Abstract
Objective
The purpose of this report is to describe a case of an aneurysmal bone cyst presenting as a pathologic fracture in a young athlete.
Case report
A 12-year-old patient presented to a chiropractic teaching clinic with a 1-week history of posterior neck pain and stiffness following a helmet-to-helmet collision in football practice. Cervical spine radiographs were taken. Lateral view radiograph demonstrated a pathologic fracture through a lytic, expansive lesion in the posterior arch of C7 with mild subluxation of the C7/T1 apophyseal joints and angulation of the C7/T1 disk space. Based upon these findings, additional diagnostic imaging was ordered. Findings on advanced imaging studies included the following: On computed tomography, the C7 lesion showed medullary destruction, cortical thinning and expansion, and a horizontally oriented fracture through the spinous and lamina. Magnetic resonance imaging studies for sagittal T2 and contrast-enhanced T1-weighted magnetic resonance images revealed fluid/fluid levels in the C7 spinous and peripheral enhancement with contrast.
Outcome
The patient was referred to a local hospital for treatment. The lesion was treated with resection of the posterior arch, and an aneurysmal bone cyst was confirmed histologically. The patient developed a kyphotic deformity at the site of resection and cervical instability. A subsequent fusion was performed.
Conclusion
Aneurysmal bone cysts are rare lesions. In this case, the initial traumatic history masked the underlying pathology. Although rare, pathologic fracture should be considered in cases of vertebral fracture in young patients.
Key indexing terms: Bone cysts, Aneurysmal, Pathologic fracture, Cervical vertebrae
Introduction
Aneurysmal bone cysts (ABCs) are rare lesions that represent 1.4% to 2.3% of all primary bone tumors.1 They may occur in any bone, but most often occur in the spine and large trabecular bones. Spinal involvement occurs in 12% to 30% of all ABC cases.2 Seventy percent of spinal ABCs occur in the region of the thoracolumbar junction. The cervical spine, as seen in this case, is involved less than 25% of the time.3 The most common cervical vertebra involved is C2 (26%), followed by C5 (17%).4 There is a predilection for involvement of the posterior elements, although extension into the vertebral body through the pedicles may occur.1 Eighty percent of ABCs occur in the first 2 decades of life. The pathogenesis of ABCs is unclear.5 They may occur as a solitary lesion or secondarily to other lesions, most commonly giant cell tumors (19%-39%).1 Other secondary lesions that may be associated with ABCs include osteoblastomas, angiomas, chondroblastomas, or malignant lesions such as telangiectatic osteosarcoma.1,3,6 Aneurysmal bone cysts characteristically have cystic spaces filled with blood, spindle cell stroma, and multinucleated giant cells on histology.1 Symptoms associated with ABCs are variable and depend on location and size of the lesion, although local pain is often the chief complaint.7 The average duration of symptoms is 6 months prior to diagnosis, and neurologic deficits at presentation are seen in 50% of patients.4
The differential diagnosis of posterior arch lesions in pediatric patients includes primarily benign lesions including ABCs, osteoblastomas, osteiod osteomas, and osteochondromas.1 Of these, osteoblastomas and ABCs can present as lytic, expansive lesions in the posterior arch.8 Malignant lesions that may present in the posterior arch include chondrosarcomas, osteosarcomas, and Ewing sarcomas.1 Imaging features of malignant lesions and those of aggressive benign lesions may overlap. Such features include ill-defined margins, lytic bone destruction, and a soft tissue mass, all of which may be seen with ABCs.1
The purpose of this paper is to report a case of an ABC presenting as an acute, pathologic spinous process fracture; to report the treatment rendered; and to discuss the subsequent complications resulting from treatment.
Case Report
A 12-year-old, previously healthy boy presented to a chiropractic teaching clinic with a 1-week history of posterior neck pain and stiffness following a helmet-to-helmet collision in American football practice. The pain was localized to the posterior cervical spine, without radiation. No substantial pain relief was achieved with over-the-counter analgesics. The patient reported feeling a “pop” and severe localized pain while trying to remove a shirt on the day of presentation.
Physical examination revealed marked tenderness at the cervicothoracic junction, without a palpable mass. Active ranges of motion were severely limited because of pain. Marked spasticity of the cervical and upper trapezius musculature was present. There were no neural deficits. Cervical fracture or instability was considered. Physical examination was terminated, and cervical spine radiography was obtained.
Cervical radiography (consisting of anteroposterior lower cervical, anteroposterior open mouth, neutral lateral, and oblique projections) revealed a pathologic fracture extending through a lytic, expansile lesion in the posterior arch of C7 (Fig 1). The lesion displayed a short zone of transition without sclerotic margins. The spinolaminar line was obliterated. Mild subluxation of the C7/T1 apophyseal joints and angulation of the C7/T1 disk space were present, suggesting cervical instability. The most likely differential diagnostic considerations based on the radiographic findings included ABC; osteoblastoma; and, less likely, eosinophilic granuloma. Advanced imaging was recommended for further evaluation of the lytic lesion and also the extent of the cervical fracture and suggested ligamentous injury.
Fig 1.
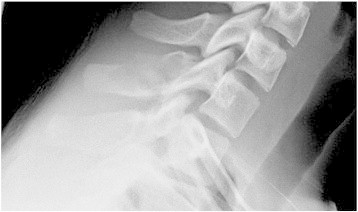
Spot lateral view of the cervical spine demonstrated a pathologic fracture through a lytic, expansive lesion in the posterior arch of C7 with mild subluxation of the C7/T1 apophyseal joints and angulation of the C7/T1 disk space.
The patient was referred for computed tomography (CT) and magnetic resonance (MR) examination of the cervical spine at an outside institution. Computed tomography revealed an expansile lesion with cortical thinning and a horizontally oriented, minimally displaced fracture of the posterior arch of C7 (Fig 2). The anterior margin of the C7 lamina was obliterated, although no definitive cord compression was appreciated. MR imaging revealed a T2-weighted hyperintense lesion demonstrating fluid/fluid levels within the C7 spinous process and laminae (Fig 3). The lesion was minimally displacing the posterior thecal sac without visualized infiltration. The pathologic fracture was better demonstrated on the CT images. There was no evidence of ligamentous injury involving the apophyseal joints on MR imaging.
Fig 2.
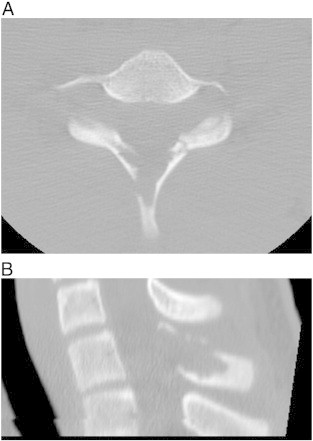
Axial (A) and sagittal (B) CT images through the C7 lesion revealed medullary destruction, cortical thinning and expansion, and a horizontally oriented fracture through the spinous and lamina.
Fig 3.

Sagittal T2- (A) and contrast-enhanced T1-weighted MR images (B) revealed fluid/fluid levels in the C7 spinous and peripheral enhancement with contrast administration. The posterior thecal sac is effaced.
The lesion was determined to most likely be of a benign etiology. Fluid/fluid levels are characteristic of an ABC, although not pathognomonic. The possibility of ABCs occurring in addition to other lesions as discussed previously complicates the differential diagnostic considerations. Differential considerations such as osteoblastomas or eosinophilic granuloma could not be excluded on the basis of imaging.
Neurosurgical consultation was obtained at a local hospital, and the lesion was treated with biopsy resection of the C7 spinous process and debridement of the tumor. The lesion was histopathologically described as a spindle cell lesion with moderate numbers of multinucleated giant cells. Centrally, there were irregularly sized cystic spaces filled with abundant red blood cells, consistent with an ABC. Following resection, the patient was discharged to home care. A hard cervical collar was recommended for use for 12 weeks postoperatively.
Follow-up cervical radiography at 12 weeks revealed a marked focal kyphosis at C7/T1 with anterolisthesis of C7 on T1. A 25° angulation at the C7/T1 disk space was present along with subluxation of the apophyseal joints (Fig 4). No tumor recurrence was suggested.
Fig 4.

A postoperative neutral lateral cervical spine radiograph demonstrated marked kyphosis at C7/T1 with subluxation of the apophyseal joints.
In light of the acquired cervicothoracic instability, neurosurgical consultation was again obtained at the hospital. The patient underwent posterior lateral mass and pedicle screw-rod fixation spanning from C5 to T2, which reduced the cervical kyphosis and returned the C7/T1 disk space and apophyseal joints to normal alignment. Straightening of the sagittal cervical curve and anterior shift of the cervical gravity line remained (Fig 5). The patient was otherwise free of disease or surgical complications.
Fig 5.
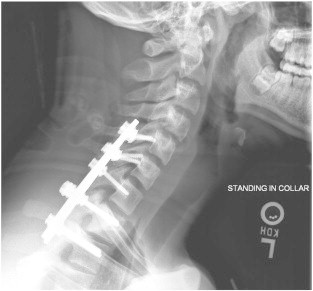
A postoperative radiograph revealed instrumentation spanning from C5 to T2. The previous kyphosis at C7/T1 was stabilized, resulting in normal anatomical alignment.
Discussion
This case report illustrates an abnormal presentation of this rare lesion. In addition, the clinical presentation of fracture masked the underlying pathology prior to cervical radiography.
The most often reported presentations of ABCs of the spine are slow, insidious onset of pain and neurologic compromise.1,4,6,9–12 Most reported cases of pathologic fracture associated with ABCs were the result of vertebra plana rather than posterior arch fracture.9,13,14 In the presented case, the patient reported no previous neck pain prior to the collision. The high-impact trauma may have been sufficient to produce a spinous process fracture, as was suspected clinically. The underlying posterior arch lesion was clinically undetectable and presented purely as an incidental finding. Outside of the setting of major trauma, spinal fracture in the pediatric population should raise the suspicion of pathologic fracture.
Surgical management consisting of complete resection or intralesional resection with curettage offers the best ABC treatment outcomes with no recurrence reported in a review by Harrop et al. Recurrence rates as high as 25% are reported with incomplete excision.13 In a review of 19 cervical spine ABC cases from 4 different institutions, 18 patients underwent an instrumented or bone graft fusion at the time of initial lesion resection.4,9,15,16
The most common postsurgical deformity associated with laminectomy in the cervical spine is kyphosis.3,17 With 64% of cervical weight bearing being provided by the posterior elements, resection can lead to an anterior shift in weight bearing and subsequent progressive kyphosis. More extensive resection of the lamina and disruption of the apophyseal joint capsule increase the risk of acquired kyphosis.8 Pediatric patients are more prone to kyphosis because of a greater degree of laxity in the cervical ligamentous structures.17 In a case series by Mehlman et al, 45% of pediatric patients undergoing laminectomy developed spinal deformity, with 60% of those patients requiring subsequent spinal fusion.18 Serial radiography is recommended for those at risk for developing cervical kyphosis.8 The decision to forego fusion at the time of initial resection in this case is unclear.
Limitations
This case reports an uncommon presentation of a rare lesion. The presentation and associated treatment cannot be generalized to all patients. The surgical treatment and outcome are reported in this paper; however, direct information regarding the surgical decision making in this case was unavailable.
Conclusion
In the case presented, the initial traumatic history clinically masked the underlying pathology. Radiographic investigation detected the preexisting lesion and determined the appropriate workup and treatment. This case illustrates the need to consider occult pathology in a traumatic setting even in the pediatric population.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.Rodallec M.H., Feydy A., Larousserie F. Diagnostic imaging of solitary tumors of the spine: what to do and say. Radiographics. 2008;28(4):1019–1041. doi: 10.1148/rg.284075156. [DOI] [PubMed] [Google Scholar]
- 2.Lim J.B., Sharma H., Reid R., Reece A.T. Aneurysmal bone cysts of the vertebrae. J Orthop Surg (Hong Kong). 2012;20(2):201–204. doi: 10.1177/230949901202000213. [DOI] [PubMed] [Google Scholar]
- 3.Beiner J.M., Sastry A., Berchuck M. An aneurysmal bone cyst in the cervical spine of a 10-year-old girl: a case report. Spine (Phila Pa 1976) 2006;31(14):E475–E479. doi: 10.1097/01.brs.0000222126.91514.cb. [DOI] [PubMed] [Google Scholar]
- 4.Novais E.N., Rose P.S., Yaszemski M.J., Sim F.H. Aneurysmal bone cyst of the cervical spine in children. J Bone Joint Surg Am. 2011;93(16):1534–1543. doi: 10.2106/JBJS.J.01430. [DOI] [PubMed] [Google Scholar]
- 5.Hsu W., Kosztowski T.A., Zaidi H.A., Dorsi M., Gokaslan Z.L., Wolinsky J.P. Multidisciplinary management of primary tumors of the vertebral column. Curr Treat Options Oncol. 2009;10(1–2):107–125. doi: 10.1007/s11864-009-0102-8. [DOI] [PubMed] [Google Scholar]
- 6.Burch S., Hu S., Berven S. Aneurysmal bone cysts of the spine. Neurosurg Clin N Am. 2008;19(1):41–47. doi: 10.1016/j.nec.2007.09.005. [Review] [DOI] [PubMed] [Google Scholar]
- 7.Graham G.N., Browne H. Primary bony tumors of the pediatric spine. Yale J Biol Med. 2001;74(1):1–8. [Review] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramme A.J., Smucker J.D. Balancing spinal stability and future mobility in the cervical spine: surgical treatment of a case of osteoblastoma with secondary aneurysmal bone cyst. Spine J. 2011;11(5):e5–e12. doi: 10.1016/j.spinee.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 9.Zenonos G., Jamil O., Governale L.S., Jernigan S., Hedequist D., Proctor M.R. Surgical treatment for primary spinal aneurysmal bone cysts: experience from Children's Hospital Boston. J Neurosurg Pediatr. 2012;9(3):305–315. doi: 10.3171/2011.12.PEDS11253. [DOI] [PubMed] [Google Scholar]
- 10.Rajput D., Tungaria A., Jaiswal A., Jain V. Aneurysmal bone cyst of clivus and C1 C2: case report and review of literature. Turk Neurosurg. 2012;22(1):105–108. doi: 10.5137/1019-5149.JTN.3051-10.1. [DOI] [PubMed] [Google Scholar]
- 11.Papagelopoulos P.J., Currier B.L., Shaughnessy W.J. Aneurysmal bone cyst of the spine. Management and outcome. Spine (Phila Pa 1976) 1998;(5):621–628. doi: 10.1097/00007632-199803010-00018. [DOI] [PubMed] [Google Scholar]
- 12.Boriani S., De Iure F., Campanacci L. Aneurysmal bone cyst of the mobile spine: report on 41 cases. Spine (Phila Pa 1976) 2001;26(1):27–35. doi: 10.1097/00007632-200101010-00007. [DOI] [PubMed] [Google Scholar]
- 13.Harrop J.S., Schmidt M.H., Boriani S., Shaffrey C.I. Aggressive "benign" primary spine neoplasms: osteoblastoma, aneurysmal bone cyst, and giant cell tumor. Spine (Phila Pa 1976) 2009;34(22 Suppl):S39–S47. doi: 10.1097/BRS.0b013e3181ba0024. [DOI] [PubMed] [Google Scholar]
- 14.de Kleuver M., van der Heul R.O., Veraart B.E. Aneurysmal bone cyst of the spine: 31 cases and the importance of the surgical approach. J Pediatr Orthop B. 1998;7(4):286–292. doi: 10.1097/01202412-199810000-00006. [Review] [DOI] [PubMed] [Google Scholar]
- 15.Zileli M., Isik H.S., Ogut F.E., Is M., Cagli S., Calli C. Aneurysmal bone cysts of the spine. Eur Spine J. 2013;22(3):593–601. doi: 10.1007/s00586-012-2510-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mesfin A., McCarthy E.F., Kebaish K.M. Surgical treatment of aneurysmal bone cysts of the spine. Iowa Orthop J. 2012;32:40–45. [PMC free article] [PubMed] [Google Scholar]
- 17.Han K., Lu C., Li J. Surgical treatment of cervical kyphosis. Eur Spine J. 2011;20(4):523–536. doi: 10.1007/s00586-010-1602-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehlman C.T., Crawford A.H., McMath J.A. Pediatric vertebral and spinal cord tumors: a retrospective study of musculoskeletal aspects of presentation, treatment, and complications. Orthopedics. 1999;22(1):49–55. doi: 10.3928/0147-7447-19990101-07. [discussion 55–6] [DOI] [PubMed] [Google Scholar]


