Abstract
This study adapted Andersen's Health Belief Model to examine the predictors of mental health services utilization among Korean American (KA) immigrants. A cross-sectional survey was used to gather data on 363 KA immigrants 18 years and older residing in New York City. Predisposing factors included gender, age, marital status, education, length of stay in the US, and religion; the need factor was depression; and enabling factors included health insurance, English proficiency, income, and perceived need for help. Approximately 8.5 % of participants reported having utilized mental health services, while 23 % reported having depressive symptoms. Shorter duration of residence in the US, lower income, and the presence of perceived need for help were significantly related to use of mental health services. The perceived need for help mediated the relationship between depression and mental health service utilization. Failure to perceive the need for psychological help continues to be a major reason that KA immigrants do not use mental health services.
Keywords: Depression, Health belief model, Korean American immigrants, Mental health service utilization, Perceived need
Introduction
As health disparities continue to be a major public health concern in the United States (US), the underutilization of mental health services by Asian Americans continues to be a critical public mental health concern (Baquet et al. 2004; Chin et al. 2007). Although Asian Americans suffer from a wide range of mental health problems, their mental health services utilization rate has been critically low (Ku and Waidmann 2003; Leong and Lau 2001). A report by the Substance Abuse and Mental Health Services Administration (SAMHSA 2008) indicates that 3.9 % of Asian American adults (ages 18 and up) utilized mental health services in 2008, compared to 6.8 % for African Americans, 7.3 % for Hispanic Americans, and 16.0 % for Caucasian Americans.
This underutilization of mental health services by Asian Americans causes more severe and lengthy mental illnesses. Asian Americans have been found to be relatively resistant to utilizing formal mental health services (Leong and Lau 2001), generally using them as a last resort when family members can no longer tolerate psychiatric symptoms (Shin 2002). In addition, many Asian Americans are unaware of mental health issues, believing instead that suffering from depression is a part of life (Bernstein 2007); consequently, they have little knowledge of mental health services and they often do not seek treatment (Jang et al. 2005; Shin 2002). Additional reasons proposed in the health care disparities literature for the gap between the need for and the utilization of mental health services by Asian Americans include stigma and shame attached to mental illness (Shea and Yeh 2008; Jang et al. 2009; Huang et al. 2007); cultural beliefs (Leong and Lau 2001); the high cost of health care and lack of language proficiency (Gong et al. 2003; Ku and Waidmann 2003; Wong et al. 2006); lack of health insurance (Ku and Waidmann 2003); and financial constraints, perceived lack of benefit from services, and lack of health care access (Abe-Kim and Takeuchi 1996). Other studies found that those who reported worse physical and mental health self-ratings were more likely to use mental health services (Kang et al. 2010; Kim et al. 2010).
Most studies of immigrants have focused on acculturation as a predictor of mental health service use and have used length of stay in the US and English proficiency as indictors for acculturation (Jang et al. 2005; Kang et al. 2010; Kim et al. 2010). More acculturated Asian Americans, who have been in the US longer and have a higher level of English proficiency, are more likely to use mental health services (Jang et al. 2005; Kim et al. 2010). Leong and Lau (2001) emphasize the importance of culturally informed conceptions of mental illness shared by Asian American subgroups to understand barriers to seeking mental health services. For example, Asian Americans consider behaviors as signs of mental illness only if they are upsetting to their social group; thus, they will generally only seek professional help for psychotic, dangerous, or disruptive behaviors, not for typical personal problems or general emotional distress, such as depression or anxiety.
Depression is a major mental health problem across all ethnic groups in the United States (Center for Disease Control and Prevention 2010). Studies have reported that immigrants have to deal with increased stress caused by migration due to major changes in lifestyle, as they have to adjust to new norms, languages, and social conditions (Choi 1997; Lee et al. 2004; Portes and Rumbaut 2006). The strain of these experiences is often associated with symptoms of depression (Choi 1997; Oh et al. 2002). Consequently, Asian Americans who have depression rarely seek the treatment they need because they consider symptoms of depression to be part of their lives rather than manifestations of an illness that can be treated (Bernstein, 2007). Furthermore, studies indicate that Asian Americans have a tendency toward somatization, which is probably their strongest form of symptom expression of affective disorder (Leong and Lau 2004); this may be due to the fact that they tend to report physical symptoms rather than their emotional distress (Park and Bernstein 2008).
However, studies of Asian Americans’ mental health services utilization typically treat them as a single homogenous group, thereby obscuring the variability across the more than 30 Asian American subgroups that differ in language, immigration history, and culture (Leong and Lau 2001). Thus, little is known about socio-cultural factors that may contribute to varying patterns of mental health problems and of mental health services use among Asian American subgroups. Asian Americans comprise of 5.6 % of the US population; Korean Americans (KAs) comprise 11 % of the Asian American population, making them the fifth largest Asian American group. They are also one of the fastest growing ethnic minorities in the US (Hoeffel et al. 2012), as their population has increased 500 % since 1970 (US Census Bureau, 2000). KAs have been found to have greater depressive symptoms compared to other East Asian groups (Kuo 1984), and the prevalence of depression among KAs has been found to be twice as high as that of the general US population (Bernstein et al. 2011). Yet theory based, comprehensive, aggregated data to better understand their underutilization of mental health services are scarce.
While correlates of mental health services use among KAs can be inferred from previous studies of Asian Americans (Kang et al. 2010; Kim et al. 2010), inferences are limited, as these studies treat Asian Americans as a homogenous group. The few studies that have specifically focused on KAs (Jang et al. 2005; Jang et al. 2009) have measured propensity to use, or attitudes toward the use of, mental health services, not the actual use thereof. In addition, there has been growing attention to the role of self-recognized need for treatment as a mediator between mental illness and use of mental health services (Kessler et al. 2001; Kim et al. 2010; Mojtabai et al. 2002; Rabinowitz et al. 2003). These studies suggest that the main reason people with mental illness do not seek mental health services is that they do not acknowledge having mental health problems.
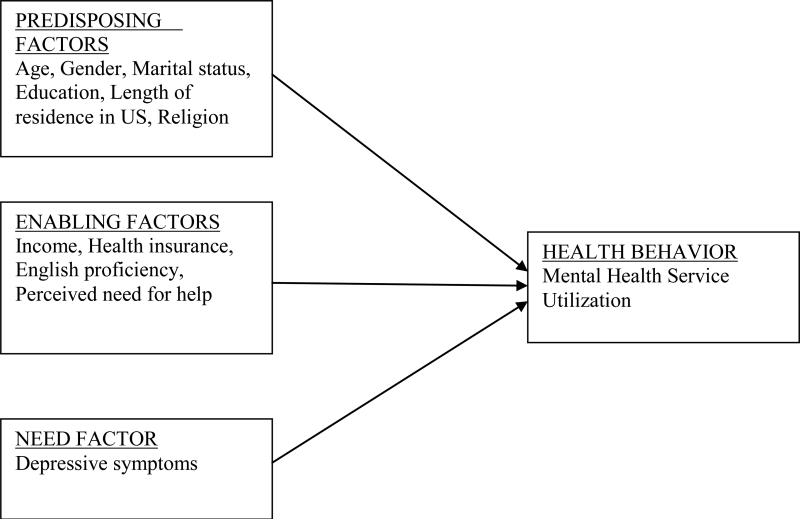
The current study examines factors that contribute to the actual use of mental health services among KA immigrants and the role of self-perceived need in mediating the relationship between depressive symptoms and mental health utilization. It incorporates Andersen's Behavioral Model of Health Care Service Use (1968) as a theoretical framework to explore factors related to this populations’ utilization of mental health care. Andersen's model suggests three factors that affect health behavior: (1) predisposing factors, including demographics, social characteristics, and individual beliefs, (2) need factors, such as an individual's self-perceived need for treatment and a practitioner's evaluation of a disease, and (3) enabling factors, such as personal resources that facilitate or are a barrier to access, as well as the availability of services in the community. It can easily be applied to immigrant and ethnic populations (Andersen et al. 1995), as it includes issues specific to ethnic groups. The conceptual model of our study is illustrated in Fig. 1.
Figure 1.
The Conceptual Framework
Methods
Study Participants and Procedure
The current study was part of a community-based Depression Project in the Korean American community. For Depression Project, a total of 475 KAs were recruited and 416(87.6 %) completed a cross-sectional survey questionnaire between May and November, 2008. Eligibility criteria included (1) self-identified Koreans, regardless of birth place, and (2) self-reported age of 18 years or older. The current study analyzes only the data of KA immigrants who self-reported (1) being born outside the US and immigrating to the US, (2) living in New York City (NYC). We decided to focus on NYC as it is the second most popular US destination for Korean immigrants due to the many Korean media, restaurants and other stores and businesses which help facilitate adjustment (Min and Kim 2010). Approximately 1 in 10 residents in NYC are Asian Americans (Asian American Federation of New York 2004) and Korean immigrants constitute NYC's third largest Asian American subgroup (Min and Kim 2010). The final sample for this current study consisted of 363 participants. Fifty-three were excluded because they did not live in NYC, were born in the US, or complete questions.
Non-probability sampling was used to recruit participants in one of three ways. A press conference was held with Korean media to present the purpose of the research and to publicize the study. Korean community organizations, such as Protestant churches, Buddhist temples, senior centers, and local hospitals, were contacted to inform them about the study and to request permission to distribute a survey questionnaire to organization members. Additional surveys were distributed to customers at, and/or owners of, Korean beauty salons, restaurants, and other retail stores. Survey questionnaires were distributed to participants who agreed to voluntarily participate. The survey was anonymous; participants were not asked for any identifying information and surveys were only identified by a number. In order to reinforce confidentiality, participants were provided with a stamped envelope addressed to the PI with instructions to place the completed survey in the envelope, seal it, and mail it to her. All study procedures were approved by the Institutional Review Board of Hunter College, the City University of New York.
Measures
Dependent Variable
Lifetime use of mental health services after immigration was measured by the question, “Have you received mental health service for your psychological distress after you immigrated to the United States?”
Independent Variables
Predisposing Factors
Predisposing factors toward mental health care utilization included gender, age, marital status, length of residence in the US, religion, and educational attainment. Gender was coded into male (0) and female (1). Marital status was dichotomized into not being currently married, including being divorced, separated, and widowed (0), and being currently married (1). Length of residence in US was categorized into four responses:<5 years (1), 5–10 years (2), 11–20 years (3), and more than 20 years (4). Religion was collapsed into two categories: Protestant (0) and others (1), including Catholic, Buddhist, other and atheist, as the majority of participants reported being Protestant (Bernstein et al. 2011). Educational attainment was coded into four categories: less than high school graduate (1), high school graduate (2), some college or college degree (3), some graduate school or graduate degree (4), and was collapsed into two categories: high school graduate or less (0) and some college education or more (1).
Mental Health Need Factor
Depression, as an indicator of psychological distress, was measured using the Patient Health Questinonaire-9 (PHQ-9). Participants were asked how often they had had any of the following symptoms over the past 2 weeks: little interest (1), feeling depressed (2), sleep problem (3), tiredness (4), eating problem (5), feeling bad about yourself (6), concentration problem (7), motor problem (8), and thoughts about hurting yourself (9). A four-point scale was rated by 0 (not at all), 1 (several days); 2 (more than half of the days), and 3 (nearly every day). A total score for the PHQ-9 was obtained by summing the item scores. These scores ranged from 0 to 27, with a higher score indicating more severe depressive symptoms. Cronbach's alpha was 0.87.
Enabling Factors
Enabling factors included English-language proficiency, income, insurance, and perceived need for help. English language proficiency was assessed by the summation of answers to three questions; participants were asked how well they could write (1), read (2), and speak (3) English, with a four-point response ranging from 1 (poor) to 4 (excellent) for each. English-language proficiency scores ranged from 0 to 12, with higher scores indicating higher proficiency. Cronbach's alpha was 0.93. Income was coded into four categories: less than $30,000 annually (1), more than or equal to $30,000 but less than $60,000 annually (2), more than or equal to $60,000 annually but less than $90,000 annually (3), and more than or equal to $90,000 annually (4); it was dichotomized into less than $30,000 annually (0) and more than or equal to $30,000 annually (1). Insurance was dichotomized into not having (0) and having (1). Perceived need for help was assessed by the single question, “Do you believe that you need help for psychological problems?”; the answers were dichotomized into no (0) and yes (1).
Data Analysis
Sample characteristics were summarized with descriptive statistics. Pearson conduct moment correlations among study variables were performed to identify potential problems with multicollinearity before logistic regression analysis. A hierarchical logistic regression was used to examine factors related to utilization of mental health services. Predisposing factors were entered in Model 1, the need factor was entered in Model 2, and enabling factors were entered in Model 3. In addition, a Sobel-Goodman mediation test was performed to determine whether perceived need for help explains the influence of depression on utilization of mental health services. Statistical analyses were conducted using STATA 10 and the traditional alpha of 0.05 for statistical significance.
Results
Descriptive Characteristics of Sample
The characteristics of the 363 participants are presented in Table 1. There were more women (58 %) than men (42 %). Age ranged from 18 to 81 years, with a mean of 46.3 years (SD = 14.2). Most respondents were currently married (65.3 %), Protestant (57.1 %), had insurance (55.2 %) and had at least some college education (55.4 %). Most (60 %) reported a yearly household income of greater than $30,000. Most (57 %) had lived in the US for ten or more years. Mean English-language proficiency was 6.59 out of 12 (SD = 2.20).
Table 1.
Sociodemographic Characteristics
| Variables | % / Mean (SD) |
|---|---|
| Gender | |
| Male | 42.15 |
| Female | 57.85 |
| Age | |
| Mean (S/D) | 46.33 (14.16) |
| Range | 18-81 |
| Marital Status | |
| Currently being married | 65.28 |
| Not being married | 34.16 |
| Education | |
| Less than high school | 5.29 |
| High school | 27.30 |
| College | 55.43 |
| Graduate school | 11.98 |
| Income | |
| Less than $30,000 | 40.12 |
| $30,000 - $59,999 | 34.88 |
| $60,000 - $89,000 | 14.53 |
| $90,000 or more | 10.47 |
| Years in the U.S. | |
| Fewer than 5 years | 14.04 |
| 5-10 years | 28.65 |
| 11-20 years | 28.94 |
| More than 20 years | 28.37 |
| Religion | |
| Protestant | 57.07 |
| Buddhism | 6.13 |
| Catholic | 23.47 |
| Other religion | 1.33 |
| None | 12.00 |
| English proficiency | |
| Mean (SD) | 6.59 (2.20) |
| Range | 3-12 |
| Insurance | |
| Yes | 55.17 |
| No | 44.83 |
Prevalence of Depression, Perceived Deed for Help, and Mental Health Service Utilization
Approximately 8.5 % of respondents reported having used mental health services for psychological distress since immigrating to the US. Approximately one-fourth (23.1 %) scored five or higher on the PHQ-9, indicating at least mild depressive symptoms and the potential need for mental health treatment (Donnelly and Kim 2008); of these, slightly less than half (45 %) reported a need for help while slightly more than half (55 %) did not perceive a need for help. Fewer than one-fifth (18.2 %) of all participants perceived a need for help.
Hierarchical Logistic Regression Analysis
Table 2 presents the results of hierarchal logistic regression analyses that examined predisposing, need and enabling factors as predictors of the use of mental health services. In Model 1, which included predisposing factors, length of residence in the US was significantly related to the lifetime use of mental health services; respondents who had lived in the US between 5 and 10 years were less likely to use mental health services than were those who had lived in the US for 5 years [OR = 0.22, 95 % CI (0.07, 0.77)] or for more than 20 years [OR = 0.20, 95 % CI (0.04, 0 0.95)]. However, there was no statistically significant difference in the use of mental health services between those who had lived in the US for <5 years and those who had lived in the US between 10 and 20 years. When depression as a need factor was entered into Model 2, length of residence remained significant and depression emerged as a significant factor associated with use of services [OR = 1.15, 95 % CI (1.05, 1.26)].
Table 2.
A Hierarchical Logistic Regression of mental health service use
| Variables | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Odd ration [95% CI] | |||
| Male | 1.22[0.52, 2.90] | 1.02 [0.42, 2.48] | 0.81 [0.32, 2.07] |
| Age | 1.01[0.97, 1.05] | 1.01 [0.97, 1.06] | 1.01 [0.97, 1.06] |
| Not being married | 1.36[0.52, 3.54] | 1.71 [0.63,4.64] | 2.46 [0.81, 7.47] |
| Years in the US (<5 years) | |||
| 5 and 10 years | 0.22 [0.07, 0.77]* | 0.15 [0.04, 0.57] | 0.20 [0.05, 0.76]* |
| 11 and 20 years | 0.38 [0.11, 1.27] | 0.31 [0.09, 1.09]** | 0.41 [0.11, 1.60] |
| > 20 years | 0.20 [0.04, 0.95]* | 0.17 [0.03, 0.83] | 0.16 [0.03, 0.91]* |
| Protestant | 2.06 [0.88, 4.83] | 2.20 [0.91, 5.31]* | 2.14 [0.86, 5.34] |
| Education | 0.95 [0.35, 2.57] | 1.00 [0.36, 2.83] | 1.36 [0.46, 4.04] |
| English-language proficiency | 0.96 [0.75, 1.22] | 1.01 [0.79, 1.28] | |
| Depression (PHQ-9) | 1.15 [1.05, 1.26]* | 1.11 [0.99, 1.25] | |
| 1.05 [0.81, 1.37] | |||
| Income | 0.27 [0.10, 0.78]* | ||
| Insurance | 2.04 [0.75, 5.57] | ||
| Perceived need for help | 3.20 [1.07, 9.51]* | ||
| Chi-square test | X2 (9) =10.38 | X2 (10) =19.25* | X2 (13) =31.98** |
Notes: CI= Confidence interval
P<0.05
p<0.01
***p<0.001
When the enabling factors of English-language proficiency, income, insurance, and perceived need for help were entered into Model 3, the effect of depression disappeared, while income and perceived need for help remained significant factors related to the use of mental health services. Those who had lived in the US between 5 and 10 years [OR = 0.20, 95 % CI (0.05, 0.76) and for more than 20 years (OR = 0.16, 95 % CI (0.03, 0.91)] were less likely to use mental health services than were those who had lived in the US for 5 years. Those who reported an annual income of $30,000 or more were less likely to report using mental health services than were those who reported an annual income of less than $30,000 [OR = 0.27, 95 % CI (0.10, 0.78)]. Those who reported needing help for psychological problems were three times more likely than others to use mental health services [OR = 3.20, 95 % CI (1.07, 9.51)].
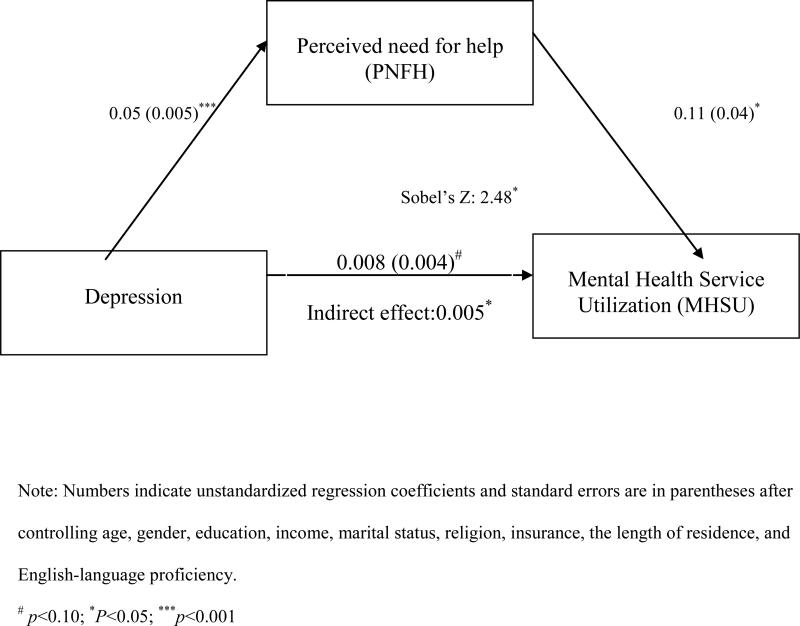
Mediation Analysis of the Perceived Need
Figure 2 presents the result of a single mediation analysis to assess the role of perceived need for help in mediating the relationship between depression and mental health services utilization (MHSU). The direct effect of the perceived need for help (PNFH) and depression on mental health services utilization was BPNFH--MHSU = 0.11 (p<0.05) and BDepression--MHSU = 0.083 (p>0.5). The direct effect of depression on perceived need for help was BDepression--PNFH = 0.05 (p<0.001). When the mediating effect of perceived need for help was tested, the indirect effect of depression on mental health use was BDepression-- PNFH-- MHSU = .005. The Soble-Goodman test indicted that the indirect effect of depression on MHSU through the mediating variable (PNFH) was statistically significant (Soble'z = 2.48, p<0.05).
Figure 2.
Mediation analysis of perceived need for help
Note: Numbers indicate unstandardized regression coefficients and standard errors are in parentheses after controlling age, gender, education, income, marital status, religion, insurance, the length of residence, and English-language proficiency.
# p<0.10; *P<0.05; ***p<0.001
Discussion
This study aimed to examine factors associated with mental health services utilization among KA immigrants living in NYC. Consistent with previous studies that have found low utilization rates among Asian Americans (Leong and Lau 2001; Kang et al. 2010; Kim et al. 2010), only 8.5 % of respondents reported using mental health services for any type of psychological distress since their immigration, although nearly a quarter of the sample reported currently experiencing mild to severe depressive symptoms. However, it is necessary to note the difference between asking participants about their use of mental health services for any type of psychological distress and measuring depression specifically. It is not known how many respondents who answered in the affirmative used mental health services specifically for depression. A future study can explore further the types of, and prevalence of, psychological distress for which KA immigrants seek mental health services. Our study demonstrates that perceived need for help is an influential factor in the use of mental health services by KA immigrants; those respondents who indicated that they perceived the need for mental health help were more likely to have pursued such care than those who did not perceive the need for it. This is consistent with findings of previous studies that show perception of need to be a key factor in help-seeking (Dhingra et al. 2010; Edlund et al. 2006; Kim et al. 2010; Kimerling and Baumrind 2005; Nguyen 2001). Our findings suggest that KA immigrants with depressive symptoms may not seek help in the mental health system because they are not aware that their symptoms might benefit from mental health services. The Korean conceptualization of depression likely explains this; rather than conceptualizing depression as a disease which requires professional help, it is instead considered a lack of will power that can be overcome by having a strong will (Park and Bernstein 2008).
Additionally, when they do seek treatment for mental health problems, Asian Americans tend to use alternative medicine, such as acupuncture, chiropractic, herbal therapy, or massage, rather than traditional western mental health services (Choi and Kim 2010; Le Meyer et al. 2009). Choi and Kim (2010) assert that because alternative medicine and therapy involve less exposure of private feeling and emotions than do traditional mental health treatment, they may be more culturally acceptable to Asian Americans. While coordinating educational efforts with alternative treatments or integrating multiple approaches may enhance utilization of mental health services, such efforts can only effectively be accomplished after further study of the extent to which KA immigrants specifically utilize alternative medicine and their reasons for doing so.
The current findings suggest the importance of community education to increase awareness of depressive symptoms and of mental health treatment as a means to improve the utilization of mental health services by KA immigrants. Such education can be initiated by Korean mental and behavioral professional organizations locally or nationally in conjunction with other major Korean community agencies. For example, Korean churches play a central role in meeting the social and cultural needs of many KA immigrants; therefore, church leaders are more likely to act as “gate keepers’’ to mental health services than are health care professionals (Lee et al. 2008). Korean churches and KA mental health professional organizations can jointly hold mental health educational workshops for KA immigrants and likely get greater participation than if such workshops were held solely by professional organizations. However, the impact of such community education programs has not been studied to determine if they could have the intended outcomes.
Our finding of an association between length of residence and utilization of mental health services is inconsistent with previous studies that reported a positive relationship between duration of residence and mental health services utilization (Dias et al. 2008; Tata and Leong 1994). In our study, KA immigrants who had lived in the US for fewer than 5 years reported a higher use of mental health services than did those who had immigrated earlier. One possible explanation may be that the initial three to 4 years after migration are particularly stressful for new immigrants due to disruptions in family life, economic barriers, and the acculturation process (Shin 2010); if KA immigrants do seek help, they may be more likely to do so during this initial post-migration period. Contrary to some studies that reported low income as a major barrier to the use of mental health services (Bledsoe 2008; Kouzis 2005), our study found that participants with higher, rather than lower, incomes utilized fewer mental health services. Dhingra et al. (2010) reported similar results from their community survey of the general population of 35 states; those in a lower income bracket (less than $50,000 annual household income) were more likely to receive mental health treatment than were those in a higher income bracket ($75,000 or more annual household income). One possible explanation is that people with greater financial resources are better equipped to cope with stress and therefore experience less of a need to receive mental health care, as the weight of financial stress may provide a greater emotional burden. For example, Oh et al. (2002) reported that immigrants who achieved high incomes perceived their environment to be more benevolent than did with those in a low income category.
Many studies suggest that younger age, more education, and being female are associated with a significantly increased likelihood of mental health services utilization (Goodwin et al. 2002; Keene and Li 2005; Steele et al. 2007). In our study, though, neither these factors nor religion were significantly related to use of mental health services. While an earlier study reports that having health insurance is associated with increased use of mental health care (Dhingra et al. 2010), our study did not support this finding. Our findings may reflect a time lag between use of mental health services and current insurance status, as we queried insurance status at the time of the survey and use of mental health services at any time after immigration. In addition, our study did not ask whether participants’ insurance covered mental health treatment, which could also factor into a decision to use or not use mental health services.
Unlike other studies (Kang et al. 2010; Kung 2004; Lee et al. 2008), this current study found no association between English-language proficiency and the use of mental health care services. This lack of association is likely to be the result of the high prevalence of bilingual providers in NYC compared to other locations.
This study has several limitations. First, the cross-sectional design prevents drawing causal inferences. Future studies with a longitudinal design will be able to address predicting factors more clearly. Second, convenience sampling of community-dwelling KA immigrants limits generalizability, as the method excludes those who are either institutionalized for severe psychological distress or are not members of any Korean community organization. Third, in the original research design of the depression Project, depression was the only psychological distress variable measured, even though respondents were asked to report their lifetime use of mental health services. Psychiatric disorders other than depression were not assessed to reflect psychological distress, potentially overlooking the variability in psychiatric disorders. Further study is warranted with more comprehensive measures of psychological distress. Fourth, the study utilized self-reported measures, the results of which can potentially be influenced by social desirability, especially if a question seeks sensitive information, such as a history of mental illness. Respondents may underreport their mental health problems, even though the researchers were not present when they answered the survey and the surveys were anonymous. Fifth, our survey questionnaires did not ask about the specific type of mental health services people received, such as psychiatric inpatient service, outpatient clinics, or family counseling centers. The types of mental health services used by KA immigrants, when they utilized them and the duration of such utilization should be studied to provide a more accurate picture of this population's approach to mental health care in order to enhance service utilization. Lastly, our study did not assess attitudes toward mental health services, as negative attitudes might serve as a barrier to care.
Conclusions
Our study is one of a very few that assessed the actual use of mental health services among KA immigrants. Results suggest that failure to perceive a need for psychological help continues to be a barrier to mental health service utilization in this population. Underutilization of mental health services will continue to be a problem as long as KA immigrants experiencing depressive symptoms do not perceive a need for help. To better address the psychological needs of KA immigrants, we need to supplement early screening efforts with public health education for this population on depression and other mental health concerns, as well as on the availability of effective mental health services for treatment. Such efforts should increase perceptions of the need for psychological help and enhance service utilization.
References
- Abe-Kim JS, Takeuchi D. Cultural competence and quality of care: Issues for mental health service delivery in managed care. Clinical Psychology: Science and Practice. 1996;3(4):273–295. [Google Scholar]
- Andersen RM. Behavioral model of families’ use of health services. Research series, no. 25. Center for Health Administration Studies, University of Chicago; Chicago, IL: 1968. [Google Scholar]
- Andersen RM, Harada N, Chiu V, Makinodan T. Application of the behavioral model to health studies of Asian and Pacific Islander Americans. Asian American and Pacific Islander Journal of Health. 1995;3(2):128–141. [PubMed] [Google Scholar]
- Asian American Federation of New York Census profile: New York City's Asian American population. 2004 Retrieved from http://www.aafny.org/cic/briefs/newyorkbrief.pdf.
- Baquet CR, Carter-Pokras O, Bengen-Seltzer B. Healthcare disparities and models for change. American Journal of Managed Care. 2004;10:5–11. [PubMed] [Google Scholar]
- Bernstein KS. Mental health issues among urban Korean American immigrants: Preliminary study. Journal of Transcultural Nursing. 2007;18(2):175–180. doi: 10.1177/1043659606298610. [DOI] [PubMed] [Google Scholar]
- Bernstein KS, Park S, Shin J, Cho S, Park Y. Acculturation, discrimination and depressive symptoms among Korean immigrants in New York City. Community Mental Health Journal. 2011;47(1):24–34. doi: 10.1007/s10597-009-9261-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bledsoe SE. Barriers and promoters of mental health services utilization in a Latino Context: A literature review and recommendations from an ecosystems perspective. Journal of Human Behavior in the Social Environment. 2008;18(2):151–183. [Google Scholar]
- Census Bureau US. Population Census. Washington, DC: US Department of Commerce. Center for Disease Control and Prevention. (2010). Current depression among adults-United States, 2006 and 2008. Morbidity and Mortality Weekly Report. 2000;59(38):1229–1260. [PubMed] [Google Scholar]
- Chin MH, Waters AE, Cook SC, Huang ES. Interventions to reduce racial and ethnic disparities in health care. Medical Care Research & Review. 2007;64(5):7S–28S. doi: 10.1177/1077558707305413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi G. Acculturative stress, social support, and depression in Korean-American families. Journal of Family Social Work. 1997;2(1):81–97. [Google Scholar]
- Choi NG, Kim J. Utilization of complementary and alternative medicines for mental health problems among Asian Americans. Community Mental Health Journal. 2010;46:570–578. doi: 10.1007/s10597-010-9322-4. [DOI] [PubMed] [Google Scholar]
- Dhingra SS, Zack M, Strine T, Pearson WS, Balluz L. Determining prevalence and correlates of psychiatric treatment with Andersen's behavioral model of health services use. Psychiatric Services. 2010;61(5):524–528. doi: 10.1176/ps.2010.61.5.524. [DOI] [PubMed] [Google Scholar]
- Dias SF, Severo M, Barros H. Determinants of health care utilization by immigrants in Portugal. BMC Health Service Research. 2008;8:207–211. doi: 10.1186/1472-6963-8-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly PL, Kim KS. The Patient Health Questionnaire (PHQ-9K) to screen for depressive disorders among immigrant Korean American elderly. Journal of Cultural Diversity. 2008;15(1):24–29. [PubMed] [Google Scholar]
- Edlund M, Unutzer J, Curran GM. Perceived need for alcohol, drug, and mental health treatment. Social Psychiatry and Psychiatry Epidemiology. 2006;41:480–487. doi: 10.1007/s00127-006-0047-1. [DOI] [PubMed] [Google Scholar]
- Gong F, Gage SJL, Tacata LA., Jr. Help-seeking behavior among Filipino Americans: A cultural analysis of face and language. Journal of Community Psychology. 2003;31:469–488. [Google Scholar]
- Goodwin RD, Hoven C, Lyons J, Stein M. Mental health service utilization in the United States. The role of personality factors. Social Psychiatry and Psychiatry Epidemiology. 2002;37:451–566. doi: 10.1007/s00127-002-0563-6. [DOI] [PubMed] [Google Scholar]
- Hoeffel EM, Rastogi S, Kim MO, Shaid H. The Asian Population. 2012:2010. Retrieved from http://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf.
- Huang ZJ, Wong FY, Ronzio C, Yu SM. Maternal depression symptomatology and mental health help seeking patterns of US and foreign born mothers. Maternal and Children Health Journal. 2007;11(3):257–267. doi: 10.1007/s10995-006-0168-x. [DOI] [PubMed] [Google Scholar]
- Jang Y, Chiriboga DA, Okazaki S. Attitudes toward mental health services: Age-group differences in Korean American adults. Aging & Mental Health. 2009;13(1):127–134. doi: 10.1080/13607860802591070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang Y, Kim G, Chiriboga DA. Health, healthcare utilization, and satisfaction with service: Barriers and facilitators for older Korean Americans. Journal of American Geriatric Society. 2005;53(9):1613–1617. doi: 10.1111/j.1532-5415.2005.53518.x. [DOI] [PubMed] [Google Scholar]
- Kang S-K, Howard DM, Kim J, Shepard Payne J, Wilton L, Kim W, et al. English language proficiency and lifetime mental health service utilization in a national representative sample of Asian Americans in the USA. Journal of Public Health. 2010;32(3):431–439. doi: 10.1093/pubmed/fdq010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keene J, Li X. Age and gender differences in health service utilization. Journal of Public Health. 2005;27(1):74–79. doi: 10.1093/pubmed/fdh208. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Bruce ML, Koch R, Laska EM, Leaf PJ, et al. The prevalence and correlates of untreated serious mental illness. Health Services Research. 2001;36:987–1007. [PMC free article] [PubMed] [Google Scholar]
- Kim G, Jang Y, Chiribiga DA, Ma GX, Schonfeld L. Factors associated with mental health service use in Latino and Asian immigrant elders. Aging and Mental Health. 2010;14(5):535–542. doi: 10.1080/13607860903311758. [DOI] [PubMed] [Google Scholar]
- Kimerling R, Baumrind N. Access to specialty mental health services among women in California. Psychiatric Services. 2005;56(6):729–734. doi: 10.1176/appi.ps.56.6.729. [DOI] [PubMed] [Google Scholar]
- Kouzis A. Social factors, need, and mental health services utilization: Findings of the National Comorbidity Survey. Research in Sociology of Health Care. 2005;23:57–78. [Google Scholar]
- Ku L, Waidmann T. How race/ethnicity, immigration status and language affect health insurance coverage. 2003 Retrieved from http://www.kff.org/uninsured/kcmu4132report.cfm.
- Kung WW. Cultural and practical barriers to seeking mental health treatment for Chinese Americans. Journal of Community Psychology. 2004;32:27–41. [Google Scholar]
- Kuo W. Prevalence of depression among Asian Americans. Journal of Nervous and Mental Disorder. 1984;172:449–457. doi: 10.1097/00005053-198408000-00002. [DOI] [PubMed] [Google Scholar]
- Le Meyer O, Zane N, Cho YI, Takeuchi DT. Use of specialty mental health services by Asian Americans with psychiatric disorders. Journal of Consulting and Clinical Psychology. 2009;77(5):1000–1005. doi: 10.1037/a0017065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HB, Hanner JA, Cho SJ, Han HR, Kim MT. Improving access to mental health services for Korean-American immigrants. Psychiatry Investigation. 2008;5:14–20. doi: 10.4306/pi.2008.5.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, Moon A, Knight BG. Depression among elderly Korean immigrants: Exploring socio-cultural factors. Journal of Ethnic & Cultural Diversity in Social Work. 2004;13(4):1–26. [Google Scholar]
- Leong FTL, Lau ASL. Barriers to providing effective mental health services to Asian Americans. Mental Health Service Research. 2001;3(4):201–214. doi: 10.1023/a:1013177014788. [DOI] [PubMed] [Google Scholar]
- Min PG, Kim C. Growth of the Korean population and changes in their settlement patterns over time, 1990–2008. 2010 Retrieved from http://www.qc.cuny.edu/Academics/Centers/RCKC/Documents/Settlement%20Patterns.pdf.
- Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Archives of General Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- Nguyen D. Acculturation, perceived need, and mental health service use by older Asian immigrant. Journal of Behavioral Health Services and Research. 2001;38(4):526–533. doi: 10.1007/s11414-011-9245-z. doi:10.1007/s11414-011-9245-z. [DOI] [PubMed] [Google Scholar]
- Oh Y, Koeske G, Sales E. Acculturation, stress, and depressive symptoms among Korean immigrants in the United States. Journal of Social Psychology. 2002;142:511–526. doi: 10.1080/00224540209603915. [DOI] [PubMed] [Google Scholar]
- Park S, Bernstein K. Depression and Korean American immigrants. Achieves of Psychiatric Nursing. 2008;22(1):12–19. doi: 10.1016/j.apnu.2007.06.011. [DOI] [PubMed] [Google Scholar]
- Portes A, Rumbaut RG. Immigrant America: A portrait. University of California Press; Berkeley, CA: 2006. pp. 168–204).. [Google Scholar]
- Rabinowitz J, Gross R, Feldman D. Perceived need and receipt of outpatient mental health services. Journal of Ambulatory Care Management. 2003;26(3):260–267. doi: 10.1097/00004479-200307000-00009. [DOI] [PubMed] [Google Scholar]
- Shea M, Yeh CJ. Asian American students’ cultural values, stigma, and relational self- construal: Correlates of attitudes toward professional help seeking. Journal of Mental Health Counseling. 2008;30:157–172. [Google Scholar]
- Shin JK. Help-seeking behaviors by Korean immigrants for depression. Issues in Mental Health Nursing. 2002;23(5):461–476. doi: 10.1080/01612840290052640. [DOI] [PubMed] [Google Scholar]
- Shin JK. Understanding the experience and manifestation of depression among Korean immigrants in New York City. Journal of Transcultural Nursing. 2010;21:73–80. doi: 10.1177/1043659609349065. [DOI] [PubMed] [Google Scholar]
- Steele LS, Dewa CS, Lin E, Lee KL. Education level, income level and mental health services use in Canada: Associations and policy implication. Health Care Policy. 2007;3(1):96–106. [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration Results from the 2008 National survey on drug use and health: National findings. 2008 Retrieved from http://www.oas.samhsa.gov.
- Tata SP, Leong FTL. Individualism-collectivism, social network orientation, and acculturation as predictors of attitudes toward seeking professional psychological help among Chinese Americans. Journal of Counseling Psychology. 1994;41(3):280–287. [Google Scholar]
- Wong EC, Marshall GN, Schell TL, Elliott MN, Hambarsoomians K, Chun C, et al. Barriers to mental health care utilization for US Cambodian refugees. Journal of Consulting and Clinical Psychology. 2006;74(6):1116–1120. doi: 10.1037/0022-006X.74.6.1116. [DOI] [PubMed] [Google Scholar]