Abstract
Background
The aim of this study was to test the ability of the Chinese version of the Mood Disorder Questionnaire (MDQ) to identify Bipolar Disorders (BD) in patients diagnosed with Major Depressive Disorder (MDD) or Unipolar Disorder (UD) in the clinical setting.
Methods
1,487 being treated for MDD or UD at 12 mental health centers across China, completed the MDQ and subsequently examined by the Mini International Neuropsychiatric Interview (MINI). Receiver Operating Characteristic(ROC) curves were used to determine the ability of the MDQ to differentiate between BD (BD, BD-I and BD-II) and MDD or UD and patients with BD-I from patients with BD-II.
Results
Of the 1,487 patients, 309 (20.8%) satisfied the DSM-IV criteria for BD: 118 (7.9%) for BD-I and 191 (12.8%) for BD-II. When only part one of the MDQ was used, the best cutoff was 7 between BD and UD (sensitivity 0.66, specificity 0.88, positive predictive value 0.59, negative predictive value 0.91), 6 between BD-II and UD, and 10 between BD-I and BD-II. If all three parts of the MDQ were used, the MDQ could not distinguish between BD and UD at a cutoff of 7 (or 6), and the sensitivity was only 0.22 (or 0.24).
Conclusion
The Chinese version of the MDQ had good psychometric features in screening bipolar disorders from depressive patients with mood disorders when part two and part three of the MDQ were ignored.
Introduction
Bipolar disorder (BD), also known as bipolar affective disorder or manic-depressive disorder. Individuals with BD experience episodes of an elevated or agitated mood known as mania/hypomania alternating with episodes of depression. Bipolar disorders have two main subtypes, bipolar I disorder (BD-I), bipolar II disorder (BD-II).The diagnosis of BD-I need one or more manic episodes. A depressive episode is not required for BD-I diagnosis, but it frequently occurs. The diagnosis of BD-II need one or more hypomanic episodes (without manic episode) and one or more major depressive episode. Bipolar disorder not otherwise specified (BD-NOS) is a catchall category, diagnosed when the disorder does not fall within a specific subtype. Hypomanic episode do not go to the full extremes of mania (i.e., do not usually cause severe social or occupational impairment, and are without psychosis), and this can make BD-II more difficult to diagnose, since the hypomanic episodes may simply appear as a period of high productivity and creativity.
BD is a common disorder. Lifetime prevalence estimates are 1.0% for BD-I, 1.1% for BD-II, and 2.4% for subthreshold BD in the general adult population (aged ≥18 years) in the United States [1]. In a large community cohort in Europe, the prevalence of bipolar disorder (BD-I and BD-II) based on the DSM-IV criteria was 5.5% [2]. Bipolar disorders cause role impairment and high mortality and economic burden [3]. In practice, many patients with BD experience a delay in initiating treatment or are given the wrong treatment because of the under-recognition and frequent misdiagnosis of this disorder [4]–[6]. Of the self-rating mania/hypomania questionnaires developed to screen for BD [7], [8], the Mood Disorder Questionnaire (MDQ) is one that has been used effectively in many countries [7], [9]–[14].
The MDQ consists of three parts. In part one, the MDQ screens for a lifetime history of manic/hypomanic symptoms using 13 yes/no items. The second part asks whether two or more manic/hypomanic symptoms have been experienced during the same period. Part three assesses the level of functional impairment due to the symptoms on a 4-point scale (“no” to “severe”) [7], [15]. There are disagreements with respect to the scoring of the MDQ. Hirschfeld et al (2000) recommended that the positive response to MDQ required the presence of at least seven symptoms that co-occur and caused moderate to severe impairment due to the manic/hypomanic symptoms [7]. Some studies [9], [11] have found that the MDQ may be insensitive in the detection of BD due to the items in part three. Some studies have proposed modifying the MDQ scoring by ignoring part three and lowering the threshold screening for BD. The patients' assessments of functional impairment in the part three were influenced mostly by their insight, an area that is typically impaired in the patients with BD [16]–[18]. Secondly, because impairment in functioning is not necessary to diagnose hypomania, requiring impairment on the MDQ to determine BD will reduce its sensitivity for detecting BD-II [19]. In an earlier and smaller-sample Chinese study, in which the threshold number of symptom items co-occurring in the same time period and causing moderate or severe impairment was not rated, patients with a total score equal to or higher than 7 were identified as potentially suffering from BD [13]. It was not clear if all three parts of the MDQ could be used in clinical settings in China.
In most studies concerning the MDQ, including the earlier study in China, testing of subjects with mood disorders was not restricted to the depressive phase [7], [9]–[13]. Still, mood phases may have an impact on the results of these self-rating questionnaires [19], [20]. Patients with BD in the depressive phase have difficulty recalling past manic/hypomanic symptoms [21]. In addition, a depressive episode is usually the first mood syndrome at the onset of BD, and depressive episodes are more frequent than manic/hypomanic episodes [22], often leading to the misdiagnosis of BD as major depressive disorder (MDD), also called unipolar depression (UD). Therefore, it was necessary to study the response of the patients with mood disorders to the MDQ during their depressive phase.
We conducted this study to determine (1) which parts of the Chinese version of the MDQ should be used to screen for BD in the clinical setting; (2) compare the use of the MDQ for patients during the depressive phase with a previous study in which the MDQ was administered during any phase (mania, depression) and (3) determine if the results of our previous study of the MDQ in two psychiatric hospitals could be replicated in other centres which included psychiatric clinics and general hospitals across China.
Methods
Study participants and settings
The Diagnostic Assessment Service for People with Bipolar Disorders in China (DASP) is an ongoing national study initiated by the Chinese Society of Psychiatry (CSP) with the aim of developing and testing the usefulness of screening tools for BD in patients treated for MDD. The first survey of the DASP project was carried out in 13 major psychiatric hospitals and units of general hospitals between September 1, 2010 and February 28, 2011. These settings were evenly distributed in China and served both catchment area patients and patients from neighboring areas. Both in- and outpatients experiencing a major depressive episode were enrolled if they were between 16 and 65 years of age, had a DSM-IV or ICD-10 diagnosis of MDD based on a review of their medical records, understood the aims of the study and provided informed consent. Exclusion criteria included a past diagnosis of BD, ongoing significant medical or neurological condition(s), depressive disorders secondary to a general medical or neurological condition, or having received electroconvulsive therapy (ECT) in the past month. The study protocol was approved by the Clinical Research Ethics Committees of the respective study centers. All patients who participated in this study completed written consent forms.
Instrument and assessment procedure
In- or outpatients in a depressive state with a diagnosis of MDD who were receiving treatment in the participating hospitals/units were referred by their treating psychiatrists to the member of the research team based at their particular site and screened for eligibility. All members of the research team were qualified psychiatrists. Patients fulfilling the study criteria were invited to participate in the study.
The patients' basic socio-demographic data were collected with a questionnaire designed for the study in a clinical interview, supplemented by a review of their medical records (Table 1). The diagnostic assessment of BD was conducted with the validated Chinese version of the Mini International Neuropsychiatric Interview (MINI) (Version 5.0) to establish DSM-IV BD-I/BD-II diagnoses [23], [24].
Table 1. Description of samples.
| BD-I | BD-II | UD | P | ||
| Number | 118 | 191 | 1178 | ||
| Age | 35.43 | 35.46 | 40.54 | <0.01 | |
| Sex | Male | 51 | 97 | 385 | <0.01 |
| Marriage state | Married | 76 | 116 | 824 | = 0.01 |
| Unmarried | 37 | 68 | 288 | ||
| Divorced | 5 | 7 | 47 | ||
| Loss | 0 | 0 | 19 | ||
| Job | Employed | 68 | 110 | 617 | >0.05 |
| Retired | 8 | 26 | 195 | ||
| Unemployed | 42 | 55 | 366 | ||
| Education | Lower than senior high school | 31 | 52 | 356 | = 0.48 |
| Senior high school Equal to a | 32 | 44 | 312 | ||
| Bachelor's degree | 47 | 85 | 465 | ||
| Postgraduate | 8 | 10 | 45 | ||
The MINI is a short, structured diagnostic interview that was developed jointly by psychiatrists and clinicians for DSM-IV psychiatric disorders. It was designed to meet the need for a short (approximately 15 minutes) but accurate structured psychiatric interview for multicenter clinical trials [23]. The Chinese version of the MINI showed strong reliability and validity in eliciting symptom criteria used to make DSM diagnoses [24]. The Chinese version of the MDQ (C-MDQ) has been validated in China [13]. The internal consistency (Cronbach's alpha) of the C-MDQ was 0.79. Sensitivity was 0.64, specificity was 0.80 and the area under curve was 0.75 at the optimal screening cutoff between BD and UD [13].
All twelve raters in this study were trained in diagnosing BD using the MINI in 20 MDD patients prior to the study. In the reliability exercise, raters' judgments of BD were compared with the best estimate clinical diagnoses [25]; the kappa values were above 0.85 for each rater. Patients younger than 18 years were included as long as they verbally agreed to participate and written consent was obtained from patients or guardians. After giving consent, patients were invited to complete the C-MDQ. Patients then underwent a DSM-IV diagnostic interview using the MINI by a rater who was blind to the C-MDQ results.
Statistical analysis
Data were analyzed using the SPSS package, Version 17.0. One-way analysis of variance (ANOVA) and t-tests were used to compare the MDQ scores among the mood disorder patients. The receiver operating characteristic (ROC) curve was used to determine whether the patients with different mood disorders (BD, BD-I, BD-II, MDD) could be differentiated and to ascertain the sensitivity (SEN) and specificity (SPE) at various cutoffs. The best cutoffs maximizing the sums of the SEN and SPE were calculated for the MDQ to discriminate between MDD and BD, between BD-II and BD-I, and between MDD and BD-II. The criterion validity of the MDQ was estimated using the SEN, SPE, positive predictive value (PPV), negative predictive value (NPV) and the area under the curve (AUC).
Results
1. Description of samples
Altogether, 1,757 patients were invited to participate in this study; 270 refused to participate or failed to complete the interview. There were no significant differences between the enrolled patients and patients who did not participate in terms of age and sex. Ultimately, 1,487 patients were included in the analysis. Of the 1,487 patients, 309 (20.8%) satisfied the DSM-IV criteria for BD: 118 (7.9%) for BD-I and 191 (12.8%) for BD-II. Table 1 displays the socio-demographic characteristics of the whole sample and separately for patients by diagnosis.
2. MDQ scores
The mean MDQ score was 7.29 (SD 3.23) for BD, 8.01 (SD 3.44) for BD-I, 6.85 (SD 3.02) for BD-II and 2.91 (SD 2.75) for UD. There was a significant difference among the scores of depressive patients with BD-I, BD-II or UD based on one-way analysis of variance (P<0.01, ANOVA). The mean MDQ score for BD patients was significantly higher than that of UD; BD-I was higher than BD-II, and BD-II was higher than UD (t-test, P<0.01).
3. Only part one of MDQ used
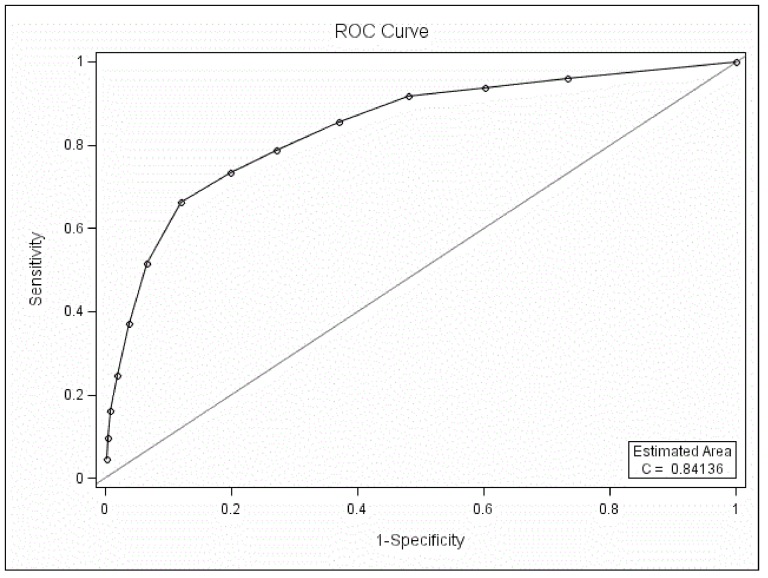
3.1. ROC curve analysis between BD and UD
The MDQ could differentiate BD patients from UD patients when only part one was used in the ROC curve analysis (P<0.05, Figure 1). The AUC was 0.84. The best screening cutoff between BD and UD was 7 (SEN 0.66, SPE 0.88, PPV 0.59, NPV 0.91).
Figure 1. ROC curve analysis between BD and BD with only part one of the MDQ scored.
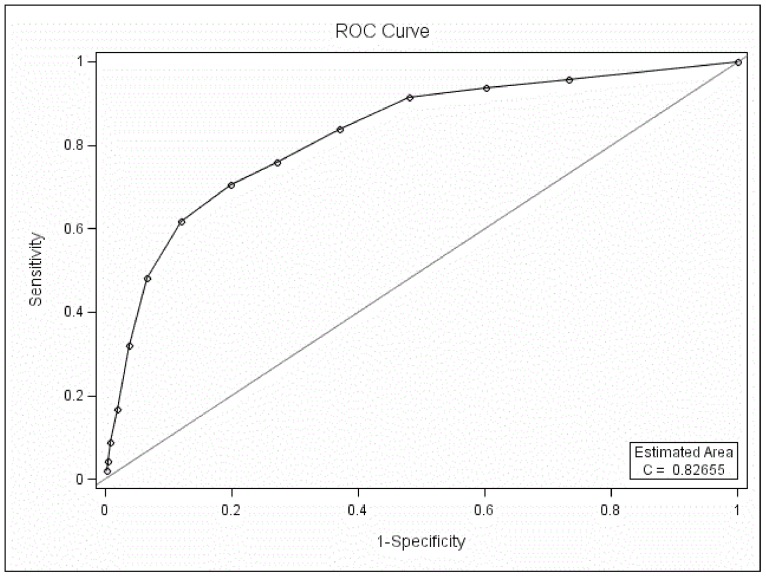
3.2. ROC curve analysis between BD-I I and UD
The MDQ could differentiate BD-II patients from UD patients when only part one was used in the ROC curve analysis (P<0.05, AUC 0.83, Figure 2). The best screening cutoff between BD-II and UD was 6 (SEN 0.71, SPE 0.80, PPV 0.37, NPV 0.94).
Figure 2. ROC curve analysis between BD-II and UD with only part one of the MDQ scored.
Because the mean MDQ score of the patients with BD-I was highest and that of UD was lowest, and MDQ could screen BD-II patients from UD patients by ROC analysis, we did not compare BD-I and UD in the ROC analysis.
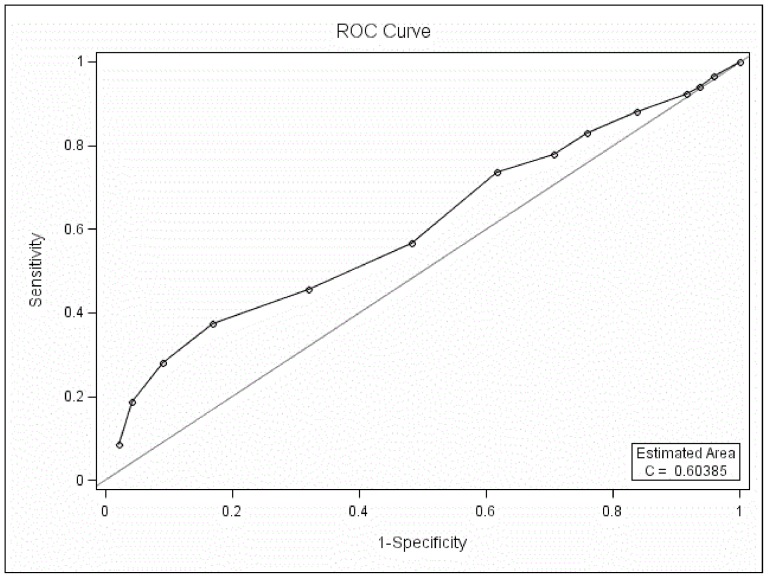
3.3. ROC curve analysis between BD-I and BD-II
The MDQ could differentiate BD-I patients from BD-II when only part one was used in the ROC curve analysis (P<0.05, AUC 0.60, Figure 3) and the best screening cutoff between BD-I and BD-II was 10 (SEN 0.37, SPE 0.83, PPV 0.58, NPV 0.59).
Figure 3. ROC curve analysis between BD-I and BD-II with only part one of the MDQ scored.
Compared to the higher AUC between BD and UD (0.84), between BD-II and UD (0.83), the AUC between BD-I and BD-II is low (0.60) and might limit its usefulness.
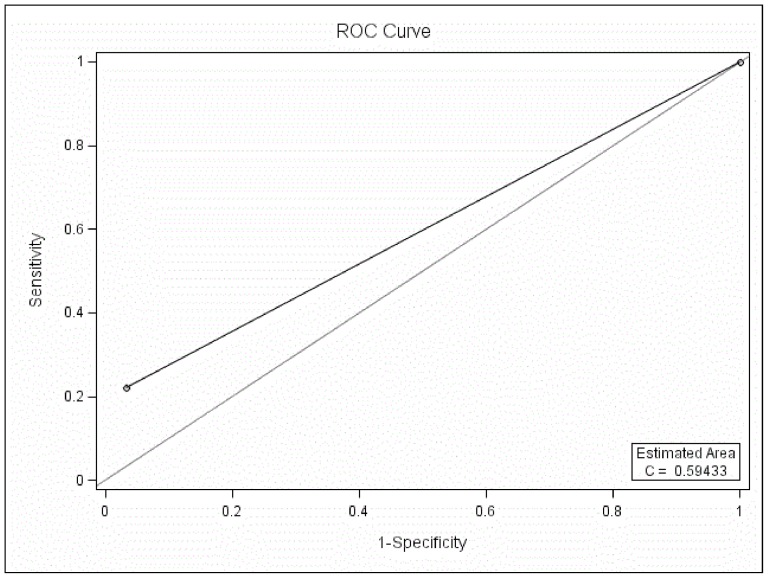
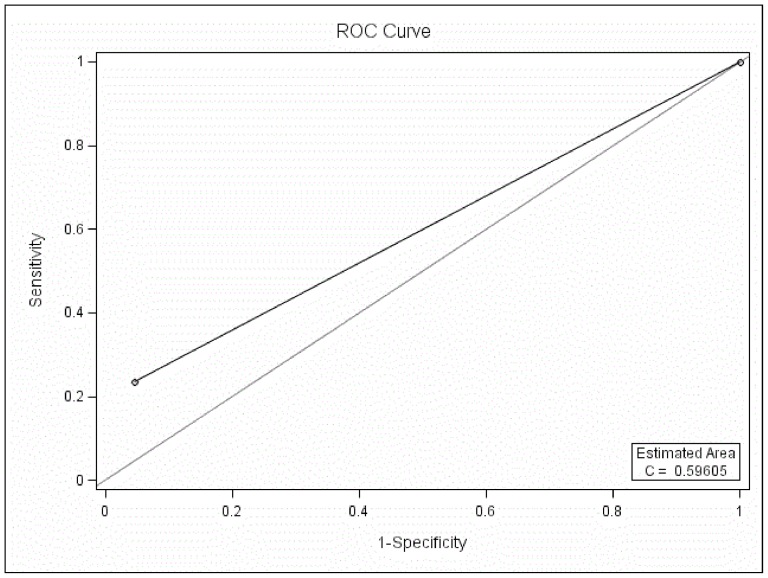
4. All three parts of MDQ used
4.1. If the cutoff was 7 between BD and UD
The MDQ could not differentiate BD patients from UD patients at the cutoff of 7 when all three parts of the MDQ were used in the ROC curve analysis (P>0.05, AUC 0.59, SEN 0.22, SPE 0.97, PPV 0.65, NPV 0.83, Figure 4).
Figure 4. ROC curve analysis between BD and UD at the cutoff of 7 with three parts of the MDQ scored.
4.2. If the cutoff was 6 between BD and UD
If the best cutoff of 6 between BD-II and UD was used as the optimal screening cutoff between BD and UD, the MDQ could not differentiate BD patients from UD when all three parts of the MDQ were used in the ROC curve analysis (P>0.05, AUC 0.60, SEN 0.24, SPE 0.96, PPV 0.58, NPV 0.83, Figure 5).
Figure 5. ROC curve analysis between BD and UD at the cutoff of 6 with three parts of the MDQ scored.
Discussion
In this study, we found that if only part one of MDQ was used, MDQ could differentiate between BD and UD, between BD-II and UD, and between BD-I and BD-II. Because the treatments of different types of mood disorders and subtypes of bipolar disorders are different, MDQ which help clinicians in differentiating mood disorders is useful in practice.
The MDQ scores of depressive patients with BD-I were higher than those with BD-II, which were higher than for those with UD. The MDQ scores of depressive patients with mood disorders were lowest in patients with UD, followed by BD-II and BD-I. The change of MDQ score in patients with mood disorders was similar to that of the earlier Chinese study, which did not limit patients to the depressive phase [13].
When only part one of the MDQ was used, the best screening cutoff between depressed patients with BD and depressed patients with UD was 7 in this study. The cutoff was identical in most of the MDQ studies conducted worldwide, including the earlier study in China in which patients could be in any mood phase [7], [9], [12]–[14]. The feature of relatively low sensitivity (0.66) and higher specificity (0.88) in this study was similar to that of other studies as well [7], [9], [13]–[14]. The stable cutoff between BD and UD suggested that the impact of the type of mood episode for the patients with mood disorders on the MDQ score was minimal and could be ignored.
Again, when only part one of the MDQ was used, the best screening cutoff between BD-I and BD-II was 10, a different finding from the cutoff of 8 in the earlier study from China. The best screening cutoff between BD-II and UD was 6, while the cutoff was 5 in an earlier study [13]. Although the definite cutoffs were different, this study demonstrated again that the MDQ could screen patients with BD-I from patients with BD-II, and patients with BD-II from UD [13]. The low AUC (0.60) between BD-I and BD-II might limit its usefulness compared to the higher AUC (0.83) between BD-II and UD.
When all three parts were used, the MDQ could not be used as a screening tool in clinical settings. Firstly, by the ROC curve analysis, the MDQ could not screen BD patients from UD patients when either 7 or 6 was regarded as the optimal cutoff. We suggest that the best screening cutoff between BD-II and UD could also be used as the optimal cutoff between BD and UD to improve screening for BD-II [13]. Secondly, the sensitivities 0.22 (or 0.24) were too low to screen at cutoffs 7 (or 6) for a screening tool. Our results were similar to the results from a study in Korea. Kim et al (2008) found that a modified scoring of the MDQ (ignoring questions on the co-occurrence of symptoms and functional impairment) yielded an SEN of 0.68 and an SPE of 0.63 for BD, whereas the values were 0.29 and 0.77, respectively, using the standard MDQ scoring [9]. The results of the Korean study were similar to ours. Therefore, we suggested that only part one of the MDQ (13 items of manic/hypomanic symptoms) should be scored if the MDQ is to be used as a screening tool for the patients with mood disorders in clinical settings.
There were two limitations in the study. Firstly, we could not compare the severity of depression between patients because no standardized instrument was used to measure the severity of depressive symptoms. Secondly, depressed patients who had a previous diagnosis of BD were excluded from the study. The subjects with BD in this study may not be representative of all BD patients.
Conclusions
Firstly, the C-MDQ, using only part one, is suitable to screen for BD in clinical settings. Secondly, the MDQ results for mood disorder patients in the depressive phase were similar to those of mood disorder patients in any mood phase. Thirdly, the results of this multicenter study were similar to those of the earlier study that was limited to two psychiatric hospitals in China.
Acknowledgments
The authors are grateful to all the clinicians who helped to organize the study at each study site.
Funding Statement
This study was funded by the grant (200602032) from the scientific and technological bureau of Shenzhen in China. The study was initiated by the Chinese Society of Psychiatry (CSP) with support from AstraZeneca China. AstraZeneca China had no role in the study design or in the generation and interpretation of the results. The funders had no role in study design, data collection and analysis,decision to publish, or preparation of the manuscript.
References
- 1. Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, et al. (2007) Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Archives of General Psychiatry 64: 543–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Angst J (1999) Major depression in 1998: are we providing optimal therapy? J Clin Psychiatry 60 (Suppl 6) 5–9. [PubMed] [Google Scholar]
- 3. Kemp DE, Hirschfeld RM, Ganocy SJ, Elhaj O, Slembarski R, et al. (2008) Screening for bipolar disorder in a county jail at the time of criminal arrest. J Psychiatric Research 42: 778–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hantouche EG, Akiskal HS, Lancrenon S, Allilaire JF, Sechter D, et al. (1998) Systematic clinical methodology for validating bipolar-II disorder: data in mid-stream from a French national multi-site study (EPIDEP). J Affect Disord 50: 163–73. [DOI] [PubMed] [Google Scholar]
- 5. Manning JS, Haykal RF, Connor PD, Akiskal HS (1997) On the nature of depressive and anxious states in a family practice setting: the high prevalence of bipolar II and related disorders in a cohort followed longitudinally. Compr Psychiatry 38: 102–8. [DOI] [PubMed] [Google Scholar]
- 6. Hirschfeld RM, Lewis L, Vornik LA (2003) Perceptions and impact of bipolar disorder: how far have we really come? Results of the national depressive and manic-depressive association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry 64: 161–74. [PubMed] [Google Scholar]
- 7. Hirschfeld RM, Williams JB, Spitzer RL, Calabrese JR, Flynn L, et al. (2000) Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry 157: 1873–5. [DOI] [PubMed] [Google Scholar]
- 8. Angst J, Adolfsson R, Bennazzi F, Gamma A, Hantouche E, et al. (2005) The HCL-32: Towards a self-assessment tool for hypomanic symptoms in outpatients. J Affect Disord 88: 217–233. [DOI] [PubMed] [Google Scholar]
- 9. Kim B, Wang RH, Son JI, Kim CY, Joo YH (2008) Bipolarity in depressive patients without histories of diagnosis of bipolar disorder and the use of the mood disorder questionnaire for the detecting bipolarity. Compr Psychiatry 49: 469–475. [DOI] [PubMed] [Google Scholar]
- 10. Hardoy MC, Cadeddu M, Murru A, Dell'Osso B, Carpiniello B, et al. (2005) Validation of the Italian version of the Mood Disorder Questionnaire for the screening of bipolar disorders. Clinical Practice and Epidemiology in Mental Health 1: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Weber RB, Gervasoni N, Dubuis V, Gex-Fabry M, Bondolfi G, et al. (2005) Screening for bipolar disorders using a French version of the Mood Disorder Questionnaire (MDQ). J Affect Disord 88: 103–108. [DOI] [PubMed] [Google Scholar]
- 12. Konuk N, Kiran S, Tamam L, Karaahmet E, Aydin H, et al. (2007) Validation of the Turkish version of the mood disorder questionnaire for screening bipolar disorder. Turkish Journal of Psychiatry 18: 147–154. [PubMed] [Google Scholar]
- 13. Yang HC, Yuan CM, Liu TB, Li LJ, Peng HJ, et al. (2011) Validity of the Chinese version Mood Disorder Questionnaire (MDQ) and the optimal cutoff screening bipolar disorders. Psychiatry Res 189: 446–50. [DOI] [PubMed] [Google Scholar]
- 14. Isometsa E, Suominen K, Mantere O, Valtonen H, Valtonen H, et al. (2003) The mood disorder questionnaire improves recognition of bipolar disorder in psychiatric care. BMC Psychiatry 3: 8–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hirschfeld RM, Holzer C, Calabrese JR, Weissman M, Reed M, et al. (2003) Validity of the Mood Disorder Questionnaire: A general population study. Am J Psychiatry 160: 178–180. [DOI] [PubMed] [Google Scholar]
- 16. Dell'Osso L, Pini S, Cassano GB, Mastrocinque C, Seckinger RA, et al. (2002) Insight into illness in patients with mania, mixed mania, bipolar depression and major depression with psychotic features. Bipolar Disorders 4: 315–322. [DOI] [PubMed] [Google Scholar]
- 17. Miller CJ, Klugman J, Berv DA, Rosenquist KJ, Ghaemi SN (2004) Sensitivity and specificity of the Mood Disorder Questionnaire for detecting bipolar disorder. J Affect Disorders 81: 167–71. [DOI] [PubMed] [Google Scholar]
- 18. Zimmerman M, Galione JN, Ruggero CJ, Chelminski I, McGlinchey JB, et al. (2009) Performance of the mood disorders questionnaire in a psychiatric outpatient setting. Bipolar Disorders 11: 759–765. [DOI] [PubMed] [Google Scholar]
- 19. Wu YS, Angst J, Ou CS, Chen HC, Lu RB (2008) Validation of the Chinese version of the Hypomania Checklist(HCL-32) as an instrument for detecting hypo(mania) in patients with mood disorders. J Affect Disord 106: 133–143. [DOI] [PubMed] [Google Scholar]
- 20. Yang HC, Yuan CM, Liu TB, Li LJ, Peng HJ, et al. (2011) Validity of the 32-item Hypomania Checklist (HCL-32) in a clinical sample with mood disorders in China. BMC Psychiatry 11: 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Akiskal HS, Benazzi F (2005) Optimizing the detection of bipolar II disorder in outpatient private practice: toward a systematization of clinical diagnostic wisdom. J Clin Psychiatry 66: 914–21. [DOI] [PubMed] [Google Scholar]
- 22. Solomon DA, Leon AC, Maser JD, Truman CJ, Coryell W, et al. (2006) Distinguishing bipolar major depression from unipolar major depression with the screening assessment of depression-polarity (SAD-P). J Clin Psychiatry 67: 434–42. [DOI] [PubMed] [Google Scholar]
- 23. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59 Suppl 20: 22–33 quiz 34–57. [PubMed] [Google Scholar]
- 24. Si TM, Shu L, Dang WM, Su YA, Chen JX, et al. (2009) Evaluation of the Reliability and Validity of Chinese Version of the Mini International Neuropsychiatric Interview in Patients with Mental Disorders (in Chinese). Chinese Mental Health Journal 23: 493–503. [Google Scholar]
- 25. Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM (1982) Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry 39: 879–83. [DOI] [PubMed] [Google Scholar]