Abstract
Background: Using a modern scientific basis, this article examines clinical findings and experimentally reproducible data that demonstrate reliably the objective reality of the auriculotherapy procedures initiated by Paul Nogier, MD, of Lyon, France.
Objective: The aims of this review are to: (1) identify the Chinese acupoints and all relevant related subjects; (2) offer a critical analysis of different auricle cartographies or ear maps; and (3) evaluate evidence for auriculotherapy with respect to the constant progress of our knowledge of nervous-system organization.
Discussion: Acupuncture points have lower electrical impedance than nonacupoints. This was demonstrated by Niboyet and Terral, utilizing a sinusoidal current with the technical arrangements of different equivalent circuits made at Unit 103 of the French National Institute of Health and Medical Research (INSERM), Montpellier, France. This work demonstrated that physical behavior associated with acupuncture corresponds to a specific histologic structure located within the dermis termed the neurovascular complex (NVC). The concept of using sham points for testing acupuncture needs to be criticized. A reproducible experimental model of analgesia has been produced using the hind limb of a rabbit; this model is a proven demonstration of the positive action of acupuncture on pain. Acupuncture analgesia is a technique that has been used effectively by Chinese researchers in the 1970s for surgical applications. The different ear maps may have to be significantly modified because of the paucity of scientific validation of most of the localizations of organs or functions and, particularly, of nervous structures. Increased knowledge about complex nervous interactions should facilitate formulation of some scientifically acceptable hypothesis to explain the action of auriculotherapy.
Conclusions: More scientific research should be performed to improve the scientific credibility of auriculotherapy.
Key Words: : Auriculotherapy, Acupoint Histology, Neurovascular Complex, Analgesia, Auricle Cartography, Central Nervous System
Introduction
Adiscussion about the scientific basis for a medical procedure implies that one must first define precisely what the necessary scientific objectives are. Any phenomenon could be considered a scientific fact, if that phenomenon is observed and measured in the best possible technical manner by an observer and if the results are reproducible by other scientists. To explain a scientific medical phenomenon, an hypothesis can be formulated and may become a law or a dogma, if it has been proved objectively according to the general principles of evidence-based medicine. With respect to a clinical practice, it is mandatory to collect a sufficient number of clinical observations and to achieve a careful analysis of clinical results on a statistically valid number of patients in order to allow that practice to be credible for the medical community. Generally speaking, there is one single “truth” despite different methodologies of investigation.*
Historically, the ear pavilion was cauterized to treat sciatica or toothache. These techniques were reported in 1850 by Lucciana in Corsica, France; and almost simultaneously by Joseph François Malgaigne, MD, in Paris, France; and Giambattista Borelli, MD, in Turin, Italy. However, because of a lack of objective mechanistic explanations, this technique was never utilized again until 1950, when some nonbiomedical healers from South-Eastern France were treating sciatic pain by cauterization of the ear antihelix. That technique was observed by the French physician Paul Nogier, MD,1 of Lyon, France, who started a long series of clinical investigations and observations that led to his 6 years of research development in Marseille, France, supported by Jaques Niboyet, PhD, from Marseilles. In 1957, Nogier published in the German Magazine for Acupuncture [Deutsche Zeitshrift für Akupunktur] his first map defining a somatotopic arrangement on the auricle with a drawing made by Gerhard Bachmann.2 The publication of Nogier's auricular map led to the very widespread and rapid diffusion of the original Nogier concept in Russia, Japan, and China. Anatomically, a primary distinction of the ear pavilion is its composition of thin skin that is firmly attached to fibrous cartilages fixed around the external auditory meatus and that gives the ear pavilion its typical shape. It has a very rich innervation and blood supply. Embryologically, the auricle is only derived from the ectoderm and mesoderm. The four mixed cranial nerves (motor and sensitive roots with ganglions) controlling the four visceral arches give the ear more than half of its innervation by the trigeminal (V), facial (VII), glossopharyngeal (IX), and vagal nerves (X), and also the cervical plexus (C2/C3). This composition of nerves allows one to consider this organ as a specific neurovascular organ.
With respect to the scientific basis of auriculotherapy, it is necessary to discuss three different aspects: (1) the acupoint identification; (2) the maps or cartographies of the ear pavilion; and (3) the central nervous system (CNS) connections and interactions.
Identification of Acupoints
Undoubtedly the most difficult aspect that needs to be discussed in detail is the evolution of the life sciences. Therefore, it necessary to consider Traditional Chinese Medicine (TCM) with its longstanding traditions of use and modern improvements of Occidental medicine because of important basic and technical progress in that system of knowledge.
According to the historical work done by Huard and Wong,3 the first written document about Chinese acupuncture is the Nei-Jing (The Inner Canon of Huangdi or Yellow Emperor's Inner Canon), probably produced during 3 bce and permanently enriched by new contributions. In 1934, Soulié de Morant, during a diplomatic mission in China, was able to learn the local language and to practice the Chinese acupuncture that he subsequently introduced in France. He published an adequate French translation of the Nei-Jing. It is amazing to know that the 14 meridians (meridian=Jing) defined in TCM as a series of distinct points along these meridian lines were unchanged until the present time.4 Their names were designated for a long time prior to a comprehensive dissection of a human body, explaining the debatable correspondence to the chosen organs: Heart, Kidneys, Gall Bladder, Liver, Spleen, Stomach, etc. In addition, they adopted the concept of “energy”—or more precisely, life force—(Qi) to try to explain all observations by describing the alleged permanent circulation of the Qi within the body in two different forms: “Yin and Yang.” The classical symbol representing them is a broad interpenetration of the two opposite forms in a complex interaction. The Qi uses the meridians to circulate, with many variations in relation to individuals, day and night, seasons, etc., and also with some specific interrelations between meridians. A specific immutable terminology exists in TCM; this terminology is not in present biomedical academic language. This situation does not make it easy to communicate across Oriental and Occidental medicines. At the present time, increasing cultural and economic exchanges are occurring between China and almost all parts of the world, which explains why teaching programs of TCM are introduced more frequently in different European countries.
In addition, it is important to realize how Occidental medicine has changed profoundly, according to the incredible progress made in all domains of science during the last 2 centuries, leading to numerous scientific discoveries. Life sciences are so advanced that no single scientist is able to have an holistic perception of biology, physiology, genetics, biochemistry, immunology, pathology, etc. The real revolution of imaging technology enables researchers to visualize, statically and dynamically, all the organs and functions in the human body by using X-rays, image scanners, magnetic resonance imaging (MRI), positron emission tomography, and tractography. It is now possible, for $1,000, to acquire information about one's own genome, opening the promising field of predictive medicine for treating a person instead of treating a disease. In this context, it seems appropriate to require precise criteria to define the scientific basis of any clinical practice,such as acupuncture—which is now divided in two parts: somatic and auricular. The first question to ask,while using the resources of modern technology, is: “What are the exact natures of the Chinese points and the meridians?” Several different answers have been provided and should be discussed. These are outlined in the sections below.
Studies on the Physical Reality of the Acupoint
In 1963, Niboyet presented two PhD theses on the measurement of the electrical resistance of the skin with direct current and particularly on the Chinese points.5,6 He methodically designed different special measurement devices and different types of single and multiple electrodes. He demonstrated that the acupoint has a lower electrical skin resistance that still can be detected after cleaning the skin and also on cadaver skin.7 That obviously eliminated the possible influence of sebum or sweat-gland secretions as indicated in some critiques.
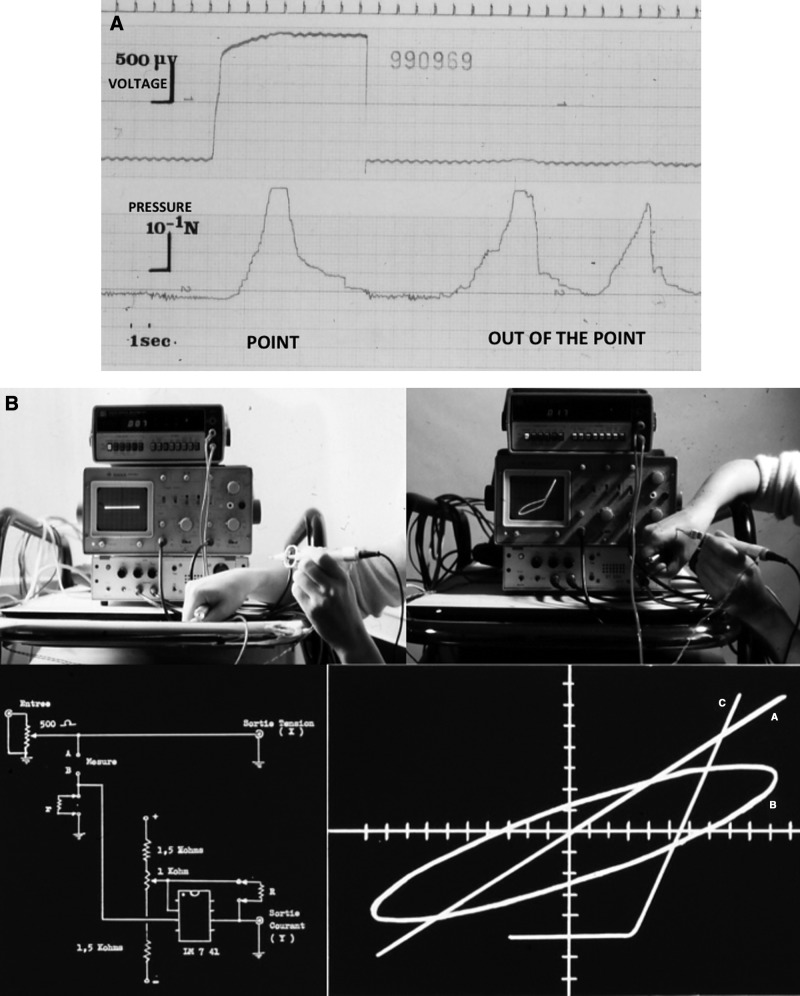
These basic experiments were reproduced in the research Unit 103, of the French National Institute of Health and Medical Research (INSERM) in Montpellier, France, by Claudie Terral, MD, PhD,8—and together with Rabischong,9—who used direct as well as sinusoidal currents on rabbits, human skin of the body and the ear pavilion (Fig.1 A and B). Different profile curves were defined by studying the output intensity on the Y axis and the output sinusoidal voltage applied on the X axis of a curve plotter corresponding to the formula: I=f(V). In this graphical representation, intensity is a function of voltage in Cartesian coordinates (not shown in Fig. 1). With a magnesium electrode, it was possible to describe a typical equivalent circuit of diode type, with a preferred selection of positive or negative current according to the polarity of the measuring electrode in contact with the specific points. Three curve profiles are normal: the (1) diode; (2) thyristor; and (3) ellipsis models. Those specific points have to be considered as active points with stable electrical signals. They can be surrounded by emerging signals that are stable or unstable, which represent some “satellite points” with a charge intensity in the order of 5–10 milliamps (mA). Eventually, some inactive high-impedance points without detectable flows can be located on the borders of the satellite points.
FIG. 1.
Electrical detection of acupoints. (A) Punctiform detector equipped with strain gauges to measure the pressure on the skin (inferior line), showing, on the left, detection of the point with a current (superior line) and, on the right, out of the point. (B) Use of the curve plotter (C. Klein, PhD thesis. Montpellier, France: Faculty of Sciences, 1976) for sinusoidal current detection with typical signals: A. resistance; B.diode; and C. capacitor. Used with permission.
These changes in the electric field are caused by diffusion or migration of accumulated charges during the mandatory injection of a current for impedance measurement. This concept of satellite points may explain later some possible action of sham points. There is typically an emission at the level of the point. Therefore, the point becomes a current generator, which can be as strong as 200 mA, possibly increasing the field of satellite points.
Histologic Reality
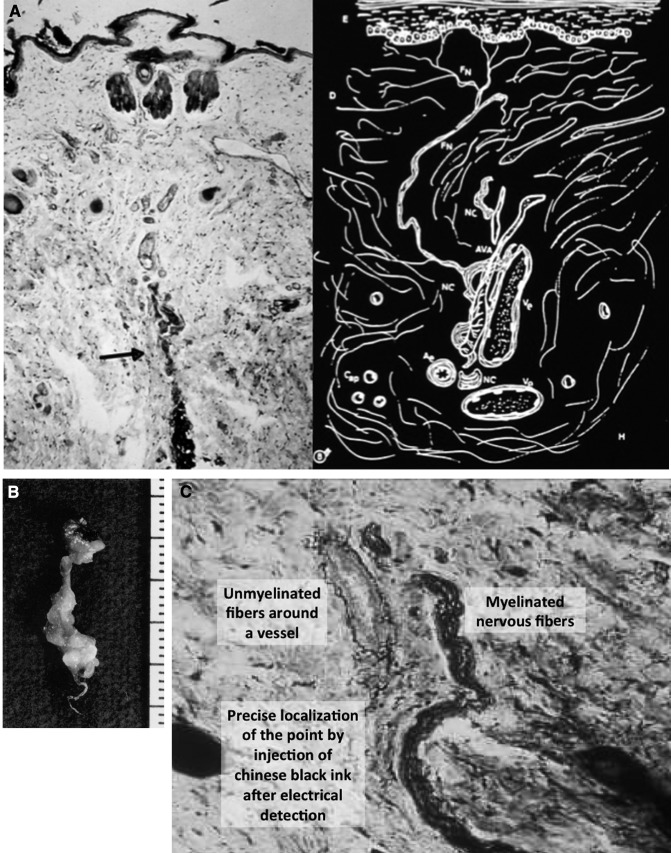
This particular electrical behavior of the point suggested the existence within the skin of a specific structure explaining the point's low electrical resistance. Two histologic studies of acupoints were made by Kim10 from North Korea in 1964 and by Kellner11 from Vienna in 1966, but without acceptable results because of an imprecise localization of the acupoint. At the INSERM Unit 103, Terral and Rabischong,12 Terral,13 and Auziech,14 from René Senelar, MD, PhD's15 histology laboratory, performed rigorous histologic investigations by marking, with black Chinese ink, the Chinese points that had been detected electrically and making serial sections with the classic colorations and impregnations used in histology laboratories. This was performed in different body parts of rabbits, including the pinna. Some biopsies were also made on the leg of a human volunteer and from material obtained from fresh human cadavers. The results of these studies confirmed the existence within the dermis of some specific histologic structures explaining the electrical data (Fig. 2A–D).
FIG. 2.
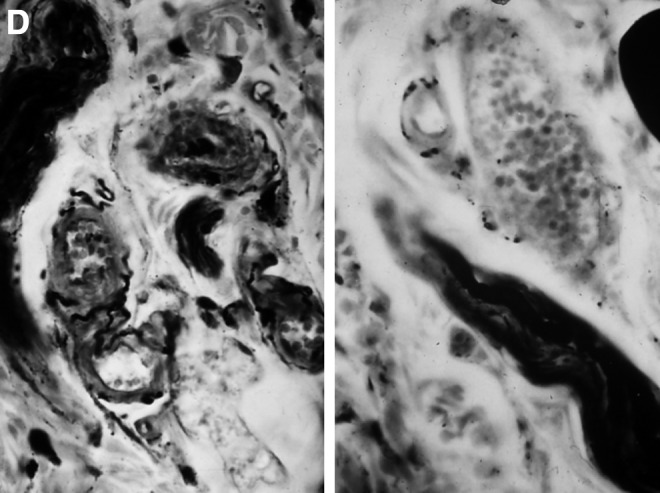
Histologic study of the acupoint. (A) Histologic section of rabbit skin on a detected point showing the neurovascular complex (NVC) with a drawn representation. (B) Sampling of a neurovascular bundle excised from the leg of a human volunteer with the complete NVC. (C) View of the myelinated and unmyelinated fibers around a vessel within the NVC. Left: black Chinese ink injected to localize the acupoint. (D) After argentic impregnation, on the left, unmyelinated nervous fibers within the wall of the artery of the NVC, and on the right, myelinated nervous fibers between vessels.
The connective tissue of the ear is modified and less dense,causing some small skin depression at certain acupoints. However, the main structure is termed the neurovascular complex (NVC), which is formed by a combination of myelinated and unmyelinated nervous fibers and small arterial and venous capillaries, plus a small lymphatic vessel. This structure has some similarity with the glomus system existing within the skin. A linear array of cholinergic fibers “creeps” into the intima and media of arterial vessels walls. Some adrenergic nerve fibers are visible in the basal lamina of the epidermis, but nothing is noted around the lymphatic small vessels. Many cells of the immune line—such as neutrophils, lymphocytes, Langerhans mast cells, and dendritic cells—can be isolated among reticuline and collagen fibers with fixed fibroblasts and fibrocytes. This observation was confirmed by an electron microscopic study done by Auziech on rabbit samples,14 which also showed osmiophilic cells around the capillary walls as well as chromatophine cells of the amine-precursor uptake and decarboxylation(APUD)–type, which are always visible in the study of acupoints that are electrically stimulated before ultramicroscopic observation. The role of mechanoreceptors also needs to be mentioned as potential modifiers of the recorded signals observed by Terral in patients with spinal-cord injuries (unpublished research).
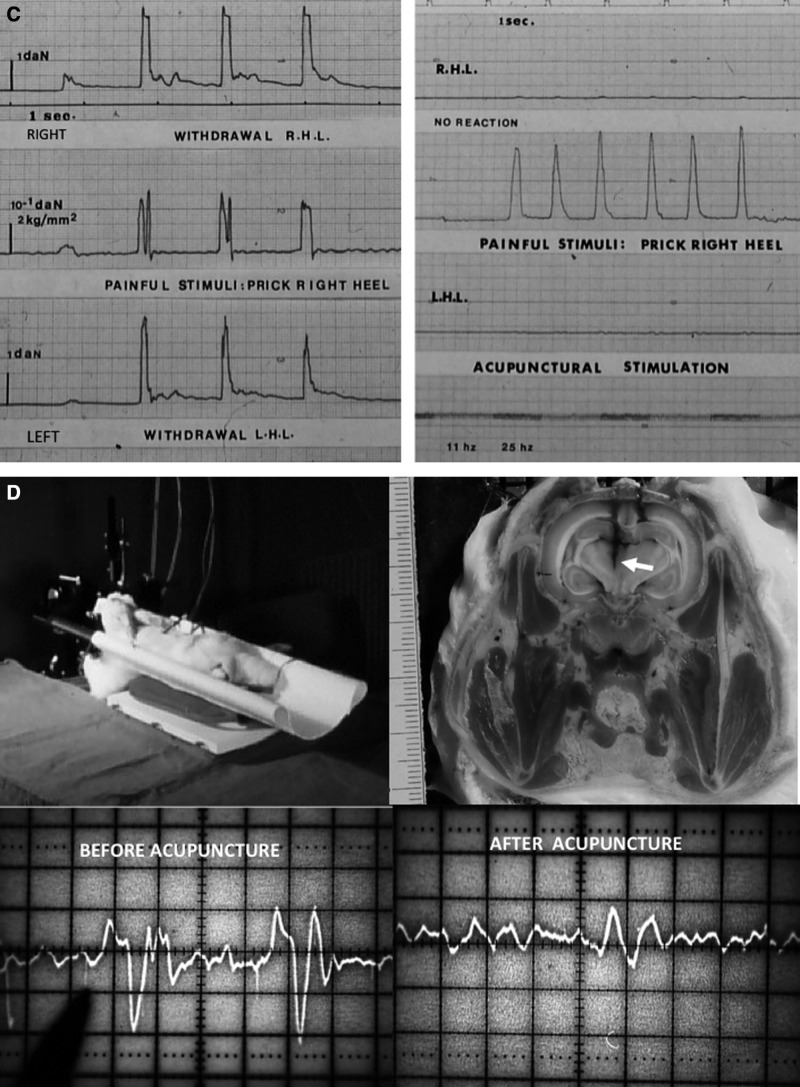
At the level of the ear pavilion, unmyelinated cholinergic fibers were found in the concha in relation to the parasympathetic nervous system. Three types of NVC were described in three identified zones: (1) the horizontal-type NVC (80/75/60 μ) with an arteriovenous capillary anastomosis in the soft connective tissue of the curve of the helix; (2) an NVC of a ball-shaped compact structure; (3) an NVC in the concha and ear lobe, of a vertical type, with no fine mesh on unmyelinated adrenergic fibers surrounding the vascular loop, which represents a different aspect than somatic acupoints (Fig. 3A and B). In fact, many of the differences existing between somatic and auricular points are caused mainly by the structure of the skin, which is very thin in the ear pavilion and thick within the body, with fat lobules in the dermis and many sensory corpuscles.
FIG. 3.
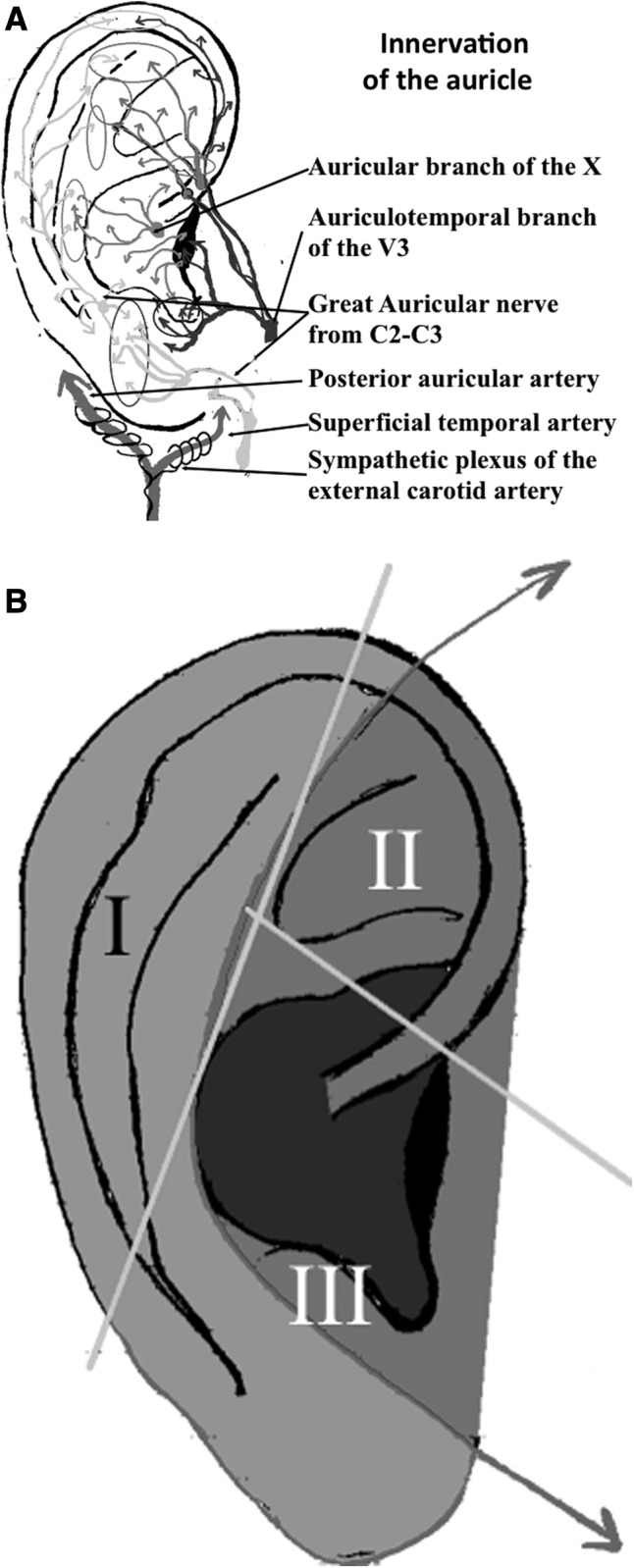
(A) Drawing of the innervation of the auricle with the different branches from V3,auricular branch of X, and cervical plexus C2–C3. (B) The three sectors of the neurovascular complex (NVC) of the auricle (Auziech O. MD thesis, Montpellier, France: University of Montpellier, 1984) corresponding to the three types of NVC: I. horizontal type; II. compact type; and III. vertical type. Used with permission.
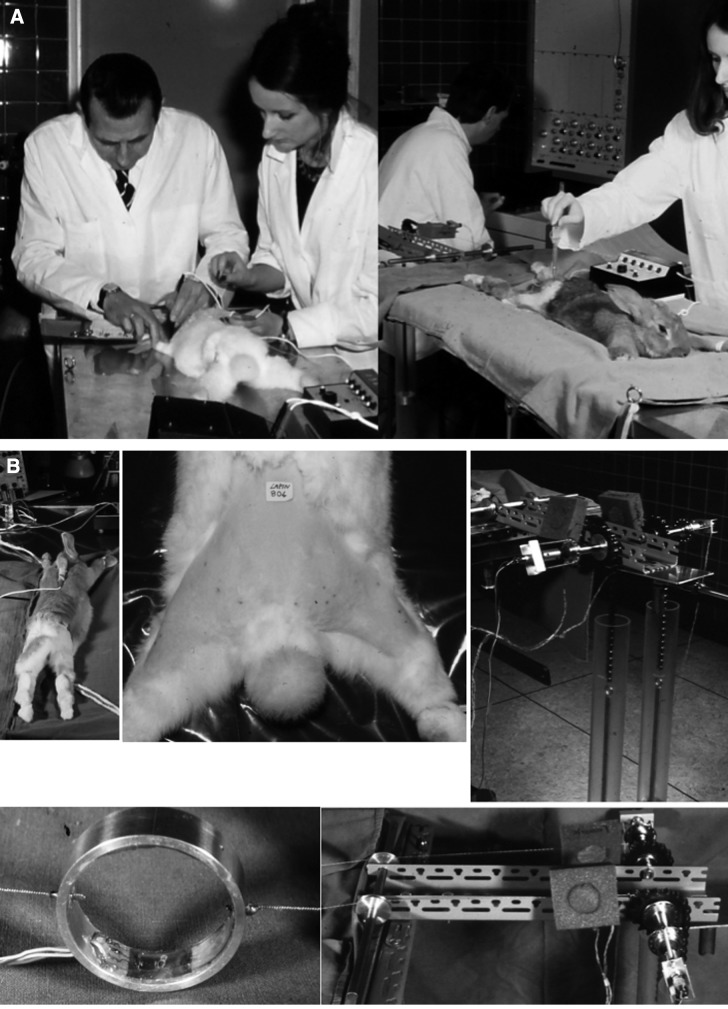
Skin Analgesia
A reproducible experimental model of analgesia induced by acupuncture was achieved on rabbits examined at the INSERM Unit 103.16 The choice of this animal was made according to its type of symmetrical locomotion by simultaneous activation of the two hind limbs for propulsion. Two needles were introduced within two detected acupoints on one side of the animal (BL 49 and ST 36) and analgesia of the limb on that side was observed clearly. To demonstrate the presence or absence of analgesia, a painful puncture of the skin was done to generate a withdrawal reflex on both hind limbs of the rabbit. If this was done on the intact side there was a withdrawal reflex, but nothing occurred if the inserted needles were on the side that had analgesia. In fact, it was not a paralysis, but a true analgesia. All parameters were recorded with appropriate equipment, particularly with strain-gauge transducers. Electrodes were also implanted in the rabbit's brain within the nucleus parafascicularis of the thalamus. The pain signal during painful stimulation was identified, and suppression of the pain signal after acupuncture activation was clearly visible. Placing the needle outside the acupoint made it impossible to achieve the inhibition of the thalamic pain signal (Fig. 4).
FIG. 4.
Experimental model of analgesia on hind limbs of rabbit. (A) Insertion of acupuncture needles by Niboyet and Terral in two acupoints. (B) Measurement of the withdrawal reactions (reflex forces) with strain-gauge transducers. (C) Record of forces after painful puncture of skin with a detector equipped with strain gauges (middle line): on the left, before, and on the right, after 20 minutes of electrical stimulation of the two acupoints of the right hind limb (there were no more withdrawal reactions). (D) Implantation of a microelectrode into the nucleus parafascicularis of the thalamus of a rabbit with its head in a stereotactic frame. Bottom left shows pain signal recorded by the thalamic electrode during painful stimulation, and bottom right shows inhibition of pain signal after acupuncture stimulation.
In addition, injection into a “naïve” intact living animal of the serum from a rabbit with acupuncture analgesia was transferable and produced an analgesia in the same corresponding anatomical area. This finding strongly supports the hypothesis of a neurosecretion of a neurotransmitter and the possibility of an enkephalin having a metameric action. The validation of this hypothesis is still in progress. In 1970, the Chinese used acupuncture analgesia effectively, first for odontology, and then for different surgical specialties, putting needles also on the ear pavilion. An elderly patient was operated for an inguinal hernia only with this analgesic technique in a well-known hospital in Paris.16,17 Niboyet reported many surgical cases seen in hospitals in China and in different veterinary schools. However, this technique requires presurgical training for patients and a longer induction time than the chemical techniques commonly used by modern anesthetists. Although not currently used in China for most surgeries, the previous Chinese discoveries demonstrated the real efficacy of somatic and auricular acupuncture for pain control.
Sham Acupuncture
This approach was introduced in 199318 and should be considered as use of a placebo to study the real efficacy of acupuncture. Sham acupuncture consists of inserting needles in incorrect points or nonacupoints. According to one Swedish sham protocol, researchers eventually used needles that retracted into their handles after contact with the skin.19,20 Many clinical trials have been conducted in different countries, organizing the trials in three distinct groups: (1) verum acupuncture; (2) sham acupuncture; and (3) a control condition. For example, Moffet, in a review21 of 229 articles on acupuncture published in English, isolated 38 acupuncture trials. Most studies (58%) found no significant differences in outcomes and 13 of 22 studies reported that sham acupuncture was as efficacious as verum acupuncture, particularly when applied to nonacupoints. The ideal double-blinding was impossible in this case, but the basic condition was for the patients to be blinded to their random group assignments. The placebo effect is very well-known in biomedical science, with factors depending on patient belief, healer behavior, and treatment conditions. A United States National Institutes of Health (NIH) large consensus statement22 on acupuncture was published in November of 1997. It appears that researchers are using sham procedures as an objective assessment of traditional acupuncture practice.23 However, numerous researchers use sham placebo to alter the therapeutic validity of the acupuncture, and this work is discussed widely in the news media. This is occurring in a period of time when all the developed countries are complaining about the tremendous increase of health care costs with a large part of the problem being caused by the pharmaceutical corporations.
Few remarks can emerge after what was said about the acupoint. There are many more NVCs than those officially accepted as acupoints by the World Health Organization (WHO) or by national acupuncture organizations. It is estimated that, in China, more than 2000 new acupoints have been discovered and defined. That means that, when an observer uses a supposedly sham acupoint, believing that he or she is inserting a needle into a presumably nonacupoint, the researcher does not actually know if it is not a nonregistered acupoint or a satellite point, as indicated by Terral, which can also have some clinical efficacy. A practitioner Robert Chu, MD, from Pasadena, California, is practicing a Tung system of acupuncture with 740 points and tendinomuscular meridians that are different from the 14 officially accepted meridians in TCM. Therefore, TCM is not including all the existing acupoints, and that changes completely the scientific credibility of these trials with sham acupuncture—especially given that the researchers are not performing electrical detection of the points as needed for certainty. It is, in fact, desirable to abandon this noncoherent and nonscientifically acceptable method of research.
In addition, it is important to know that the meridians have no anatomical reality, even if many individuals have suggested, in print, that they can identify them by using radioactive tracers24 or by meridian optics.25–27 The meridians are virtual constructions invented by the old Chinese and are similar to the constellations we can observe in the sky by artificially joining stars without physical links and not located in the same plane.
In conclusion of this section, in the author's opinion, the reality of the somatic and auricular acupoints needs to be demonstrated to be recognized as an undisputable scientific fact that is easily reproducible by any objective observer. Acupoints are not motor points, which are located by penetration within the muscle of the motor nervous fibers. TCM does not cover all the biologic complexity of the very large biologic network within the human skin. It is nonetheless a place to begin, or to continue, more-serious scientific investigations about acupuncture.
Ear Pavilion Cartographies
Standardization of auricular acupuncture is not a trivial task, because it requires a consensus of many countries throughout the world. In fact, Nogier, after much research work, was able to publish his first auriculotherapy map in 1957, depicting a fetus with head down projected on the ear pavilion.28 His technique was rapidly and largely diffused to other countries, which led to a need for international terminology and standards, which was, fortunately, well-recognized by international bodies. Nomina Anatomica is the “bible” for all anatomists, describing in Latin all terms defining the different parts of body organs, agreed upon under the concurrence of an international group of experts.29 The revised versions of 1950 and 199829,30 are used by all medical books and include 30 terms for the different parts of the external ear: helix; antihelix; tragus; antitragus; scapha; fossa triangularis; lobule; concha; and tubercule of Darwin.
The contribution of WHO standardization was decisive, as was the crucial role for auricular acupuncture by Terry Oleson,31,32 which stimulated and initiated further positive debates.33 Many WHO working group meetings were organized: in 1982 in Manila, in 1985 in Hong Kong, in 1987 in Seoul, in 1989 in Geneva, and in 1990 in Lyon. Thirty-nine auricular points were adopted, but some discrepancies between China and Europe were resolved during a meeting in Beijing in 2010 (personal communication P. Rabischong).
Therefore the need for common terminology regarding ear-pavilion cartography corresponds to mandatory transcription of the data accumulated during patient clinical examinations. This should facilitate communication between practitioners and medical researchers publishing academic reviews or textbooks. At present, two different systems have emerged: (1) a linear grid system or (2) a circular grid pattern. In 2003 Oleson presented his cartography of the ear pavilion with zones adopted by Winfried Wojak, MD, PhD34: 7 zones on the lateral side and 3 on the medial side, with vertical and horizontal lines that identify a point by three numbers. A three-dimensional version of this cartography was shown in 2012 during the 7th International Symposium of Auriculotherapy in Lyon, France, June 8–9.31
One of the most practical circular grid representations was introduced by Marco Romoli35 and used a sectogram, which is very useful for collecting data, following the evolution of a patient's health progress, and performing statistical analysis of clinical cases. First presented in 1981, Romoli's grid starts at Nogier's point zero considered by Nogier as the geometrical center of the ear. Three semiaxes (I, II, and III) subdivide the auricle. Romoli evaluated the reliability of this sectogram when it was utilized by 385 physicians during seminars organized between 2004 and 2007. David Alimi MD,36 proposed a newer circular grid pattern called a segmentogram, starting from the middle part of the tragus with a first oblique line joining the anterior border of the helix and lobule and with letters and numbers for radial and circular lines. Approved in 2010 by the board of the World Federation of Chinese Medicine Societies (WFCMS), it would be useful to have a larger international evaluation and adoption. In any event, as revealed by the existence at least of three valid systems, it seems very difficult to achieve a consensus for a definite choice of a unique system.
The content of these charts will very critical when scientific validation of the final choice is examined objectively and carefully. A principal question concerns the availability of different technical procedures that allows naming of a structure on a specific part of the auricle. Obviously, the clinical experience involving collection of patients' data and observing the relationships between the clinical dysfunctions of organs and the noted signs on the auricle is the most productive and useful method. Nogier rapidly imagined some simple instruments that could be used to palpate the auricle, when searching for painful zones or points. After the basic work of Niboyet on the impedance of acupoints, many punctiform electrical detectors were devised. In addition, a collaboration in the 1970s at the research INSERM Unit 103 allowed researchers including Nogier, Niboyet, Jarricot, Bourdiol, and Casez, all belonging to the Groupe Lyonnais d'Etudes Médicales (GLEM) to provide courses, animal experimentation, and cadaver dissections in order to define the scientific bases of somatic and auricular acupuncture. The pressure pain test with diverse modalities has since been taught and demonstrated to many medical specialists who attended the GLEM courses in Marseilles and Lyon.
The experiments performed by Bourdiol37 and Nogier of the thumb pinching test showed how a typical pain disappeared after removing a clamp, because of the emergence of changes in the auricular zone of the thumb. This demonstration suggested a connection between a zone of the auricle and a particular organ and was confirmed using functional MRI (fMRI) by Alimi38 and Liboni et al.39 repeating the demonstration. This study showed images in the somatosensory cortex corresponding to the zone of the hand with occasional bilateral activation. However, it is important to remember that fMRI is based on the possible identification, by a special signal, of the hyperoxygenated venous blood flow occurring after activation of a group of cortical neurons. This corresponds to “blood oxygen level dependency” (a bold effect). More blood is given to working neurons under the control of astrocytes. This also presupposes that the blood supply is of a terminal type, without anastomoses, before cortical distribution. Therefore, fMRI does not provide a direct translation of neuronal activity and has limited resolution. Performing fMRI slices in the three conventional planes cannot guarantee true detection of the thumb area.
Other researchers have presented auricle maps with many points corresponding not only to body organs of the locomotor system, digestive tract, urogenital apparatus, endocrine glands, etc. These researchers have presented maps with points corresponding also to pathologic dysfunctions, such as migraine, anxiety, vertigo, etc., and to central-nervous structures such as the corpus callosum, anterior commissure, brainstem, thalamus, basal ganglia, etc. Of course there are important differences among cartographies and great debates about the various maps. In the current author's opinion, the maps are achieved without any acceptable scientific proof and depend only on the imagination of their creators. The possible connections between certain organs and the CNS appear to be in relation to the richness of the innervation of the auricle, particularly by the trigeminal nerve (V), which has the longest brainstem nucleus, and by the vagal nerve, which is responsible for the parasympathetic control of all visceral organs. The WHO working group recommended to accept only auricular points that have proven efficacy. However, there has been no scientific validation of the location of CNS structures on the auricle.
Nogier, Bourdiol, and Bahr created in 1981 the concept of auriculomedicine, based principally on a special reflex called by Nogier RAC [reflexe auriculo-cardiaque] and translated in English by Pierre Magnin, MD, as the VAS [vascular autonomic signal].40 This term is not appropriate, because medicine is a therapy that covers all the specialties and cannot be reduced to a controversial sector of the body and a nonspecific vascular reflex. Nogier was an excellent acupuncturist and received extensive training on how to palpate arterial pulses. This technique was commonly used by Chinese practitioners,41 who described many variations of pulses in relation to physiology and pathology. Therefore, since the beginning of his work on the auricle, Nogier palpated the radial pulses of his patients, and he described a pulse modification that he later called the VAS. The heart does not have the sufficient power alone to push all the body's blood within the very long arterial and capillary network. An important “boost” is provided by the arteries, which are supple tubes equipped within their walls by a smooth muscle, which can, under sympathetic nervous system control, create two extreme states of vasoconstriction or vasodilatation. The heart pump does not ensure continuous blood propulsion. However, there is an intermittent pulsed flow created by systolic contractions that generates all along the vessels up to the capillaries a wave having a higher velocity than the blood flow itself (in the order of 9 m/sec). The intensity of these waves depends both upon the heart and upon the tonicity of the arterial wall. This phenomena explains why an abnormal rigidity of the arteries can cause hypertension. The cardiac rhythm is very sensitive to emotions and to many outside or inside phenomena.
Sensing the VAS, with the thumb of one hand of the observer placed on the radial artery of the patient and the other touching or palpating the auricle, is not an easy task. It requires long training, which is also an argument that leads to doubt about this technique's reliability and reproducibility. In addition, the VAS has never been scientifically measured with the appropriate transducers, despite the unpublished investigations conducted by Magnin in France with a mechanical sensor and by J.H. Navach, MD, in the United States42 with an infrared photo pulse sensor and bidirectional Doppler imaging. These studies are not totally convincing at the present time.43
Use of light for auriculotherapy is also debatable. Photons do play a role in the stimulation of some part of the skin and they do generate a pigmentation reaction. But using colored light, as described in the books of Rouxeville et al.,44,45 using colored filters, as Van Wijk did,46 to treat acupoints in the auricle or on the body, has no real scientific basis. It is also the case for the different frequencies described by Nogier. The domain of molecules and atoms is the quantum world, which is not accessible to human natural senses. In the current author's opinion, it is pure imagination to refer to it to explain auriculotherapy. Modern opto-genetics is a very promising field that enables the transfer of a pigment, such as rhodopsine, to body neurons and to achieve inhibition or activation in relation to the red or green coloring of the light stimulation. However, the situation is completely different in the auricle, where there are no body neurons but only nervous fibers and some immune cells. For auriculotherapy to become accepted by all the medical community, in the current author's opinion, it is important to remove the cartographies that are not scientifically acceptable from auriculotherapy and propose cartographies based on scientific experiments.
The CNS Connections
According to the advancement of our knowledge about the nervous system—in all the specific and complementary domains of neuroanatomy, neurocytology, genetics, neurophysiology, neurochemistry, neuroimmunology, neuropathology, and modern imaging techniques—it seems feasible to understand better the complex processes of somatic and auricular acupuncture.47
Two basic facts have to be taken in consideration.
First, humans have very complicated biologic systems that are well-organized to carry out very precise physiologic functions to sustain life. When a biologic process or a structure looks quite odd, or is exposed in a nonacceptable manner by an untrained observer, it is mandatory to evaluate the situation. The skin of the body is full of NVCs, which, obviously, do not exist only for a medical practitioner to place needles in them. They are related to homeostasis, maintenance of the skin, and control of the blood supply to internal organs, playing a specific role in the thermoregulation process. In other words, what is thought of from the outside as a “bizarre” structure is understood to be logically integrated within the body after appropriate scientific investigations explaining the structure's physiologic role clearly. Different forms of pain are one of the most successful targets of acupuncture treatment and it is important to understand the organization of the main CNS pain-control centers in the spinal cord, brainstem, reticular formation, thalamus, and cortex. The pain signal has two modalities: (1) an alarm system traveling as fast as possible to the cerebral cortex for protection of structures; and (2) an emotional component related to the organization of the limbic system and prefrontal cortex. A complex processing system integrating many different sensitive inputs operates at the level of the thalamus; this explains the possibility of an interaction between two different types of pain: (1) chronic pain located anywhere in the body, which generates a permanent oscillatory circuit; and (2) an induced pain accomplished by needling or stimulating an acupoint. This could create extinction of the chronic pain and this may explain the immediate clinical positive results noted. In addition, the many neurotransmitter secretion centers located within the CNS (monoamines and acetylcholine) play a great role, collectively, in shedding light some prolonged actions of auriculotherapy as well as somatic acupuncture. This is an hypothesis that is deductible from experiments.
Second, it is important to educate medical students and beginning medical doctors properly by organizing high-quality courses with different levels, in which an understanding of neuroanatomy is a main objective. It is also particularly important that teachers, avoid giving false conceptions or personal interpretations of what is taught unless it is rigorously proven by the scientific method.
Conclusions
After reviewing the scientific data related to auriculotherapy, it seems no longer possible to doubt the reality of the acupoints and the efficacy of this therapy particularly for addressing pain. However, this does not mean that work should cease in this field.
The great amount of work that has been performed up to the present time to attempt standardization of auricular nomenclature should be recognized and new work in this area should be encouraged. Current auricle cartographies have to be revised in order to eliminate the registered points that are without scientific validation, particularly those points related to the CNS. The present knowledge about all aspects of CNS organization should be disseminated more among practitioners in order to improve their understanding of the neurophysiologic mechanisms that explain the efficiency of both somatic and auricular acupuncture. It might also be useful in the future to have more common meetings of the two types of acupuncture.
Disclosure Statement
No competing financial interests exist.
EDITOR'S NOTE: This viewpoint expressed by the author represents a dualistic, mechanistic Western paradigm as contrasted with the Eastern paradigm that includes the existence of many truths. Another contrast is with modern physics, which posits the existence of multiverses. We wish to present a broad range of perspectives, including those that may differ from those of many proponents of auriculotherapy.
References
- 1.Nogier Paul. Treatise of Auriculotherapy [in French]. Moulins-les-Metz: Maisonneuve; 1969 [Google Scholar]
- 2.Nogier P. Acupuncture of the ear pavilion [in German]. Deutsche ZeitshriftfürAkupunktur (DZA) 1957;Band VI:25–35 [Google Scholar]
- 3.Huard P, Wong M. Chinese Medicine, 2nd ed. [in French]. Paris: PUF; 1969 [Google Scholar]
- 4.Soulié de Morant G. TheTrueChinese Acupuncture: Doctrine/Diagnostic/Therapeutic (1934) [in French]. Paris: Mercure de France; 1971 [Google Scholar]
- 5.Niboyet JE. The Lowest Electrical Resistance of Punctiform Surfaces and Cutaneous Routes Corresponding to “Points” and “Meridians”: Basis of Acupuncture [in French]. PhD thesis. Marseille, France: Faculty of Sciences; 1963 [Google Scholar]
- 6.Niboyet JE. Recent Data on the Skin Physiology [in French]. Second doctoral thesis. Marseille, France: Faculty of Sciences; 1963 [Google Scholar]
- 7.Niboyet JE. The least resistance to electricity of punctiform surfaces and of cutaneous points and meridians: Basis of acupuncture. In: Treatise of Acupuncture [in French]. Maisonneuve: Sainte-Ruffine; 1970:123–350 [Google Scholar]
- 8.Terral C. Identification and trial of explanation of the least electrical resistance points of the skin [in French]. MS thesis. Montpellier, France: Faculty of Sciences and of Medicine; 1986 [Google Scholar]
- 9.Terral C, Rabischong P. A scientific basis for acupuncture? J Altern Complement Med. 1997;3(suppl1):S55–S65 [Google Scholar]
- 10.Kim BH. On the Kyungrak System [in Korean]. Pyongyang: D.P.R.K.; 1964 [Google Scholar]
- 11.Kellner G. On a vascularized nerve-ending corpuscle of the Krause end-organ type [in German]. Z Mikrosk Anat Forsch, 1966:75(1):130–144 [PubMed] [Google Scholar]
- 12.Terral C, Rabischong P. Functional role of least electrical resistance points for the homeostasis regulation [in French]. In: Auricular Acupuncture: Acta of Alba [in French]. Montpellier, France: Sauramps Médical; 2003:132–144 [Google Scholar]
- 13.Terral C. Pain and Acupuncture: From Research to Clinical Practice [in French]. Montpellier, France: Sauramps Médical; 2009 [Google Scholar]
- 14.Auziech O. Histological study of the least electrical resistance cutaneous points and analysis of their possible role in the acupunctural phenomenon [in French]. MD thesis. Montpellier, France: Faculty of Medicine; 1984 [Google Scholar]
- 15.Senelar R. Auziech O. Histophysiology of the Acupoint and Traditional Chinese Medicine [in French]. In: Encyclopedia of Natural Medicine [in French], IB-2C. Paris; 1989 [Google Scholar]
- 16.Rabischong P, Niboyet JE, Terral C, et al. Pain problems and experimental basis of acupunctural analgesia [in French]. Nouv Press Méd. 1975;4(28):2013–2020 [PubMed] [Google Scholar]
- 17.Rabischong P, Niboyet JE, Terral C, Senelar R, Casez R. Experimental basis of acupuncture analgesia [in French]. Nouv Press Méd. 1975;4(28):2021–2026 [PubMed] [Google Scholar]
- 18.Margolin A, Chang P, Avants SK, Kosten TR. Effects of sham and real auricular needling: Implications for trials of acupuncture for cocaine addiction. Am J Chin Med. 1993;21(2):103–111 [DOI] [PubMed] [Google Scholar]
- 19.Park J, White A, Stevinson C, Ernst E, James M. Validating a new non-penetrating sham acupuncture device: Two randomised controlled trials. Acupunct Med. 2002;20(4):168–174 [DOI] [PubMed] [Google Scholar]
- 20.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352(9125):364–365 [DOI] [PubMed] [Google Scholar]
- 21.Moffet HH. Sham acupuncture may be as efficacious as true acupuncture: A systematic review of clinical trials. J Altern Complement Med. 2009;15(3):213–216 [DOI] [PubMed] [Google Scholar]
- 22.National Institutes of Health (NIH) Acupuncture. NIH Consensus Development Conference Statement, November3–5,1997:1–34 Online document at: www.consensus.nih.gov/1997/1997acupuncture107html.htm Accessed February19, 2014 [Google Scholar]
- 23.White P, Lewith G, Hopwood V, Prescott P. The placebo needle, is it a valid and convincing placebo for use in acupuncture trials? A randomized, single-blind, cross-over pilot trial. Pain. 2003;106(3);401–409 [DOI] [PubMed] [Google Scholar]
- 24.Li L, Liu H, Li YZ, et al. The human brain response to acupuncture on same-meridian acupoints: Evidence from an fMRI study. J Altern Complement Med. 2008;14(6):673–678 [DOI] [PubMed] [Google Scholar]
- 25.Yang HQ, Xie SS, Li H, Wang YH. On optics of human meridians. Sciences in China: Series G. Physics, Mechanics Astronomy. 2009;52(4):502–507 [Google Scholar]
- 26.Dhond RP, Witzel T, Hämäläinen M, Kettner N, Napadow V. Spatiotemporal mapping the neural correlates of acupuncture with MEG. J Altern Complement Med. 2008;14(6):679–688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li HY, Yang JF, Chen M, et al. Visualized regional hypodermic migration channels of interstitial fluid in human beings: Are these ancient meridians? J Altern Complement Med. 2008;14(6):621–628 [DOI] [PubMed] [Google Scholar]
- 28.Nogier P. The Man in the Ear. Sainte-Ruffine, France: Maisonneuve; 1985 [Google Scholar]
- 29.Federative Committee on Anatomical Terminology Terminologia Anatomica: international Anatomical Terminology [revision of Nomina Anatomica]. Stuttgart: Thieme Verlag; 1998 [Google Scholar]
- 30.Whitmore I. Terminologia Anatomica: New terminology for the new anatomist Anat Rec. 1999;257(2):50–53 [DOI] [PubMed] [Google Scholar]
- 31.Oleson T. International standardization of auricular acupuncture nomenclature [presentation]. Proceedings of the 7th International Symposium of Auriculotherapy. Lyon, France, June8–9, 2012:81–94 [Google Scholar]
- 32.Oleson T. Auricular landmarks identified on a three-dimensional ear model [presentation]. Proceedings of the 7th International Symposium of Auriculotherapy. Lyon, France, June8–9, 2012:53–59 [Google Scholar]
- 33.Zhao B. Thoughts and strategies of developing an international standard of auricular acupuncture points [presentation]. Proceedings of the 7th International Symposium of Auriculotherapy. Lyon, France, June8–9, 2012:95–105 [Google Scholar]
- 34.Oleson T. Auriculotherapy Manual: Chinese and Western Systems of Ear Acupuncture, 3rd ed. Amsterdam: Elsevier Health Sciences; 2003 [Google Scholar]
- 35.Romoli M. The use of the auricular sectogram for diagnostic and therapeutic purposes [presentation]. Proceedings of the 7th International Symposium of Auriculotherapy. Lyon, France, June8–9, 2012:61–65 [Google Scholar]
- 36.Alimi D. The need to have an international nomenclature in auriculotherapy [presentation; in French]. Proceedings of the 7th International Symposium of Auriculotherapy. Lyon, France, June8–9, 2012:107–117 [Google Scholar]
- 37.Bourdiol RJ. Elements of Auriculotherapy. Moulins-lez-Metz, France: Maisonneuve; 1982 [Google Scholar]
- 38.Alimi D,Geissmann A, Gardeur D. Auricular acupuncture stimulation measured on functional magnetic resonance imaging. Med Acupunct. 2007;13(2):18–21 [Google Scholar]
- 39.Liboni W, Romoli M, Allais G, et al. The fMRI for the auricular acupuncture validation: Experimental protocol [presentation; in Italian]. Acti XXII Congresso Nationale Soc Ital Rifles Ago Auri (SIRAA): November16–17, 2007 [Google Scholar]
- 40.Marignan M, Vulliez C. Is the VAS finally elucidated? [presentation; in French]. Proceedings of the 7th International Symposium of Auriculotherapy Lyon, France, June8–9, 2012:187–194 [Google Scholar]
- 41.Xu L, Meng MQH, Shi C, Wang K, Li N. Quantitative analyses of pulse images in Traditional Chinese Medicine. Med Acupunct. 2008;20(3):175–189 [Google Scholar]
- 42.Navach JH. The vascular autonomic system pulse, recording techniques [presentation]. First International Congress of Acupuncture and Auricular Medicine, Mallorca, Spain, September19, 1980 [Google Scholar]
- 43.Ackerman JM. Energy Fields in Medicine: A Study of Device Technology Based on Acupuncture Meridians and Chi Energy. Kalamazoo, MI: The John E.Fetzer Foundation; 1989 [Google Scholar]
- 44.Rouxeville Y. Personalized Auricular Acupuncture [in French]. Montpellier, France: Sauramps Médical; 2000 [Google Scholar]
- 45.Rouxeville Y, Méas Y. Panorama of Auriculotherapy and Auriculomedicine [in French]. Paris: Springer-Verlag France; 2011 [Google Scholar]
- 46.Van Wijk WR, Ackerman JM, Van Wijk EPA. Effects of a color filter used in auriculomedicine on ultraweak photon emission of the human body. J Altern Complement Med. 2006;12(10):955–962 [DOI] [PubMed] [Google Scholar]
- 47.Rabischong P. Anatomy, embryology and neurophysiology. In: Romoli M, ed. Auricular Acupuncture Diagnosis Edinburgh: Churchill Livingstone; 2010:15–35 [Google Scholar]