
- 2. Curtis JR, Arora T, Matthews RS, et al. Is withholding osteoporosis medication after fracture sometimes rational? A comparison of the risk for second fracture versus death. J Am Med Dir Assoc. 2010;11:584–591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dolan MM, Hawkes WG, Zimmerman SI, et al. Delirium on hospital admission in aged hip fracture patients: prediction of mortality and 2-year functional outcomes. J Gerontol A Biol Sci Med Sci. 2000;55:M527–M534 [DOI] [PubMed] [Google Scholar]
- 4. Handoll HH, Cameron ID, Mak JC, Finnegan TP. Multidisciplinary rehabilitation for older people with hip fractures. Cochrane Database Syst Rev. 2009:CD007125. [DOI] [PubMed] [Google Scholar]
- 5. Nguyen-Oghalai TU, Ottenbacher KJ, Kuo YF, et al. Disparities in utilization of outpatient rehabilitative care following hip fracture hospitalization with respect to race and ethnicity. Arch Phys Med Rehabil. 2009;90:560–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc. 2002;50:1644–1650 [DOI] [PubMed] [Google Scholar]
- 7. Lyons AR. Clinical outcomes and treatment of hip fractures. Am J Med. 1997;103:51S–63S [DOI] [PubMed] [Google Scholar]
- 8. Cumming RG, Nevitt MC, Cummings SR. Epidemiology of hip fractures. Epidemiol Rev. 1997;19:244–257 [DOI] [PubMed] [Google Scholar]
- 9. Katelaris AG, Cumming RG. Health status before and mortality after hip fracture. Am J Public Health. 1996;86:557–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD. Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int. 2011;22:2439–2448 [DOI] [PubMed] [Google Scholar]
- 11. Services USDoHaH Bone Health and Osteoporosis: A Report to the Surgeon General. Rockville MD: U.S. Department of Health and Human Services; 2004. [Google Scholar]
- 12. Grabowski DC, O’Malley AJ, Barhydt NR. The costs and potential savings associated with nursing home hospitalizations. Health Aff (Millwood). 2007;26:1753–1761 [DOI] [PubMed] [Google Scholar]
- 13. Gleckman H. What About Long-Term Care? Washington, DC: Urban Institute; 2009 [Google Scholar]
- 14. Johnson R, Park J. Who Purchases Long-Term Care Insurance? Washington, DC: Urban Institute; 2011 [Google Scholar]
- 15. Kaiser Medicaid: A Primer 2009. Menlo Park, CA: The Kaiser Commission on Medicaid and the Uninsured; 2009. [Google Scholar]
- 16. Black DM, Cummings SR, Karpf DB, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348 1535–1541 [DOI] [PubMed] [Google Scholar]
- 17. Black DM, Thompson DE, Bauer DC, et al. Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab. 2000;85:4118–4124 [DOI] [PubMed] [Google Scholar]
- 18. Centers for Medicare & Medicaid Services, CfMMS Chronic Condition Warehouse. 2012. http://www.ccwdata.org/index.htm, 2012. [Google Scholar]
- 19. Kilgore ML, Morrisey MA, Becker DJ, et al. Health care expenditures associated with skeletal fractures among Medicare beneficiaries, 1999–2005. J Bone Miner Res. 2009;24:2050–2055 [DOI] [PubMed] [Google Scholar]
- 20. Taylor AJ, Gary LC, Arora T, et al. Clinical and demographic factors associated with fractures among older Americans. Osteoporos Int. 2011;22:1263–1274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yun H, Kilgore M, Curtis J, et al. Identifying types of nursing facility stays using medicare claims data: an algorithm and validation. Health Serv Outcomes Res Methodol. 2010;10:100–110 [Google Scholar]
- 22. Schneeweiss S, Rassen JA, Glynn RJ, Avorn J, Mogun H, Brookhart MA. High-dimensional propensity score adjustment in studies of treatment effects using health care claims data. Epidemiology. 2009;20:512–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Guo S, Fraser M. Propensity Score Analysis - Statistical Methods and Applications. 1st ed Thousand Oaks, CA: SAGE; 2009 [Google Scholar]
- 24. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619 [DOI] [PubMed] [Google Scholar]
- 25. Kilgore M, Smith W, Curtis J, et al. Evaluating comorbidity scores based on health service expenditures. MMWR. 2012;2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stalenhoef PA, Diederiks JP, Knottnerus JA, Kester AD, Crebolder HF. A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol. 2002;55:1088–1094 [DOI] [PubMed] [Google Scholar]
- 27. Tinetti ME, Williams TF, Mayewski R. Fall risk index for elderly patients based on number of chronic disabilities. Am J Med. 1986;80:429–434 [DOI] [PubMed] [Google Scholar]
- 28. Austin PC. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med. 2008;27:2037–2049 [DOI] [PubMed] [Google Scholar]
- 29. Lee W. Propensity score matching and variations on the balancing test: a working paper. Melbourne Institute of Applied Economic and Social Research; 2006 [Google Scholar]
- 30. Rosenbaum P, Rubin D. Constructing a control group using multivariate matched sampling methods. Am Stat. 1985;39:33–38 [Google Scholar]
- 31. Haentjens P, Magaziner J, Colón-Emeric CS, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152:380–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Day J. Population Projections of the United States by Age, Sex, Race, and Hispanic Origin: 1995–2050. Washington DC: Bureau of the Census; 1996 [Google Scholar]
- 33. Foundation NO National Osteoporosis Foundation 2002 America’s Bone Health: The State of Osteoporosis and Low Bone Mass in Our Nation. Washington DC: National Osteoporosis Foundation; 2002 [Google Scholar]
- 34. Brown RD, Jr, Ransom J, Hass S, et al. Use of nursing home after stroke and dependence on stroke severity: a population-based analysis. Stroke. 1999;30:924–929 [DOI] [PubMed] [Google Scholar]
- 35. Centers for Disease Control and Prevention Prevalence of Stroke — United States, 2006–2010. Atlanta GA: Centers for Disease Control and Prevention; 2012 [Google Scholar]
- 36. Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. BMJ. 2003;326:1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Black DM, Delmas PD, Eastell R, et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–1822 [DOI] [PubMed] [Google Scholar]
- 39. Koroukian SM, Dahman B, Copeland G, Bradley CJ. The utility of the state buy-in variable in the Medicare denominator file to identify dually eligible Medicare-Medicaid beneficiaries: a validation study. Health Serv Res. 2010;45:265–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. O’Regan C, Wu P, Arora P, Perri D, Mills EJ. Statin therapy in stroke prevention: a meta-analysis involving 121,000 patients. Am J Med. 2008;121:24–33 [DOI] [PubMed] [Google Scholar]
- 41. Salkeld G, Cameron ID, Cumming RG, et al. Quality of life related to fear of falling and hip fracture in older women: a time trade off study. BMJ. 2000;320:341–346 [DOI] [PMC free article] [PubMed] [Google Scholar]