Abstract
Objective
The purpose of this case report is to describe the chiropractic and dental comanagement of a patient with temporomandibular dysfunction, headaches, and myalgia.
Clinical features
A 38-year-old black female patient presented for chiropractic care with a chief concern of jaw pain, tinnitus, headaches, and neck and shoulder soreness of 8 months’ duration. The patient rated the pain a 6/10. The patient had a maximum mouth opening of 42 mm, graphed evidence of disk displacement, loss of translation on opening of the right temporomandibular joint viewed on the lateral radiograph, and numerous areas of point tenderness on the Kinnie-Funt Chief Complaint Visual Index. She had decreased lateral cervical flexion.
Intervention and outcome
Dental treatment consisted of an anterior repositioning splint. Chiropractic care consisted of Activator treatment to the pelvis and the thoracic and cervical spine. Manual manipulation of the temporomandibular joint was performed along with a soft tissue technique intraorally on the lateral pterygoid. Postisometric relaxation in the head and neck region was also done. The patient was treated 6 times over 3 weeks. At the end of treatment, the patient had a pain rating of 0/10, maximum mouth opening of 49 mm, no tender points on the follow-up Kinnie-Funt, and increased cervical range of motion.
Conclusion
The patient demonstrated increased mouth opening, decreased pain rating, improved Kinnie-Funt visual index, and an increased cervical lateral flexion range of motion after 3 weeks of a combination of chiropractic and dental care.
Key indexing terms: Temporomandibular joint disorders, Delivery of care, Chiropractic, Dentistry
Introduction
Temporal mandibular dysfunction (TMD) affects more than 25% of the general population.1 A study documenting the use of complementary and alternative medicine (CAM) for TMD showed nearly two-thirds of patients reported using CAM services for treatment.2 As patients are already seeking alternative care, it is possible that collaborative efforts between professions could address coexisting problems in patients with TMD.
A patient with TMD may have multiple conditions that may be related and managed separately. For example, a case described a patient who presented to a doctor of chiropractic with low back pain and obtained relief after the addition of dental orthopedic treatment.3 The opposite results may occur, such as a patient with jaw pain who was treated dentally with no relief and then chiropractic care provided the patient with relief.4
There have been arguments for a more holistic and collaborative approach to treating TMD. The stomatognathic system includes all of the structures involved in speech and in the reception, mastication, and deglutition of food.6 Ramirez et al5 suggest that “The team work structure can be the best option to obtain the best functional state in the stomatognathic system.” As well, there are various associations between TMD and musculoskeletal pain. For example, a study found a correlation between sleep bruxism and the occurrence of TMD and arthralgia.7 The stomatognathic system has an important effect on the nervous system, and TMD can have related symptoms such as tinnitus and headache.8 For example, a study showed a correlation between cervicogenic headaches and TMD, with 44.1% of participants with cervicogenic headaches also having TMD.9
At present, there are few reports of collaborative approaches between dentists and doctors of chiropractic for the comanagement of TMD. Therefore, the purpose of this study is to describe the collaborative treatment of a patient with TMD, headaches, and myalgia.
Case Report
A 38-year-old black female patient presented for chiropractic treatment with a chief concern of TMD, headaches, and neck and shoulder pain with a duration of 8 months.
The patient had a history of a head-on collision 16 years prior in which she hit her face on the steering wheel. She also reported a 20-year history of bruxism. The patient reported no current prescription or over-the-counter medication use. Prior to her visit, the patient was diagnosed with TMD by an otorhinolaryngologist who also gave a preliminary diagnosis of fibromyalgia and therefore referred her to a dentist. The dentist evaluated the patient and referred her for chiropractic care and comanagement.
History revealed that her jaw pain was on the left side with clicking and popping with jaw range of motion. The patient reported constant pain on the left frontal aspect of her head with retroorbital pressure that she rated at a 6/10 on a numeric pain scale.10,11 She had an increase in pain with chewing, and nothing reduced it. The patient had associated tinnitus in the left ear.
The patient filled out the Kinnie-Funt Chief Complaint Visual Index for Head, Neck, and Facial Pain and TMJ Dysfunction to list and prioritize her complaints (Fig 1). She ranked the following as her top 3 complaints: pressure behind the eyes; “migraine”-type headache; and an inability to open smoothly, evenly. The patient also noted additional complaints on the form of clenching; grinding; clicking; popping jaw joints; ringing in the ears; neck pain with tired, sore neck muscles; and shoulder aches.
Fig 1.
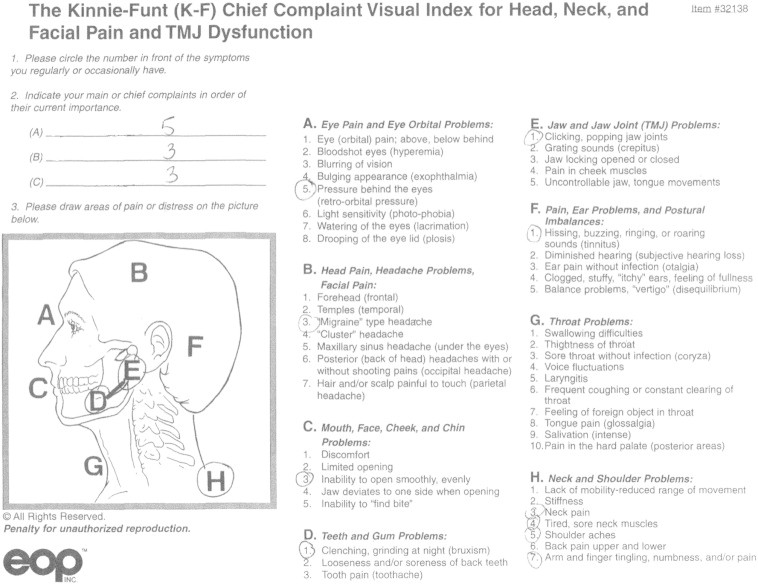
Initial Kinnie-Funt visual index. (Kinnie-Funt index reproduced with permission of EOP Inc, Little Canada, MN)
This patient was evaluated initially with the joint vibration analysis (Biopak from Bio-Research Associates, Inc, Brown Deer, WI). The results showed the mandible deflecting 8 mm to the left at the maximal mouth opening (MMO) of 42 mm. Continued measurement of the MMO was performed with the TheraBite ruler (Atos Medical, Horby, Sweden). This method has been used in the research to measure MMO.12 There were vibration and increased friction found on the left side showing a small-amplitude vibration indicative of a posterior disk derangement that reduces. Vibrational analysis has been researched and shown to differentiate a temporomandibular joint (TMJ) with a reducing disk vs a normal TMJ.12 This is similarly seen in research showing an anterior disk derangement that reduces.13 The graph below shows several recurring vibrations, most notably the one marked “2” at a regular interval approximately an inch long that occurs just after the peak in the curve (Fig 2). Lateral radiographs of the TMJ were done bilaterally to show the translation of the joints (Fig 3). The right TMJ had less translation as compared with the left correlating with palpation of the TMJ, which showed a reduction in motion on the right. Muscles in the head, neck, and facial region were found to have moderate to severe tenderness including the temporalis, masseter, medial and lateral pterygoids, buccinator, lateral TMJ capsule, posterior TMJ space, trapezius, sternocleidomastoid, splenius capitus, and suboccipitals. Cervical range of motion was found to be reduced during active range of motion with right lateral flexion at 25 and left lateral flexion at 35. All other ranges were within normal limits. The cervical range of motion was measured with a single-bubble inclinometer.14
Fig 2.
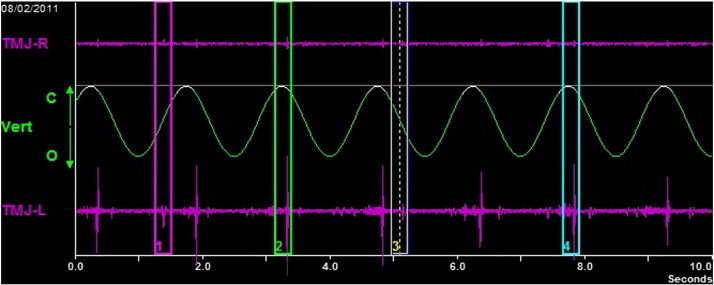
Joint vibrational analysis. (Color version of figure is available online.)
Fig 3.
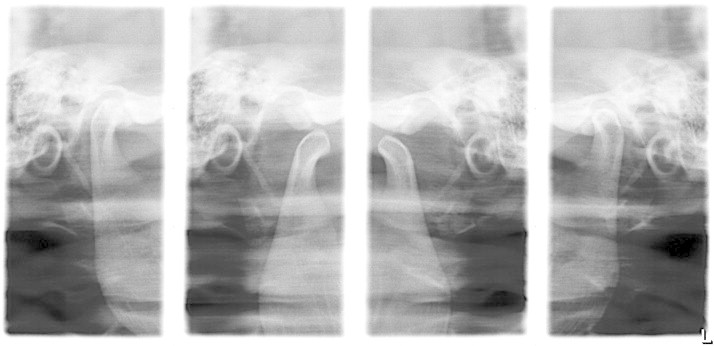
Lateral TMJ radiographs open and closed.
Chiropractic treatment included spinal manipulative therapy of the pelvis and the cervical and thoracic spine with Activator technique according to Activator protocol. The pelvis was adjusted to correct pelvic unleveling; and the thoracic spine was adjusted along with the cervical spine to address the point tenderness in the neck and shoulder region, as well as to help with any altered head position and to increase the MMO.15 Because the positions of the jaw and head and neck are intricately linked,16 manual therapy was performed on the left TMJ. This was done by placing the thumb on the left lower molars intraorally and the index finger hooking on to the inferior aspect of the mandible on that side. Then the wrist was ulnar deviated to distract the joint; and while in distraction, the mandible was moved in such a manner that the mandibular condyle moved medial and lateral attempting to recapture the disk. Furthermore, postisometric relaxation was performed on the trapezius, suboccipital, and masseter muscles. This technique is commonly used and has been shown to be effective in other case reports.17,18 Myofascial release was performed on the lateral pterygoid by having the patient open slightly and sliding the index finger along the gingiva to the lateral pterygoid and then having the patient turn her head away from the side of contact. The opposite hand was then placed flat on the temporal bone, and light compressions were done; as the lateral index slid back, the lateral pterygoid relaxed. A study using a similar technique for a pterygoid release intraorally found improvement in MMO and in jaw pain at rest and upon opening in patients with TMD.19,20 This treatment was performed twice a week for 3 weeks for a total of 6 visits. The diagnosis and care given to the patient were communicated to the dentist.
Dental comanagement consisted of an initial, temporary anterior repositioning splint made out of heated beads directly molded in the patient’s mouth. Impressions were then taken to make a custom-made splint that is inserted on the mandible and a maxillary splint for nighttime both used for mandibular advancement. Anterior repositioning splints have been shown in the research to be good at reducing not only joint pain but also joint sounds in patients with TMD.21 Anterior repositioning splints are used to stretch the muscles, recapture the disk, and unload the joint. Splints can be used in phase I treatment, which is a reversible procedure before more permanent treatment is done. Phase I treatment could also include other treatments such as trigger point injections, myofascial release, medications such as muscle relaxers, electric stimulation, or meditation. Additional treatment in phase II is sometimes necessary including orthodontics, restorative treatment, or orthognathic surgery by the dentist or surgeon to stabilize the occlusion in the new condylar position.22 Phase II treatments are more irreversible procedures.22
Outcomes measured included the Kinnie-Funt chief complaint visual index initially and then the follow-up Kinnie-Funt, numeric pain rating, MMO, and cervical range of motion. At 1 week after treatment, the patient reported less of all her symptoms except bruxism on the follow-up Kinnie-Funt (Fig 4). Her numeric pain rating was 1/10, and her MMO was 50 mm. After 3 weeks and the conclusion of chiropractic treatment, the patient reported no longer having any of her symptoms on the follow-up Kinnie-Funt (Fig 4) except for bruxism. Her numeric pain rating was 0/10, with an MMO of 49 mm. Her cervical lateral flexion was 45 bilateral. The patient followed up for final evaluation at 6 weeks after her initial visit for delivery of her permanent splint and reported no recurrence of TMD, headaches, and myalgia. There was no further follow-up. The patient gave consent to publish this case report.
Fig 4.
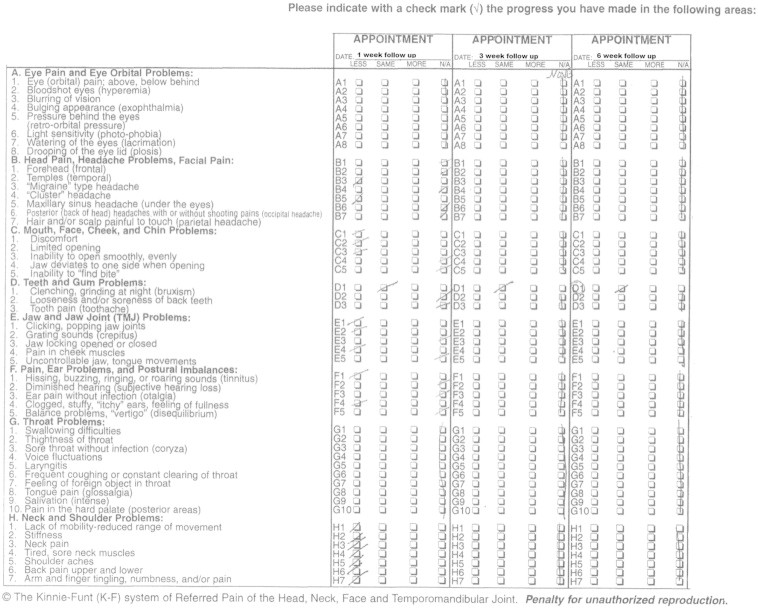
Follow up Kinnie-Funt visual index. (Kinnie-Funt index reproduced with permission of EOP Inc, Little Canada, MN)
Discussion
This case study is one of the first in the literature to describe collaborative approaches between dentists and doctors of chiropractic for the comanagement of TMD. The patient in this study responded well to the combined short course of care (6 treatments in 3 weeks) for TMD, headaches, and myalgia.
Research has shown central sensitization in some patients with TMD.8,23 This may explain the resolution of the patient’s numerous complaints in the head and neck region in addition to the TMD. The secondary referred pain from orofacial pathology and chronic painful stimuli in TMD alters the normal physiological processing in the brain and sensitizes the central nervous system.5 Another article discusses this central sensitization in patients with TMD, stating that they exhibit enhanced temporal summation to noxious stimuli and impaired central inhibitory mechanisms and this allows for enhanced sensitivity to pain at the TMD and sites distant from the head and neck region.8,23 Sensitization could be the mechanism by which widespread pain in TMD occurs.8,23 The trigeminal nerve gives the main afferent conduction in the pathophysiology and the transmission of headache in humans.5 This connection shows how patients with TMD can also have headaches and patients with headaches should also be screened for TMD. A study showed that when participants with cervicogenic headaches also received manual therapy for their TMD, they had significantly decreased headache intensities and increased neck function.9
In this case, the patient also had tinnitus, which was resolved with treatment. The tensor veli palatini and tensor tympani muscles are innervated by the medial pterygoid nerve, a branch of the mandibular nerve, which is a branch of the trigeminal nerve.5 This may be the connection showing why the patient’s tinnitus resolved with treatment and why many patients with TMD also complain of otic symptomology. This patient had multiple tender muscles and trigger points in her head, neck, and face with local and referred pain patterns. A study showed that the local and referred pain elicited from active trigger points in these regions shared similar pain patterns as spontaneous TMD, which supports the concept of peripheral and central sensitization mechanisms in myofascial TMD.24 This sensitization may be why the patient had so many tender points and why the otorhinolaryngologist gave a preliminary suggestion of fibromyalgia. Through the trigeminal nerve connections from the TMJ, cervical spine and ear can be made.
Patients with TMD can have numerous complaints, and their condition may become chronic. This is why we feel that a collaborative approach may be beneficial for the patient. Not only is holistically treating the stomatognathic system important, but it is important to address the associated complaints in the head and neck region to desensitize the nervous system by facilitating inhibitory pathways such as the descending inhibitory pathway after stimulation of areas such as the periaqueductal gray area through the propriospinal tract. These inhibitory pathways may be decreased in heightened central excitatory states in chronic pain conditions such as TMD.8 These patients can be helped by being evaluated by more than one practitioner because of the wide array of symptoms causing difficulty with the differential diagnosis.25 This may be why having more than one specialist treating a case with different viewpoints can potentially bring faster and more permanent resolution to a case.26 This is also why advanced training may be advantageous to these providers.26 We feel that this case report contributes to a better understanding of patients’ high use of CAM for TMD and the potential interaction of the cervical and masticatory muscles for these patients.
Limitations
One of the limitations of this case report is that we did not complete a long-term follow-up. Checking the patient’s Kinnie-Funt visual index at 6 months and 1 year after the end of treatment would have given more data on the long-term effects. There also were several methods and targeted tissues in the manual therapy, including adjustments, postisometric relaxation, and other myofascial release techniques. This makes it difficult to determine what was the effective treatment or if it was necessary to perform a combination of all therapies. Posttreatment diagnostics would have been beneficial to see the increase in translation of the TMJ, and a follow-up joint vibrational analysis could have shown a reduction or absence in the vibration on the left. There are different causes of TMD including but not limited to disk derangement, osteoarthritis, and myofascial pain sources. As this is just one case report, the effects of the comanagement should not be generalized to other patients with TMD. The patient may also have improved because of the normal course of the disorder. Further research and other case studies should be done with a specific category of TMD, like an articular disk displacement, and fewer manual therapies with the dental splint to isolate the better method.
Conclusion
This case report described how collaboration between a dentist and a doctor of chiropractic may help to provide quick resolution for patients with TMD, headaches, and myalgia. With 25% of the population having some form of TMD and taking into account the neurological and biomechanical connection to the cervical spine, dentists and chiropractors have the potential to help patients improve symptoms through comanagement.
Funding Sources and Potential Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Acknowledgment
This case report is submitted as partial fulfillment of the requirements for the Master of Science in Advanced Clinical Practice in the Lincoln College of Post-professional, Graduate, and Continuing Education at the National University of Health Sciences.
References
- 1.McNeely M., Olivo S., Magee D. A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys Ther. 2006;86(5):710–725. [PubMed] [Google Scholar]
- 2.DeBar L.L., Vuckovic N., Schneider J., Ritenbaugh C. Use of complementary and alternative medicine for temporomandibular disorders. J Orofac Pain. 2003;17(3):224–236. [PubMed] [Google Scholar]
- 3.Chinappi A.S., Getzoff H. Chiropractic/dental cotreatment of lumbosacral pain with temporomandibular joint involvement. J Manipulative Physiol Ther. 1996;19(9):607–612. [PubMed] [Google Scholar]
- 4.DeVocht J.W., Schaeffer W., Lawrence D.J. Chiropractic treatment of temporomandibular disorders using the activator adjusting instrument and protocol. Altern Ther Health Med. 2005;11(6):70–73. [PubMed] [Google Scholar]
- 5.Ramirez L.M., Sandoval G.P., Ballesteros L.E. Temporomandibular disorders: referred cranio-cervico-facial clinic. Med Oral Patol Cir Bucal. 2005;1(10):E18–E26. [PubMed] [Google Scholar]
- 6.Stedman’s concise medical dictionary. 4th ed. Lippincott, Williams & Wilkins; Baltimore, MD: 2001. [Google Scholar]
- 7.Fernandes G., Franco A.L., Siqueira J.T., Goncalves D.A., Camparis C.M. Sleep bruxism increases the risk for painful temporomandibular disorders, depression, and non-specific physical symptoms. J Oral Rehabil. 2012;39(7):538–544. doi: 10.1111/j.1365-2842.2012.02308.x. [DOI] [PubMed] [Google Scholar]
- 8.Sessle B.J. Peripheral and central mechanisms of orofacial inflammatory pain. Int Rev Neurobiol. 2011;97:179–2069. doi: 10.1016/B978-0-12-385198-7.00007-2. [DOI] [PubMed] [Google Scholar]
- 9.Von Piekartz H., Ludtke K. Effect of treatment of temporomandibular disorders in patients with cervicogenic headache: a single-blind, randomized controlled study. Cranio. 2011;29(1):43–56. doi: 10.1179/crn.2011.008. [DOI] [PubMed] [Google Scholar]
- 10.Bijur P.E., Latimer C.T., Gallagher E.J. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10(4):390–392. doi: 10.1111/j.1553-2712.2003.tb01355.x. [DOI] [PubMed] [Google Scholar]
- 11.Jensen M.P., Karoly P., Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- 12.Radke J., Garcia R., Jr., Ketcham R. Wavelet transforms of TM joint vibrations: a feature extraction tool for detecting reducing displaced disks. Cranio. 2001;19(2):84–90. doi: 10.1080/08869634.2001.11746156. [DOI] [PubMed] [Google Scholar]
- 13.Huang Z.S., Lin X.F., Li X.L. Characteristics of temporomandibular joint vibrations in anterior disk displacement with reduction in adults. Cranio. 2011;29(4):276–283. doi: 10.1179/crn.2011.041. [DOI] [PubMed] [Google Scholar]
- 14.Pringle R.K. Intra-instrument reliability of 4 goniometers. J Chiropr Med. 2003;2(3):91–95. doi: 10.1016/S0899-3467(07)60051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.George J.W., Fennema J., Maddox A., Nessler M., Skaggs C.D. The effect of cervical spine manual therapy on normal mouth opening in asymptomatic subjects. J Chiropr Med. 2007;6(4):141–145. doi: 10.1016/j.jcme.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chinappi A.S., Jr., Getzhoff H. The dental-chiropractic cotreatment of structural disorders of the jaw and temporomandibular joint dysfunction. J Manipulative Physiol Ther. 1995;18(7):476–481. [PubMed] [Google Scholar]
- 17.Skaggs C.D., Winchester B.A., Vianim M., Prather H. A manual therapy and exercise approach to meralgia paresthetica in pregnancy: a case report. J Chiropr Med. 2006;5(3):92–96. doi: 10.1016/S0899-3467(07)60140-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emary P. Use of post-isometric relaxation in the chiropractic management of a 55-year-old man with cervical radiculopathy. J Can Chiropr Assoc. 2012;56(1):9–17. [PMC free article] [PubMed] [Google Scholar]
- 19.Kalamir A., Polland H., Vitello A., Bonello R. Intra-oral myofascial therapy for chronic myogenous temporomandibular disorders: a randomized, controlled pilot study. J Man Manip Ther. 2010;18(3):139–146. doi: 10.1179/106698110X12640740712374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalamir A., Bonello R., Graham P., Vitiello A.L., Pollard H. Intraoral myofascial therapy for chronic myogenous temporomandibular disorder: a randomized controlled trial. J Manipulative Physiol Ther. 2012;35(1):26–37. doi: 10.1016/j.jmpt.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 21.Madani A., Mirmortazami A. Comparison of three treatment options for painful temporomandibular joint clicking. J Oral Science. 2011;53(3):349–354. doi: 10.2334/josnusd.53.349. [DOI] [PubMed] [Google Scholar]
- 22.Brenkert D.R. Orthodontic treatment for the temporomandibular joint patient following splint therapy to stabilize a displaced disk(s): a systemized approach. Part II. Cranio. 2010;28(4):260–265. [PubMed] [Google Scholar]
- 23.Kindler L., Bennetti R., Jones K. Central sensitivity syndromes: mounting pathophysiologic evidence to link fibromyalgia with other common chronic pain disorders. Pain Manag Nurs. 2011;12(1):15–24. doi: 10.1016/j.pmn.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fernandez-de-las-penas C., Galen-del-rio F., Alonso-blanco C., Jimenez-garcia R., Arendt-nielsen L., Svensson P. Referred pain from muscle trigger points in the masticatory and neck-shoulder musculature in women with temporomandibular disorders. J Pain. 2010;11(12):1295–1304. doi: 10.1016/j.jpain.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Nobrega J., Siqueira S., Siqueira J., Teixeira M. Differential diagnosis in atypical facial pain: a clinical study. Arq Neuropsiquiatr. 2007;65(2A):256–261. doi: 10.1590/s0004-282x2007000200013. [DOI] [PubMed] [Google Scholar]
- 26.Riva J., Muller G., Hornich A., Mior S., Gupta A., Burnie S. Chiropractors and collaborative care: an overview illustrated with a case report. J Can Chiropr Assoc. 2010;54(3):147–154. [PMC free article] [PubMed] [Google Scholar]


