Abstract
Spine of the child has unique anatomy and growth potential to grow to adult size. Tuberculosis (TB) spine results in bone loss as well as disturbed growth potential, hence spinal deformities may progress as the child grows. The growth potential is also disturbed when the disease focus is surgically intervened. Surgery is indicated for complications such as deformity, neurological deficit, instability, huge abscess, diagnostic dilemma and in suspected drug resistance to mycobacterium tuberculosis. The child on antitubercular treatment needs to be periodically evaluated for weight gain and drug dosages need to be adjusted accordingly. The severe progressive kyphotic deformity should be surgically corrected. Mild to moderate cases should be followed up until maturity to observe progression/improvement of spinal deformity. The surgical correction of kyphotic deformity in active disease is less hazardous than in a healed kyphosis. The internal kyphectomy by extra pleural approach allows adequate removal of internal salient in paraplegic patients with healed kyphotic deformity.
Keywords: Kyphus correction, pediatric tuberculosis, osteoarticular tuberculosis, tuberculosis of spine
DEVELOPMENT OF VERTEBRAL COLUMN
The spine of a child is not a replica of a miniature adult. It has a unique anatomy and has growth potential to grow from child to adult size, hence it needs special considerations.1
The vertebrae develop from one ossification center for the vertebral body and two centers for the lateral masses. Each center has a direct blood supply. These centers have a central nucleus of bone with surrounding cartilage. There are secondary centers on the tip of the spinous process, facets, transverse process and an apophyseal ring at both superior and inferior end of the vertebral body. The younger the child, smaller is the size of the spine. The intervertebral disc and annulus are further expandable.2
The vertebral column grows both in length and width from intrauterine life to adult size. In utero the spine grows at a much accelerated rate followed by an increased rate immediately after birth. It grows at a steady rate from 2 years to 10 years of age. During the prepubertal growth phase it grows at an increased rate once again.1 Any coexisting spinal deformity also progresses during the growth phase. The longitudinal growth of thoracic and lumbar vertebrae occurs at a rate of 0.8-1.1 mm/year.3 The thoracic disc grows 0.2-0.6 mm/year and the lumbar disc grows 0.3-0.8 mm/year.4,5 Each vertebral ring apophysis adds to the axial column growth of 0.5 mm/year, thus every vertebra contributes on an average 1 mm growth per year. This growth is at a faster pace during the accelerated growth phase, i.e., first 2 years and prepubertal phase.
DEVELOPMENT OF KYPHOSIS
The vertebral growth is controlled by loading of the vertebral bodies.6,7 The growth is retarded when the ring apophysis is loaded while reduction in loading (pressure) accelerates growth. The growth occurs symmetrically when the ring apophysis is uniformly loaded. The asymmetrical loading of the ring apophysis affects the growth potential differentially and some part adds to the growth more than the other, consequently leading to the development and progression of the spinal deformity. In a deformed spine, the ring apophysis is loaded asymmetrically hence the growth either adds to the deformity or corrects the spinal deformity depending on the type of loading on the vertebral body. When one part of the ring apophysis is loaded more than the other part of the same apophysis, the part that is loaded will have a suppressed growth and the remaining part will grow at a faster pace thus adding to the deformity in one or more planes. The spinal growth that occurs in a kyphotic spine depends on the severity of kyphotic deformity and type of loading.
The proximal vertebrae stabilize on distal vertebral bodies in the whole width in mild to moderate kyphotic deformities; hence the growth of the disease segment will occur with minor variation in different part/segment of the vertebrae. Hence the kyphotic deformity will either remain stationary or will improve/progress a little. This has been described by Rajasekaran et al. as Type II or III.8 In severe degree of kyphosis, the proximal vertebrae rests on distal vertebrae at one point [Figure 1]. It produces a wedging of distal epiphyseal ring. The proximal vertebral apophyseal ring is loaded in anterior half, hence growth is retarded while the apophyseal ring posterior to point pressure continue to increase at an accelerated rate hence whatever growth occurs is added to the kyphosis. The growing posterior part of the VB adds to the internal salient predisposing the spinal cord for late onset paraplegia.
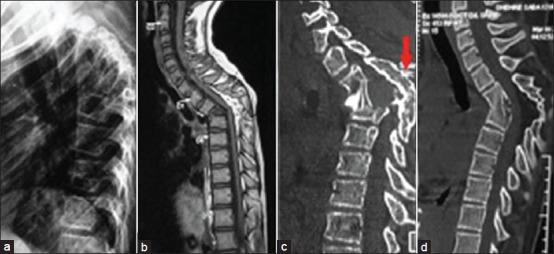
Figure 1.
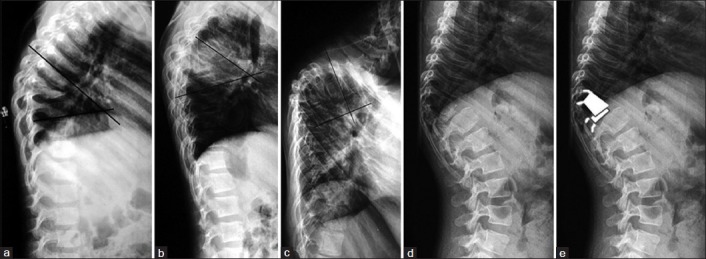
Lateral x-rays of spine in 3 children shows (a, b) moderate kyphotic deformity (c) severe kyphotic deformity following TB of spine. (d, e) Lateral x-rays and line diagramme showing the proximal vertebrae resting on anterior surface on to distal vertebrae
In a long segment disease, the anterior vertebral bodies are destroyed almost completely, hence proximal vertebral column bends over the distal column until the proximal healthy vertebra rests on the distal healthy vertebra in order to provide stability to the spine. During the collapse of the spine, the facet joints subluxate/dislocate at multiple levels. This results in unloading of many vertebrae at the apex of kyphosis and whatever growth occurs is added to the kyphosis. Hence the vertebrae in the apex of kyphosis are taller than the rest of the vertebral column. The increasing kyphosis associated with increased internal salient leads to stretching of spinal cord and consequent late onset paraplegia. Rajasekaran reported in a series of TB spine in children on a long followup that 44% kyphosis do not progress, 17% remains stationary and 39% deformity progresses.8
MAGNITUDE OF TB SPINE IN CHILDREN
TB spine is reported in infants as latent tuberculosis (TB).9,10 The incidence of spinal tuberculosis in children is variable. It is reported as 58% of all spine tuberculosis in Korea, 1/3rd of all patients as reported from Chennai (India) and 26% in Hong Kong.11,12,13,14,15 It produces severe bone loss as well as growth affection; hence the sequelae are serious. The vertebral bodies in children are cartilaginous. Younger the child, larger is the cartilage volume in each vertebral body. Hence whenever a tubercular infection affects the vertebral bodies the cartilage loss occurs rapidly and consecutively severe deformities occur within a short span of time in comparison to adults [Figure 2].
Figure 2.
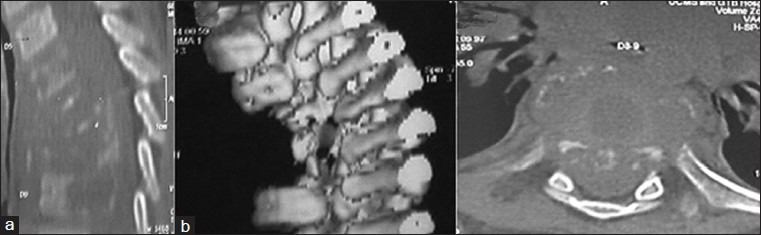
(a) Computed tomography (CT) scan (sagittal section) of upper dorsal spine in a 3 year old child shows 5 vertebral body disease. The vertebral body almost disappeared (b) on 3D reconstruction and (c) axial CT shows no trace of bone in VB
The growth potential of the vertebral bodies is also damaged secondary to the disease and consequent to surgical intervention. The apophyseal ring is partially or completely damaged when the disease focus is excised partially or completely while decompressing the spinal cord. Consequently the growth potential is affected partially or totally. The growth changes of solidly fused kyphotic block after surgery were evaluated in a series of 117 children of spinal TB operated for various surgical procedures.16 Those cases which were operated for anterior resection and fusion particularly in dorsal spine spanning several segment showed the worst results for progression of kyphotic deformity as total anterior growth potential is destroyed and growth of posterior column continued unabated. The “Dimeglio formula” states that for each vertebral segment 0.7 mm/year of longitudinal growth is lost after posterior arthrodesis.3 When posterior fusion is added to the anterior radical resection and fusion, the progression of deformity was not severe as the posterior growth was also retarded. Where only anterior debridement was done the progression of the deformity was the least because the anterior growth potential was retained partially. The author concluded that the radical anterior surgery destroys the anterior growth and limits the capacity for spinal remodeling and posterior column does contribute to some growth.16,17 However there is no evidence to suggest that the disproportionate posterior growth contributes to progression of deformity after anterior spinal fusion in children.18,19
Every effort should be made to avoid vertebral damage by diagnosing TB early before severe damage occurs [Figure 3]. The surgery should involve limited resection of bone and these patients should be followed until skeletal maturity to carefully monitor the effect of growth on spinal deformity.
Figure 3.
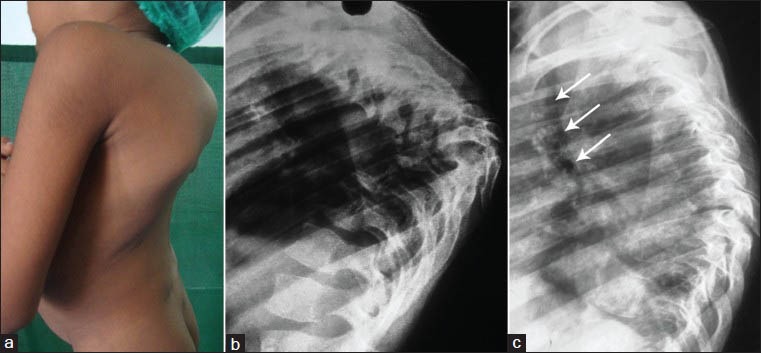
(a) Clinical photograph of a 6 year old child reported with severe kyphosis following long segment tuberculosis of spine. (b) lateral x-rays shows severe kyphosis with destruction of D5-9 vertebral bodies (c) the lateral x-rays of the same patient taken 3 months before (which patient was carrying) also shows widening of prevertebral soft tissue shadow seen as deviation of tracheal shadow infront of upper dorsal spine (white arrows). The diagnosis was missed at this stage
MANAGEMENT
The children with TB spine usually present with persistent localized back pain, loss of appetite, weakness of both lower limb and inability to walk. The child is usually pale, listless and anemic. They also have a cautious gait and tend to walk keeping both hands at thigh to support the trunk. If the cervical spine is involved, they walk supporting the head with both hands.20 Clinically, one may find a knuckle/angular spinal deformity with or without a local/distant palpable cold abscess. TB spine in children is suspected clinically and the diagnosis can be confidently made on plain X-rays and magnetic resonance imaging (MRI) observations supported by raised ESR and positive Mantoux test. When clinicoradiological diagnoses is doubtful, the fine-needle aspiration cytology/biopsy for a histopathological diagnosis is indicated.
DRUG THERAPY
TB of the spine is a medical disease; surgical intervention is indicated for spinal deformity, neurological complications, instability, large abscesses and to obtain tissue in a case of diagnostic dilemma and suspected MDR TB.12,17 The drug therapy is similar to adults except that we need to prescribe the drugs as per weight of the child. The dosage schedule can be divided into 4 weight groups: Less than 10 kg, 10-17 kg, 18-25 kg and 25 kg and above.21 Rifampicin and isoniazid are advised as 75 mg each and pyrazinamide 250 mg and ethambutol 200 mg/day for a child weighing <10 kg. The doses are doubled, tripled and quadrupled for the above mentioned weight bands respectively.
The major concern regarding ATT is the under dosing of individual drugs. The modification of drug dosage is required when child gains weight on treatment and moves to another weight band, hence the weight of these patients should be monitored on successive visits.
The drugs which are toxic to children such as streptomycin and ethambutol are given in consultation with Pediatricians with due care to avoid the development of toxicity. Cases of TB spine which report for the first time with paraplegia are treated by a judicious combination of nonoperative and surgical modalities. The patients with neurological deficit developing on conservative treatment, remaining stationary for 4 weeks or more, deteriorating on nonoperative treatment require surgical decompression. In general, uncomplicated spinal TB is to be treated with ATT and suitable orthoses. The plain X-ray needs to be evaluated carefully for evidence of panvertebral lesion, a potentially unstable lesion which can be suspected on observing scoliosis on AP view or translation of proximal vertebra over distal in lateral view. Such cases should be surgically stabilized.
CONSIDERATION OF SPINAL DEFORMITY
Patients diagnosed as TB spine with no or minimal kyphosis generally report early to clinicians. The treatment principle, diagnosis, drug therapy are the same as for adults. Even if the TB lesion heals the deformity may improve/deteriorate subsequently as the child grows to adulthood. The patients should be kept under observation while on treatment for progression of kyphosis. The patient should be evaluated once a year for the appearance/progression of the kyphosis until skeletal maturity.
In patients who report with kyphotic deformity of some severity, the disease will heal under the influence of ATT but kyphosis either will remain stationary or deteriorate while on treatment and thereafter in the growth phase. The deformity of the spine in these patients will continue to increase in the active phase and even after healing of disease. The progression of deformity depends on the severity of angle before treatment, level of lesion and age of the patients. In children 39% deformity increases 44% deformity spontaneously improves and 17% the kyphus remains same as achieved after healing of the disease.8 In children less than 7 years with 3 or more vertebral body affection in a dorsal or dorsolumbar spine the deformity produced is severe and it progresses further.
The persistent kyphotic deformity leaves tremendous biomechanical stresses on the proximal or distal part of the spine and spinal cord. On longer followup these patients are likely to develop severe canal stenosis in the proximal/distal spine and/or late onset paraplegia. The cardiorespiratory embarrassment with painful costo-pelvic impingement secondary to severe kyphotic deformity, pose a risk for major surgical undertaking in cases of late onset paraplegia. The correction of such severe kyphosis is hazardous and fraught with complications. The spinal cord undergoes atrophic or myelomalacic/syringomyelic changes as a result of movement of spinal cord over angular internal salient in severe kyphotic deformity. The concomitant vascular or intrinsic damage of the spinal cord adds a risk of neural deterioration and consequent delayed or poor neural recovery following inadvertent handling of the spinal cord while excising the hard internal salient.17
Only 39% of children develop a progressive kyphotic deformity, hence it is important to identify these 39% children in the early active stages of the disease. The clinical risk factors for developing progressive kyphosis are age less than 7 years, more than three vertebral body affection and the disease at lower dorsal and dorsolumbar junctional area. The radiological “spine at risk” signs are facet subluxation, retropulsion, toppling and lateral translation.8 The kyphotic deformity progresses if 2 or more spine at risk signs are observed in the presence of the clinical risk factors.
The intervertebral disc is balloon shaped and well hydrated in children. It retains its shape and size in children in granulation tissue of an active lesion. The disc still continues to maintain its shape and does not allow proximal spine to stabilize on distal segment by osseous fusion once the lesion achieves healed status. Consequently the children have an unstable spine and deformity progresses on vertical loading when the patient walks or bends forward.
Those kyphotic deformities which are likely to show progression should be considered for correction of kyphosis in active disease or early posttreatment stage as surgery is easier and associated with less risk in the active stage. The posterior spinal fusion was advocated as a method to halt posterior column growth to stop the progression of the kyphosis. The spines that have features of progressive kyphosis, continue to grow in kyphosis in spite of successful posterior spinal fusion.17
CORRECTION OF KYPHOSIS
The principles of kyphotic deformity correction are anterior debridement/corpectomy, posterior column shortening, posterior instrumentation and anterior and posterior fusion performed sequentially simultaneously in a single stage.22,23,24,25,26 One or two staged anterior decompression and followed by posterior instrumented stabilization has been described to prevent posttreatment deterioration of kyphosis.27
This can be performed by (i) extra pleural anterolateral approach, (ii) posterior midline approach.
Extra pleural anterolateral approach
It allows single stage correction of kyphosis in dorsal and dorsolumbar spine.22 The patient is placed in right lateral position. The apex of the lesion is approached by removing 3 ribs on the left side and anterior corpectomy is performed. The anterior wound is packed and posterior exposure is done to expose the apex vertebra and interlaminar space for 3 segments on either side and sublaminar wires are passed. The posterior complex of the apex vertebra is excised along with the pedicle on the left side; the corresponding rib and the pedicle on the right side are also removed. A preshaped (prebent) Hartshill rectangle is placed and the distal sublaminar wires are tightened followed by the tightening of the proximal sublaminar wires [Figure 4].22,28
Figure 4.
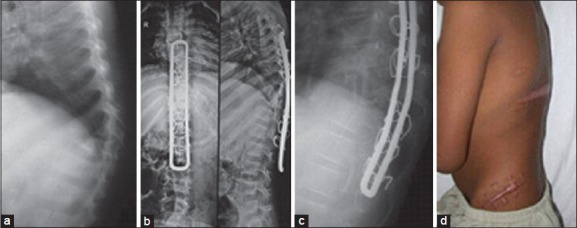
A 5 year old child with TB of spine on anti tubercular treatment for 6 months presented with a radiological signs of progressive kyphotic deformity (a) Standard extra pleural anterolateral decompression was done with stabilization using a closed Hartshill (b and c) was done (d) clinical photograph showing the surgical scar over iliac crest and healed posterior T-incision
This is a good procedure for children of any age in active disease and/or partially treated by ATT. The advantages are (a) The patient is in lateral position in the extra pleural approach hence remains stable during the procedure and does not require temporary stabilization (b) The avoidance of exposure of the chest cavity and retroperitoneal space makes it less morbid (c) The simultaneous exposure of anterior and posterior columns of the spine allows the opportunity to work on both anterior and posterior segments simultaneously.
The authors believe that Hartshill rectangle as the implant of choice in younger children to be placed deep in the paraspinal muscles. The Hartshill rectangle open at one end allows the spine to grow longitudinally and it does not act as a posterior tether. In multiple VB affection, the sublaminar wires can take purchase against the healthy posterior complex, hence the span of instrumentation can be minimised.
Posterior midline approach
The spine is exposed by midline approach in the prone position. The pedicle screws are inserted 2-3 segments above and below the lesion. Temporary stabilization by a precontoured rod is done on one side. 2-3 ribs are removed on both sides and decancellation of the apex vertebra is done. The same is repeated on the other side by shifting the temporary stabilization rod. Anterior resection is done gradually [Figure 5]. Laheri et al. (n = 28) reported good deformity correction by posteolateral retropleural approach and used segmental spinal instrumentation with the Hartshill rectangle for posterior stabilization.29 Guven et al. and Lee et al. performed kyphosis correction in active disease by a single stage transpedicular approach and reported good deformity correction with minimal loss of correction till complete healing of disease.30,31 However, Gokce et al. reported correction of kyphosis from 51.1[0] to 23o in lower dorsal and dorsolumbar spine by a posterior wedge osteotomy and posterior fusion by the posterior midline approach.32
Figure 5.

A 5 year female with (a) kyphus deformity (b) preoperative X-ray and (c) magnetic resonance imaging after 6 months of anti tubercular treatment and (d) postoperative X-ray showing kyphus correction using pedicle screws (e) healed posterior midline incision (e) 2 years followup x-rays of the same patient, the anterior vertebral body height has increased on followup
SEVERE KYPHOSIS IN HEALED LESION
Severe kyphosis is not a mere disfigurement. It produces progressive restriction of pulmonary functions. Louw reported 23 patients of severe kyphosis, 11 (47.8%) had more than 50% restriction of pulmonary functions, whereas 10 (43.5%) had between 25-50% and 2 (8.71%) had mild restriction of pulmonary functions.33 Correction of such severe kyphosis of long standing is a technically demanding surgery with higher risk of neurologic injury. Yau et al. performed a multistaged surgery where anterior osteotomy and decompression was performed after fitting a halo pelvic distractor. In the second stage posterior osteotomy and fusion was done. As a third stage, again anterior fusion was done. The patient was maintained in halo pelvic distractor until sound fusion was achieved. The mean preoperative kyphosis in this series was 115.5° could be corrected to 28.3° while three patients died. The author concluded that it may be a relatively small reward for such a major undertaking. Such treatment should be instituted where deformity is severe with active disease and paraplegia or death from chest complication is imminent.33 For patients with healed disease in whom danger of paraplegia and rapid progression of deformity are less, the hazard of deformity correction outweighs the gain hence it should not be carried out for cosmetic reasons only.33,34 Even for late onset paraplegia the surgeon should not be too ambitious to correct deformity and the patient should be forewarned about the risk of neural deterioration and risk to life. Transpedicular decancellation osteotomy35,36 has also been described for healed posttubercular kyphosis at dorsolumbar spine. This method has been reported with a successful correction of kyphosis in dorsolumbar and lumbar kyphosis with mean preoperative kyphosis correction from 29.9° to 12.2°33 and mean preoperative kyphosis from 58.8° to 13.7° respectively in two series.36
The principles of such correction are also the same with anterior corpectomy, posterior column shortening, closing/opening wedge osteotomy and instrumented stabilization. In such instances since there is no active disease hence pedicle screw construct with posterior only multilevel modified vertebral column resection can allow good deformity correction. Few studies have been reported where the deformity correction has been performed by the closing-opening wedge osteotomy procedure with pedicle screw fixation.37
PARAPLEGIA WITH HEALED DISEASE (LATE ONSET PARAPLEGIA)
The patients usually are successfully treated and achieved healed status more than 10 years ago. They have a severe kyphotic deformity and now have developed gradual onset clinical feature of upper motor neuron neural deficit. The appearance of neural deficit may be caused by reactivation of tuberculosis at/above/below the apex of kyphosis. It may be secondary to intrinsic changes in the spinal cord secondary to acute angular internal salient. We need to differentiate on history whether the patient has unrecovered neural deficit from the initial disease or reappearance/progression of neural deficit. MRI is useful to differentiate recrudescence from paraplegia with healed disease.17
Anterior decompression and fusion is advocated in all such cases. The internal salient can be removed either by transthoracic transpleural anterior approach or by the extra pleural anterolateral approach. The internal kyphectomy allows anterior decompression and anterior transposition of the spinal cord. The response to anterior decompression is faster, better and safe in patients with active disease. Although in patients with healed disease the anterior decompression is technically more difficult and the recovery less satisfactory.34 Complications such as neural deterioration (transient or permanent) and CSF fistula have been reported and patients should be warned before the surgery about the possibility of neural deterioration.38
The extra pleural anterolateral or costotransversectomy approach allows direct exposure of internal salient and it does not jeopardize the already compromised pulmonary function.39 The posterior 5 cm of three crowded ribs at apex are removed along with the transverse processes. Care is needed to remain extra pleural or retroperitoneal. Segmental intercostal nerves serve as a guide to intervertebral foramina. Two or three pedicles at apex are resected and dura is seen. One or more intercostal vessels are ligated and cut. The pleura are elevated at the apex of kyphosis. The removal of posterior half of the collapsed vertebrae is done with a high speed burr leaving behind posterior rim until last to avoid forward migration of the dural sac. This allows spinal cord to be transposed anteriorly and adequate length of anterior dura is exposed [Figure 6]. Cortical strut grafting is performed as far anteriorly as possible after exposing the proximal and distal limits of angular kyphus.
Figure 6.
Preoperative (a) X-ray lateral view (b) sagittal T1WI MRI show kyphus deformity internal gibbus at D3 in an 11-year-old girl following old childhood diseases. The lesion has no activity. (c) immediate postoperative sagittal reconstruction image shows internal kyphectomy and anterior transposition of the spinal cord (d) same image at one year followup shows incorporated bone graft
INSTRUMENTATION IN CHILDREN
The vertebral bodies in children are smaller. As a result of kyphotic deformity and active disease the paraspinal muscles are wasted. It is difficult to procure the adequate size of pedicle screw in very young children (<5 years). The profile of pedicle screw is likely to produce ischemia of skin and consequent wound dehiscence or ulcer. In children with multiple vertebral body involvement, there are instances where intraosseous abscess is so large that pus starts to drain through holes made for pedicle scew insertion. In such instances the hartshill rectangle is a useful implant [Figure 7]. The children should be kept in lateral position until such time the wound heals. In a very young child the Hartshill rectangle which is open at the distal end becomes a good implant. However, it should be bent properly and seated in soft tissue. The children should be placed on a Minerva jacket for 3-4 months till such time anterior and posterior fusion is achieved. The parents should be advised not to take children on shoulder least the anterior graft/cage collapse and sublaminar wire gives way [Figure 8].
Figure 7.
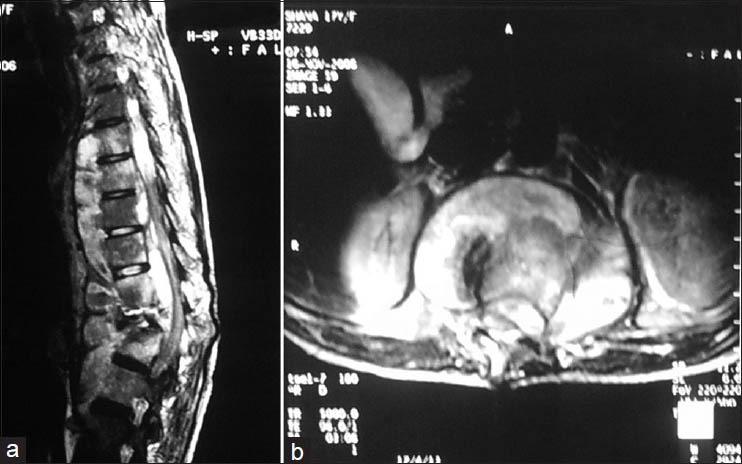
(a) T2W1 magnetic resonance imaging sagittal section shows a 9 vertebral body affection with kyphosis correction was done by pedicle screw insertion, each hole for pedicle screw showed pus, hence hartshill fixation was performed where sublaminar wires took purchase against healthy lamina (b) Intraosseous abscess communicating with anterior prevertebral collection seen in axial section
Figure 8.

Clinical photograph of a child taken on shoulder by mother. The patient was operated for kyphus correction with Hartshill fixation. The kyphus has progressed as Hartshill has given way
Summarily the children with TB spine should be kept under followup till skeletal maturity. The patient with severe kyphotic deformity or showing clinicoradiological prediction of progressive kyphosis should be surgically treated for deformity correction. The surgical approach, type of instrumentation and followup require individualized approach. The late onset paraplegia is better prevented than treated.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Sarwark J, Aubin CE. Growth considerations of the immature spine. J Bone Joint Surg Am. 2007;89:8–13. doi: 10.2106/JBJS.F.00314. [DOI] [PubMed] [Google Scholar]
- 2.Soames RW. Skeletal system. In: Williams LH, Berry MM, Collins P, Dyson M, Dussek J, Ferguson MW, editors. Gray's Anatomy: The Anatomical Basis of Medicine and Surgery. 38th ed. New York: Churchill Livingstone; 1995. pp. 510–36. [Google Scholar]
- 3.Dimeglio A, Ferran JL. Three-dimensional analysis of the hip during growth. Acta Orthop Belg. 1990;56:111–4. [PubMed] [Google Scholar]
- 4.Roaf R. Vertebral growth and its mechanical control. J Bone Joint Surg Br. 1960;42-B:40–59. doi: 10.1302/0301-620X.42B1.40. [DOI] [PubMed] [Google Scholar]
- 5.Taylor JR. Growth of human intervertebral discs and vertebral bodies. J Anat. 1975;120(Pt 1):49–68. [PMC free article] [PubMed] [Google Scholar]
- 6.Mehlman CT, Araghi A, Roy DR. Hyphenated history: The Hueter-Volkmann law. Am J Orthop (Belle Mead NJ) 1997;26:798–800. [PubMed] [Google Scholar]
- 7.Stokes IA, Mente PL, Iatridis JC, Farnum CE, Aronsson DD. Enlargement of growth plate chondrocytes modulated by sustained mechanical loading. J Bone Joint Surg Am. 2002;84-A:1842–8. doi: 10.2106/00004623-200210000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Rajasekaran S. The natural history of posttubercular kyphosis in children. Radiological signs which predict late increase in deformity. J Bone Joint Surg Br. 2001;83:954–62. doi: 10.1302/0301-620x.83b7.12170. [DOI] [PubMed] [Google Scholar]
- 9.Consigilieri G, Kakarla UK, Theodore N. Pott disease in a 13-month-old: Case report. Neurosurgery. 2011;68:E1485–90. doi: 10.1227/NEU.0b013e318210c81b. [DOI] [PubMed] [Google Scholar]
- 10.Lee IC, Quek YW, Tsao SM, Chang IC, Sheu JN, Chen JY. Unusual spinal tuberculosis with cord compression in an infant. J Child Neurol. 2010;25:1284–7. doi: 10.1177/0883073809357938. [DOI] [PubMed] [Google Scholar]
- 11.Moon MS, Kim SS, Lee BJ, Moon JL. Spinal tuberculosis in children: Retrospective analysis of 124 patients. Indian J Orthop. 2012;46:150–8. doi: 10.4103/0019-5413.93676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.A controlled trial of ambulant out-patient treatment and in-patient rest in bed in the management of tuberculosis of the spine in young Korean patients on standard chemotherapy a study in Masan. Korea. First report of the Medical Research Council Working Party on Tuberculosis of the Spine. J Bone Joint Surg Br. 1973;55:678–97. [PubMed] [Google Scholar]
- 13.A controlled trial of anterior spinal fusion and debridement in the surgical management of tuberculosis of the spine in patients on standard chemotherapy: A study in Hong Kong. Br J Surg. 1974;61:853–66. doi: 10.1002/bjs.1800611102. [DOI] [PubMed] [Google Scholar]
- 14.A 10-year assessment of a controlled trial comparing debridement and anterior spinal fusion in the management of tuberculosis of the spine in patients on standard chemotherapy in Hong Kong. Eighth Report of the Medical Research Council Working Party on Tuberculosis of the Spine. J Bone Joint Surg Br. 1982;64:393–8. doi: 10.1302/0301-620X.64B4.7047536. [DOI] [PubMed] [Google Scholar]
- 15.A 10-year assessment of controlled trials of inpatient and outpatient treatment and of plaster-of-Paris jackets for tuberculosis of the spine in children on standard chemotherapy. Studies in Masan and Pusan, Korea. Ninth report of the Medical Research Council Working Party on Tuberculosis of the Spine. J Bone Joint Surg Br. 1985;67:103–10. doi: 10.1302/0301-620X.67B1.2857181. [DOI] [PubMed] [Google Scholar]
- 16.Schulitz KP, Kothe R, Leong JC, Wehling P. Growth changes of solidly fused kyphotic bloc after surgery for tuberculosis. Comparison of four procedures. Spine (Phila Pa 1976) 1997;22:1150–5. doi: 10.1097/00007632-199705150-00016. [DOI] [PubMed] [Google Scholar]
- 17.Jain AK, Dhammi IK, Jain S, Mishra P. Kyphosis in spinal tuberculosis-Prevention and correction. Indian J Orthop. 2010;44:127–36. doi: 10.4103/0019-5413.61893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Upadhyay SS, Saji MJ, Sell P, Yau AC. The effect of age on the change in deformity after radical resection and anterior arthrodesis for tuberculosis of the spine. J Bone Joint Surg Am. 1994;76:701–8. doi: 10.2106/00004623-199405000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Upadhyay SS, Saji MJ, Sell P, Hsu LC, Yau AC. The effect of age on the change in deformity after anterior débridement surgery for tuberculosis of the spine. Spine (Phila Pa 1976) 1996;21:2356–62. doi: 10.1097/00007632-199610150-00010. [DOI] [PubMed] [Google Scholar]
- 20.Tuli S. 3rd ed. New Delhi: Jaypee Brothers; 2004. Tuberculosis of the Skeletal System: Bones, Joints, Spine and Bursal Sheaths. [Google Scholar]
- 21.Lodha R, Menon PR, Kabra SK. Concerns on the dosing of anti tubercular drugs for children in RNTCP. Indian Pediatr. 2008;45:852–4. [PubMed] [Google Scholar]
- 22.Jain AK, Dhammi IK, Jain S, Kumar J. Simultaneously anterior decompression and posterior instrumentation by extra pleural retroperitoneal approach in thoracolumbar lesions. Indian J Orthop. 2010;44:409–16. doi: 10.4103/0019-5413.69315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jain AK, Dhammi IK. Tuberculosis of the spine: A review. Clin Orthop Relat Res. 2007;460:39–49. doi: 10.1097/BLO.0b013e318065b7c3. [DOI] [PubMed] [Google Scholar]
- 24.Mukhtar AM, Farghaly MM, Ahmed SH. Surgical treatment of thoracic and lumbar tuberculosis by anterior interbody fusion and posterior instrumentation. Med Princ Pract. 2003;12:92–6. doi: 10.1159/000069113. [DOI] [PubMed] [Google Scholar]
- 25.Moon MS, Woo YK, Lee KS, Ha KY, Kim SS, Sun DH. Posterior instrumentation and anterior interbody fusion for tuberculous kyphosis of dorsal and lumbar spines. Spine (Phila Pa 1976) 1995;20:1910–6. doi: 10.1097/00007632-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Güven O. Posterior instrumentation and anterior interbody fusion for tuberculous kyphosis of dorsal and lumbar spines. Spine (Phila Pa 1976) 1996;21:1840–1. doi: 10.1097/00007632-199608010-00028. [DOI] [PubMed] [Google Scholar]
- 27.Jain AK. Tuberculosis of the spine. Clin Orthop Relat Res. 2007;460:2–3. doi: 10.1097/BLO.0b013e318073bd29. [DOI] [PubMed] [Google Scholar]
- 28.Jain AK, Maheshwari AV, Jena S. Kyphus correction in spinal tuberculosis. Clin Orthop Relat Res. 2007;460:117–23. doi: 10.1097/BLO.0b013e3180514bfe. [DOI] [PubMed] [Google Scholar]
- 29.Laheri VJ, Badhe NP, Dewnany GT. Single stage decompression, anterior interbody fusion and posterior instrumentation for tuberculous kyphosis of the dorso-lumbar spine. Spinal Cord. 2001;39:429–36. doi: 10.1038/sj.sc.3101185. [DOI] [PubMed] [Google Scholar]
- 30.Güven O, Kumano K, Yalçin S, Karahan M, Tsuji S. A single stage posterior approach and rigid fixation for preventing kyphosis in the treatment of spinal tuberculosis. Spine (Phila Pa 1976) 1994;19:1039–43. doi: 10.1097/00007632-199405000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Lee SH, Sung JK, Park YM. Single-stage transpedicular decompression and posterior instrumentation in treatment of thoracic and thoracolumbar spinal tuberculosis: A retrospective case series. J Spinal Disord Tech. 2006;19:595–602. doi: 10.1097/01.bsd.0000211241.06588.7b. [DOI] [PubMed] [Google Scholar]
- 32.Gokce A, Ozturkmen Y, Mutlu S, Caniklioğlu M. Spinal osteotomy: Correcting sagittal balance in tuberculous spondylitis. J Spinal Disord Tech. 2008;21:484–8. doi: 10.1097/BSD.0b013e3181586023. [DOI] [PubMed] [Google Scholar]
- 33.Yau AC, Hsu LC, O’Brien JP, Hodgson AR. Tuberculous kyphosis: Correction with spinal osteotomy, halo-pelvic distraction and anterior and posterior fusion. J Bone Joint Surg Am. 1974;56:1419–34. [PubMed] [Google Scholar]
- 34.Moon MS. Tuberculosis of the spine. Controversies and a new challenge. Spine (Phila Pa 1976) 1997;22:1791–7. doi: 10.1097/00007632-199708010-00022. [DOI] [PubMed] [Google Scholar]
- 35.Bezer M, Kucukdurmaz F, Guven O. Transpedicular decancellation osteotomy in the treatment of posttuberculous kyphosis. J Spinal Disord Tech. 2007;20:209–15. doi: 10.1097/01.bsd.0000211271.89485.f1. [DOI] [PubMed] [Google Scholar]
- 36.Kalra KP, Dhar SB, Shetty G, Dhariwal Q. Pedicle subtraction osteotomy for rigid posttuberculous kyphosis. J Bone Joint Surg Br. 2006;88:925–7. doi: 10.1302/0301-620X.88B7.17366. [DOI] [PubMed] [Google Scholar]
- 37.Rajasekaran S, Vijay K, Shetty AP. Single-stage closing-opening wedge osteotomy of spine to correct severe posttubercular kyphotic deformities of the spine: A 3-year followup of 17 patients. Eur Spine J. 2010 Apr;19:583–92. doi: 10.1007/s00586-009-1234-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hsu LC, Cheng CL, Leong JC. Pott's paraplegia of late onset. The cause of compression and results after anterior decompression. J Bone Joint Surg Br. 1988;70:534–8. doi: 10.1302/0301-620X.70B4.3403593. [DOI] [PubMed] [Google Scholar]
- 39.Wong YW, Leong JC, Luk KD. Direct internal kyphectomy for severe angular tuberculous kyphosis. Clin Orthop Relat Res. 2007;460:124–9. doi: 10.1097/BLO.0b013e31805470db. [DOI] [PubMed] [Google Scholar]


