Hypothyroidism is present in 1.4% to 13% of patients with hyperlipidemia.1 Overt hypothyroidism is a secondary cause of hyperlipidemia and associated coronary heart disease.2 Cholesterol profiles may be improved by treating overt hypothyroidism.
Current guidelines from the National Cholesterol Education Program, the American Association of Clinical Endocrinologists, and the American Thyroid Association recommend screening for hypothyroidism in patients with newly diagnosed hyperlipidemia prior to starting a lipid-lowering agent.3–6 It is unclear how well these guidelines are being followed in clinical practice. We performed a retrospective cohort study to determine the prevalence of thyroid function screening in patients with newly diagnosed hyperlipidemia at an inner-city academic medical center (Boston Medical Center [BMC]).
Methods
Boston University Medical Campus’s institutional review board approved the protocol and approved a waiver of informed consent. We conducted a retrospective medical chart review of patients at least 18 years old with a total serum cholesterol level of at least 200 mg/dL or low-density lipoprotein cholesterol (LDL-C) level of at least 160 mg/dL managed at BMC’s general internal medicine or family medicine clinics from 2003 to 2011. Patients who had previously been prescribed lipid-lowering agents or thyroid medications were excluded. (To convert cholesterol and LDL-C to millimoles per liter, multiply by 0.0259.)
Demographic data and the proportion of patients with serum thyroid function testing obtained within about 6 months of the initial cholesterol elevation were determined. We ascertained the proportion of patients with abnormal serum thyroid-stimulating hormone (TSH) concentrations among those tested and determined whether patients were subsequently treated with levothyroxine within 6 months or with a lipid-lowering agent within 1 year.
Results
There were 8795 patients (mean [SD] age, 53 [12] years; 55% were women; 45%, African American; 24%, white; 16%, Hispanic) with new hyperlipidemia within the study period (Table).Thyroid function testing rates were higher among white patients (58%) than in other races/ethnicities (45%–59%; P < .01), and among women (60%) than men (37%; P < .01).
Table.
Demographics of 8795 Patientsa
| Characteristic | No. (%)b | |
|---|---|---|
| Total | Screened | |
| Sex | ||
| Women | 4840 (55) | 2881 (60) |
| Men | 3955 (45) | 1468 (37) |
| Race/ethnicity | ||
| White | 2082 (24) | 1204 (58) |
| African American | 3927 (45) | 1837 (47) |
| Hispanic | 1409 (16) | 656 (47) |
| Asian | 286 (3) | 129 (45) |
| Native American | 17 (0.19) | 10 (59) |
| Other | 938 (11) | 442 (47) |
| Unknown | 136 (2) | 71 (52) |
| Boston Medical Center clinic | ||
| General internal medicine | 7118 (81) | 3569 (50) |
| Family medicine | 1677 (19) | 780 (47) |
Abbreviations: LDL, low-density lipoprotein; TSH, thyroid stimulating hormone.
Mean (SD) age, 53 (12) years [range, 18–95 years]. Mean (SD) cholesterol and low-density lipoprotein cholesterol (LDL-C) levels, 242 (46) mg/dL, and 185 (29) mg/dL, respectively; mean thyroid-stimulating hormone (TSH) level, 1.52 mIU/L [range, 0.01–370.92]. To convert cholesterol and LDL-C to millimoles per liter, multiply by 0.0259.
P= .01 for percentage screened for all comparisons.
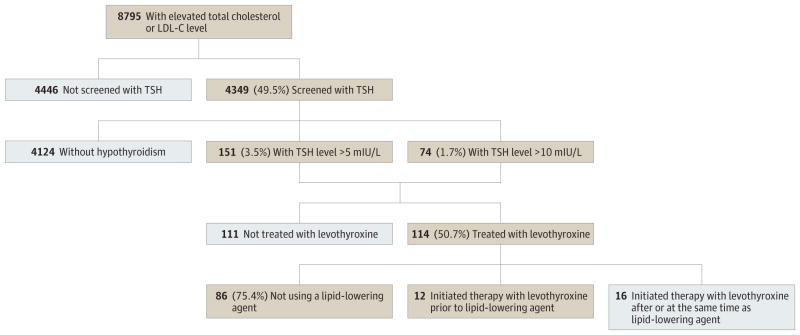
Serum TSH level was checked within about 6 months of the hyperlipidemia diagnosis in 49.5%, of whom 226 (5.2%) had an elevated level: 151 (3.5%) had a TSH level of 5 to 10 mIU/L; 74 (1.7%) had a TSH level greater than 10 mIU/L. Of those with an elevated TSH level, 114 (50.7%) were treated with levothyroxine, including 52 of 74 patients (70.3%) with a TSH level greater than 10 mIU/L. Eight hundred patients (18.3%) also had peripheral thyroid function tests checked (21 [2.6%] had overt hypothyroidism; 89 [11.1%], subclinical hypothyroidism). Among patients treated with levothyroxine, only 25% (vs 44% of patients with hyperlipidemia not treated with levothyroxine) were also prescribed a lipid-lowering agent within 1 year (Figure).
Figure. Flowchart of Patients Evaluated.
LDL-C indicates low-density lipoprotein cholesterol; TSH, thyroid-stimulating hormone.
Discussion
Only about 50% of patients with newly diagnosed hyperlipidemia were screened for thyroid dysfunction, despite current guidelines. Testing resulted in a diagnosis of hypothyroidism in 5.2%, consistent with findings in previous studies.1 Patients with TSH levels greater than 10 mIU/L, for whom levothyroxine treatment is recommended, comprised only 1.7% of screened patients.6
Approximately 50% of those with elevated TSH levels were treated with levothyroxine; 30% of patients with TSH levels greater than 10 mIU/L were not treated. Among patients who received levothyroxine, a considerable proportion (75%)did not require a lipid-lowering agent within 1 year. Although 79% of these patients had correction of their hypothyroidism, 60.5% did not have lipid levels rechecked. Among those whose lipid levels were rechecked, 21 (61.8%) no longer had hyperlipidemia.
Strengths of this study include the large sample and diverse inner-city population. However, this was a retrospective study, and we could not evaluate whether patients received screening and/or levothyroxine and antilipemic treatment at other medical institutions during the time frame studied.
We conclude that the low rate of thyroid function testing in patients with new-onset hyperlipidemia demonstrates the need for more awareness of current guidelines. Future studies are needed to better understand reasons for low thyroid function screening rates among patients with hyperlipidemia and cost-effectiveness of hypothyroidism screening and treatment among these patients. Thyroid function screening guidelines for patients with hyperlipidemia may need revision if future studies demonstrate lack of cost-effectiveness; our results show that current guidelines may be underused.
Acknowledgments
Funding/Support: This work was supported by National Institutes of Health (NIH) grant 7K23HD068552 to Dr Leung.
Footnotes
Author Contributions: Dr Willard had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Role of the Sponsor: The NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Previous Presentation: This work was previously presented as a poster abstract at the American Association of Clinical Endocrinologists Annual Meeting; May 3, 2013; Phoenix, Arizona.
Study concept and design: All authors.
Acquisition of data: Willard.
Analysis and interpretation of data: All authors.
Drafting of the manuscript: Willard.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Willard, Leung.
Administrative, technical, or material support: Leung.
Study supervision: Leung, Pearce.
Contributor Information
Devina L. Willard, Department of Medicine, Boston Medical Center, Boston, Massachusetts.
Angela M. Leung, Division of Endocrinology, Department of Medicine, University of California, Los Angeles, Los Angeles.
Elizabeth N. Pearce, Section of Endocrinology, Diabetes, and Nutrition; Department of Medicine, Boston University School of Medicine, Boston, Massachusetts.
References
- 1.Tagami T, Kimura H, Ohtani S, et al. PHPH Study Group. Multi-center study on the prevalence of hypothyroidism in patients with hypercholesterolemia. Endocr J. 2011;58(6):449–457. doi: 10.1507/endocrj.k11e-012. [DOI] [PubMed] [Google Scholar]
- 2.Razvi S, Shakoor A, Vanderpump M, Weaver JU, Pearce SHS. The influence of age on the relationship between subclinical hypothyroidism and ischemic heart disease: a meta-analysis. J Clin Endocrinol Metab. 2008;93(8):2998–3007. doi: 10.1210/jc.2008-0167. [DOI] [PubMed] [Google Scholar]
- 3.Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Washington, DC: US Department of Health and Human Services; 2001. [Google Scholar]
- 4.Jellinger PS, Smith DA, Mehta AE, et al. AACE Task Force for Management of Dyslipidemia and Prevention of Atherosclerosis. American Association of Clinical Endocrinologists’ guidelines for management of dyslipidemia and prevention of atherosclerosis. Endocr Pract. 2012;18(suppl 1):1–78. doi: 10.4158/ep.18.s1.1. [DOI] [PubMed] [Google Scholar]
- 5.Ladenson PW, Singer PA, Ain KB, et al. American Thyroid Association guidelines for detection of thyroid dysfunction. Arch Intern Med. 2000;160(11):1573–1575. doi: 10.1001/archinte.160.11.1573. [DOI] [PubMed] [Google Scholar]
- 6.Garber JR, Cobin RH, Gharib H, et al. American Association of Clinical Endocrinologists and American Thyroid Association Taskforce on Hypothyroidism in Adults. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract. 2012;18(6):988–1028. doi: 10.4158/EP12280.GL. [DOI] [PubMed] [Google Scholar]