Abstract
Introduction
Syphilis remains a major public health problem in sub-Saharan Africa, including Burkina Faso. However, few published data are available on the prevalence of syphilis in the general population. This study had two main objectives: to determine the seroprevalence of syphilis in a cohort of 37,210 first time blood donors and to study socio-demographic factors associated with the risk of infection by Treponema pallidum.
Methods
Antibodies to Treponema pallidum were screened for, by using Reagin Rapid Test (RPR) and their presence was confirmed by treponema pallidum haemagglutination test (TPHA).
Results
The overall seroprevalence of syphilis was 1.5% among first time blood donors and was significantly different between centers (p <0.001). The infection was significantly higher in men than women among blood donors in Ouagadougou and Fada N′gourma (P = 0.001 and P = 0.034). The overall seroprevalence of syphilis among blood donors was not associated with either age group or HIV status. In contrast, a significantly high seroprevalence of syphilis was observed in blood donors with HBsAg (P = 0.014) and anti-HCV (P = 0.007) positive.
Conclusion
Our report shows a low seroprevalence of syphilis in the representative sample of the population of Burkina Faso. The seroprevalence of syphilis remains unequally distributed between urban and rural areas and was not associated with HIV infection.
Keywords: Syphilis, HIV, blood donor, seroprevalence, Burkina Faso
Introduction
According to the World Health Organization (WHO), each year about 340 million new infections are due to sexually transmitted diseases such as chlamydia, gonorrhea, syphilis and Trichomonas [1]. Syphilis remains a major public health problem in sub-Saharan Africa, including Burkina Faso. It is diagnosed routinely in all blood donors using non-treponemal and treponemal tests such as Rapid Plasma Reagin test (RPR) and T. pallidum haemagglutination Test (TPHA) [2, 3]. Screening for syphilis in Burkina Faso is performed for pregnant women prenatal medical examination of pregnant women, medical prescription in case of clinical suspicion, for the United States of America visa's applicants and for medical screening among new recruits of the army. In Burkina Faso, few published data are available on the prevalence of syphilis in the population. Previous studies have reported a regional variation in the prevalence of syphilis among pregnant women [4, 5] and blood donors[6, 7]; however, most of these studies had several limitations. In fact, they involved a small sample size and the sociodemographic factors associated with the risk of syphilis infection were not systematically studied. Furthermore, the relationship between syphilis and other viruses such as human immunodeficiency virus (HIV), hepatitis B and C viruses (HBV and HCV) were not always considered.
This study has two main objectives: to determine the seroprevalence of syphilis in a cohort of 37,210 first time blood donors recruited in the regional blood transfusion centres of Ouagadougou, Bobo-Dioulasso, Fada N′gourma and Koudougou and to study the socio-demographic factors associated with the risk of infection by Treponema pallidum in the population.
Methods
Donors recruitment
A retrospective analysis of blood donors' data from January to December 2010 was conducted in 4 regional blood transfusion centres in Burkina Faso: Ouagadougou (Central region), Bobo-Dioulasso (High-Basins), Koudougou (Central West region) and Fada N'gourma (Eastern Region). The four blood transfusion centres cover the needs in blood products of the surrounding group of provinces as shown in Figure 1. Voluntary donors were all healthy subjects, selected after responding to a panel of questions comprising a medical background ; and individuals aged 17-64 years with a weight >50 kg, were included for blood donation. All donors answered questions intending to exclude recipients of previous blood transfusion, individuals having experienced jaundice or signs of hepatitis, pregnant women and people having experienced a high-risk sexual behaviour within 2 weeks preceding the intended donation. The socio-demographic characteristics of selected donors were recorded in a database, and venous blood was collected in blood banking bags following standard procedures. In each centre, blood collection was conducted as previously described [8]
Figure 1.
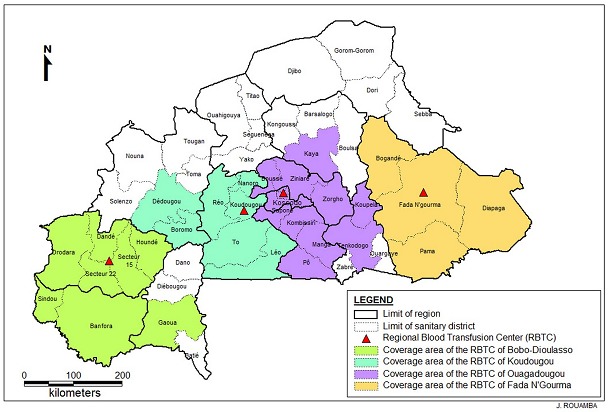
Regional blood transfusion centres and area of coverage in Burkina Faso in 2010
Ethical considerations: This study was approved by the CERBA/Saint Camille Ethics Committee. However, because of the retrospective nature of the study, informed consent was not obtained from the study subjects.
Serological analysis: Antibodies to Treponema pallidum were detected using, Rapid Plasma Reagin test (RPR; Cypress Diagnostics, Langdorp, Belgium) and their presence confirmed by Treponema pallidum haemagglutination test (TPHA, Cypress Diagnostics, Langdorp, Belgium).
Antibodies to HIV types 1 and 2 were screened for using Vironostika HIV Uni-Form II Ag/Ab (Biomérieux, Boxtel,the Netherlands). All samples reactive for HIV, HBsAg and HCV were re-tested for confirmation using a second enzyme-linked immunosorbent assay (Bio-Rad, Marnes la Coquette, France). A result was considered positive if both the first and second tests were positive.
Statistical analysis: Data were analyzed using Statistical Package for the Social Sciences (SPSS version 17; SPSS Inc. Chicago, IL, USA) and EPI-Info version 6.04 dfr (CDC, Atlanta, GA, USA). Odds ratio was calculated to determine risk factors associated with syphilis. P values below 0.05 were considered statistically significant.
Results
Of the 37,210 first time blood donors recruited in the four regional blood transfusion centers, 72.5% (95% CI 72.0 to 73.0) were men and 27.5 (95% CI 26.3 to 28.4) were females. The majority of donors belonged to the age group 20-29 years (58.1%, 95% CI 57.4 to 58.8) and were mainly recruited in urban (70.2%) than rural areas (29.8%) (Table 1). The number of blood donors was respectively 16 925 (45.5%), 8859 (23.8%), 6599 (17.7%) and 4827 (13.0%) in blood transfusion centres of Ouagadougou, Bobo- Dioulasso, Fada and N′gourma and Koudougou. The overall seroprevalence of syphilis was 1.5% among first time blood donors and was significantly different between centers (p <0.001), the highest being observed in Koudougou (2.5%) and lowest in Bobo-Dioulasso (0.7%) (Table 2). The overall seroprevalence of syphilis among blood donors was not associated with either age group or HIV status. In contrast, significantly higher seroprevalence of syphilis was observed in blood donors with HBsAg (P = 0.014) and anti-HCV (P = 0.007) positive.
Table 1.
Sociodemographic characteristics of first-time blood donors in Burkina Faso
| Characteristics | Total number | Percentage | 95% CI |
|---|---|---|---|
| Gender | |||
| Male | 26981 | 72.5 | 72.0-73.0 |
| Female | 10229 | 27.5 | 26.3-28.4 |
| Age groups (years) | |||
| < 20 | 8130 | 21.8 | 20.9-22.7 |
| 20-29 | 21630 | 58.1 | 57.4-58.8 |
| 30-39 | 4792 | 12.9 | 12.0-13.9 |
| 40-49 | 2052 | 5.5 | 4.5-6.5 |
| ≥50 | 606 | 1.6 | 0.6-2.6 |
| Location of blood donation | |||
| Urban areas | 26123 | 70.2 | 69.6-70.8 |
| Rural areas | 11087 | 29.8 | 28.9-30.7 |
| Blood groups | |||
| A | 8430 | 22.7 | 21.8-23.6 |
| AB | 2157 | 5.8 | 4.8-6.8 |
| B | 10476 | 28.2 | 27.3-29.1 |
| O | 16147 | 43.4 | 42.6-44.2 |
| Rhesus (RH) Type | |||
| Positive | 32073 | 86.2 | 85.8-86.6 |
| Negative | 5137 | 13.8 | 12.9-14.7 |
CI = Confidence Interval
Table 2.
Seroprevalence of syphilis among first-time blood donors in 2010
| Characteristics | Total number | Number of syphilis positive | Percentage | P-values |
|---|---|---|---|---|
| Blood centres | ||||
| Bobo-Dioulasso | 8859 | 63 | 0.7 | < 0.001a |
| Fada N'gourma | 6599 | 99 | 1.5 | |
| Koudougou | 4827 | 121 | 2.5 | |
| Ouagadougou | 16925 | 290 | 1.7 | |
| Gender | ||||
| Male | 26981 | 458 | 1.7 | < 0.001b |
| Female | 10229 | 115 | 1.1 | |
| Age groups (years) | ||||
| < 20 | 8130 | 114 | 1.4 | 0.203a |
| 20-29 | 21630 | 359 | 1.7 | |
| 30-39 | 4792 | 69 | 1.4 | |
| 40-49 | 2052 | 23 | 1.1 | |
| ≥50 | 606 | 8 | 1.3 | |
| Location of blood donation | ||||
| Urban areas | 26123 | 355 | 1.4 | < 0.001b |
| Rural areas | 11087 | 218 | 2.0 | |
| Co-Infections | ||||
| HBV | 0.014b | |||
| Positive | 4998 | 97 | 1.9 | |
| Negative | 32212 | 476 | 1.5 | |
| HCV | ||||
| Positive | 2513 | 55 | 2.2 | 0.007b |
| Negative | 34697 | 518 | 1.5 | |
| HIV | 0.662b | |||
| Positive | 802 | 10 | 1.2 | |
| Negative | 36408 | 563 | 1.5 | |
| Blood groups | ||||
| O | 16147 | 227 | 1.4 | 0.068b |
| Non-O | 21063 | 346 | 1.6 |
Pearson Chi square
Fischer's Exact test (2-sided); Significant P-values in Bold
The seroprevalence of syphilis was examined in detail by blood transfusion centre as shown in Tables 3 and 4. The infection was significantly higher in men than women among blood donors in Ouagadougou and Fada N′gourma (P = 0.001 and P = 0.034). Syphilis was not associated with any age group in donors of all blood transfusion centers, even though a slightly higher seroprevalence was observed among blood donors in the age group 20-29 years in Ouagadougou (P = 0.052) (Table 3). Regarding the place of blood donation, the seroprevalence of syphilis was significantly higher in rural compared to urban areas of Ouagadougou and Fada N′gourma (P <0.001) (Tables 3 and 4). The association between syphilis and HIV, HBV and HCV was examined in blood donors. There was no association between HIV and syphilis among all donors of all blood transfusion centers. The seroprevalence of syphilis was higher among donors with HBsAg and anti-HCV positive tests in Bobo-Dioulasso (P = 0.003) and Ouagadougou (P <0.001). No socio-demographic factors were associated with syphilis among blood donors in Koudougou (Table 4).
Table 3.
Socio-demographic characteristics of first-time blood donors at Ouagadougou and Bobo-Dioulasso according to syphilis in 2010
| Ouagadougou | Bobo-Dioulasso | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | N Total | Syphilis Positive N (%) | OR (95% CI) | P-values | N Total | Syphilis Positive N (%) | OR (95% CI) | P-values |
| Gender | ||||||||
| Male | 11427 | 223 (2.0) | 1.6 (1.2-2.1) | 0.001 | 6903 | 51 (0.7) | 1.2 (0.6-2.4) | 0.649 |
| Female | 5498 | 67 (1.2) | 1 | - | 1956 | 12 (0.6) | 1 | |
| Age groups | ||||||||
| < 20 | 3316 | 54 (1.6) | 1.6 (0.8-3.3) | 0.147 | 2371 | 14 (0.6) | NA | - |
| 20-29 | 9659 | 183 (1.9) | 1.9 (1.0-3.7) | 0.052 | 5466 | 45 (0.8) | NA | - |
| 30-39 | 2510 | 38 (1.5) | 1.5 | |||||
| (0.7-3.1) | 0.237 | 667 | 3 (0.4) | NA | - | |||
| 40-49 | 1083 | 11 (1.0) | 1 | - | 298 | 1 (0.3) | 1 | - |
| ≥ 50 | 357 | 4 (1.1) | 1.1 (0.3-3.8) | 0.772 | 57 | 0 (0.0) | - | - |
| Location of blood donation | ||||||||
| Urban areas | 13265 | 192 (1.4) | 1 | - | 5670 | 45 (0.8) | 1.4 (0.8-2.5) | 0.218 |
| Rural areas | 3660 | 98 (2.7) | 1.9 (1.5-2.4) | < 0.001 | 3189 | 18 (0.6) | 1 | - |
| HBV | ||||||||
| AgHBs positive | 2057 | 41 (2.0) | 1.2 (0.9-1.7) | 0.253 | 1038 | 15 (1.4) | 2.4 (1.3-4.4) | 0.003 |
| AgHBs negative | 14868 | 249 (1.7) | 1 | - | 7821 | 48 (0.6) | 1 | - |
| HCV | ||||||||
| Seropositive | 879 | 29 (3.3) | 2.1 (1.4-3.1) | < 0.001 | 532 | 3 (0.6) | 1 | - |
| Seronegative | 16046 | 261 (1.6) | 1 | - | 8327 | 60 (0.7) | 1.3 (0.4-5.1) | 0.677 |
| HIV | ||||||||
| Seropositive | 323 | 5 (1.5) | 1 | - | 164 | 0 (0.0) | - | - |
| Seronegative | 16602 | 285 (1.7) | 1.1 (0.4-3.1) | 0.817 | 8695 | 63 (0.7) | NA | - |
| Blood groups | ||||||||
| O | 7373 | 107 (1.5) | 1 | - | 3766 | 27 (0.7) | 1.0 (0.6-1.7) | 0.955 |
| Non-O | 9552 | 183 (1.9) | 1.3 (1.0-1.7) | 0.020 | 5093 | 36 (0.7) | 1 | - |
Table 4.
Socio-demographic characteristics of first time blood donors at Fada N'gourma and Koudougou according to syphilis
| Fada N'gourma | Koudougou | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | N Total | Syphilis Positive N (%) | OR (95% CI) | P-values | N Total | Syphilis Positive N (%) | OR (95% CI) | P-values |
| Gender | ||||||||
| Male | 5001 | 84 (1.7) | 1.8 (1.0-3.3) | 0.034 | 3650 | 100 (2.7) | 1.6 (0.9-2.6) | 0.068 |
| Female | 1598 | 15 (0.9) | 1 | - | 1177 | 21 (1.8) | 1 | - |
| Age groups | ||||||||
| < 20 | 1350 | 19 (1.4) | 1.1 (0.4-3.2) | 0.788 | 1093 | 27 (2.5) | 1.6 (0.23-32.1) | 0.534 |
| 20-29 | 3474 | 52 (1.5) | 1.2 (0.5-3.1) | 0.663 | 3031 | 79 (2.6) | 1.7 (0.2-32.6) | 0.511 |
| 30-39 | 1163 | 19 (1.6) | 1.3 (0.5-3.7) | 0.554 | 452 | 9 (2.0) | 1.3 (0.2-27.0) | 0.648 |
| 40-49 | 483 | 6 (1.2) | 1 | - | 188 | 5 (2.7) | 1.7 (0.2-39.1) | 0.530 |
| ≥ 50 | 129 | 3 (2.3) | 1.8 (0.4-8.6) | 0.406 | 63 | 1 (1.6) | 1 | - |
| Location of blood donation | ||||||||
| Urban areas | 4387 | 49 (1.1) | 1 | - | 2801 | 69 (2.5) | 1 | - |
| Rural areas | 2212 | 50 (2.3) | 2.1 (1.4-3.1) | < 0.001 | 2026 | 52 (2.6) | 1.0 (0.7-1.5) | 0.821 |
| HBV | ||||||||
| AgHBs positive | 1198 | 23 (1.9) | 1.4 (0.8-2.2) | 0.186 | 705 | 18 (2.6) | 1.0 (0.6-1.7) | 0.932 |
| AgHBs negative | 5401 | 76 (1.4) | 1 | - | 4122 | 103 (2.5) | 1 | - |
| HCV | ||||||||
| Seropositive | 633 | 12 (1.9) | 1.3 (0.7-2.5) | 0.389 | 469 | 11 (2.3) | 1 | - |
| Seronegative | 5699 | 87 (1.5) | 1 | - | 4358 | 110 (2.5) | 1.1 (0.6-2.1) | 0.814 |
| HIV | ||||||||
| Seropositive | 147 | 2 (1.4) | 1 | - | 141 | 3 (2.1) | 1 | - |
| Seronegative | 6425 | 97 (1.5) | 1.3 (0.3-7.8) | 0.513 | 4686 | 118 (2.5) | 1.2 (0.4-4.7) | 0.526 |
| Blood groups | ||||||||
| O | 2908 | 42 (1.4) | 1 | - | 2100 | 51 (2.4) | 1 | - |
| Non-O | 3691 | 57 (1.5) | 1.1 (0.7-1.6) | 0.740 | 2727 | 70 (2.6) | 1.1 (0.7-1.6 | 0.761 |
Discussion
In the present report the seroprevalence of syphilis among first-time blood donors was 1.5%. This prevalence is relatively low compared to higher seroprevalence of 7.5% and 5.7% reported in previous studies respectively in Ghana [9] and Cameroon [10]. Syphilis' seroprevalence was higher in men compared to women. This finding could be explained by the high multiple sexual partners frequently observed in men compared to women [11]. The seroprevalence of syphilis showed a regional variation in blood donors in Burkina Faso in 2010; the highest was found in the Central-west region (Koudougou) and the lowest in the high-basins region (Bobo-Dioulasso). Syphilis' low prevalence has been previously reported in Bobo-Dioulasso [4]. However, the seroprevalence of 0.7% found in the present report is three times higher than the prevalence of 0.24% reported by Sombié et al (2000) in pregnant women.
We showed that syphilis in this study was not evenly distributed according to place of blood collection, as significantly higher seroprevalence was found in rural areas compared to urban ones among blood donors in Ouagadougou and Fada N′gourma. The low prevalence in urban areas could be explained by better prevention campaigns against sexually transmitted diseases compared to rural areas. The overall seroprevalence of syphilis was associated with HBV and HCV among blood donors. High co-infections of syphilis with HBV and HCV have been reported in previous studies [12, 13]. The seroprevalence of syphilis was associated with HBV and HCV among blood donors in Bobo-Dioulasso and Ouagadougou, respectively.
In many previous studies conducted in Africa [14, 15], it has been reported that sexually transmitted diseases such as syphilis increase the risk of HIV infection. Surprisingly, we did not find any association between HIV status and syphilis serology among blood donors. Our results are at variance with those of previous studies, but several arguments can be made to explain the observed discrepancy. Firstly, the lack of association between HIV and syphilis could indicate that the mode of transmission of both diseases may be partly distinct in first-time blood donors. Indeed, the high prevalence of syphilis among blood donors could be partly explained by the plausible existence of non-venereal Treponema in Burkina Faso. Indeed, eight countries have known endemic yaws in 2011 including four neighboring Burkina Faso such as Benin, Ivory Coast, Ghana and Togo [16]. Secondly, HIV and syphilis infections may not be spatially related in Burkina Faso. A recent study in South Africa has shown divergent spatial patterns in the prevalence of the HIV and syphilis in South African pregnant women. HIV was more prevalent in urban areas than elsewhere, while syphilis had a high prevalence in rural areas [17].
Conclusion
We report on a representative sample of the population of Burkina Faso a low seroprevalence of syphilis. Syphilis' seroprevalence remains unequally distributed between urban and rural areas and was not associated with HIV infection.
Acknowledgments
We thank all the participants of this study and The National blood transfusion centre staff.
Competing interests
The authors declare that they have no competing interests
Authors’ contributions
CB, MS, BMN and AK designed the study. CB and TI analyzed data. CB, BMN and TRC wrote the paper. JS corrected and approved the final version of the paper. All the authors read and approved the final version of the paper.
References
- 1.WHO. Geneva: WHO; 2001. Global Prevalence and Incidence of Selected Curable Sexually Transmitted Infections: Overview and Estimates. [PubMed] [Google Scholar]
- 2.Lowhagen GB. Syphilis: test procedures and therapeutic strategies. Semin. 1990 Jun;9(2):152–9. [PubMed] [Google Scholar]
- 3.Wiwanitkit V. Biological false reactive VDRL tests: when to re-test? Southeast Asian J Trop Med Public Health. 2002;33(Suppl 3):131–2. [PubMed] [Google Scholar]
- 4.Sombie I, Meda N, Cartoux M, Tiendrebeogo S, Ouangre A, Yaro S, et al. Seroprevalence of syphilis among women attending urban antenatal clinics in Burkina Faso, 1995-8. The DITRAME Study Group. DIminunation de la TRAnsmission Mere-Enfant. Sex Transm Infect. 2000 Aug;76(4):314–6. doi: 10.1136/sti.76.4.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kirakoya-Samadoulougou F, Defer MC, Yaro S, Fao P, Ilboudo F, Langani Y, et al. Low seroprevalence of syphilis in Burkina Faso. Sex Transm Infect. 2011 Feb;87(1):35–7. doi: 10.1136/sti.2010.042465. [DOI] [PubMed] [Google Scholar]
- 6.Kania D, Sangare L, Sakande J, Koanda A, Nebie YK, Zerbo O, et al. A new strategy to improve the cost-effectiveness of human immunodeficiency virus, hepatitis B virus, hepatitis C virus, and syphilis testing of blood donations in sub-Saharan Africa: a pilot study in Burkina Faso. Transfusion. 2009 Oct;49(10):2237–40. doi: 10.1111/j.1537-2995.2009.02276.x. [DOI] [PubMed] [Google Scholar]
- 7.Nagalo MB, Sanou M, Bisseye C, Kabore MI, Nebie YK, Kienou K, et al. Seroprevalence of human immunodeficiency virus, hepatitis B and C viruses and syphilis among blood donors in Koudougou (Burkina Faso) in 2009. Blood Transfus. 2011 Oct;9(4):419–24. doi: 10.2450/2011.0112-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nagalo BM, Bisseye C, Sanou M, Kienou K, Nebie YK, Kiba A, et al. Seroprevalence and incidence of transfusion-transmitted infectious diseases among blood donors from regional blood transfusion centres in Burkina Faso, West Africa. Trop Med Int Health. 2012 Feb;17(2):247–53. doi: 10.1111/j.1365-3156.2011.02902.x. [DOI] [PubMed] [Google Scholar]
- 9.Adjei AA, Kudzi W, Armah H, Adiku T, Amoah AG, Ansah J. Prevalence of antibodies to syphilis among blood donors in Accra, Ghana. Jpn J Infect Dis. 2003 Aug;56(4):165–7. [PubMed] [Google Scholar]
- 10.Noubiap JJ, Joko WY, Nansseu JR, Tene UG, Siaka C. Sero-epidemiology of human immunodeficiency virus, hepatitis B and C viruses, and syphilis infections among first-time blood donors in Edea, Cameroon. Int J Infect Dis. 2013 Jan;17(10):832–7. doi: 10.1016/j.ijid.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 11.Ophori EA, Atanunu O, Johnny EJ, Adu M. Seroprevalence of syphilis in apparently healthy students from a tertiary institution in Benin City, Nigeria. Jpn J Infect Dis. 2010 Nov;63(6):437–9. [PubMed] [Google Scholar]
- 12.Buseri FI, Muhibi MA, Jeremiah ZA. Sero-epidemiology of transfusion-transmissible infectious diseases among blood donors in Osogbo, south-west Nigeria. Blood Transfus. 2009 Oct;7(4):293–9. doi: 10.2450/2009.0071-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tessema B, Yismaw G, Kassu A, Amsalu A, Mulu A, Emmrich F, et al. Seroprevalence of HIV, HBV, HCV and syphilis infections among blood donors at Gondar University Teaching Hospital, Northwest Ethiopia: declining trends over a period of five years. BMC Infect Dis. 2010;10:111. doi: 10.1186/1471-2334-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feller L, Chandran R, Marnewick JC, Chikte UM, Gugushe TS, Meyerov R, et al. Syphilis in the context of HIV infection. Sadj. 2011 Jul;66(6):288–91. [PubMed] [Google Scholar]
- 15.Braunstein SL, Ingabire CM, Kestelyn E, Uwizera AU, Mwamarangwe L, Ntirushwa J, et al. High human immunodeficiency virus incidence in a cohort of Rwandan female sex workers. Sex Transm Dis. 2011 May;38(5):385–94. doi: 10.1097/olq.0b013e31820b8eba. [DOI] [PubMed] [Google Scholar]
- 16.WHO. YAWS. 2012 http://www.who.int/mediacentre/factsheets/fs316/en/index.html. Accessed 25th October 2013.
- 17.Manda SO, Lombard CJ, Mosala T. Divergent spatial patterns in the prevalence of the human immunodeficiency virus (HIV) and syphilis in South African pregnant women. Geospat Health. 2012 May;6(2):221–31. doi: 10.4081/gh.2012.140. [DOI] [PubMed] [Google Scholar]


