Abstract
Herniation of nucleus pulposus leading to leg pain is the commonest indication for lumbar spine surgery. However, there is no consensus when to stop conservative treatment and when to consider for surgery. A systematic review of literature was done to find a consensus on the issue of when should surgery be performed for herniation of nucleus pulposus in lumbar spine was conducted. Electronic database searches of Medline, Embase and Pubmed Central were performed to find articles relating to optimum time to operate in patients with herniation of nucleus pulposus in lumbar spine, published between January 1975 and 10 December 2012. The studies were independently screened by two reviewers. Disagreements between reviewers were settled at a consensus meeting. A scoring system based on research design, number of patients at final followup, percentage of patients at final followup, duration of followup, journal impact factor and annual citation index was devised to give weightage to Categorize (A, B or C) each of the articles. Twenty one studies fulfilled the criteria. Six studies were of retrospective design, 13 studies were of Prospective design and two studies were randomized controlled trials. The studies were categorized as: Two articles in category A (highest level of evidence), 12 articles in category B (moderate level of evidence) while seven articles in Category C (poor level of evidence). Category A studies conclude that duration of sciatica prior to surgery made no difference to the outcome of surgery in patients with herniation of nucleus pulposus in the lumbar spine. Ten out of 12 studies in Category B revealed that longer duration of sciatica before surgery leads to poor results while 2 studies conclude that duration of sciatica makes no difference to outcome. In category C, five studies conclude that longer duration of sciatica before surgery leads to poor outcome while two studies find no difference in outcome with regards to duration of sciatica. A qualitative and quantitative analysis was performed which favoured the consensus that longer duration of sciatica leads to poorer outcome. A systematic and critical review of literature revealed that long duration of preoperative leg pain lead to poor outcome for herniation of nucleus pulposus. Only a broad time frame (2-12 months) could be derived from the review of literature due to lack of high quality studies and variable and contrasting results of the existing studies. While surgery performed within six months was most commonly found to lead to good outcome of surgery, further studies are needed to prove this more conclusively. At this stage it is felt that time alone should not be the basis of recommending surgery and multiple other variables should be considered in a shared decision making process between the surgeon and the patient.
Keywords: Discectomy, lumbar, microdiscectomy, disc prolapse
INTRODUCTION
Sciatica due to herniation of nucleus pulposus of intervertebral disc is one of the commonest symptoms of patients seeking consultation in spine clinic. Lifetime incidence of sciatica varies from 13 to 40% respectively. The annual incidence of an episode of sciatica ranges from 1 to 5%.1,2,3 The natural course of intervertebral disc herniation is usually favorable. In a placebo-controlled double-blinded trial, Weber et al.4 found a significant reduction in pain within 4 weeks in 70% of patients with sciatica. The commonly used conservative measures for management of radicular pain due to herniated nucleus pulposus of the lumbar spine are rest, analgesics, physical therapy and transforaminal or epidural corticosteroid injections. On the other hand, incomplete resolution of symptoms or inadequate response to conservative measures may result in surgery in 10% of patients.5 Herniation of nucleus pulposus is the commonest indication for lumbar spine surgery.6,7,8 Absolute indications for discectomy include - neurological deficit causing weakness of functionally important muscles such as hip abductors, ankle dorsiflexors, ankle plantarflexors, cauda equina syndrome and progressive neurological deficit in spite of conservative treatment.5,9,10 The commoner relative indications for discectomy include persistent pain refractory to conservative care and pain that adversely affects the quality of life.11,12 Though surgery is commonly performed for these indications, there is no agreement on when conservative treatment should be abandoned and surgery considered. Moreover shared decision making, that involves the patient's desire to proceed with surgery or avoid it, always raises the clinically important question as to whether the outcome of surgery will be compromised if surgery is delayed and what is the critical time period during which surgery should be performed. Numerous studies have attempted to address the issue of optimum timing of surgery for herniation of nucleus pulposus with conflicting results.13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31 Hence, a systematic review of literature was conducted to try to find a consensus on the issue of when one should do surgery for herniation of nucleus pulposus in the lumbar spine.
MATERIALS AND METHODS
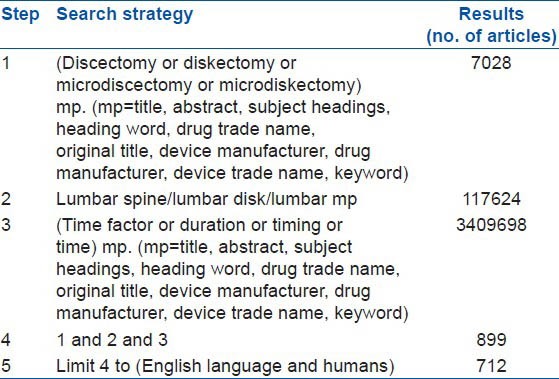
Electronic database searches of Medline, Embase and Pubmed Central were performed to find articles relating to optimum time to operate in patients with herniation of nucleus pulposus in the lumbar spine, published from January 1975 to 10 December 2012. This study was not a metaanalysis. Inclusion criteria were: Studies which had patients undergoing primary discectomy as the surgical procedure for herniation of nucleus pulposus and sciatica, studies which correlate duration of preoperative sciatica with regards to the outcome of discectomy, herniations of nucleus pulposus diagnosed clinically and radiologically (magnetic resonance imaging, Myelography, computed tomography scan) or seen intraoperatively, studies with a minimum of 30 patients at last followup, studies with a minimum followup of 6 months. Exclusion criteria were: Studies in languages other than English, nonhuman studies, economic evaluation studies, herniations of nucleus pulposus managed only conservatively or by fusion, studies specifically targeting special patient groups like adolescents, Workers compensation patients, patients more than 70 years old. Since operation techniques, diagnostic methods and indications for surgery have changed over a period of time, articles prior to 1975 were excluded. The keywords used were discectomy, diskectomy, microdiscectomy, microdiskectomy, lumbar vertebrae, lumbar spine, lumbar disk, lumbar, time factor, duration, timing, time. Search strategy used and the results are presented in Tables 1–3.
Table 1.
Medline search results
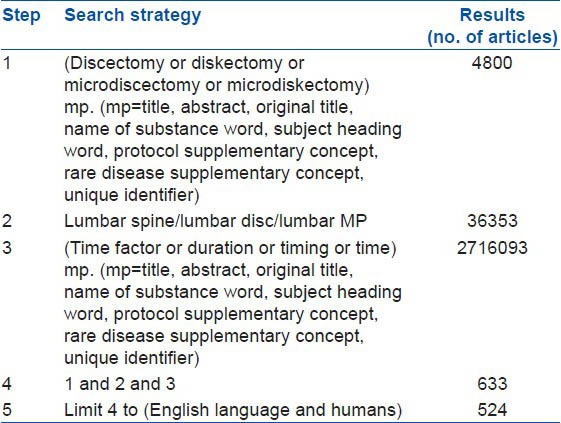
Table 3.
Pubmed Central search results
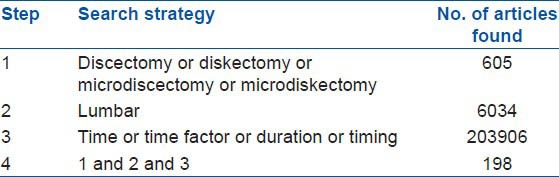
Table 2.
Embase search results
Five hundred and twenty four articles found in the Ovid Medline search were hand searched by their titles and 18 articles found to meet the inclusion and exclusion criteria. On reading the abstracts of these 18 articles, only 13 articles were found to meet the inclusion and exclusion criteria.
Seven hundred and twelve articles found in the Embase database search were hand searched by their titles and 22 articles were found to meet the inclusion and exclusion criteria. On reading the abstracts of these 22 articles, only 16 articles were found to meet the inclusion and exclusion criteria.
One hundred and ninety eight articles found by Pubmed Central search were hand searched by their titles and three articles were found to meet the inclusion and exclusion criteria. On reading the abstracts of these three articles, only two articles were found to meet the inclusion and exclusion criteria.
Thus, the search strategy resulted in 14 articles from Medline search, 16 articles from Embase search and two articles from Pubmed Central search. However, there were numerous common articles between the searches. Hence, combining the three searches, 17 articles were found. Since one of articles by Peul et al.32 was the interim result of another article33 by the same authors, the final article33 alone was included. Another study by Vrooman et al.34 was excluded as they studied time to surgery after onset of symptoms and did not evaluate the outcome of surgery. A study by Sutheerayongprasert et al.35 was excluded for similar reasons. Thus 14 articles remained from the search. The references within these 14 articles were searched and 11 more articles were found. On reading these 11 articles, two of the articles-by Peul et al. and Osterman et al.36,37 were excluded because in both these randomized controlled trials, preoperative duration of sciatica was constant (6-12 weeks) for all patients and hence not a variable used for prediction of outcome. Two more articles by Salenius and Laurent.38 and Dvorak et al.39 were excluded because the conclusion regarding when to operate was an opinion of the authors without any supporting data or statistical background mentioned in the articles. Thus, a total of 21 articles were found.
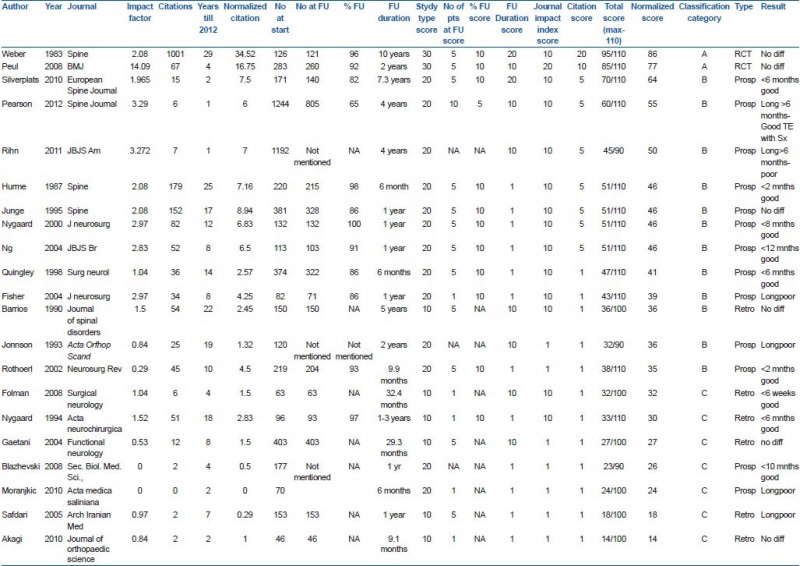
The studies were independently screened by two reviewers. Disagreements between reviewers were settled at a consensus meeting. The type of research design, number of patients at the start of the study and at final followup, percentage of patients at final followup, duration of followup, impact factor of journals in which the articles were published and annual citation index for each article were noted in tabular form for comparison. Annual citation index was calculated as the number of citations of the article until December 2012 divided by the difference between the year of publication of the article and 2012. A scoring system based on research design, number of patients at final followup, percentage of patients at final followup, duration of followup, journal impact factor and annual citation index was devised to give weight age to each of the articles. According to the research design, 30 points were allotted to Randomized controlled trials, 20 points to prospective studies and ten points to retrospective studies. Studies with more than 500 patients received ten points, 100-500 patients received five points and <100 patients received one point. Considering the percentage of patients remaining at followup, studies with more than 80% followup received ten points, 60-80% followup received five points and <60% followup received one point. Depending on the duration of followup, articles with more than 5 years followup duration received 20 points, those with 2-5 years followup received ten points and those articles with <2 years followup received one point. According to the impact factor of the journals for the year 2012, articles in journals with impact factor more than four received 20 points, those in journals with impact index one to four received ten points and those in journals with impact index less than one received one point. As per the annual citation index of the articles, articles with citation index more than 20 received 20 points, those with citation index more than 10-20 received ten points, those with citation index more than five to ten received five points and those with citation index five or less than five received one point. This scoring system is shown in Table 4.
Table 4.
Scoring system for articles
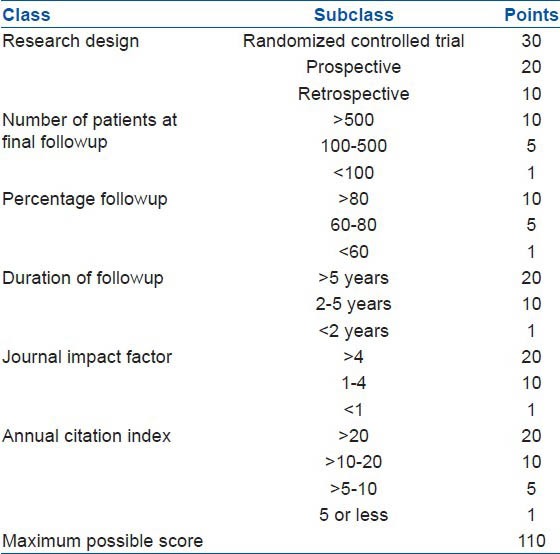
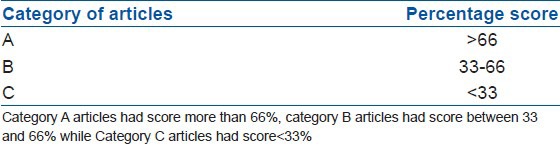
A maximum of 110 points was possible for every article. However, some of the prospective studies did not mention the number of patients at final followup (and hence the percentage followup). Furthermore, for most retrospective studies, number of patients at followup was available without mention of a number of patients at the start of study and hence percentage followup was not possible. Hence, the maximum possible scores possible were 90 points, 100 points or 110 points. To normalize the total scores of articles for comparison, the percentage scores of the maximum possible scores were found. The articles were divided into three categories according to their percentage scores [Table 5].
Table 5.
Category of articles as per the percentage score
RESULTS
A total of 21 studies which met the inclusion criteria were found. Six studies were of Retrospective design, 13 studies were of Prospective design and two studies were Randomized controlled trials. At the initiation of the study, five studies had <100 patients, 14 studies had between 100 and 500 patients while two studies had more than 500 patients. At followup, five studies had <100 patients, 12 studies had between 100 and 500 patients, one study had more than 500 patients while three studies had not mentioned the number of patients at followup. According to the percentage of patients at final followup, 11 studies had more than 80% followup, one study had between 60-80% followup, for eight retrospective studies percentage followup was not applicable while for three studies calculation of percentage followup was not possible due to unavailability of data of the number of patients at final followup. Considering the duration of followup, 11 studies had followup of <2 years, eight studies had 2-5 years of followup while two studies had more than 5 years of followup. Considering Journal impact index, seven articles belonged to journals with impact index less than one, 13 articles belonged to journals with impact index between one and four while one article belonged to Journal (JAMA) with impact index more than four. As per the citation index, 12 articles had citation index of five or less, seven articles had citation index in the range more than 5-10 while there was one article each in the range more than 10-20 and more than 20. A detailed analysis of the studies is shown in Table 6. The raw data is presented as Appendix 1.
Table 6.
Results

Two articles31,33 in Category A (highest level of evidence), 12 articles13,15,19,20,21,23,24,26,27,28,29,30 in Category B (moderate level of evidence) while seven articles14,16,17,18,22,25,40 in Category C (poor level of evidence) were found. Both the Category A studies conclude that duration of sciatica prior to surgery makes no difference to the outcome of surgery in patients with herniation of nucleus pulposus in the lumbar spine.
Ten out of 12 studies in Category B feel longer duration of sciatica before surgery leads to poorer results while 2 studies conclude that duration of sciatica makes no difference to the outcome.
In Category C studies, five studies conclude that longer duration of sciatica before surgery leads to poorer outcome while two studies find no difference in the outcome with regards to the duration of sciatica.
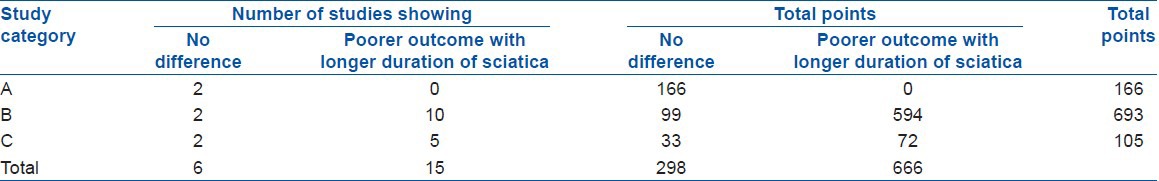
Thus conflicting results in our review were found as regards timing of surgery after herniation of nucleus pulposus in the lumbar spine. A qualitative and quantitative analysis was performed to arrive at a consensus. In the Quantitative analysis, the total number of points of studies (as determined by our scoring system) across all categories showing no difference in the outcome with the duration of sciatica was compared with those showing poorer outcome with increased duration of sciatica. As can be seen in Table 7, the results showed more than twice the number of points of studies showing poorer outcome with longer duration of sciatica (666 points) when compared to those showing no difference in the outcome with time (298 points). Thus, the quantitative analysis favored the consensus that longer duration of sciatica leads to poorer outcome.
Table 7.
Quantitative analysis of results
A detailed qualitative analysis of the studies was also performed which consisted of attempting to find limitations of studies with seemingly high level of evidence. In randomized controlled trail conducted by Weber,31 the primary conclusion was that the long term outcomes of conservative treatment versus surgery are similar for patients with herniation of nucleus pulposus of the lumbar spine. Weber31 also mentions that duration of sciatica makes no difference to the outcome. However, Weber31 has only compared groups of patients having different durations of sciatica with the outcome in each group. Since multivariate analysis has not been performed, interactions amongst variables have been disregarded. Furthermore, randomization does not apply to the conclusions done for the duration of sciatica. Hence, less weightage is given by us to the conclusion regarding the timing of surgery in Weber's study.
In the randomized controlled trial by Peul et al.33 the conclusion is that 2 year outcomes of conservative treatment versus surgery are similar in patients with herniation of nucleus pulposus of lumbar spine. The duration of sciatica for all the patients in the study is 6-12 weeks. Hence, there is not much variation in the duration of sciatica in this study. Also, Peul et al.33 have 40% crossover rate in the conservative group. This decreases the validity of their conclusions especially that related to the outcome of treatment with respect to the duration of sciatica.
Studies in Category C14,16,17,18,22,25,40 are of an inferior quality as determined by our scoring system. Hence, the results of these studies were not considered. Majority of studies in Category B (ten out of 12) state that longer duration of sciatica leads to poorer outcome of intervention. A recent prospective study by Rihn et al.(Spine Patient Outcomes Research Trail [SPORT])28 concludes that patients with symptom duration of 6 months or less had better outcomes (with conservative or operative treatment) compared to patients with symptoms duration of more than 6 months. However, there were significant baseline differences in the two groups. These differences included the type of herniation of nucleus pulposus, the presence of neurological deficit, operative time, percentage of patients who reported depression, percentage of patients who perceived that the problem was getting worse and percentage of patients who had a preference for surgical treatment. Pearson et al.26 conducted an as treated analysis of combined prospective randomized controlled trial and observational cohort study of intervertebral herniation of nucleus pulposus in SPORT. The Treatment Effect (TE) of surgery was defined as: TE = Change in Oswestry Disability Indexsurgery - Change in Oswestry Disability Indexnonoperative. They determined the modifiers of TE of surgery for intervertebral herniation of nucleus pulposus using subgroup analysis of 37 baseline variables. In minimally adjusted univariate analysis, they found longer duration of symptoms (>6 months) was one of the factors associated with a greater TE with surgery (P = 0.09) suggesting that patients with longer duration of symptoms (>6 months) had a better outcome with surgery compared to nonoperative treatment. However, in multivariate analysis, they found only marital status, presence or absence of joint pain and symptom trend as the three independent treatment modifiers. Silverplats et al.30 performed a prospective study of 171 patients undergoing lumbar discectomy for single level herniation of nucleus pulposus. They found duration of leg pain of <6 months and duration of sick leave of <2 months was related to better objective and subjective outcome in the short term (2 years) and long term followup (5-10 years; mean 7.3 years).
Hurme et al.19 conducted a prospective study of 357 consecutive patients with herniation of nucleus pulposus of the lumbar spine, younger than 55 years of age, who had not retired and who had no previous back surgery. Using stepwise regression analysis, they found long duration of preoperative sciatica (more than 2 months) was a predictor of poor results. Quigley et al.27 performed a prospective study of 374 patients undergoing unilateral single-level microdiscectomies. Using univariate and multivariate logistical regression analysis, they found Workman's Compensation claim and length of symptoms – more than 6 months (P < 0.0001 for both) affect the surgical outcome. However, the duration of followup for the study was short (6 months). Nygaard et al.24 performed a prospective cohort study for 132 patients who underwent microdiscecomy for single level primary herniation of nucleus pulposus in the lumbar spine. Of the various factors studied as predictors of outcome using multiple linear regression analysis, they found duration of leg pain and duration of sick leave as statistically significant. Using univariate analysis, they found that leg pain of more than 8 months duration increased risk of poor clinical results. Rothoerl et al.29 performed a prospective consecutive study of 219 patients undergoing primary conventional discectomy for monosegmental herniation of nucleus pulposus in lumbar spine. They found statistically significant worse outcomes in patients suffering from leg pain or sensory deficit for more than 2 months compared to those suffering for <2 months. Hence they recommend conservative care for up to 2 months for herniation of nucleus pulposus in lumbar spine. Ng et al.23 prospectively studied 113 patients with single level herniation of nucleus pulposus in lumbar spine undergoing primary discectomy by single surgeon. They found a statistically significant increased risk of poor outcome for Oswestry Disability Index and Low Back Pain Outcome Score (but not for visual analog scale) if the duration of sciatica exceeded 12 months prior to surgery.
Two of the studies15,20 found that longer duration of symptoms were associated with poor outcome but did not give the time limit. Jönsson20 performed a prospective consecutive study of 120 patients undergoing discectomy for single level herniation of nucleus pulposus in lumbar spine. The mean preoperative duration of leg pain was 13 months. Using Mann Whitney test, they found prolonged duration of symptoms were associated with poor outcomes. Using dose-response analysis of the time factors, they found that the risk of having a poor outcome increased continuously with time; however, it was not possible for them to identify a threshold value. Fisher et al.15 studied a prospective cohort of 82 patients who underwent elective lumbar discectomy and assessed health-related quality of life (HRQOL) and the appropriateness of surgery. They found that the duration of time between symptom onset and surgery inversely influenced HRQOL.
Two studies13,21 found no difference in the outcome with regards to duration of sciatica. Barrios et al.13 conducted a 5 year retrospective analysis of 150 patients with low back pain and/or radicular pain operated by discectomy after 4 weeks of failed conservative treatment. Using multivariate stepwise regression analysis and Chi square test with Yates correction, they did not find significant correlation between duration of symptoms (less than or more than 6 months) and outcome of surgery. Junge et al.21 performed a multicentric prospective study of 381 patients undergoing discectomy for herniation of nucleus pulposus in lumbar spine with the aim to find out good and bad predictors of surgery. Using multivariate discriminate analysis, they found that duration of sciatica did not have any significant effect on the outcome of surgery.
DISCUSSION
Herniation of nucleus pulposus in lumbar spine can give rise to radicular pain sciatica, the duration of which varies from days to weeks to months, sometimes years. Usually conservative treatment is recommended for sciatica during the initial acute phase with the hope that pain will subside with resorption of herniated nucleus pulposus. However, it not clear as to when surgery should be considered to overcome such pain. When a noxious stimulus is prolonged, it leads to changes in the neural system which maintains pain even after the stimulus is removed.41 Central hypersensitivity can maintain hyperalgesia without inputs from the injured peripheral tissue.42 Following a noxious stimulation like herniation of nucleus pulposus, there is sensitization of neurons in dorsal horn of spinal cord and other areas in the somatosensory pathway reflected by increased spontaneous activity, reduced thresholds or increased responsivity to afferent inputs, prolonged after discharges to repeated stimulation, and expansion of the peripheral receptive field of dorsal horn neurons.41 It has been shown that a nerve constriction injury produces profound changes in spinal cord physiology, function and metabolic activity.43,44,45 Clinical neurosurgery studies reveal that neurons in the somatosensory thalamus of patients with neuropathic pain display abnormal bursting activity, high spontaneous firing rates and evoked responses to stimulation of body areas which normally do not activate these neurons.46,47,48,49
Recently, Jancalek et al.50 found that regenerative effects of decompression on the myelinated axons were more pronounced after 1 week of compression when compared to after 5 weeks of compression in rat spines. Hence, they recommend early surgical decompression after failure of 2-3 months of conservative treatment to prevent irreversible morphological changes in the nerve root and worse clinical outcome.
There is immunological evidence of development of antiglycospingolipid antibodies in patients with sciatica.51 There are many studies to evaluate the role of inflammatory markers in acute disc herniation. Phospholipase A2,52,53,54,55 nitric oxide,56 interleukin (IL)-857 IL-658 have been shown to play a role in experimental studies. We could not find similar studies evaluating role of inflammatory markers in chronic sciatica.
The qualitative as well as the quantitative analysis of the studies in our review showed that longer duration of sciatica leads to poorer outcome with surgery. However, it should be noted that this is not a metaanalysis. In Category B studies, though majority of studies mention that longer duration of leg pain leads to poorer outcome, there is no consensus on the issue of how long!! While four studies find surgery at 6 months as the time limit for good results versus poor results, one study finds 8 months, another one finds 12 months, two studies find 2 months as the time limit and two studies fail to find a time limit. However, after a systematic study of the suggested time durations, a recommendation can be made that surgery should be performed between 2 and 12 months of onset of sciatica. Only a broad time frame (2-12 months) could be derived from the review of literature due to lack of high quality studies and variable and contrasting results of the existing studies. However, this broad time frame needs to be qualified within limits of acceptance. It could be definitively said that surgery should not be performed before 2 months and after 12 months in patients with herniation of nucleus pulposus of lumbar spine, however again the research question was not when “not” to perform surgery. This ultimately remains a shared decision making between the surgeon and patient, our current work provides guidelines for discussion with patients in the preoperative period. Surgery done prior to 2 months from the onset of sciatica is too early as the symptoms might resolve by the 2 month mark while a surgery performed after 12 months almost always leads to poorer outcome with patients suffering from chronic neuropathic pain and sensory disturbances in spite of removal of painful stimulus. This is well supported and reasoned by clinical and experimental research.
Since most of the studies performed a multivariate analysis, there were many other variables found affecting the outcome. Variables which predicted poor outcome were -long duration of sick leave, low education status, age more than 40 years, single or divorced marital status, preoperative presence and duration of neurological deficit, preoperative chronic low back pain, multiple sites of pain in the body, presence of joint pains, reduced mobility preoperatively, patients under Worker's compensation, high preoperative pain/functional disability scores, regular consumption of analgesics and intraoperative complications.
A critical and systematic review of the literature revealed that long duration of preoperative leg pain was found to lead to poor outcome. Though surgery performed within 6 months was most commonly found to lead to good outcome of surgery, further studies are needed to prove this more conclusively. At this stage it is felt that time alone should not be the basis of recommending surgery, hence the practice of telling patients that they need “urgent” surgery for pain due to herniation of nucleus pulposus has no scientific basis.
Appendix 1
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Frymoyer JW. Back pain and sciatica. N Engl J Med. 1988;318:291–300. doi: 10.1056/NEJM198802043180506. [DOI] [PubMed] [Google Scholar]
- 2.Frymoyer JW. Lumbar disk disease: Epidemiology. Instr Course Lect. 1992;41:217–23. [PubMed] [Google Scholar]
- 3.Stafford MA, Peng P, Hill DA. Sciatica: A review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br J Anaesth. 2007;99:461–73. doi: 10.1093/bja/aem238. [DOI] [PubMed] [Google Scholar]
- 4.Weber H, Holme I, Amlie E. The natural course of acute sciatica with nerve root symptoms in a double-blind placebo-controlled trial evaluating the effect of piroxicam. Spine (Phila Pa 1976) 1993;18:1433–8. [PubMed] [Google Scholar]
- 5.Saal JA, Saal JS. Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy. An outcome study. Spine (Phila Pa 1976) 1989;14:431–7. doi: 10.1097/00007632-198904000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Hasue M, Fujiwara M. Epidemiologic and clinical studies of long term prognosis of low-back pain and sciatica. Spine (Phila Pa 1976) 1979;4:150–5. doi: 10.1097/00007632-197903000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G. An international comparison of back surgery rates. Spine (Phila Pa 1976) 1994;19:1201–6. doi: 10.1097/00007632-199405310-00001. [DOI] [PubMed] [Google Scholar]
- 8.Weinstein J. Chicago IL: American Hospital Association Press; 2000. Dartmouth Atlas of Musculoskeletal Health Care. [PubMed] [Google Scholar]
- 9.Komori H, Shinomiya K, Nakai O, Yamaura I, Takeda S, Furuya K. The natural history of herniated nucleus pulposus with radiculopathy. Spine (Phila Pa 1976) 1996;21:225–9. doi: 10.1097/00007632-199601150-00013. [DOI] [PubMed] [Google Scholar]
- 10.Splendiani A, Puglielli E, De Amicis R, Barile A, Masciocchi C, Gallucci M. Spontaneous resolution of lumbar disk herniation: Predictive signs for prognostic evaluation. Neuroradiology. 2004;46:916–22. doi: 10.1007/s00234-004-1232-0. [DOI] [PubMed] [Google Scholar]
- 11.Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, et al. Surgical vs nonoperative treatment for lumbar disk herniation: The Spine Patient Outcomes Research Trial (SPORT): A randomized trial. JAMA. 2006;296:2441–50. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the maine lumbar spine study. Spine (Phila Pa 1976) 2005;30:927–35. doi: 10.1097/01.brs.0000158954.68522.2a. [DOI] [PubMed] [Google Scholar]
- 13.Barrios C, Ahmed M, Arrotegui JI, Björnsson A. Clinical factors predicting outcome after surgery for herniated lumbar disc: An epidemiological multivariate analysis. J Spinal Disord. 1990;3:205–9. [PubMed] [Google Scholar]
- 14.Blazhevski B, Filipche V, Cvetanovski V, Simonovska N. Predictive value of the duration of sciatica for lumbar discectomy. Prilozi. 2008;29:325–35. [PubMed] [Google Scholar]
- 15.Fisher C, Noonan V, Bishop P, Boyd M, Fairholm D, Wing P, et al. Outcome evaluation of the operative management of lumbar disc herniation causing sciatica. J Neurosurg. 2004;100:317–24. doi: 10.3171/spi.2004.100.4.0317. [DOI] [PubMed] [Google Scholar]
- 16.Folman Y, Shabat S, Catz A, Gepstein R. Late results of surgery for herniated lumbar disk as related to duration of preoperative symptoms and type of herniation. Surg Neurol. 2008;70:398–401. doi: 10.1016/j.surneu.2007.04.022. [DOI] [PubMed] [Google Scholar]
- 17.Gaetani P, Aimar E, Panella L, Debernardi A, Tancioni F, Rodriguez y, Baena R. Surgery for herniated lumbar disc disease: Factors influencing outcome measures. An analysis of 403 cases. Funct Neurol. 2004;19:43–9. [PubMed] [Google Scholar]
- 18.Safari GH, Nayebaghaie H, Azhari SJ, Shabehpour M. Prognostic value of preoperative sciatalgia in lumbar disc surgery. Arch Iranian Med. 2005;8:300–3. [Google Scholar]
- 19.Hurme M, Alaranta H. Factors predicting the result of surgery for lumbar intervertebral disc herniation. Spine (Phila Pa 1976) 1987;12:933–8. doi: 10.1097/00007632-198711000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Jönsson B. Patient-related factors predicting the outcome of decompressive surgery. Acta Orthop Scand Suppl. 1993;251:69–70. doi: 10.3109/17453679309160123. [DOI] [PubMed] [Google Scholar]
- 21.Junge A, Dvorak J, Ahrens S. Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine (Phila Pa 1976) 1995;20:460–8. doi: 10.1097/00007632-199502001-00009. [DOI] [PubMed] [Google Scholar]
- 22.Moranjkiæ M, Ercegovic Z, Hodzic M, Brikic H. Outcome prediction in lumbar disc herniation surgery. Acta Med Sal. 2010;39:75–80. [Google Scholar]
- 23.Ng LC, Sell P. Predictive value of the duration of sciatica for lumbar discectomy. A prospective cohort study. J Bone Joint Surg Br. 2004;86:546–9. [PubMed] [Google Scholar]
- 24.Nygaard OP, Kloster R, Solberg T. Duration of leg pain as a predictor of outcome after surgery for lumbar disc herniation: A prospective cohort study with 1-year followup. J Neurosurg. 2000;92:131–4. doi: 10.3171/spi.2000.92.2.0131. [DOI] [PubMed] [Google Scholar]
- 25.Nygaard OP, Romner B, Trumpy JH. Duration of symptoms as a predictor of outcome after lumbar disc surgery. Acta Neurochir (Wien) 1994;128:53–6. doi: 10.1007/BF01400653. [DOI] [PubMed] [Google Scholar]
- 26.Pearson A, Lurie J, Tosteson T, Zhao W, Abdu W, Weinstein J. Who should have surgery for spinal stenosis? Treatment effect predictors in SPORT. Spine (Phila Pa 1976) 2012;37:1792–802. doi: 10.1097/BRS.0b013e3182634b04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quigley MR, Bost J, Maroon JC, Elrifai A, Panahandeh M. Outcome after microdiscectomy: Results of a prospective single institutional study. Surg Neurol. 1998;49:263–7. doi: 10.1016/s0090-3019(97)00448-5. [DOI] [PubMed] [Google Scholar]
- 28.Rihn JA, Hilibrand AS, Radcliff K, Kurd M, Lurie J, Blood E, et al. Duration of symptoms resulting from lumbar disc herniation: Effect on treatment outcomes: Analysis of the Spine Patient Outcomes Research Trial (SPORT) J Bone Joint Surg Am. 2011;93:1906–14. doi: 10.2106/JBJS.J.00878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rothoerl RD, Woertgen C, Brawanski A. When should conservative treatment for lumbar disc herniation be ceased and surgery considered? Neurosurg Rev. 2002;25:162–5. doi: 10.1007/s101430100184. [DOI] [PubMed] [Google Scholar]
- 30.Silverplats K, Lind B, Zoëga B, Halldin K, Rutberg L, Gellerstedt M, et al. Clinical factors of importance for outcome after lumbar disc herniation surgery: Long term followup. Eur Spine J. 2010;19:1459–67. doi: 10.1007/s00586-010-1433-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976) 1983;8:131–40. [PubMed] [Google Scholar]
- 32.Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356:2245–56. doi: 10.1056/NEJMoa064039. [DOI] [PubMed] [Google Scholar]
- 33.Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW Leiden-The Hague Spine Intervention Prognostic Study Group. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: Two year results of a randomised controlled trial. BMJ. 2008;336:1355–8. doi: 10.1136/bmj.a143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vroomen PC, de Krom MC, Knottnerus JA. Predicting the outcome of sciatica at short-term followup. Br J Gen Pract. 2002;52:119–23. [PMC free article] [PubMed] [Google Scholar]
- 35.Sutheerayongprasert C, Paiboonsirijit S, Kuansongtham V, Anuraklekha S, Hiranyasthiti N, Neti S. Factors predicting failure of conservative treatment in lumbar-disc herniation. J Med Assoc Thai. 2012;95:674–80. [PubMed] [Google Scholar]
- 36.Peul WC, Arts MP, Brand R, Koes BW. Timing of surgery for sciatica: Subgroup analysis alongside a randomized trial. Eur Spine J. 2009;18:538–45. doi: 10.1007/s00586-008-0867-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Osterman H, Seitsalo S, Karppinen J, Malmivaara A. Effectiveness of microdiscectomy for lumbar disc herniation: A randomized controlled trial with 2 years of followup. Spine (Phila Pa 1976) 2006;31:2409–14. doi: 10.1097/01.brs.0000239178.08796.52. [DOI] [PubMed] [Google Scholar]
- 38.Salenius P, Laurent LE. Results of operative treatment of lumbar disc herniation. A survey of 886 patients. Acta Orthop Scand. 1977;48:630–4. doi: 10.3109/17453677708994809. [DOI] [PubMed] [Google Scholar]
- 39.Dvorak J, Gauchat MH, Valach L. The outcome of surgery for lumbar disc herniation. I. A 4-17 years’ followup with emphasis on somatic aspects. Spine (Phila Pa 1976) 1988;13:1418–22. doi: 10.1097/00007632-198812000-00015. [DOI] [PubMed] [Google Scholar]
- 40.Akagi R, Aoki Y, Ikeda Y, Nakajima F, Ohtori S, Takahashi K, et al. Comparison of early and late surgical intervention for lumbar disc herniation: Is earlier better? J Orthop Sci. 2010;15:294–8. doi: 10.1007/s00776-010-1457-1. [DOI] [PubMed] [Google Scholar]
- 41.Coderre TJ, Katz J, Vaccarino AL, Melzack R. Contribution of central neuroplasticity to pathological pain: Review of clinical and experimental evidence. Pain. 1993;52:259–85. doi: 10.1016/0304-3959(93)90161-H. [DOI] [PubMed] [Google Scholar]
- 42.Torebjörk HE, Lundberg LE, LaMotte RH. Central changes in processing of mechanoreceptive input in capsaicin-induced secondary hyperalgesia in humans. J Physiol. 1992;448:765–80. doi: 10.1113/jphysiol.1992.sp019069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cameron AA, Cliffer KD, Dougherty PM, Willis WD, Carlton SM. Changes in lectin, GAP-43 and neuropeptide staining in the rat superficial dorsal horn following experimental peripheral neuropathy. Neurosci Lett. 1991;131:249–52. doi: 10.1016/0304-3940(91)90625-4. [DOI] [PubMed] [Google Scholar]
- 44.Sugimoto T, Bennett GJ, Kajander KC. Transsynaptic degeneration in the superficial dorsal horn after sciatic nerve injury: Effects of a chronic constriction injury, transection, and strychnine. Pain. 1990;42:205–13. doi: 10.1016/0304-3959(90)91164-E. [DOI] [PubMed] [Google Scholar]
- 45.Mao J, Price DD, Coghill RC, Mayer DJ, Hayes RL. Spatial patterns of spinal cord [14C]-2-deoxyglucose metabolic activity in a rat model of painful peripheral mononeuropathy. Pain. 1992;50:89–100. doi: 10.1016/0304-3959(92)90116-S. [DOI] [PubMed] [Google Scholar]
- 46.Gorecki J, Hirayama T, Dostrovsky JO, Tasker RR, Lenz FA. Thalamic stimulation and recording in patients with deafferentation and central pain. Stereotact Funct Neurosurg. 1989;52:219–26. doi: 10.1159/000099504. [DOI] [PubMed] [Google Scholar]
- 47.Hirayama T, Dostrovsky JO, Gorecki J, Tasker RR, Lenz FA. Recordings of abnormal activity in patients with deafferentation and central pain. Stereotact Funct Neurosurg. 1989;52:120–6. doi: 10.1159/000099492. [DOI] [PubMed] [Google Scholar]
- 48.Lenz FA, Kwan HC, Dostrovsky JO, Tasker RR. Characteristics of the bursting pattern of action potentials that occurs in the thalamus of patients with central pain. Brain Res. 1989;496:357–60. doi: 10.1016/0006-8993(89)91088-3. [DOI] [PubMed] [Google Scholar]
- 49.Rinaldi PC, Young RF, Albe-Fessard D, Chodakiewitz J. Spontaneous neuronal hyperactivity in the medial and intralaminar thalamic nuclei of patients with deafferentation pain. J Neurosurg. 1991;74:415–21. doi: 10.3171/jns.1991.74.3.0415. [DOI] [PubMed] [Google Scholar]
- 50.Jancalek R, Dubovy P. An experimental animal model of spinal root compression syndrome: An analysis of morphological changes of myelinated axons during compression radiculopathy and after decompression. Exp Brain Res. 2007;179:111–9. doi: 10.1007/s00221-006-0771-5. [DOI] [PubMed] [Google Scholar]
- 51.Brisby H, Balagué F, Schafer D, Sheikhzadeh A, Lekman A, Nordin M, et al. Glycosphingolipid antibodies in serum in patients with sciatica. Spine (Phila Pa 1976) 2002;27:380–6. doi: 10.1097/00007632-200202150-00011. [DOI] [PubMed] [Google Scholar]
- 52.Chen C, Cavanaugh JM, Ozaktay AC, Kallakuri S, King AI. Effects of phospholipase A2 on lumbar nerve root structure and function. Spine (Phila Pa 1976) 1997;22:1057–64. doi: 10.1097/00007632-199705150-00002. [DOI] [PubMed] [Google Scholar]
- 53.Franson RC, Saal JS, Saal JA. Human disc phospholipase A2 is inflammatory. Spine (Phila Pa 1976) 1992;17:S129–32. doi: 10.1097/00007632-199206001-00011. [DOI] [PubMed] [Google Scholar]
- 54.Olmarker K, Blomquist J, Strömberg J, Nannmark U, Thomsen P, Rydevik B. Inflammatogenic properties of nucleus pulposus. Spine (Phila Pa 1976) 1995;20:665–9. doi: 10.1097/00007632-199503150-00006. [DOI] [PubMed] [Google Scholar]
- 55.Saal JS, Franson RC, Dobrow R, Saal JA, White AH, Goldthwaite N. High levels of inflammatory phospholipase A2 activity in lumbar disc herniations. Spine (Phila Pa 1976) 1990;15:674–8. doi: 10.1097/00007632-199007000-00011. [DOI] [PubMed] [Google Scholar]
- 56.Brisby H, Olmarker K, Rosengren L, Cederlund CG, Rydevik B. Markers of nerve tissue injury in the cerebrospinal fluid in patients with lumbar disc herniation and sciatica. Spine (Phila Pa 1976) 1999;24:742–6. doi: 10.1097/00007632-199904150-00003. [DOI] [PubMed] [Google Scholar]
- 57.Brisby H, Byröd G, Olmarker K, Miller VM, Aoki Y, Rydevik B. Nitric oxide as a mediator of nucleus pulposus-induced effects on spinal nerve roots. J Orthop Res. 2000;18:815–20. doi: 10.1002/jor.1100180520. [DOI] [PubMed] [Google Scholar]
- 58.Takahashi H, Suguro T, Okazima Y, Motegi M, Okada Y, Kakiuchi T. Inflammatory cytokines in the herniated disc of the lumbar spine. Spine (Phila Pa 1976) 1996;21:218–24. doi: 10.1097/00007632-199601150-00011. [DOI] [PubMed] [Google Scholar]


