Abstract
Objective
To evaluate whether Medicare Part D has reduced racial/ethnic disparities in prescription drug utilization and spending.
Data
Nationally representative data on white, African American, and Hispanic Medicare seniors from the 2002–2009 Medical Expenditure Panel Survey are analyzed. Five measures are examined: filling any prescriptions during the year, the number of prescriptions filled, total annual prescription spending, annual out-of-pocket prescription spending, and average copay level.
Study Design
We apply the Institute of Medicine's definition of a racial/ethnic disparity and adopt a difference-in-difference-in-differences (DDD) estimator using a multivariate regression framework. The treatment group consists of Medicare seniors, the comparison group, adults without Medicare aged 55–63 years.
Principal Findings
Difference-in-difference-in-differences estimates suggest that for African Americans Part D increased the disparity in annual spending on prescription drugs by $258 (p = .011), yet had no effect on other measures of prescription drug disparities. For Hispanics, DDD estimates suggest that the program reduced the disparities in annual number of prescriptions filled, annual total and out-of-pocket spending on prescription drugs by 2.9 (p = .077), $282 (p = .019) and $143 (p < .001), respectively.
Conclusion
Medicare Part D had mixed effects. Although it reduced Hispanic/white disparities related to prescription drugs among seniors, it increased the African American/white disparity in total annual spending on prescription drugs.
Keywords: Medicare Part D, prescription drugs, utilization and spending, racial/ethnic disparities
Medicare Part D is the single most important extension to Medicare since the program's inception. Part D, which took effect in January 2006, makes prescription drug insurance available to all beneficiaries at a reasonable premium. Under Part D every beneficiary can purchase a drug insurance plan from a range of plans offered by private health insurers, with premium subsidies available to persons with low income and few resources.
In this article we examine whether Medicare Part D has had any effects on racial/ethnic disparities in prescription drug use and spending. Using nationally representative data from the 2002–2009 Medical Expenditure Panel Survey (MEPS), we employ a difference-in-difference-in-differences (DDD) methodology to isolate the effects of Part D, comparing changes in racial/ethnic disparities among Medicare seniors that occurred following the introduction of Part D to changes in racial/ethnic disparities among adults without Medicare, aged 55–63 years, over the same period.
Background
Research has documented that prior to 2006 there were substantial racial/ethnic disparities in the utilization of prescription drugs among older adults (Reed, Hargraves, and Cassil 2010; Briesacher, Limcangco, and Gaskin 2004; Safran et al. 2005; Gaskin et al. 2006; Gellad, Haas, and Safran 2007). Studies showed that whites used more prescription drugs and had higher total prescription drug expenditures than either African Americans or Hispanics. For instance, among beneficiaries without drug coverage, African Americans and Hispanics used 10–40 percent fewer medications, on average, compared to whites, and they spent up to 60 percent less on their medications (Briesacher et al. 2004).
Not surprisingly, these differences in utilization and spending were highly correlated with self-reports of being unable to afford medications, as well as self-reports of cost-related medication nonadherence (CRN) (Reed et al. 2010; Wilson, Axelsen, and Tang 2005; Soumerai et al. 2006; Safran et al. 2010; Gellad, Haas, and Safran 2007). African Americans and Hispanics were particularly vulnerable to experiencing problems paying for their medications (Gellad, Haas, and Safran 2007). In 2003, 25 percent of African American and Hispanic seniors, compared to 11 percent of white seniors, reported spending less on food and other basic needs to pay for prescription drugs, and 40 percent of African Americans and Hispanics reported cost as their reason for nonadherence to prescribed medications, compared to 28 percent of whites (Gellad, Haas, and Safran 2007). CRN is known to increase the risk of adverse health events, such as a heart attack or stroke, as well as the complications arising from chronic health conditions, such as diabetes (Heisler et al. 2004; Sokol et al. 2005; Gibson et al. 2010; Jensen and Li 2012).
Previous studies document that Medicare Part D decreased beneficiaries' out-of-pocket costs by approximately 13–18 percent (Lichtenberg and Sun 2007; Madden et al. 2008; Levy and Weir 2009; Safran et al. 2010; Engelhardt and Gruber 2011; Liu et al. 2011). Yet it is not clear whether Part D has affected racial/ethnic disparities in prescription drug use and spending. This study examines this issue.
Methods
Using data from the MEPS, we estimate the effects of Medicare Part D on disparities in prescription drug utilization and spending using a pre period and post period with comparison group design, applying the Institute of Medicine's definition of a disparity. The pre period for our analysis covers 2002–2005 and the post period covers 2006–2009. Medicare beneficiaries aged 65 years and older (at the beginning of each year) comprise the “treatment” group, and adults aged 55–63 years (at the beginning of the year) who do not have Medicare comprise the “comparison” group. In our analysis, we do not follow the same individuals across the pre period and post period. That is not possible to do with MEPS. Rather, we compare disparities in prescription drug utilization and spending among Medicare seniors during the pre period to disparities in these measures among Medicare seniors during the post period, and then examine whether the changes that occurred were any different from the changes in disparities that occurred within the comparison group. Figure 1 provides a schematic of our research design and sample counts.
Figure 1.
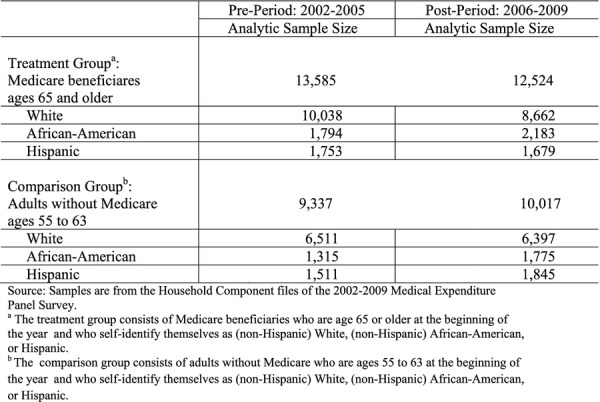
Counts of Individuals in the Treatment and Comparison Groups before and after Medicare Part D (Overall Total Sample of 45,463 Individuals).
Data
We use the Household Component (HC) files of the 2002–2009 MEPS. MEPS is an ongoing, nationally representative survey of the U.S. civilian, noninstitutionalized population, conducted annually by the Agency for Healthcare Research and Quality (AHRQ) (Cohen et al. 1997). We limit our attention to individuals who self-report being (non-Hispanic) African American, Hispanic, or (non-Hispanic) white, based on MEPS's questions regarding race and ethnicity. Other minority groups are not examined due to their small sample counts in MEPS.
Our final analytic sample includes a total of 45,463 MEPS respondents, 26,109 of whom are in the treatment group and 19,354 of whom are in the comparison group. Within the treatment group there were 13,585 individuals (whites = 10,038; African Americans = 1,794; Hispanics = 1,753) who were surveyed between 2002 and 2005 and 12,524 individuals (whites = 8,662; African Americans = 2,183; and Hispanics = 1,679) who were surveyed between 2006 and 2009. In the comparison group there were 9,337 individuals (whites = 6,511; African Americans = 1,315; Hispanics = 1,511) who were surveyed between 2002 and 2005 and 10,017 individuals (whites = 6,397; African Americans = 1,775; Hispanics = 1,845) who were surveyed between 2006 and 2009.
Variable-specific nonresponse rates generally ranged from 0 to 5 percent. Two summary indices of overall physical and mental health, however, showed nonresponse rates in the 7–9 percent range, specifically, the norm-based physical component summary scale (NBPCS) and the norm-based mental component summary scale (NBMCS), both calculated from Version 2 of the Short Form 12 Health Survey (SF12-V2) (Ware et al. 2002). We used a multiple imputation technique (Little and Rubin 2002) to estimate the missing values for these variables and created five complete sets of data, reestimating the regression models for each set, re-calculating disparities on each of these complete sets of data, and then taking the average according to rules in Little and Rubin (2002) to incorporate the uncertainty of the missing data into the standard errors.
Throughout, we adjust for the clustered and stratified survey design of MEPS and weight all estimates using the AHRQ-supplied weights. We used Stata 12 for all analyses.
Dependent and Independent Variables
We examine racial/ethnic disparities in five measures: (1) whether any prescriptions are filled during the year; (2) the number of prescriptions (including refills) filled during the year; (3) total positive annual spending on prescription drugs; (4) out-of-pocket positive annual spending on prescription drugs; and (5) average copay for prescription drugs, defined as the ratio of out-of-pocket spending to total spending. In the utilization and expenditures sections of MEPS, questions were asked regarding each prescription filled during the previous round, if any were, and the total and out-of-pocket cost of each prescription. With each participant's consent, MEPS staff verified the detailed prescription information reported using actual pharmacy records. If consent was not granted, the data are the participant's own self-reported information. Any prescriptions filled and the annual number of prescriptions filled are from the utilization section of MEPS, and total and out-of-pocket annual spending on prescription drugs are from the expenditures section of MEPS. Before beginning the analysis, total and out-of-pocket spending were converted to inflation-adjusted 2007 dollars using the all-items Consumer Price Index.
Andersen's conceptual framework guides our choice of explanatory variables for the models to be estimated (Andersen 1968, 1995). Each model includes need-related variables, such as age, gender, and measures of health and functioning. We also include predisposing and enabling factors such as marital status, education, income, health insurance, location, and language. To control for health and functioning, we include a range of variables. Two (0,1) indicators for whether self-rated health and self-rated mental health, respectively, are fair or poor, as opposed to good or better, are included in the models, as well as (0,1) indicators for whether the individual reports any heart problems, diabetes, asthma, arthritis, or hypertension. For physical functioning, we include the number of functional limitations reported. We also include two summary indices of overall physical and mental health, specifically, the NBPCS and the NBMCS. Marital status is measured with a (0,1) indicator for whether the individual is currently married. Education is measured by a series of mutually exclusive (0,1) indicators for whether education is less than high school, college degree, graduate school degree, or another degree, with high school serving as the reference category. Household income is measured using four mutually exclusive categories: poor or near poor (household income is less than 125 percent of the federal poverty level [FPL]), low income (household income is 125–199 percent of FPL), middle income (household income is 200–399 percent of FPL), and high income (household income is at least 400 percent of FPL), with low income serving as the reference category. For health insurance we include a (0,1) indicator for whether the individual reports (at any time during the past year) having Medicaid, as well as (0,1) indicators describing the nature of their private insurance holdings, specifically, whether the individual holds HMO coverage, private non-HMO insurance, or has no private insurance, with the last of these serving as the reference category. We also control for whether the individual resides in an urban area, and his or her US Census region, with the Northeast as the reference category. Finally, all models adjust for English language fluency, with a (0,1) indicator for whether the individual conducted his or her MEPS interview in English. Table 1 provides descriptive statistics on the variables, reported separately for the treatment and comparison group.
Table 1.
Characteristics of the Comparison Group (Individuals without Medicare, Aged 55–63 years) and the Treatment Group (Medicare Beneficiaries, Aged 65 years and Older) before Part D
|
Comparison† (N = 9,337) |
Treatment‡ (N = 13,585) |
||||
|---|---|---|---|---|---|
| Description | Mean | SE | Mean | SE | |
| Dependent variables | |||||
| Any prescriptions filled* | 1 if any prescription gets filled during the year | 0.81 | 0.01 | 0.93 | 0.00 |
| Number of pres. drugs* | Annual number of prescriptions filled | 22.14 | 0.46 | 30.18 | 0.49 |
| Cost of pres. drugs* | Total cost of prescription drugs during the year | 1,602.24 | 37.46 | 2,056.75 | 54.12 |
| Out-of-pocket cost of drugs* | Annual out-of-pocket cost of prescription drugs | 590.27 | 15.87 | 1,058.12 | 21.65 |
| Copay* | Annual out-of-pocket cost/annual total cost | 0.46 | 0.01 | 0.58 | 0.01 |
| Independent variables | |||||
| Need-related | |||||
| Age* | Age at the beginning of the year | 58.66 | 0.05 | 74.40 | 0.11 |
| Female* | 1 if individual is female | 0.55 | 0.01 | 0.59 | 0.01 |
| Poor/Fair health* | 1 if individual rates her health as poor/fair | 0.18 | 0.01 | 0.25 | 0.01 |
| Poor/Fair mental health | 1 if individual rates his mental health as poor/fair | 0.07 | 0.00 | 0.09 | 0.00 |
| PCS* | Physical component summary SF12 | 46.74 | 0.19 | 40.60 | 0.16 |
| MCS | Mental component summary SF12 | 51.70 | 0.16 | 51.62 | 0.15 |
| Function_index*,§ | Index of physical limitation | 3.68 | 0.14 | 8.93 | 0.16 |
| Diabetes* | 1 if individual diagnosed with diabetes | 0.14 | 0.01 | 0.19 | 0.01 |
| Heart* | 1 if individual has any heart problem | 0.17 | 0.01 | 0.34 | 0.01 |
| Asthma | 1 if individual diagnosed with asthma | 0.11 | 0.01 | 0.09 | 0.00 |
| Arthritis* | 1 if individual diagnosed with arthritis | 0.41 | 0.01 | 0.55 | 0.01 |
| High blood pressure* | 1 if individual diagnosed with high blood pressure | 0.51 | 0.01 | 0.65 | 0.01 |
| Marital status | |||||
| Married* | 1 if individual is married | 0.72 | 0.01 | 0.54 | 0.01 |
| Education | |||||
| Less than high school* | 1 if individual has no high school diploma | 0.12 | 0.01 | 0.27 | 0.01 |
| High school (omitted) | 1 if individual has high school diploma | 0.51 | 0.01 | 0.50 | 0.01 |
| College and graduate school* | 1 if individual has a college or graduate degree | 0.30 | 0.01 | 0.18 | 0.01 |
| Other degree* | 1 if individual has other degrees | 0.08 | 0.01 | 0.05 | 0.00 |
| Household income level | |||||
| Poor or near poor* | 1 if household income < 125% FPL | 0.10 | 0.01 | 0.17 | 0.01 |
| Low income (omitted)* | 1 if household income is 125–199% FPL | 0.08 | 0.00 | 0.20 | 0.01 |
| Middle income* | 1 if household income is 200–399% FPL | 0.25 | 0.01 | 0.30 | 0.01 |
| High income* | 1 if household income ≥400% FPL | 0.57 | 0.01 | 0.32 | 0.01 |
| Health insurance | |||||
| Medicaid* | 1 if individual has Medicaid | 0.05 | 0.00 | 0.08 | 0.00 |
| Private HMO insurance* | 1 if individual holds private HMO insurance | 0.31 | 0.01 | 0.09 | 0.01 |
| Private non-HMO insurance | 1 if individual holds private non-HMO insurance | 0.50 | 0.01 | 0.44 | 0.01 |
| No private* insurance (omitted)* | 1 if individual holds no private insurance | 0.19 | 0.01 | 0.46 | 0.01 |
| Location | |||||
| Northeast | 1 if individual lives in Northeast | 0.20 | 0.01 | 0.21 | 0.01 |
| Midwest | 1 if individual lives in Midwest | 0.24 | 0.01 | 0.23 | 0.01 |
| South | 1 if individual lives in South | 0.37 | 0.01 | 0.37 | 0.01 |
| West | 1 if individual lives in West | 0.19 | 0.01 | 0.19 | 0.01 |
| Metropolitan area | 1 if individual lives in a statistical metropolitan area | 0.80 | 0.01 | 0.78 | 0.01 |
| Language | |||||
| English language | 1 if language of the interview is English | 0.97 | 0.00 | 0.96 | 0.00 |
Note. The variables listed are the explanatory variables in the estimated regression models. Tables A1–A2 report detailed descriptive statistics stratified by race and ethnicity for the comparison and treatment groups for the periods before and after Medicare Part D.
The mean of this variable differs significantly between the comparison and treatment group at the alpha = .01 level.
Comparison group consists of adults without Medicare, aged 55–63 years, who self-report being white, African American, or Hispanic.
Treatment group consists of Medicare beneficiaries, aged 65 years and older, who self-report being white, African American, or Hispanic.
Function-Index is an index of limitations on activities of daily living (ADLs) and instrumental activities of daily living (IADLs).
Source: Data are from the household component files of the 2002–2005 Medical Expenditure Panel Survey.
Institute of Medicine (IOM) Definition and Measurement of a Disparity
We adopt the IOM definition of a racial or ethnic disparity (IOM 2002).1 In its 2002 report, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, the IOM defines a disparity as “a difference in access or treatment provided to members of different racial or ethnic groups that is not justified by the underlying health conditions or treatment preferences of patients.” McGuire et al. (2006) and Cook et al. (2010) describe the methods for implementing this definition, and we apply their methods here.
Briefly, we use a four-step procedure to calculate disparities. First, for each outcome measure, we fit a multivariate regression using the explanatory variables described above that allows for the effects of key explanatory variables to vary by race and ethnicity. Second, we transform the distribution of the health status explanatory variables for each minority group to be the same as their distribution among whites, while leaving the non-need-related variables unchanged. These transformations are made using the “rank-and-replace” method described by Cook et al. (2010, p. 831). Specifically, we apply Cook et al.'s rank-and-replace techniques to the health status summary index score obtained from the model we estimate in step one. Third, we then use the fitted regression from step one to calculate predicted values of the outcome measure for each minority group member using their transformed health status summary index score along with their actual values for other variables in the model. Finally, we average these predictions by population group and calculate a disparity in the outcome measure as the difference between the average hypothetical value for that outcome in the minority group and the average value for that outcome among whites. In the treatment group, disparities are measured before Part D and then after Part D, and the same is done in the comparison group. To measure the standard errors for the IOM predictions, we replicated our entire sample 100 times (with replacement) using Stata's bootstrapping procedure for the case of complex survey design (Kolenikov 2010), reestimated the IOM disparities with each bootstrapped sample, and then calculated the standard deviation of those 100 estimates as the measure of their standard error.
Difference-in-Difference-in-Differences and Regression Framework for Evaluation
We adopt a DDD methodology to estimate Part D's effects on racial/ethnic disparities in prescription utilization, prescription drug spending, and beneficiary copay levels. DDD methods are valid if, in the absence of Part D, both the treatment and comparison groups would have experienced similar trends in racial/ethnic disparities over the period. Before estimating the models we consider this issue and formally test for trend similarities in the outcome variables during the years leading up to Part D (see Table 2).
Table 2.
Trends in the Unadjusted Differences between whites and African Americans, and between whites and Hispanics, for Five Outcomes Related to Prescription Drugs before the Introduction of Medicare Part D
|
whites vs African Americans |
whites vs Hispanics |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome Measures | Difference 2002–2003 | Difference 2004–2005 | Difference over Time | DDD | t (p-value) | Difference 2002–2003 | Difference 2004–2005 | Difference Over Time | DDD | t (p-value) |
| Any prescriptions filled | ||||||||||
| Treatment (65+) | 4% | 1% | −3% | −6% | −1.49 | 5% | 4% | −1% | 0% | −0.20 |
| Comparison (55–63) | 3% | 6% | 3% | (0.135) | 13% | 12% | −1% | (0.844) | ||
| Total number Rx filled* | ||||||||||
| Treatment (65+) | −2.92 | −3.10 | −0.18 | −2.18 | −0.67 | 3.22 | 1.77 | −1.45 | −1.03 | −0.37 |
| Comparison (55–63) | −3.27 | −1.27 | 2.00 | (0.501) | 3.60 | 3.18 | −0.42 | (0.712) | ||
| Rx total spending† | ||||||||||
| Treatment (65+) | −77.98 | 69.32 | 147.30 | 18.85 | 0.08 | 228.42 | 305.21 | 76.79 | 4.53 | 0.02 |
| Comparison (55–63) | −25.37 | 130.08 | 128.45 | (0.933) | 260.40 | 332.66 | 72.26 | (0.986) | ||
| Rx out-of-pocket spending‡ | ||||||||||
| Treatment (65+) | 178.06 | 159.03 | −19.03 | −83.32 | −0.77 | 242.95 | 285.14 | 42.19 | 130.12 | 1.05 |
| Comparison (55–63) | 16.55 | 80.84 | 64.29 | (0.295) | 105.89 | 17.96 | −87.93 | (0.295) | ||
| Average copay§ | ||||||||||
| Treatment (65+) | 9% | 6% | −3% | −3% | −0.80 | 7% | 8% | 1% | 1% | 0.32 |
| Comparison (55–63) | −2% | −2% | 0% | (0.421) | −10% | −10% | 0% | (0.750) | ||
Note. Estimates are for comparison and treatment groups and are based on racial/ethnic differences in unadjusted averages of outcomes of interest prior to PartD. For instance, during 2002–2003 period, on average, 93% of older whites versus 89% of African Americans had any prescriptions filled (difference = 93–89% = 3%). During 2004–2005, there is 1% difference between older whites and older African Americans in having any prescriptions filled (difference = 93–92% = 1%). However, among comparison group, the average difference between whites and African Americans rose from 3% in 2002–2003 to 6% in 2004–2005. Although the disparity trends were not the same between the comparison and treatment group, the diverging trends were not statistically significant. Comparison group consists of adults without Medicare, aged 55–63, who self-report being white, African American, or Hispanic. Treatment group consists of Medicare beneficiaries, aged 65 or older, who self-report being white, African American, or Hispanic.
Unadjusted differences in average number of prescriptions filled over the period between whites and African Americans, and whites and Hispanics who had at least one prescription filled.
Unadjusted differences in average total cost of prescriptions over the period between whites and African Americans, and whites and Hispanics who had at least one prescription filled.
Unadjusted differences in average out-of-pocket cost of prescriptions over the period between whites and African Americans, and whites and Hispanics who had positive out-of-pocket cost.
Unadjusted differences in average copay (out-of-pocket/total cost) over the period between whites and African Americans, and whites and Hispanics who had positive total and out-of-pocket cost.
Source: Data are from the household component files of the 2002–2003 and 2004–2005 Medical Expenditure Panel Survey.
The regression equation below illustrates the basic structure of the models we estimate before calculating IOM disparities. In this equation, Medicare seniors comprise the “treatment group,” and adults without Medicare, aged 55–63 years, comprise the “comparison group”:
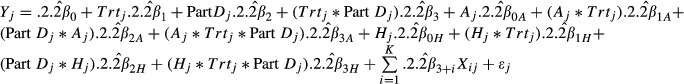 |
Here, j indexes an individual and Y is one of the outcome measures, such as total annual spending on drugs. “Part D” is a (0,1) indicator for whether the individual was surveyed after January 2006 or before then (1 if after, 0 if before), and “Trt” is a (0,1) indicator for membership in the treatment group (1 if yes, 0 if no). “A” and “H” are (0,1) indicators for whether the individual is African American or Hispanic, respectively (1 if yes, 0 if no). Finally, the Xi's are other relevant explanatory variables, such as demographic and socioeconomic characteristics, and for some of the Xi's, their interactions with the race/ethnicity indicators.2
For any prescriptions filled we fit a logistic regression (reported in the on-line supplemental material for this paper, Table B1). For the positive number of prescriptions filled and for each positive expenditure measure we fit a generalized linear model (GLM) (McCullagh and Nelder 1989). On the basis of a modified Park test (Park 1966) and other recommended diagnostics (Manning and Mullahy 2001; Deb, Manning, and Norton 2010), we chose a GLM with a log link and gamma distribution for the two expenditure measures and chose a GLM with a log link and negative binomial distribution for the total number of prescriptions filled (Tables B2–B4 in the on-line supplemental material). Finally, for copay level we fit an ordinary least squares model.
In our regression models we treat the MEPS 2006 data as part of the post Part D period, because Part D took effect from January 1, 2006. However, a more appropriate approach might be to simply exclude the 2006 data from the dataset, thereby defining the post period to be 2007–2009. Because many seniors were still signing up for Part D in the first quarter of 2006, one could argue they were “not exposed” to their Part D coverage for the full year. Would our results change if we instead drop the 2006 data? We address this issue at the end of our results section.
Results
Table 1 provides definitions and descriptive statistics for the variables. The average age of Medicare seniors (the treatment group) is 74.4 years, and the average age of adults without Medicare aged 55–63 years (the comparison group) is 58.7 years. Compared to adults in the comparison group, Medicare seniors are less healthy and have more functional limitations (e.g., their average physical component summary score is 40.6 versus 46.7 in the comparison group (p < .001), and their average functional limitations score is 8.9 versus 3.7 in the comparison group (p < .001)). Medicare seniors also have less formal education (e.g., 27 percent vs. 12 percent report less than a high school education) and have lower annual household income (37 percent vs. 18 percent have household income that is less than 199 percent of FPL). Tables A1 and A2 in the on-line supplemental material to this paper provide descriptive statistics stratified by race/ethnicity for the treatment and comparison groups, respectively.
Table 2 reports the unadjusted trends in the gap between African Americans and whites, and between Hispanics and whites in the years leading up to Part D. Our purpose in examining these trends is to assess whether racial/ethnic disparities in the treatment and comparison groups appear to have been on similar trajectories prior to the intervention of Part D. If not, then DDD methods are not valid (Bertrand, Duflo, and Mullainathan 2004). The first column in Table 2 lists each of the outcome variables. The second column reports the observed differences between African Americans and whites during 2002–2003, and the third column reports such differences during 2004–2005. The fourth column reports the changes in the gap over time, and the fifth column reports the net DDD results between the two time periods and between the comparison and treatment groups. The right side of Table 2 (columns 7 through 11) reports analogous statistics comparing whites and Hispanics.
The statistics in Table 2 reveal that prior to Part D, the differences in unadjusted disparity trends were not statistically significant. While prior to 2006 trends in disparities between African Americans/whites in any prescriptions filled, in total number of prescriptions, and in out-of-pocket cost, and between Hispanics/whites in out-of-pocket cost were diverging between the comparison and treatment groups, the net differences were not statistically significant. The lack of significant differences in these trends between the groups suggests we can proceed with a DDD approach for evaluating changes in disparities. We return to this point later in the discussion. We now proceed to the main analysis.
Table 3 reports for the treatment and comparison groups the IOM-adjusted estimates of the average values for the five outcome measures and the IOM disparity between whites and African Americans in those outcome measures, prior to and after Part D. Table 4 is a similar table that compares whites and Hispanics. The estimates in these two tables were derived from simulations using the multivariate regressions reported in Tables B1–B5 (reported on-line), after assigning African Americans and Hispanics the same distribution of need-related variables that whites display.
Table 3.
Institute of Medicine Estimates of Outcomes Related to Prescription Drugs for the Comparison and Treatment Groups during 2002–2005 and 2006–2009 between whites and African Americans
|
whites |
African Americans |
Disparities |
||||
|---|---|---|---|---|---|---|
| Outcome Measures | 02–05 | 06–09 | 02–05 | 06–09 | 02–05 | 06–09 |
| Any prescriptions filled | ||||||
| Treatment (65+) | 93% | 93% | 85%*** | 86%*** | 8% | 7% |
| Comparison (55–63) | 83% | 82% | 69%*** | 69%*** | 14% | 13% |
| Total number Rx filled | ||||||
| Treatment (65+) | 30.94 | 33.36 | 28.85* | 29.95*** | 2.09 | 3.41 |
| Comparison (55–63) | 21.60 | 22.01 | 18.64*** | 19.40*** | 2.96 | 2.61 |
| Rx total spending | ||||||
| Treatment (65+) | $2,161.73 | $2,399.75 | $1,850.40*** | $1,876.40*** | $311.33 | $523.35++ |
| Comparison (55–63) | $1,594.13 | $1,754.46 | $1,165.51*** | $1,371.43*** | $428.62 | $383.03 |
| Rx out-of-pocket | ||||||
| Treatment (65+) | $1,113.07 | $735.14 | $782.38*** | $455.30*** | $330.69 | $279.84++ |
| Comparison (55–63) | $582.13 | $509.34 | $412.29*** | $389.32*** | $169.84 | $120.02+++ |
| Average copay | ||||||
| Treatment (65+) | 59% | 38% | 53%*** | 32%*** | 6% | 6% |
| Comparison (55–63) | 45% | 41% | 49%*** | 45%*** | −4% | −4% |
Note. Estimates of number of prescriptions filled, total prescription cost, and out-of-pocket cost are based on samples with positive amounts of utilization and expenditure. Estimates for the comparison and treatment groups are based on the adjusted regression models reported in Tables B1–B5. Comparison group consists of adults without Medicare, aged 55–63, who self-report being white, African American, or Hispanic. Treatment group consists of Medicare beneficiaries aged 65 and older, who self-report being white, African American, or Hispanic.
*, *** Significantly different from the estimate for whites at the alpha = .10, .05, and .01 level, respectively.
++, +++ Significantly different from the 2002–2005 estimate at the alpha = .10, .05 and .01 level, respectively.
Source: Data are from the household component files of the 2002–2009 Medical Expenditure Panel Survey.
Table 4.
Institute of Medicine Estimates of Outcomes Related to Prescription Drugs for the Comparison and Treatment Groups during 2002–2005 and 2006–2009 between whites and Hispanics
|
whites |
Hispanics |
Disparities |
||||
|---|---|---|---|---|---|---|
| Outcome measures | 02–05 | 06–09 | 02–05 | 06–09 | 02–05 | 06–09 |
| Any prescriptions filled | ||||||
| Treatment (65+) | 93% | 93% | 88%*** | 88%*** | 5% | 5% |
| Comparison (55–63) | 83% | 82% | 70%*** | 69%*** | 13% | 13% |
| Total number Rx filled | ||||||
| Treatment (65+) | 30.94 | 33.36 | 26.39*** | 30.58*** | 4.55 | 2.78 |
| Comparison (55–63) | 21.60 | 22.01 | 17.44*** | 16.74*** | 4.16 | 5.27 |
| Rx total spending | ||||||
| Treatment (65+) | $2,161.73 | $2,399.75 | $1,697.39*** | $1,912.37*** | $464.34 | $487.38 |
| Comparison (55–63) | $1,594.13 | $1,754.46 | $1,185.12*** | $1,040.76*** | $409.01 | $713.70+++ |
| Rx out-of-pocket | ||||||
| Treatment (65+) | $1,113.07 | $735.14 | $775.34*** | $453.39*** | $337.73 | $281.75 |
| Comparison (55–63) | $582.13 | $509.34 | $496.43*** | $336.66*** | $85.70 | $172.68+++ |
| Average copay | ||||||
| Treatment (65+) | 59% | 38% | 52%*** | 30%*** | 7% | 8% |
| Comparison (55–63) | 45% | 41% | 55%*** | 51%*** | −10% | −10% |
Note. Estimates of number of prescriptions filled, total prescription cost, and out-of-pocket cost are based on samples with positive amounts of utilization and expenditure. Estimates for the comparison and treatment groups are based on the adjusted regression models reported in Tables B1–B5. Comparison group consists of adults without Medicare, aged 55–63, who self-report being white, African American, or Hispanic. Treatment group consists of Medicare beneficiaries aged 65 and older, who self-report being white, African American, or Hispanic.
Significantly different from the estimate for whites at the alpha = .10, .05, and .01 level, respectively.
Significantly different from the 2002–2005 estimate at the alpha = .10, .05 and .01 level, respectively.
Source: Data are from the household component files of the 2002–2009 Medical Expenditure Panel Survey.
Tables 3 and 4 reveal that, both before Part D and after it, there were significant racial/ethnic disparities in prescription drug utilization and spending among older adults. In both the treatment and comparison groups, older African Americans and Hispanics were significantly less likely than older whites to fill any prescriptions at all, and to fill fewer when they did fill any. Annual total and out-of-pocket expenditures on prescription drugs were also significantly lower among older African Americans and Hispanics than among older whites. In contrast to the comparison group, prior to and after Part D, older African Americans and Hispanics had lower average copays for their prescription drugs. Following Part D, regardless of race or ethnicity, the average copay in the treatment group fell by about a third, whereas in the comparison group it fell by only about 7–9 percent. To assess whether racial/ethnic disparities actually changed as a result of Part D, we now turn to Table 5, which summarizes our overall key findings.
Table 5.
Difference-in-Difference-in-Differences Estimates of Effects of Medicare Part D on Institute of Medicine (IOM) Disparities in Five Outcomes Related to Prescription Drugs between whites and African Americans, and between whites and Hispanics
|
whites vs. African Americans |
whites vs. Hispanics |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome Measures | Difference 2002–2005 | Difference 2006–2009 | Difference Over Time | DDD | t (p-Value) | Difference 2002–2005 | Difference 2006–2009 | Difference Over Time | DDD | t (p-Value) |
| Any prescriptions filled | ||||||||||
| Treatment (65+) | 8% | 7% | −1% | −0% | −0.39 (.699) | 5% | 5% | 0% | 0% | 0.37 (.710) |
| Comparison (55–63) | 14% | 13% | −1% | 13% | 13% | 0% | ||||
| Total number Rx filled | ||||||||||
| Treatment (65+) | 2.09 | 3.41 | 1.32 | 1.67 | 1.10 (.271) | 4.55 | 2.78 | −1.77 | −2.88* | −1.77 (.077) |
| Comparison (55–63) | 2.96 | 2.61 | −0.35 | 4.16 | 5.27 | 1.11 | ||||
| Rx total spending | ||||||||||
| Treatment (65+) | $311.33 | $523.35 | $212.02 | $257.61** | 2.53 (.011) | $464.34 | $487.38 | $23.04 | −$281.65** | −2.35 (.019) |
| Comparison (55–63) | $428.62 | $383.03 | −$45.59 | $409.01 | $713.70 | $304.69 | ||||
| Rx out-of-pocket spending | ||||||||||
| Treatment (65+) | $330.69 | $279.84 | −$50.85 | −$1.03 | −0.04 (.968) | $337.73 | $281.75 | −$55.98 | −$142.96*** | −3.86 (.000) |
| Comparison (55–63) | $169.84 | $120.02 | −$49.82 | $85.70 | $172.68 | $86.98 | ||||
| Average copay | ||||||||||
| Treatment (65+) | 6% | 6% | 0% | −0% | −1.04 | 7% | 8% | 1% | 1% | 0.62 |
| Comparison (55–63) | −4% | −4% | 0% | 0.296 | −10% | −10% | 0% | 0.536 | ||
Note. Estimates for the comparison and treatment groups are based on the adjusted regression models reported in Tables B1–B5 and the IOM disparity estimates from Tables 3 and 4. Comparison group consists of adults without Medicare, aged 55–63, who self-report being white, African American, or Hispanic. Treatment group consists of Medicare beneficiaries aged 65 and older, who self-report being white, African American, or Hispanic.
*, **, *** Significantly different from zero at the alpha = .10, .05, and .01 level, respectively.
Source: Data are from the household component files of the 2002–2009 Medical Expenditure Panel Survey.
Table 5 reports estimates of the effects of Part D on the IOM disparities between minorities and whites, based on the estimated disparities reported in the last two columns of Tables 3 and 4. The left side summarizes our findings regarding disparities between African Americans and whites, while the right side summarizes our findings regarding disparities between Hispanics and whites. As shown, among seniors the disparity in any prescriptions filled between African American and white seniors fell by 1 percent (p = .213) following implementation of Part D. However, in the comparison group the disparity in any prescriptions filled between African Americans and whites also fell by 1 percent (p = .817). Thus, in the DDD estimate of the “net effect” of Medicare Part D, which is the difference between these amounts, there was no reduction (p = .699) in the disparity. DDD estimates show that Part D also had no significant effects on the African American/white disparity in annual number of prescriptions filled, in annual out-of-pocket spending on prescription drugs, or in average copay level.
Part D had a significant effect on the African American/white disparity in annual total spending on prescription drugs. The DDD net effect of Part D was a $258 (p = .011) increase in the disparity in annual total spending. The increase occurred because the disparity in total spending rose $212 among Medicare seniors (p = .015) following Part D, but it also fell $46 among near-elders (p = .502). The DDD net effect of Part D is the difference between these amounts, which is $212-(-$46) or $258. Following Part D total spending on drugs rose among both white and African American seniors, but it rose more among whites than among African Americans, hence the increase by $212 in the disparity for this group.
Part D also had a few significant effects on disparities between Hispanic and white seniors. Although Part D had no DDD net effect on the disparity in any prescriptions filled or the disparity in average copay, the program did reduce Hispanic/white disparities in each of the other three utilization and spending measures. The DDD net effect of Part D on the Hispanic/white disparity in total number of prescriptions filled annually was a drop of 2.88 prescriptions (p = .077). The DDD net effect of the program on the Hispanic/white disparity in total annual spending on prescription drugs was a $282 (p = .019) drop, and the DDD net effect on the Hispanic/white disparity in annual out-of-pocket spending on drugs was a $143 (p < 0.001) drop.
When we reestimated all of these models without inclusion of the 2006 data, our findings barely changed. Specifically, our estimates of any prescriptions filled and the number of prescriptions filled were effectively the same (rounding to two decimals) for each subpopulation as they were before. Without 2006 data, our estimated disparities for total and out-of-pocket prescription drug spending in the treatment group were slightly different (by $61 and $4, respectively, for whites vs. Hispanics, and by $1 and $3, respectively, for whites vs. African Americans).
Discussion
Three main findings emerge from this analysis. First, based on a DDD econometric approach, Medicare Part D significantly increased the disparity between African American and white seniors in total annual spending on prescription drugs by $258.
Second, Part D significantly reduced Hispanic/white disparities in the annual number of prescriptions filled, in total annual spending on prescription drugs, and in annual out-of-pocket spending on prescription drugs. Due to Part D, these disparities fell by 2.88, $282, and $143, respectively, based on DDD measures of change.
Third, Part D had no effects on African American/white disparities in whether any prescriptions filled, in the number of prescriptions, on annual out-of-pocket spending on drugs, or on average copay. Nor did Medicare Part D have any effects on the Hispanic/white disparity in filling any prescriptions during a year or on average copay.
African Americans' disparity increase in annual total spending on prescription drugs is attributable to two things: a larger increase in annual total spending among white seniors than among African American seniors, and to a reduction in the total spending disparity among near-elders. While white seniors experienced large increases in both the number of prescriptions filled (by 8 percent) and total spending on drugs (by 11 percent) after Part D, both of these measures increased minimally (by 1 percent) among African American seniors. On the other hand, while there was no significant increase in number of prescriptions filled among African American near-elders, their total spending on prescription drugs rose substantially (by 18 percent).
Hispanic seniors, falling disparities are attributable to increases in their prescription drug utilization and spending vis-à-vis whites. We note here that those increases in utilization and spending among Hispanics were large enough to essentially lift them onto the same footing as African Americans. That is, adjusted average utilization and spending on prescription drugs are now quite similar for African American and Hispanic seniors, whereas prior to Part D they were significantly lower for Hispanics.
One explanation for why Hispanics saw large changes in utilization and spending may be their higher rate of enrollment in Medicare Advantage (MA) plans that have drug coverage, as opposed to stand-alone drug plans (Neuman, Strollo, and Cuterman 2007; Levy and Weir 2009). It is also worth noting that, as shown in Table 5, among adults aged 55–63 racial/ethnic disparities in several of these outcome variables actually worsened between the early and later part of the decade. We think these trends are explained by the great economic recession that began in December 2007, and the fact that disproportionately more Hispanics lost employer-sponsored health insurance over this period, which is the main source of drug insurance among non elderly adults (Mahmoudi and Jensen 2012).
Although Part D reduced Hispanic/white disparities in prescription drug utilization and spending, it is still the case that significant disparities remain both for Hispanic and African American seniors. Why? The persistence in these disparities may be due to a number of factors. First, there are still differences in sources of prescription drug coverage across subpopulations, and different sources provide different depths of insurance protection. Generally speaking, employer plans tend to offer the most generous drug benefits, followed by MA plans, and stand-alone drug plans (Neuman et al. 2007). After Part D, most seniors who had employer-sponsored plans kept their employer-sponsored drug insurance (Levy and Weir 2009). In our data relatively fewer African American and Hispanic seniors reported holding employer-sponsored coverage. Many said they had an MA plan or Medicaid. Thus, differences in the nature of drug insurance across populations may partially explain this persistence of disparities. However, other reasons have to do with the determinants of drug use and spending, more generally. African American and Hispanics more often lack any usual source of care, more frequently encounter transportation difficulties, and tend to have lower income, less education, and sometimes English language barriers, all of which depress their use of health care, including prescription drugs (Cooper, Hill, and Powe 2002; Chin et al. 2007; Mahmoudi and Jensen 2012, 2013).
One question that inevitably arises when considering racial/ethnic disparities is whether the higher utilization and spending on prescription drugs among whites represents “overuse” or whether the lower utilization and spending among African Americans and Hispanics represents “underuse.” Just because health care disparities exist does not imply underuse is occurring in minority populations. It could be that some overuse is occurring among whites. This study has not addressed this issue. Until the optimal utilization of prescription drugs is known, it will remain unanswered and an important issue for research.
This analysis is not without limitations. First, the most suitable comparison group would have been a group of Medicare beneficiaries aged 65 and older who were not eligible for Part D. Unfortunately, no such group exists, so like most prior studies (Basu, Yin, and Alexander 2010; Liu et al. 2011), we chose adults aged 55–63 without Medicare as our comparison group. Second, our DDD research design is unable to fully disentangle the effects of Part D from the effects of changes in Medicare's MA program that were also occurring post-2003 (McGuire, Newhouse, and Sinaiko 2011). Thus, the changes in disparities uncovered here are likely partly attributable to growth in MA enrollments among minority seniors, because many MA plans were adding drug coverage over this period. Recall, we uncovered some subtle differences in Table 2 between the treatment and comparison groups in the pre-2006 trends in disparities. Even though we determined those differences were statistically insignificant, they raise a question of whether our comparison and treatment groups would have indeed experienced similar trends in disparities absent Part D. One reason to suspect they might not have has to do with some other changes to Medicare that occurred under the 2003 Medicare Modernization and Improvement Act (MMA). In addition to creating Part D, the MMA also changed the MA program in important ways. Specifically, Medicare began subsidizing payments to MA plans in 2004, and with those additional payments many MA plans expanded their benefits, including prescription drug benefits. As a result, many more seniors enrolled in MA plans (McGuire et al. 2011). From 2002 to 2007, the period we study here, MA enrollments rose 50 percent, or from 5.6 to 8.4 million (Gold et al. 2012). MA enrollment was related to race and ethnicity, with minorities more likely to enroll (Shimada et al. 2009; Levy and Weir 2009). For this reason, racial/ethnic differences in utilization and spending on prescription drugs among Medicare seniors may have already started on a different trajectory post-2003, vis-à-vis racial/ethnic differences in the comparison group. In other words, the changes in Medicare's MA program that were also occurring may have influenced the trajectories in prescription drug disparities. What this means is that we cannot fully disentangle the effects of Part D from the effects of changes in Medicare's MA program that were simultaneously occurring. Third, there may be differences in preferences and attitudes across racial/ethnic groups that we are unable to measure, and these may have also contributed to racial/ethnic disparities in access and utilization (Ayanian et al. 1999). Fourth, because of their small sample sizes in MEPS, we were unable to distinguish between Cubans, Puerto Ricans, Mexicans, and other Hispanics within the overall Hispanic population. Finally, in this analysis, we examined all Medicare seniors. Thus, our results might differ for specific subgroups of Medicare beneficiaries, such as seniors with specific chronic conditions.
In summary, Medicare Part D increased the African American/white disparity in total annual spending on prescription drugs, with no effects on other African American/white measures of disparities in prescription drugs. For Hispanic/white disparities, however, Medicare Part D reduced disparities in the annual number of prescriptions filled, and in total and out-of-pocket annual spending on prescription drugs, with no effects on filling any prescriptions or on average copay.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: We acknowledge funding from the Center for Retirement Research at Boston College (grant no. BC11-D4) and from the Blue Cross and Blue Shield of Michigan Foundation (grant no. 1699.SAP). The opinions expressed here are not those of the University of Michigan or Wayne State University. We thank Allen Goodman, audience members at the 2012 American Society of Health Economists (ASHEcon) conference, and the anonymous reviewers for helpful comments on earlier versions of this paper. Any remaining errors are those of the authors.
Disclosures: None.
Disclaimers: None.
Notes
We also estimated disparities using two other alternative definitions of a racial/ethnic disparity: the unadjusted difference across groups in the average value of the outcome measure, and the “residual direct effect” estimate of a disparity (Cook, McGuire, and Miranda 2007). Due to space limitations these results are not presented or discussed in this article. However, these estimates that apply alternative definitions are available from the authors upon request.
We also tested the “variance inflation factors” to verify that each model was multicollinearity-free (Kmenta 1971).
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article
Author Matrix.
Table A1: Characteristics of Medicare Beneficiaries, Ages 65 and Over, by Race and Ethnicity in 2002–2005 and 2006–2009.
Table A2: Characteristics of Adults without Medicare, Ages 55–63, by Race and Ethnicity in 2002–2005 and 2006–2009.
Table B1: Logit Regression Results for Having Any Prescriptions Filled during the Past Year: 2002–2009.
Table B2: GLM Regression Results for the Positive Number of Prescriptions Filled during the Past Year: 2002–2009.
Table B3: GLM Regression Results for the Total Positive Expenditure of Prescription Drugs during the Past Year: 2002–2009.
Table B4: GLM Regression Results for Positive Out-of-Pocket Expenditure of Prescriptions Filled during the Past Year: 2002–2009.
Table B5: OLS Regression Results for the Prescription Drugs Co-pay during the Past Year: 2002–2009.
Reference
- Andersen R. A Behavioral Model of Families' Use of Health Services. Chicago, Iavioral Model and Access to Medical Care: Does It Maenter for Health Administration Studies; 1968. [Google Scholar]
- Andersen R. “Revisiting the Behavioral Model and Access to Medical Care: Does It Matter?”. Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. “The Effect of Patients' Preferences on Racial Differences in Access to Renal Transplantation”. New England Journal of Medicine. 1999;341(22):1661–9. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- Basu A, Yin W, Alexander GC. “Impact of Medicare Part D on Medicare-Medicaid Dual-Eligible Beneficiaries' Prescription Utilization and Expenditures”. Health Services Research. 2010;45(1):133–51. doi: 10.1111/j.1475-6773.2009.01065.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertrand M, Duflo E, Mullainathan S. “How Much Should We Trust Differences-in-Differences Estimates?”. The Quarterly Journal of Economics. 2004;119(1):249–75. [Google Scholar]
- Briesacher BA, Limcangco R, Gaskin D. “Racial and Ethnic Disparities in Prescription Coverage and Medication Use”. Health Care Financial Review. 2004;25(2):63–76. [PMC free article] [PubMed] [Google Scholar]
- Chin MH, Walters AE, Cook SC, Huang ES. “Interventions to Reduce Racial and Ethnic Disparities in Health Care”. Medical Care Research and Review. 2007;64(5 suppl):7S–28S. doi: 10.1177/1077558707305413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen JW, Monheit AC, Beauregard KM, Cohen SB, Lefkowitz DC, Potter D, Sommers JP, Taylor AK, Arnett R., 3rd “The Medical Expenditure Panel Survey: A National Health Information Resource”. Inquiry. 1997;33(4):373. [PubMed] [Google Scholar]
- Cook B, McGuire T, Miranda J. “Measuring Trends in Mental Health Care Disparities, 2000–2004”. Psychiatric Services. 2007;58(12):1533–40. doi: 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- Cook B, McGuire TG, Lock K, Zaslavsky AM. “Comparing Methods of Racial and Ethnic Disparities Measurement across Different Settings of Mental Health Care”. Health Services Research. 2010;45(3):825–47. doi: 10.1111/j.1475-6773.2010.01100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LA, Hill MN, Powe NR. “Designing and Evaluating Interventions to Eliminate Racial and Ethnic Disparities in Health Care”. Journal of General Internal Medicine. 2002;17(6):477–86. doi: 10.1046/j.1525-1497.2002.10633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deb P, Manning W, Norton E. 2010. “Preconference Course: Modeling Health Care Costs and Counts” [accessed on June 10, 2010]. Available at http://www.ispor.org/OpenSourceIndex/cached/Modeling_Health_Care_Costs_and_Use_Files/ASHE2010_Minicourse_Cost_Use_slides.pdf.
- Engelhardt GV, Grubera J. “Medicare Part D and the Financial Protection of the Elderly”. American Economic Journal: Economic Policy. 2011;3(4):77–102. [Google Scholar]
- Gaskin DJ, Briesacher BA, Limcangco R, Brigantti BL. “Exploring Racial and Ethnic Disparities in Prescription Drug Spending and Use among Medicare Beneficiaries”. American Journal of Geriatric Pharmacotherapy. 2006;4(2):96–111. doi: 10.1016/j.amjopharm.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Gellad WF, Haas JS, Safran DG. “Race/Ethnicity and Nonadherence to Prescription Medications among Seniors: Results of a National Study”. Journal of General Internal Medicine. 2007;22(11):1572–8. doi: 10.1007/s11606-007-0385-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson TB, Song X, Alemayehu B, Wang SS, Waddell JL, Bouchard JR, Forma F. “Cost Sharing, Adherence, and Health Outcomes in Patients with Diabetes”. American Journal of Managed Care. 2010;16(8):589–600. [PubMed] [Google Scholar]
- Gold MR. 2012. Medicare Advantage 2012 Data Spotlight: Enrollment Market Update: Henry J. Kaiser Family Foundation.
- Heisler M, K. M Langa, E. L Eby, A. M Fendrick, M. U Kabeto, Piette JD. “The Health Effects of Restricting Prescription Medication Use Because of Cost”. Medical Care. 2004;42(7):626–34. doi: 10.1097/01.mlr.0000129352.36733.cc. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine (IOM); 2002. [Google Scholar]
- Jensen GA, Li Y. “Long-Run Health Effects of Cost-Related Non-Adherence to Prescribed Medications Among Adults in Late Midlife”. Journal of Pharmaceutical Health Services Research. 2012;3(2):85–93. [Google Scholar]
- Kmenta J. Elements of econometrics. New York, NY: Macmillan; 1971. [Google Scholar]
- Kolenikov S. “Resampling Variance Estimation for Complex Survey Data”. Stata Journal. 2010;10(2):165–99. [Google Scholar]
- Levy H, Weir D. “Take-up of Medicare Part D: Results from the Health and Retirement Study”. Journal of Gerontology: Social Sciences. 2009;65B(4):492–501. doi: 10.1093/geronb/gbp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenberg FR, Sun SX. “The Impact of Medicare Part D on Prescription Drug Use by the Elderly”. Health Affairs. 2007;26(6):1735–44. doi: 10.1377/hlthaff.26.6.1735. [DOI] [PubMed] [Google Scholar]
- Little RJ, Rubin DB, D B Rubin, Hoboken NJ. Statistical Analysis with Missing Data. Wiley; 2002. [Google Scholar]
- Liu FX, Alexander GC, Crawford SY, Pickard AS, Hedeker D, Walton SM. “The Impact of Medicare Part D on Out-of-Pocket Costs for Prescription Drugs, Medication Utilization, Health Resource Utilization, and Preference-Based Health Utility”. Health Services Research. 2011;46(4):1104–23. doi: 10.1111/j.1475-6773.2011.01273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden JM, Graves AJ, Zhang F, Adams AS, Briesacher BA, Ross-Degnan D, Gurwitz JH, Pierre-Jacques M, Safran DG, Adler GS, Soumerai SB. “Cost-related Medication Nonadherence and Spending on Basic Needs Following Implementation of Medicare Part D”. Journal of the American Medical Association. 2008;299(16):1922–8. doi: 10.1001/jama.299.16.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmoudi E, Jensen GA. “Diverging Racial and Ethnic Disparities in Access to Physician Care: Comparing 2000 and 2007”. Medical Care. 2012;50(4):327. doi: 10.1097/MLR.0b013e318245a111. [DOI] [PubMed] [Google Scholar]
- Mahmoudi E, Jensen GA. “Exploring Disparities in Access to Physician Services among Older Adults: 2000–2007”. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2013;68(1):128–38. doi: 10.1093/geronb/gbs105. [DOI] [PubMed] [Google Scholar]
- Manning WG, Mullahy J. “Estimating Log Models: To Transform or Not to Transform?”. Journal of Health Economics. 2001;20(4):461–94. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- McCullagh P, Nelder JA. Generalized Linear Models. Boca Raton, FL: Chapman & Hall/CRC; 1989. [Google Scholar]
- McGuire TG, M Alegria, B Cook, K. B Wells, A. M Zaslavsky. “Implementing the Institute of Medicine Definition of Disparities: An Application to Mental Health Care”. Health Services Research. 2006;41(5):1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire TG, J. P Newhouse, A. D Sinaiko. “An Economic History of Medicare Part C”. Milbank Quarterly. 2011;89(2):289–332. doi: 10.1111/j.1468-0009.2011.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuman P, Strollo MK, Guterman S, Rogers WH, Li A, Rodday AM, Safran DG. “Medicare Prescription Drug Benefit Progress Report: Findings from a 2006 National Survey of Seniors”. Health Affairs (Millwood) 2007;26(5):w630–43. doi: 10.1377/hlthaff.26.5.w630. [DOI] [PubMed] [Google Scholar]
- Park RE. “Estimation with Heteroscedastic Error Terms”. Econometrica. 1966;34(4):888. [Google Scholar]
- Reed MC, Hargraves JL, Cassil A. “Unequal Access: African-American Medicare Beneficiaries and the Prescription Drug Gap”. Issue Brief (Center for Studying Health System Change) 2003;(64):1. [PubMed] [Google Scholar]
- Safran DG, Neuman P, Schoen C, Kitchman MS, Wilson IB, Cooper B, Li A, Chang H, Rogers WH. “Prescription Drug Coverage and Seniors: Findings from a 2003 National Survey”. Health Aff (Millwood) 2005;24:W5. doi: 10.1377/hlthaff.w5.152. [DOI] [PubMed] [Google Scholar]
- Safran DG, Strollo MK, Guterman S, Li A, Rogers WH, Neuman P. “Prescription Coverage, Use and Spending before and after Part D Implementation: A National Longitudinal Panel Study”. Journal of General Internal Medicine. 2010;25(1):10–7. doi: 10.1007/s11606-009-1134-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimada SL, Zaslavsky AM, Zaborski LB, O'Malley AJ, Heller A, Cleary PD. “Market and Beneficiary Characteristics Associated with Enrollment in Medicare Managed Care Plans and Fee-for-Service”. Medical Care. 2009;47(5):517–23. doi: 10.1097/MLR.0b013e318195f86e. [DOI] [PubMed] [Google Scholar]
- Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. “Impact of Medication Adherence on Hospitalization Risk and Healthcare Cost”. Medical Care. 2005;43(6):521. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- Soumerai SB, Pierre-Jacques M, Zhang F, Ross-Degnan D, Adams AS, Gurwitz J, Adler G, Safran DG. “Cost-Related Medication Nonadherence Among Elderly and Disabled Medicare Beneficiaries: A National Survey 1 Year Before the Medicare Drug Benefit”. Archives of Internal Medicine. 2006;166(17):1829. doi: 10.1001/archinte.166.17.1829. [DOI] [PubMed] [Google Scholar]
- Ware J, Kosinski M, Turner-Bowker D, Gandek B. Health Assessment Lab: Boston, MA; Lincoln, RI; 2002. “SF-12v2: How to Score Version 2 of the SF-12 Health Survey.” Quality Metric Incorporated. [Google Scholar]
- Wilson J, Axelsen K, Tang S. “Medicaid Prescription Drug Access Restrictions: Exploring the Effect on Patient Persistence with Hypertension Medications”. American Journal of Managed Care. 2005;11(Spec No):SP27–34. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Matrix.
Table A1: Characteristics of Medicare Beneficiaries, Ages 65 and Over, by Race and Ethnicity in 2002–2005 and 2006–2009.
Table A2: Characteristics of Adults without Medicare, Ages 55–63, by Race and Ethnicity in 2002–2005 and 2006–2009.
Table B1: Logit Regression Results for Having Any Prescriptions Filled during the Past Year: 2002–2009.
Table B2: GLM Regression Results for the Positive Number of Prescriptions Filled during the Past Year: 2002–2009.
Table B3: GLM Regression Results for the Total Positive Expenditure of Prescription Drugs during the Past Year: 2002–2009.
Table B4: GLM Regression Results for Positive Out-of-Pocket Expenditure of Prescriptions Filled during the Past Year: 2002–2009.
Table B5: OLS Regression Results for the Prescription Drugs Co-pay during the Past Year: 2002–2009.


