To the Editor: Venous thromboembolism (VTE), including both deep venous thrombosis (DVT) and pulmonary embolism (PE), is an important cause of morbidity and mortality in children. Although there is heightened awareness of this disease and its risk factors in children, there has been minimal evaluation of diagnostic tests (clinical prediction models, imaging modalities, and D-dimer assays) in children compared to adults.(1) ELISA based D-dimer assays have excellent sensitivity for the diagnosis of VTE in adults and this may permit the exclusion of VTE.(2) However, the utility of D-dimer assays for VTE in children has not been evaluated.
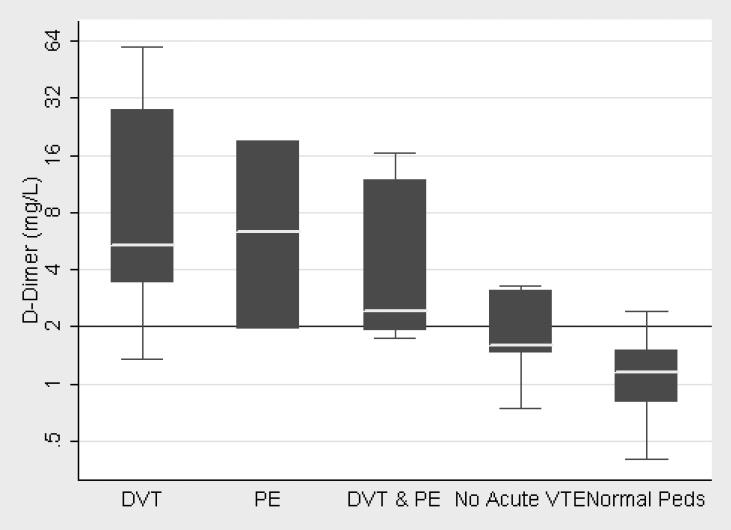
We performed a retrospective chart review of patients ≤21 years of age at Johns Hopkins Hospital with suspected VTE, imaging studies, and quantitative D-dimer. We used a discharge and billing database to identify patients and extracted information on potential risk factors, clinical findings, laboratory and imaging studies, and treatment. D-dimer was measured with an immunoturbidimetric assay on a Blood Coagulation System (BCS) analyzer (Advanced D-dimer; Dade-Behring) per the manufacturer's specifications. We identified 33 patients (20 male and 13 female) with diagnostic imaging studies and measurement of D-dimer within 72 hours. Twenty-six had acute VTE (15 DVT, 3 PE and 8 both], 6 with unchanged chronic VTE (5 DVT and 1 PE), and 1 without VTE (suspected PE). Most patients had multiple acquired risk factors for VTE with central venous catheters (54%), infections (40%), and immobility (42%) most frequent. D-dimer was significantly elevated in children with VTE (median 5.0, IQR 2.05-16.44) compared to children with negative evaluations for acute VTE (median 1.58, IQR 1.46-3.11, P<0.01) and pediatric controls [(median 1.2, IQR 0.8-1.5, P<0.0001) Figure 1]. There was minimal overlap between the groups with and without acute VTE. The normal range of D-dimer was similar in healthy adults (>40 years old, 0.43-2.24 mg/L) and children (2-12 years old, 0.4-2.27 mg/L).
Figure 1.
D-dimer (log-scale) by diagnosis and the normal range for children 2 – 12 years of age
We found that the D-dimer test was sensitive but only moderately specific for the diagnosis of VTE in children, and that the performance varied with the chosen cut-off. This assay is approved for the diagnosis of VTE in adults; the cut-off is 1.6 mg/L as the normal range is significantly higher than many D-dimer assays.(3) A D-dimer 1.75 mg/L was 92% sensitive (95% CI 75 – 99) and 57% specific (95% CI 18 – 90). Raising the threshold of the D-dimer to >2 mg/dl decreased the sensitivity to 77% (95% CI 56 – 91) while increasing the specificity to 71% (95% CI 29 – 96) for the diagnosis of VTE (Table 1). In a previous study of hospitalized adults from our institution,(4) the sensitivity of this test at a threshold of 2 mg/L was comparable (70% in adults versus 77% in children), however the specificity was considerably lower (42% in adults versus 71% in children). We calculated the area under the ROC [0.86 (95% CI 0.72-1.0)] to assess the performance of the D-dimer test to diagnose VTE. The greater the area under the curve, the better the performance of the diagnostic test with an area of 0.5 corresponding to a test that performs no better than flipping a coin.
Table 1.
Diagnostic Test Characteristics by Cut-Off (95% CI)
| D-Dimer | Sensitivity | Specificity | PPV | NPV | Area under ROC |
|---|---|---|---|---|---|
| ≥1.5 mg/dl | 96% (80-100) | 43% (10-82) | 86% (68-96) | 75% (19-99) | 0.86 (0.72-1.0) |
| ≥1.75 mg/dl | 92% (75-99) | 57% (18-90) | 89% (71-98) | 67% (22-96) | 0.86 (0.72-1.0) |
| ≥ 2 mg/dl | 77% (56-91) | 71% (29-96) | 91% (71-99) | 45% (17-77) | 0.86 (0.72-1.0) |
PPV indicates positive predictive value; NPV, negative predicitive value; ROC, receiver operating characteristic.
While the utility of the D-dimer testing has been studied extensively in adults, its performance for the diagnosis of VTE in pediatric patients has not been evaluated. A report of children with PE from a single institution described elevated levels of D-dimer in 6 of 10, but the normal range was not described.(5) In children with acute thrombotic events, elevated D-dimer was found to be predictive of poor outcome (persistent thrombosis, VTE recurrence, or post-thrombotic syndrome); however, measurement of D-dimer was semi-quantitative and its predictive value for the diagnosis of VTE was not reported.(6) In both adults and children, an elevated D-dimer after treatment of VTE appears to be a risk factor for recurrent thrombus.(6-8) To our knowledge, this is the first report that describes the sensitivity of D-dimer measurements for the diagnosis of VTE in children.
The incidence of VTE is significantly lower in children than adults, but perhaps even more challenging to diagnose. Compression ultrasonography of the lower extremities (sensitivity 91% and specificity 99%)(9) and MR venography (sensitivity 92% and specificity 95%)(10) have only been validated against the gold standard (contrast venography) in adults. D-dimer assays, in particular automated assays with rapid turn around times like the immunoturbidimetric assay used in this study, offer several advantages over other diagnostic modalities for VTE. They are relatively inexpensive and readily available in the outpatient and inpatient setting. A normal level in adults may potentially exclude VTE and avoid the need for expensive and time consuming imaging studies. Further prospective trials are necessary to validate our findings in children, as well as to address the utility of the D-dimer in selected subsets of pediatric patients.
Footnotes
The contributions of the individual authors to this work were as follows.
Designed research (JJS, PT, CMT,) performed research (JJS, PT, CMT, TK), analyzed data (JJS), and wrote the paper (JJS, CMT, TK).
REFERENCES
- 1.van Ommen CH, Peters M. Venous thromboembolic disease in childhood. Semin Thromb Hemost. 2003;29:391–404. doi: 10.1055/s-2003-42589. [DOI] [PubMed] [Google Scholar]
- 2.Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J, Kovacs G, Mitchell M, Lewandowski B, Kovacs MJ. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003;349:1227–1235. doi: 10.1056/NEJMoa023153. [DOI] [PubMed] [Google Scholar]
- 3.510(k) Summary for Advanced D-Dimer Assay. Office of in Vitro Diagnostic Devices: Food and Drug Administration; 2004. [Google Scholar]
- 4.Brotman DJ, Segal JB, Jani JT, Petty BG, Kickler TS. Limitations of D-dimer testing in unselected inpatients with suspected venous thromboembolism. Am J Med. 2003;114:276–282. doi: 10.1016/s0002-9343(02)01520-6. [DOI] [PubMed] [Google Scholar]
- 5.Rajpurkar M, Warrier I, Chitlur M, Sabo C, Frey MJ, Hollon W, Lusher J. Pulmonary embolism--experience at a single children's hospital. Thrombosis Research. 2007;119:699–703. doi: 10.1016/j.thromres.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 6.Goldenberg NA, Knapp-Clevenger R, Manco-Johnson MJ. Elevated plasma factor VIII and D-dimer levels as predictors of poor outcomes of thrombosis in children. N Engl J Med. 2004;351:1081–1088. doi: 10.1056/NEJMoa040161. [DOI] [PubMed] [Google Scholar]
- 7.Eichinger S, Minar E, Bialonczyk C, Hirschl M, Quehenberger P, Schneider B, Weltermann A, Wagner O, Kyrle PA. D-dimer levels and risk of recurrent venous thromboembolism. JAMA. 2003;290:1071–1074. doi: 10.1001/jama.290.8.1071. [DOI] [PubMed] [Google Scholar]
- 8.Palareti G, Legnani C, Cosmi B, Valdre L, Lunghi B, Bernardi F, Coccheri S. Predictive value of D-dimer test for recurrent venous thromboembolism after anticoagulation withdrawal in subjects with a previous idiopathic event and in carriers of congenital thrombophilia. Circulation. 2003;108:313–318. doi: 10.1161/01.CIR.0000079162.69615.0F. [DOI] [PubMed] [Google Scholar]
- 9.Lensing AW, Prandoni P, Brandjes D, Huisman PM, Vigo M, Tomasella G, Krekt J, Wouter Ten Cate J, Huisman MV, Buller HR. Detection of deep-vein thrombosis by real-time B- mode ultrasonography. N Engl J Med. 1989;320:342–345. doi: 10.1056/NEJM198902093200602. [DOI] [PubMed] [Google Scholar]
- 10.Sampson F, Goodacre S, Thomas S, van Beek E. The accuracy of MRI in diagnosis of suspected deep vein thrombosis: systematic review and meta-analysis. European Radiology. 2007;17:175–181. doi: 10.1007/s00330-006-0178-5. [DOI] [PubMed] [Google Scholar]