Abstract
Rationale and Objectives:
Carpal tunnel syndrome (CTS) is the most common peripheral nerve entrapment syndrome. Strong pinch or grip with wrist flexion has been considered a risk factor for CTS. Studying median nerve displacement during wrist movements may provide useful information about median nerve kinematic changes in CTS patients. The purpose of this study was to evaluate the deformability and mobility of the median nerve in CTS patients compared to healthy subjects.
Materials and Methods:
Dynamic ultrasound images were obtained in 20 affected wrists of 13 patients with CTS. Results were compared to complementary data obtained from both wrists of 10 healthy subjects reported in a previous study. Initial and final median nerve shape and position were measured and analyzed for six defined wrist movements. The deformation ratios for each movement were defined as the median nerve area, perimeter and circularity of the final position normalized by respective values assessed in the initial position. The median nerve displacement vector and magnitude were also calculated.
Results:
The deformation ratio for circularity was significant less in CTS patients compared to healthy subjects during wrist flexion (P<0.05). The mean vector of median nerve displacement during wrist flexion was significantly different between CTS patients and healthy subjects (P<0.05). The displacement magnitude of the median nerve was found to be less in CTS patients compared to healthy subjects during most movements, with the exception of wrist extension with fingers extended.
Conclusions:
CTS Patients differ from normal subjects with regard to mobility and deformability of the median nerve.
Keywords: Ultrasound, Median Nerve, Carpal Tunnel Syndrome
INTRODUCTION
Carpal tunnel syndrome (CTS) is the most common peripheral nerve entrapment syndrome, and its precise etiology remains largely unclear. Like other peripheral nerves, the median nerve is exposed to various mechanical stresses related to limb postures and movements. In the case of the median nerve in the carpal tunnel, the relevant movements are of the fingers and wrist. The median nerve response to these stresses is a combination of displacement and deformation (1). Both displacement and deformation are known to vary from normal in CTS patients, due to increased carpal tunnel pressure and to fibrosis in the median nerve and the surrounding tissue in the carpal tunnel (2, 3).
Actuated by finger or wrist motion, the median nerve can displace in three dimensions. Longitudinal sliding of the median nerve in the carpal tunnel has been observed both in vitro and in vivo (4-9). Reduced longitudinal excursion of the median nerve at the carpal tunnel has been identified in CTS patients.(5, 10) Transverse motion of the median nerve has also been studied in the carpal tunnel in normal subjects (11, 12) and CTS patients (1, 13). Nakamichi et al. found reduced transverse motion of the median nerve during passive flexion and extension of the index finger in CTS patients (1). Erel et al. studied the transverse motion of the median nerve during passive extension of the digits at the metacarpophalangeal joint from 90° flexion to neutral. Their results showed that in CTS patients there was a significant reduction in transverse movement on the more symptomatic side compared to the contralateral (13).
Compared to finger movement, wrist movements may have more influence on the pathomechanism of CTS. Activities performed with the wrist flexed or extended have been considered to be risk factors for CTS (14). Wrist position affects not only the interstitial fluid pressure in the carpal tunnel (3, 15, 16), but also the direct contact pressure on the median nerve from the adjacent tissues, including the flexor tendons, subsynovial connective tissue (SSCT) within the carpal tunnel, and the wrist flexor retinaculum (15, 17, 18). The shear strain index between the tendon and median nerve is higher at 60 degrees of wrist flexion compared to 30 degrees of flexion, full wrist extension or neutral wrist positions (19). The gliding resistance of flexor tendons against the flexor retinaculum is also significantly increased at 60 degrees of wrist flexion compare to the neutral position (20).
Despite the importance of wrist position in the pathomechanism of CTS, there are few studies that have addressed the transverse deformation and mobility of the median nerve associated with wrist movement (21-24). For normal subjects, quantitative data of the median nerve displacement and deformation were obtained either by MR imaging or high frequency ultrasound (22, 23). Consistent findings which showed the median nerve adopting a rounder shape with the wrist flexion compared to the wrist neutral position were reported in these studies. For CTS patients, Allmann et al. investigated the median nerve during wrist flexion and extension in CTS patients. However, only qualitative displacement results were reported, and deformation of the median nerve was not described (21). To our knowledge, no studies have compared quantitatively the median nerve motion and deformation during wrist motion between CTS patients and healthy controls.
In this study, we investigated both the deformation and mobility of the median nerve in the cross-sectional plane during six different hand and wrist motions in CTS patients and compared these results to those previously reported for normal subjects (23). Our hypothesis was that the deformability and mobility of the median nerve in response to maximal wrist flexion, extension or ulnar deviation may be reduced in patients with CTS. We believe that such information could be valuable to the study of kinematics of the median nerve in patients with CTS.
MATERIALS AND METHODS
Thirteen patients with clinically diagnosed CTS were recruited (6 men, 7 women, mean age 50.9 with a range of 41-60 years) according the diagnostic criteria of the Quality Standards Subcommittee of the American Academy of Neurology (25). Among them, 7 patients had bilateral CTS and the remaining 6 patients had unilateral CTS, thus a total of 20 wrists with CTS were included in this study. Patients were excluded if they had the following conditions: rheumatoid arthritis; osteoarthritis; degenerative joint disease in the hand or wrist; flexor tendinitis in the hand or wrist; space occupying lesions of the wrist; coexistent neurologic diseases, such as polyneuropathy, proximal median neuropathy, cervical radiculopathy, diabetes mellitus; history of fractures or other trauma to the hand or wrist; other systematic diseases. Similar methods were applied in a previous study of normal subjects, which reported on 10 healthy volunteers (4 men, 6 women, mean age: 39.1 with a range of 25-56 years) with no clinical signs or symptoms of CTS (23). Both wrists were evaluated in each volunteer. Thus a total of 20 wrists were examined in the previous study, which will serve as a control group for the current study.
Ultrasound Examination
Each subject was imaged while sitting with the shoulder in the neutral position and the forearm supinated. The forearm of the subject was placed on a custom-made table with the wrist in the neutral position. An ultrasound scanner (Acuson Sequoia C512, Siemens Medical Solutions, Malvern, PA, USA) was used, equipped with a linear array transducer (15L8; frequency: 8-14MHz). The depth of the ultrasound image was adjusted to 25-30 mm, depending on the tissue thickness of the examined hand. Ultrasound examinations were performed by a radiologist with more than 5 years of experience in musculoskeletal ultrasound. The image acquisition frame rate was set to 70 Hz with minimal image compression.
The transducer was placed at the proximal carpal tunnel. The proximal carpal tunnel was defined as the area between the pisiform and the scaphoid tubercle; these two landmarks are palpable on the palm of the hand and could be easily identified on ultrasound with the characteristics of hyperechoic surface and strong posterior acoustic shadowing. The transducer was maintained perpendicular to the median nerve in order to get clear images and to avoid anisotropic artifact. To stabilize the transducer during finger or wrist motion and to minimize compression of the tissue within the carpal tunnel, a custom-made transducer-fixing device was fastened at the subjects’ palm (23). To measure the wrist angle during wrist movement, a 2-axis tilt sensor (CXT102, Crossbow Technology, Inc., Milpitas, CA, USA) functioning as a goniometer was fixed to the back of the hand. Both dorsal-palmar and radial-ulnar rotational motion was collected during the wrist movements. The tilt sensor only registers angulation relative to the gravity vector. To allow it measure wrist angle for both motion planes, difference orientations of the wrist and sensor relative to the wrist were required. It was mounted with its base parallel to the dorsal plane of the hand for the wrist dorsal-palmar movement (the first position of the wrist was at the horizontal plane). For the wrist radial-ulnar movement, the forearm was rotated such that wrist radial-ulnar movement followed the vertical plane, and the tilt sensor was repositioned to allow its base to again be parallel with the horizontal plane. Tilt sensor data measuring wrist angles were collected concurrently with ultrasound data at a sample rate of 36 Hz.
Dynamic ultrasound images were obtained during the following finger and wrist movements:
Finger flexion, defined as the wrist held in the neutral position while all four fingers and the thumb moved from full finger extension to maximal flexion, forming a fist;
Wrist flexion with fingers extended, defined as wrist motion from the neutral position to maximal flexion while all fingers and the thumb were held in full extension;
Wrist flexion with fingers flexed, defined as wrist motion from the neutral position to maximal flexion while all fingers and the thumb were held in full flexion to form a fist;
Wrist extension with fingers extended, defined as wrist motion from the neutral position to maximal extension while all fingers and the thumb were held in full extension;
Wrist extension with fingers flexed, defined as wrist motion from the neutral position to maximal extension while all fingers and the thumb were held in full flexion to form a fist;
Wrist ulnar deviation with fingers extended, defined as wrist motion from the neutral position to maximal ulnar deviation while the fingers and the thumb were held in full extension.
Before data collection, the subjects would practice the motion 2-3 times with the examiner. All movements were repeated again 3 times for the experiment. The clip in which the median nerve was observed most clearly was chosen for final analysis.
Image Analysis
Images were evaluated using Analyze 11.0 software (Mayo Clinic, Rochester, MN, USA). After the initial and final frames of the motion were selected, the median nerve was outlined manually using a continuous boundary trace just within the echogenic boundary of the nerve (26). The following parameters of the median nerve were calculated automatically: area, perimeter, circularity, and the centroid coordinates. Circularity was defined as:
| Equation 1 |
If the circularity was 1, the outlined polygon resembled a perfect circle; a value less than 1 indicated a deviation from a circle (e.g., oval or irregular shaped polygon). The centroid was defined as the center of area of the outlined median nerve and was expressed in Cartesian coordinates x (radial-ulnar axis) and y (palmar-dorsal axis).
To assess the deformability of the median nerve, we calculated deformation ratios for area, perimeter and circularity. The deformation ratio was defined as the value in the final position normalized by the respective value in the initial position. Deformation ratios closer to 1 imply that the measurements of the parameter calculated in the initial and final positions were very similar. The more the deformation ratio deviates from 1 the greater the difference between the measurement of the parameter in the first and final positions.
To assess the mobility of the median nerve, we calculated the displacements in radial-ulnar (x) and palmar-dorsal directions (y) by comparing the initial and final centroid positions. The median nerve displacement vector was defined as the final position of median nerve relative to its initial position in each wrist movement. The magnitude of the median nerve displacement was defined as:
| Equation 2 |
The sign convention for motion analysis was such that the palmar and ulnar directions were defined as positive and the radial and dorsal directions were defined as negative values.
Normalization of Measurements
Displacement vector and displacement magnitude of the median nerve were normalized to hand length. Hand length was defined as the distance from the tip of the middle finger to the midline of the distal wrist crease when the forearm and hand were supinated on a table and was measured with a ruler on which the minimal scale was millimeter (27). Normalized results were presented as Normalized Units (NU) in which 1 NU = 1% of the normalized length. Thus for example, if the hand length was 100 mm and the displacement magnitude of the median nerve was 3 mm, the measurement would be expressed as 3 NU (i.e., 3% of the normalized length). The mean hand length of all wrists of CTS patients in this study was 184.55 ± 9.85 mm. Thus, one NU was roughly 1.85± 0.10 mm.
Statistical Analysis
JMP 9.0 (SAS Institute, Cary, North Carolina, USA) and Matlab (MathWorks Inc., Natick, MA, USA) were used for statistical analysis. Mardia’s bivariate test for normality was performed on median nerve displacement data. All results are expressed as a mean ± standard deviation (SD). The unpaired t- test was used to analyze the differences in the means of maximal wrist angles, deformation ratios, and normalized displacement magnitude of the median nerve between patient data collected in this study and normal data previously reported (23). The difference of the median nerve displacement vector between patients data of this study and normal data previously reported (23) was analyzed using the bivariate Mardia’s two-sample test and the Mardia-Watson-Wheeler non-parametric test (28). The mean vector (in polar coordinates) was used to represent the sample center. The standard ellipse, representative of sample variation, and Hotelling’s confidence ellipse parameters (α = 0.05) were calculated for each motion to describe sample variation. P-values of less than 0.05 were considered statistically significant. This study protocol was reviewed and approved by the Institutional Review Board of our institution.
RESULTS
Maximal Wrist Angles during Wrist Movements
The mean ± SD maximal wrist angles during wrist extension with fingers extended or flexed in CTS patients (35.75±7.28 degrees and 37.80±10.55 degrees, respectively) were significantly lower than those in healthy subjects (45.66±12.25 degrees and 48.04±10.27 degrees, respectively) (both P=0.004) (Figure 1). There were no differences in wrist angle between CTS patients and healthy subjects for the other movements (P>0.05).
Figure 1.
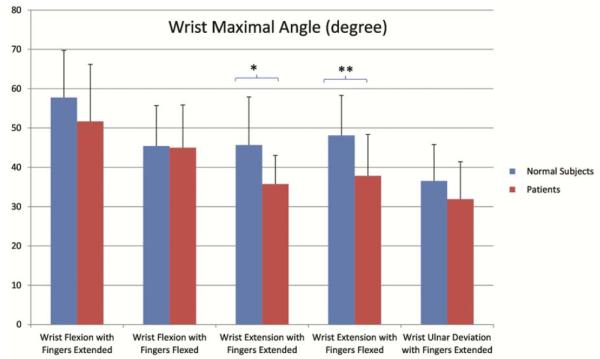
The comparison of the wrist angles between CTS patients and healthy subjects. The maximal wrist angle during wrist extension with fingers extended or flexed in CTS patients was significantly lower than those in healthy subjects.
Deformation Ratio of the Median Nerve
The deformation ratios of area, perimeter and circularity of the median nerve during finger and wrist movements are shown in Table 1. For wrist flexion with fingers flexed, the deformation ratio of median nerve perimeter was significantly higher in CTS patients than that in healthy subjects (P=0.024) (ratio for both groups was less than 1). For wrist flexion with fingers extended or flexed and wrist ulnar deviation with fingers extended, the deformation ratio of circularity in CTS patients was significantly less than that in healthy subjects (P=0.009, P=0.004 and P<0.001, respectively) (Figure 2) (ratio for both groups was bigger than 1). For finger flexion and wrist extension with fingers extended or flexed, no difference in any deformation ratio of the median nerve was found between the CTS patients and healthy subjects.
Table 1.
Median nerve deformation parameters.
| Wrist Motions | Area Deformation Ratio |
Perimeter Deformation Ratio |
Circularity Deformation Ratio |
|---|---|---|---|
| Finger Flexion | |||
| Patients | 1.00±0.16 | 0.98±0.08 | 1.05±0.13 |
| Healthy Subjects | 0.99±0.12 | 0.98±0.09 | 1.09±0.15 |
|
Wrist Flexion with Fingers
Extended |
|||
| Patients | 0.93±0.20 | 0.87±0.16 | 1.23±0.16** |
| Healthy Subjects | 1.06±0.24 | 0.86±0.16 | 1.49±0.38 |
|
Wrist Flexion with Fingers
Flexed |
|||
| Patients | 0.98±0.21 | 0.89±0.13* | 1.25±0.28** |
| Healthy Subjects | 0.94±0.22 | 0.79±0.15 | 1.57±0.36 |
|
Wrist Extension with
Fingers Extended |
|||
| Patients | 1.01±0.20 | 1.02±0.14 | 0.99±0.20 |
| Healthy Subjects | 1.03±0.15 | 0.97±0.11 | 1.12±0.19 |
|
Wrist extension with
Fingers Flexed |
|||
| Patients | 0.97±0.20 | 1.0±0.12 | 0.99±0.20 |
| Healthy Subjects | 0.98±0.15 | 0.98±0.12 | 1.05±0.22 |
|
Wrist Ulnar Deviation with
Fingers Extended |
|||
| Patients | 0.97±0.20 | 0.90±0.12 | 1.19±0.16** |
| Healthy Subjects | 1.02±0.27 | 0.93±0.20 | 1.53±0.32 |
P<0.05;
P<0.01
Figure 2.
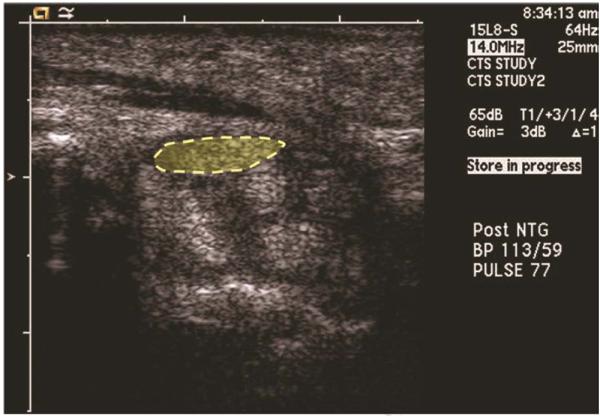
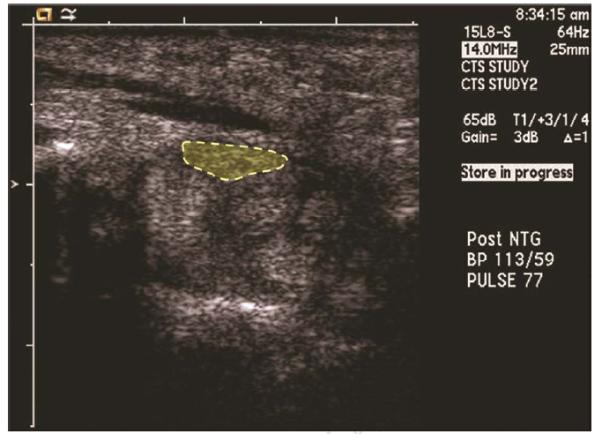
The median nerve at the carpal tunnel in a patient with CTS. A. At the start of wrist maximal flexion with fingers extended, the enlarged median nerve (dashed ellipse) was located between the flexor retinaculum and flexor tendons on transverse ultrasound. B. At the end of the movement the median nerve (dashed ellipse) was still located between the flexor retinaculum and flexor tendons and had moved only slightly towards the ulnar side of the carpal tunnel.
Displacement Vector of the Median Nerve
Mean vectors for all movements are included in Table 2. Included are vector magnitude (ρ) and vector direction (θ), major and minor confidence ellipse axes (a and b) and inclination of the ellipse (ψ). Solid ellipses represent standard deviation, dashed ellipses represent 95% confidence limits and the radial line represents the mean vector for each group.
Table 2.
Median nerve displacement mean vector and confidence limits in patients with CTS and healthy subjects.
| Mean ρ (NU) | Mean θ | a(NU) | b(NU) | ψ | |
|---|---|---|---|---|---|
| Finger Flexion | |||||
| Patients | 0.1 | 28.9 ° | 0.5 | 0.2 | 9.1 ° |
| Healthy Subjects | 0.2 | 117.3 ° | 0.5 | 0.2 | −16.0 ° |
| Wrist Flexion with Fingers Extended | |||||
| Patients | 0.8 | 137.3 ° ** | 1.0 | 0.3 | −6.2 ° |
| Healthy Subjects | 1.5 | 267.1 ° | 1.2 | 0.5 | −11.9 ° |
| Wrist Flexion with Fingers Flexed | |||||
| Patients | 1.0 | 331.4 ° ** | 1.0 | 0.4 | 4.5 ° |
| Healthy Subjects | 1.8 | 295.0 ° | 1.1 | 0.5 | −11.7 ° |
| Wrist Extension with Fingers Extended | |||||
| Patients | 0.2 | 144.4 ° * | 0.7 | 0.2 | −12 ° |
| Healthy Subjects | 0.4 | 225.6 ° | 0.5 | 0.2 | −7.8 ° |
| Wrist Extension with Fingers Flexed | |||||
| Patients | 0.6 | 184.4 ° | 0.5 | 0.2 | −0.7 ° |
| Healthy Subjects | 0.5 | 182.0 ° | 0.5 | 0.2 | −2.5 ° |
| Wrist Ulnar Deviation with Fingers Extended | |||||
| Patients | 1.8 | 190 9 ° ** | 0.8 | 0.3 | 14.6 ° |
| Healthy Subjects | 2.8 | 188.5 ° | 0.3 | 0.2 | −5.2 ° |
P<0.05;
P<0.01
ρ = vector length; θ = vector angle; a = major ellipse axes for variation of the confidence limits; b = minor ellipse axes for variation of the confidence limits; ψ = inclination of the ellipse
Note: 1 normalized unit (NU) is approximately 1.8 mm
The mean vectors for all movements in CTS patients and healthy subjects are displayed in Table 2. This table includes data published previously, with regard to the normal subjects (23), and compares that data with those in the patients studied here. With the exception of wrist flexion with fingers extended, all motions were found to have a normal distribution. A significant difference in the mean median nerve displacement vector was found between CTS patients and healthy subjects for wrist flexion with fingers extended or flexed (P<0.01), wrist extension with fingers extended (P<0.05) and wrist ulnar deviation with fingers extended (P<0.01) (Figures 3A-3D). No significant difference was found between healthy subjects and patients for movements of finger flexion (P=0.217) or wrist extension with fingers flexed (P=0.106) (Figures 3E, 3F).
Figure 3.
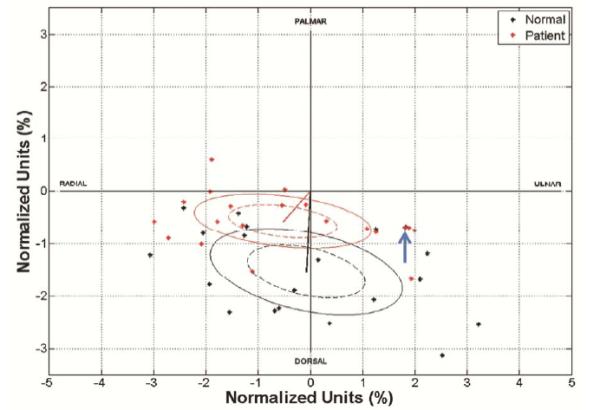
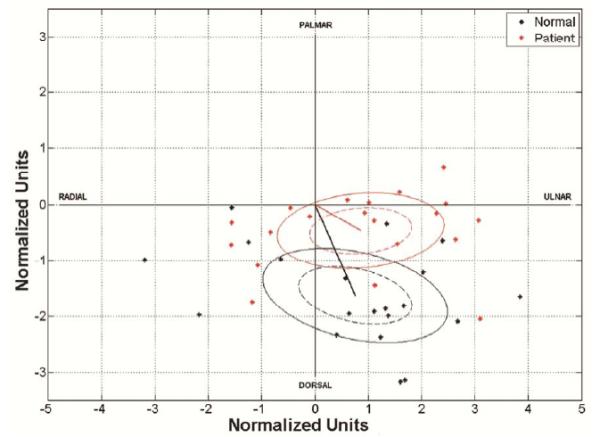
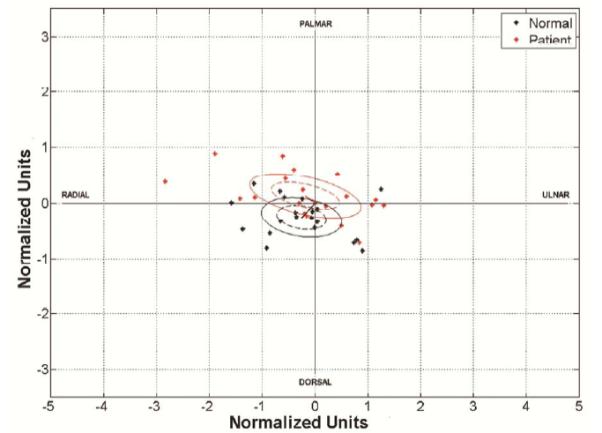
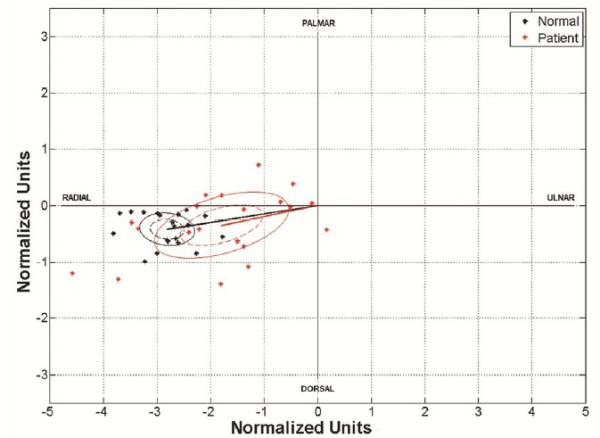
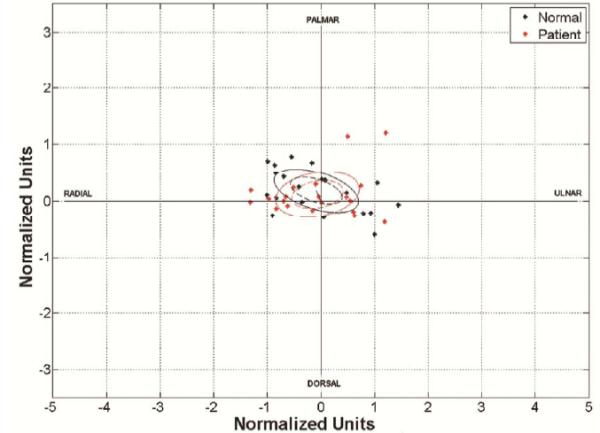
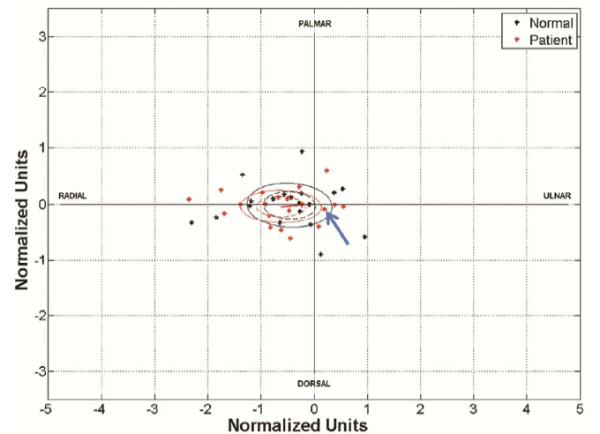
The median nerve displacement vectors in CTS patients. Solid ellipses represent standard deviation, dashed ellipses represent 95% confidence limits and the radial line represents the mean vector for each group. A. Wrist flexion with fingers extended. The arrow indicates two superimposed points from a patient and a healthy subject respectively. B. Wrist flexion with fingers flexed. C. Wrist extension with fingers extended. D. Wrist ulnar deviation with fingers extended. E. Finger flexion. F. Wrist extension with fingers flexed. The arrow indicates two superimposed points from a patient and a healthy subject respectively.
Normalized Magnitude of the Median Nerve Displacement
The normalized magnitudes of median nerve displacement are shown in Table 3. The normalized magnitudes of median nerve displacement in CTS patients were significantly less in wrist flexion with and without finger flexion, and wrist ulnar deviation compared to those in normal subjects (P=0.016, P=0.010 and P=0.005, respectively). No significant difference was found in the normalized magnitude of median nerve displacement for finger flexion and wrist extension with fingers extended or flexed between two groups (P>0.05).
Table 3.
Median nerve displacement normalized magnitudes.
| Magnitude of Median Nerve Displacement (NU) |
|
|---|---|
| Finger Flexion | |
| Patients | 0.75±0.44 |
| Healthy Subjects | 0.82±0.33 |
| Wrist Flexion with Fingers Extended | |
| Patients | 1.74±0.78* |
| Healthy Subjects | 2.36±0.79 |
| Wrist Flexion with Fingers Flexed | |
| Patients | 1.71±0.90** |
| Healthy Subjects | 2.46±0.84 |
| Wrist Extension with Fingers Extended | |
| Patients | 0.90±0.68 |
| Healthy Subjects | 0.77±0.46 |
| Wrist Extension with Fingers Flexed | |
| Patients | 0.85±0.56 |
| Healthy Subjects | 0.81±0.58 |
|
Wrist Ulnar Deviation with Fingers
Extended |
|
| Patients | 1.93±1.23** |
| Healthy Subjects | 2.86±0.51 |
P<0.05;
P<0.01
Note: 1 normalized unit (NU) is approximately 1.8 mm
DISCUSSION
Associations have been made between repetitive hand and wrist motions and the possible effect on the development of CTS (29, 30). Therefore, it is important to understand the kinematics of the median nerve during different wrist motions. In this study we evaluated the deformability and mobility of the median nerve at the proximal carpal tunnel during finger and wrist movements in CTS patients and compared these results to those previously reported for normal subjects (23). We found that with maximal wrist flexion with or without finger flexion and maximal ulnar deviation, the median nerve deformed and moved less in patients with CTS compared to healthy subjects.
Many studies have investigated deformation and mobility of the median nerve using imaging modalities, such as MRI and ultrasound (11-13, 22, 23, 31-33). Most studies have focused on the effect of finger motion (11-13, 33). Fewer studies have investigated median nerve displacement in the transverse plane during wrist movement (22-24, 31, 32). Most of these studies investigated the effect of wrist motion on median nerve shape and/or displacement in healthy subjects (22, 24, 34). They found that the median nerve remained palmar during wrist extension and, in most subjects, moved dorsally during wrist flexion. Greening et al. found reduced median nerve displacement in the transverse plane in patients with non-specific arm pain (31, 32). No CTS patients were included in their studies. Allmann et al. found that in 65% of the CTS patients included in the study, the median nerve moved less and remained near the flexor retinaculum during wrist flexion while the same occurred in only 27% of normal subjects (21). These results are consistent with our findings.
We observed that the deformation of the median nerve in CTS patients was decreased compared to healthy subjects. The normal median nerve deforms to accommodate finger or wrist movement (11, 12, 24). This may be related to the specific internal structure of median nerve. Histologically, the median nerve is composed of axons, which are bundled by several connective tissue layers (35, 36). The extensibility of these layers is critical for the nerve to accommodate tensile or compressive stress by elongating, gliding or deforming. In CTS progressive fibrosis has been found in the epineurial and perineurial connective tissues (37, 38). This fibrosis may result in a permanently decreased compliance of the median nerve during its movement in the carpal tunnel. Orman et al. used ultrasound elastography to evaluate the stiffness of median nerve in the carpal tunnel (39). They found that the median nerve was stiffer in patients with CTS than in normal subjects, which is consistent with the results of our study.
We also observed that the mobility of the median nerve was decreased in CTS patients. In the healthy carpal tunnel the tendons and nerve are surrounded by subsynovial connective tissue (SSCT), which is filmy and supple, and thus can facilitate smooth gliding and deformation of the median nerve in the carpal tunnel. In patients with CTS, the SSCT is fibrotic (40-42), which may cause the median nerve and tendons to become attached to adjacent structures, preventing the nerve from moving freely and causing it to become compressed between tendons and the flexor retinaculum during wrist flexion. This may explain why CTS symptoms are provoked by Phalen’s maneuver. Enlargement of the median nerve may also impair its mobility. An increased median nerve cross-sectional area is a well-known finding in CTS patients (43, 44). The decreased cross-sectional area of the carpal tunnel in wrist flexion (34) combined with the enlarged median nerve may further hinder the median nerve from moving dorsally between the flexor tendons.
Lastly, we found that the decreases in deformation and displacement of the median nerve in CTS patients were more evident during wrist flexion. This may be related to changes in the anatomy or pressure within the carpal tunnel during wrist flexion, compared to wrist extension or the neutral wrist position. In wrist flexion both the proximal and distal part of the carpal tunnel cross-sectional area are decreased compared to the neutral position (34, 45, 46). Furthermore the flexor tendons move palmarly with wrist flexion (47). Palmar movement of the flexor tendons may further contribute to the increased contact pressure on the median nerve.
Our study has several limitations. First, our study has a small sample size. Yet even with this small sample size we were able to note significant differences between CTS patients and healthy subjects (23). Second, the ultrasonographic results could not be correlated with the severity of the CTS due to the small sample size. Future studies with larger sample size are necessary to explore the relationship between the mobility and deformability of the median nerve and the severity of CTS. The data presented in the current study will serve as a useful baseline for future studies. Third, although we performed dynamic ultrasound of the median nerve, we only analyzed the median nerve in the first and final image of the movement. Dynamic changes, such as the path of motion, were not analyzed. This may provide additional useful information. However, analysis of the median nerve motion path is labor intensive and quantification is difficult. Measurement of the median nerve parameters in the first and last image is therefore a simple method for evaluating the mobility and deformability of the median nerve during wrist movement.
In summary, our study showed that CTS patients have a decreased deformability and mobility of the median nerve at the proximal carpal tunnel in the transverse plane with wrist flexion and ulnar deviation of the wrist. This study has revealed differences in median nerve transverse kinematics in the carpal tunnel between CTS patients and healthy subjects. Further studies with a larger sample of patients are necessary to determine if changes of kinematics of the median nerve can be related to severity of CTS and if these measurements may be usefulness for predicting treatment response.
Acknowledgements
This study was funded by grants from NIH/NIAMS AR 49823, Mayo Foundation, and UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Nakamichi K, Tachibana S. Restricted motion of the median nerve in carpal tunnel syndrome. J Hand Surg Br. 1995;20(4):460–4. doi: 10.1016/s0266-7681(05)80153-6. [DOI] [PubMed] [Google Scholar]
- 2.Ikeda K, Sarnura N, Tornita K. Segmental carpal canal pressure in patients with carpal tunnel syndrome. J Hand Surg Am. 2006;31A(6):925–9. doi: 10.1016/j.jhsa.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 3.Werner CO, Elmqvist D, Ohlin P. Pressure and nerve lesion in the carpal tunnel. Acta Orthop Scand. 1983;54(2):312–6. doi: 10.3109/17453678308996576. [DOI] [PubMed] [Google Scholar]
- 4.Coppieters MW, Alshami AM. Longitudinal excursion and strain in the median nerve during novel nerve gliding exercises for carpal tunnel syndrome. J Orthop Res. 2007;25(7):972–80. doi: 10.1002/jor.20310. [DOI] [PubMed] [Google Scholar]
- 5.Hough AD, Moore AP, Jones MP. Reduced longitudinal excursion of the median nerve in carpal tunnel syndrome. Arch Phys Med Rehabil. 2007;88(5):569–76. doi: 10.1016/j.apmr.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Szabo RM, Bay BK, Sharkey NA, Gaut C. Median Nerve Displacement through the Carpal Canal. J Hand Surg Am. 1994;19A(6):901–6. doi: 10.1016/0363-5023(94)90087-6. [DOI] [PubMed] [Google Scholar]
- 7.Tuzuner S, Ozkaynak S, Acikbas C, Yildirim A. Median nerve excursion during endoscopic carpal tunnel release. Neurosurgery. 2004;54(5):1155–60. doi: 10.1227/01.neu.0000119232.57668.98. discussion 60-1. [DOI] [PubMed] [Google Scholar]
- 8.Wright TW, Glowczewskie F, Wheeler D, Miller G, Cowin D. Excursion and strain of the median nerve. J Bone Joint Surg Am. 1996;78A(12):1897–903. doi: 10.2106/00004623-199612000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Yamaguchi T, Osamura N, Zhao CF, An KN, Amadio PC. Relative longitudinal motion of the finger flexors, subsynovial connective tissue, and median nerve before and after carpal tunnel release in a human cadaver model. J Hand Surg Am. 2008;33A(6):888–92. doi: 10.1016/j.jhsa.2008.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Korstanje JW, Scheltens-De Boer M, Blok JH, et al. Ultrasonographic assessment of longitudinal median nerve and hand flexor tendon dynamics in carpal tunnel syndrome. Muscle Nerve. 2012;45(5):721–9. doi: 10.1002/mus.23246. [DOI] [PubMed] [Google Scholar]
- 11.van Doesburg MH, Yoshii Y, Villarraga HR, et al. Median nerve deformation and displacement in the carpal tunnel during index finger and thumb motion. J Orthop Res. 2010;28(10):1387–90. doi: 10.1002/jor.21131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoshii Y, Villarraga HR, Henderson J, Zhao C, An K-N, Amadio PC. Ultrasound assessment of the displacement and deformation of the median nerve in the human carpal tunnel with active finger motion. J Bone Joint Surg Am. 2009;91A(12):2922–30. doi: 10.2106/JBJS.H.01653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Erel E, Dilley A, Greening J, Morris V, Cohen B, Lynn B. Longitudinal sliding of the median nerve in patients with carpal tunnel syndrome. J Hand Surg Br. 2003;28(5):439–43. doi: 10.1016/s0266-7681(03)00107-4. [DOI] [PubMed] [Google Scholar]
- 14.de Krom MC, Kester AD, Knipschild PG, Spaans F. Risk factors for carpal tunnel syndrome. Am J Epidemiol. 1990;132(6):1102–10. doi: 10.1093/oxfordjournals.aje.a115753. [DOI] [PubMed] [Google Scholar]
- 15.Keir PJ, Wells RP, Ranney DA, Lavery W. The effects of tendon load and posture on carpal tunnel pressure. J Hand Surg Am. 1997;22(4):628–34. doi: 10.1016/S0363-5023(97)80119-0. [DOI] [PubMed] [Google Scholar]
- 16.Rempel DM, Keir PJ, Bach JM. Effect of wrist posture on carpal tunnel pressure while typing. J Orthop Res. 2008;26(9):1269–73. doi: 10.1002/jor.20599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ko C, Brown TD. A fluid-immersed multi-body contact finite element formulation for median nerve stress in the carpal tunnel. Comput Methods Biomech Biomed Engin. 2007;10(5):343–9. doi: 10.1080/10255840701430480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith EM, Sonstegard DA, Anderson WH., Jr. Carpal tunnel syndrome: contribution of flexor tendons. Arch Phys Med Rehabil. 1977;58(9):379–85. [PubMed] [Google Scholar]
- 19.Yoshii YC, Zhao C, Zhao KDT, Zobitz ME, An K-N, Amadio PC. The effect of wrist position on the relative motion of tendon, nerve, and subsynovial connective tissue within the carpal tunnel in a human cadaver model. J Orthop Res. 2008;26(8):1153–8. doi: 10.1002/jor.20640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao CF, Ettema AM, Samura N, Berglund LJ, An KN, Amadio PC. Gliding characteristics between flexor tendons and surrounding tissues in the carpal tunnel: A biomechanical cadaver study. J Orthop Res. 2007;25(2):185–90. doi: 10.1002/jor.20321. [DOI] [PubMed] [Google Scholar]
- 21.Allmann KH, Horch R, Uhl M, et al. MR imaging of the carpal tunnel. Eur J Radiol. 1997;25(2):141–5. doi: 10.1016/s0720-048x(96)01038-8. [DOI] [PubMed] [Google Scholar]
- 22.Goetz JE, Thedens DR, Kunze NM, Lawler EA, Brown TD. Day-to-day variability of median nerve location within the carpal tunnel. Clin Biomech. 2010;25(7):660–5. doi: 10.1016/j.clinbiomech.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang Y, Zhao C, Passe SM, Filius A, Thoreson AR, An KN, Amadio PC. Quantitative Transverse Ultrasound to Analyze the Median Nerve Deformation and Displacement in the Human Carpal Tunnel during Wrist Movements. Ultrasound Med Biol. 2013 Nov 6; doi: 10.1016/j.ultrasmedbio.2013.09.009. doi:pii: S0301-5629(13)01017-X. 10.1016/j.ultrasmedbio.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeiss J, Skie M, Ebraheim N, Jackson WT. Anatomic Relations between the Median Nerve and Flexor Tendons in the Carpal-Tunnel - Mr Evaluation in Normal Volunteers. Am J Roentgenol. 1989;153(3):533–6. doi: 10.2214/ajr.153.3.533. [DOI] [PubMed] [Google Scholar]
- 25.Report of the Quality Standards Subcommittee of the American Academy of Neurology. Book Practice parameter for carpal tunnel syndrome (summary statement) Report of the Quality Standards Subcommittee of the American Academy of Neurology. 1993 Nov 01;:2406–9. Practice parameter for carpal tunnel syndrome (summary statement) ed. City1993. [PubMed] [Google Scholar]
- 26.Duncan I, Sullivan P, Lomas F. Sonography in the diagnosis of carpal tunnel syndrome. AJR Am J Roentgenol. 1999;173(3):681–4. doi: 10.2214/ajr.173.3.10470903. [DOI] [PubMed] [Google Scholar]
- 27.Clerke AM, Clerke JP, Adams RD. Effects of hand shape on maximal isometric grip strength and its reliability in teenagers. J Hand Ther. 2005;18(1):19–29. doi: 10.1197/j.jht.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 28.Batschelet E. Circular Statistics in Biology. Academic Press; 1981. [Google Scholar]
- 29.Harber P, Bloswick D, Beck J, Pena L, Baker D, Lee J. Supermarket checker motions and cumulative trauma risk. J Occup Med. 1993;35(8):805–11. doi: 10.1097/00043764-199308000-00018. [DOI] [PubMed] [Google Scholar]
- 30.Martin S. Carpal tunnel syndrome: a job-related risk. Am Pharm. 1991;NS31(8):21–4. doi: 10.1016/s0160-3450(16)33808-9. [DOI] [PubMed] [Google Scholar]
- 31.Greening J, Lynn B, Leary R, Warren L, O'Higgins P, Hall-Craggs M. The use of ultrasound imaging to demonstrate reduced movement of the median nerve during wrist flexion in patients with non-specific arm pain. J Hand Surg Br. 2001;26(5):401–6. doi: 10.1054/jhsb.2001.0582. [DOI] [PubMed] [Google Scholar]
- 32.Greening J, Smart S, Leary R, Hall-Craggs M, O'Higgins P, Lynn B. Reduced movement of median nerve in carpal tunnel during wrist flexion in patients with non-specific arm pain. Lancet. 1999;354(9174):217–8. doi: 10.1016/s0140-6736(99)02958-x. [DOI] [PubMed] [Google Scholar]
- 33.van Doesburg MH, Henderson J, Yoshii Y, et al. Median nerve deformation in differential finger motions: ultrasonographic comparison of carpal tunnel syndrome patients and healthy controls. J Orthop Res. 2012;30(4):643–8. doi: 10.1002/jor.21562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Skie M, Zeiss J, Ebraheim NA, Jackson WT. Carpal-Tunnel Changes and Median Nerve Compression during Wrist Flexion and Extension Seen by Magnetic-Resonance-Imaging. J Hand Surg Am. 1990;15A(6):934–9. doi: 10.1016/0363-5023(90)90019-n. [DOI] [PubMed] [Google Scholar]
- 35.Gamble HJ, Eames RA. An Electron Microscope Study of the Connective Tissues of Human Peripheral Nerve. J Anat. 1964;98:655–63. [PMC free article] [PubMed] [Google Scholar]
- 36.Geuna S, Raimondo S, Ronchi G, et al. Chapter 3: Histology of the peripheral nerve and changes occurring during nerve regeneration. Int Rev Neurobiol. 2009;87:27–46. doi: 10.1016/S0074-7742(09)87003-7. [DOI] [PubMed] [Google Scholar]
- 37.Clark BD, Barr AE, Safadi FF, et al. Median nerve trauma in a rat model of work-related musculoskeletal disorder. J Neurotrauma. 2003;20(7):681–95. doi: 10.1089/089771503322144590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.O'Brien JP, Mackinnon SE, MacLean AR, Hudson AR, Dellon AL, Hunter DA. A model of chronic nerve compression in the rat. Ann Plast Surg. 1987;19(5):430–5. doi: 10.1097/00000637-198711000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Orman G, Ozben S, Huseyinoglu N, Duymus M, Orman KG. Ultrasound elastographic evaluation in the diagnosis of carpal tunnel syndrome: initial findings. Ultrasound Med Biol. 2013;39(7):1184–9. doi: 10.1016/j.ultrasmedbio.2013.02.016. [DOI] [PubMed] [Google Scholar]
- 40.Ettema AM, Amadio PC, Zhao C, Wold LE, An KN. A histological and immunohistochemical study of the subsynovial connective tissue in idiopathic carpal tunnel syndrome. J Bone Joint Surg Am. 2004;86-A(7):1458–66. doi: 10.2106/00004623-200407000-00014. [DOI] [PubMed] [Google Scholar]
- 41.Lluch AL. Thickening of the synovium of the digital flexor tendons: cause or consequence of the carpal tunnel syndrome? J Hand Surg Br. 1992;17(2):209–12. doi: 10.1016/0266-7681(92)90091-f. [DOI] [PubMed] [Google Scholar]
- 42.Oh J, Zhao C, Zobitz ME, Wold LE, An KN, Amadio PC. Morphological changes of collagen fibrils in the subsynovial connective tissue in carpal tunnel syndrome. J Bone Joint Surg Am. 2006;88(4):824–31. doi: 10.2106/JBJS.E.00377. [DOI] [PubMed] [Google Scholar]
- 43.Visser LH, Smidt MH, Lee ML. High-resolution sonography versus EMG in the diagnosis of carpal tunnel syndrome. J Neurol Neurosurg Psychiatry. 2008;79(1):63–7. doi: 10.1136/jnnp.2007.115337. [DOI] [PubMed] [Google Scholar]
- 44.Wong SM, Griffith JF, Hui AC, Lo SK, Fu M, Wong KS. Carpal tunnel syndrome: diagnostic usefulness of sonography. Radiology. 2004;232(1):93–9. doi: 10.1148/radiol.2321030071. [DOI] [PubMed] [Google Scholar]
- 45.Horch RE, Allmann KH, Laubenberger J, Langer M, Stark GB. Median nerve compression can be detected by magnetic resonance imaging of the carpal tunnel. Neurosurgery. 1997;41(1):76–82. doi: 10.1097/00006123-199707000-00016. [DOI] [PubMed] [Google Scholar]
- 46.Yoshioka S, Okuda Y, Tamai K, Hirasawa Y, Koda Y. Changes in Carpal-Tunnel Shape during Wrist Joint Motion - Mri Evaluation of Normal Volunteers. J Hand Surg Br. 1993;18B(5):620–3. doi: 10.1016/0266-7681(93)90018-b. [DOI] [PubMed] [Google Scholar]
- 47.Keir PJ, Wells RP. Changes in geometry of the finger flexor tendons in the carpal tunnel with wrist posture and tendon load: an MRI study on normal wrists. Clin Biomech. 1999;14(9):635–45. doi: 10.1016/s0268-0033(99)00012-1. [DOI] [PubMed] [Google Scholar]


