Abstract
Background:
Majority of C1 fractures can be effectively treated conservatively by immobilization or traction unless there is an injury to the transverse ligament. Conservative treatment usually involves a long period of immobilization in a halo-vest. Surgical intervention generally involves fusion, eliminating the motion of the upper cervical spine. We describe the treatment of unstable Jefferson fractures designed to avoid these problems of both conservative and invasive methods.
Materials and Methods:
A retrospective review of 12 patients with unstable Jefferson fractures treated with transoral osteosynthesis of C1 between July 2008 and December 2011 was performed. A steel plate and C1 lateral mass screw fixation were used to repair the unstable Jefferson fractures. Our study group included eight males and four females with an average age of 33 years (range 23-62 years).
Results:
Patients were followed up for an average of 16 months after surgery. Range of motion of the cervical spine was by and large physiologic: Average flexion 35° (range 28-40°), average extension 42° (range 30-48°). Lateral bending to the right and left averaged 30° and 28° respectively (range 12-36° and 14-32° respectively). The average postoperative rotation of the atlantoaxial joint, evaluated by functional computed tomography scan was 60° (range 35-72°). Total average lateral displacement of the lateral masses was 7.0 mm before surgery (range 5-12 mm), which improved to 3.5 mm after surgery (range 1-6.5 mm). The total average difference of the atlanto-dens interval in flexion and extension after surgery was 1.0 mm (range 1-3 mm).
Conclusions:
Transoral osteosynthesis of the anterior ring using C1 lateral mass screws is a viable option for treating unstable Jefferson fractures, which allows maintenance of rotation at the C1-C2 joint and restoration of congruency of the atlanto-occipital and atlantoaxial joints.
Keywords: Jefferson fractures, osteosynthesis, transoral approach
INTRODUCTION
Jefferson fractures of C1 constitutes 25% of all craniocervical injuries, 2-13% of all cervical spine injuries, and approximately 1.3% of all spinal fractures.1,2 There is a high prevalence of concomitant fractures of the axis, especially odontoid fractures.3,4 The unstable Jefferson fracture of C1 is characterized by outward displacement of the lateral masses (LMD) in response to axial load.5,6 Treatment algorithms in determining surgical versus nonsurgical treatment of unstable Jefferson fractures have not reached a consensus, but treatment decisions are often based on the integrity of the transverse ligament and on the fact whether fractures occur in combination with other unstable spinal injuries. Conservative treatment of unstable Jefferson injuries includes immobilization and traction while surgical procedures typically involve posterior fusion of either C1-C2 or occiput-C2. Fusion procedures lead to loss of range of motion, particularly elimination of C1-C2 rotation and C0-C1 flexion/extension.7 There are few reports describing treatment of unstable Jefferson fractures with osteosynthesis of C1 via a transoral approach without C1-C2 fusion.8 The purpose of this study is to introduce a motion-preserving surgical technique of reduction and stabilization for unstable Jefferson fracture and to evaluate clinical outcomes.
MATERIALS AND METHODS
A retrospective review of 12 patients with unstable Jefferson fractures treated with a transoral osteosynthesis of C1 between July 2008 and December 2011 was performed. Eight males and four females with an average age of 33 years (range 23-62 years) were evaluated. All patients underwent radiologic evaluation via plain cervical spine radiographs, computed tomography (CT) and magnetic resonance imaging (MRI). The mode of injury was road traffic injuries (n=4), falls (n=5) and diving injuries (n=3). All patients complained of neck pain, stiffness and decreased range of motion without neurologic deficit. Three patients had bilateral fractures of the anterior arch (anterior 1/2 Jefferson fractures, Landells and Van Petegghem type I) [Figure 1a–f]. Five patients had anterior arch fractures with an associated posterior arch fracture (semi-ring Jefferson fracture, Landells and Van Petegghem type II) [Figure 2A]. Two patients had bilateral fractures of the anterior arch associated with a posterior arch fracture (anterior 3/4 Jefferson fracture, Landells and Van Petegghem type II), one patient presented with a comminuted anterior arch fracture associated with a C6 burst fracture [Figure 3A]. One patient had an anterior arch fracture associated with aplasia of the posterior arch. Seven patients had an intact transverse ligament and five patients had avulsion of the insertion of the transverse ligament (Dickman type II). Raney-Crutchfield Tong was applied after admission to stabilize the fracture using weights between 2 and 3 kg.
Figure 1.
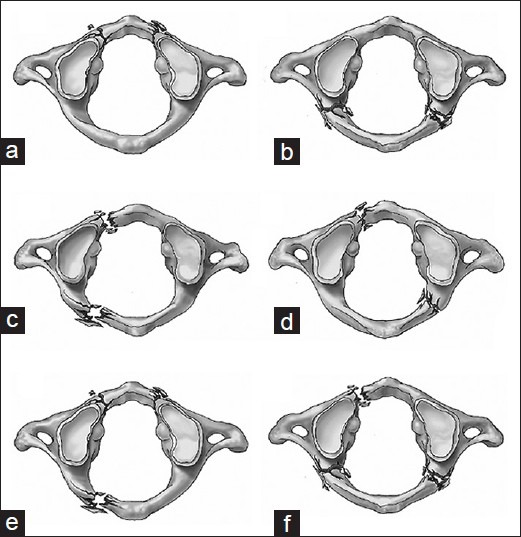
A line diagram showing anterior 1/2 Jefferson fractures (a) and posterior 1/2 Jefferson fractures (b) are both Landells and Van Peteghem type I with isolated arch fractures. Semi-ring Jefferson fracture (c and d) are Landells and Van Peteghem type II, which also includes anterior 3/4 Jefferson fracture (e) and posterior 3/4 Jefferson fracture (f)
Figure 2A.
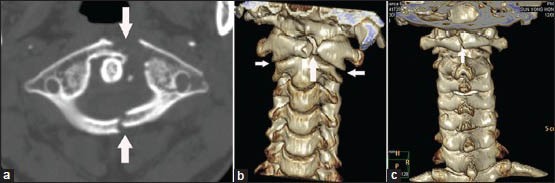
(a-c) Preoperative axial computed tomography (CT) scan and three-dimensional reconstruction CT shows anterior arch fracture associated with posterior arch fracture in the atlas, both of lateral mass displacement are about 7.0 mm
Figure 3A.
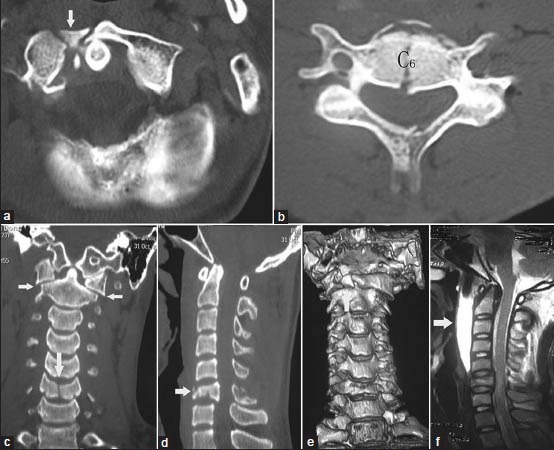
(a-e) Preoperative axial plane, coronal plane, sagittal plane computed tomography (CT) scan and three dimensional reconstruction CT shows anterior arc comminution fractures on the right side associated with C6 burst fracture, the height of C6 vertebrae lost half, both of lateral mass displacement are about 6.0 mm (f) T2-weighted images in the sagittal plane show the gap and the signal intensity changes between C1 and C3 level. Prevertebral hematoma is indicated by solid white arrows, the width of prevertebral hematoma is about 9.8 mm in C1-C3 level, dural sac was partly compressed in C6 level, no abnormal spine cord signals
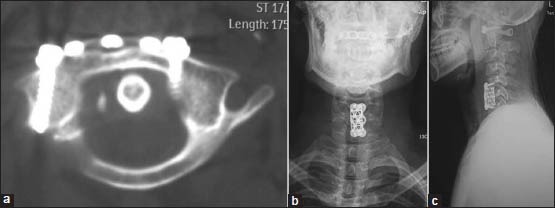
Figure 2C.
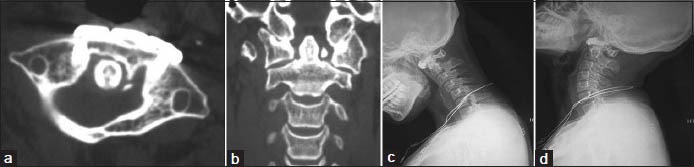
(a and b) Axial and coronal plane computed tomography at 2 years followup showing satisfactory osseous fusion, the good position of the screws and good reduction of the fracture. The lateral displacement of the lateral masses was improved to 2.0 mm (c and d) dynamic flexion/extension lateral radiographs of cervical spine showing no C1-C2 instability
Figure 2D.
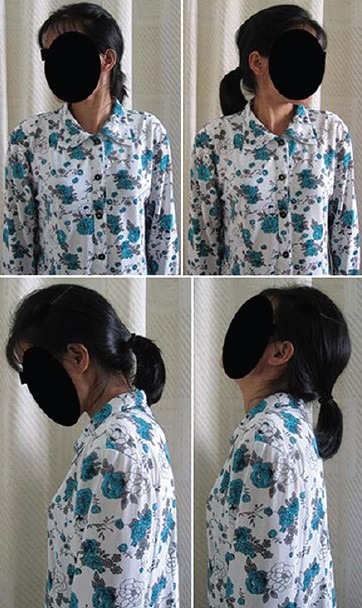
The clinical photograph of the same patient at 2 years followup showing full range of motion of the cervical spine including more than 60° of rotation in each direction
Figure 3B.
(a-c) At 6 months followup, axial computed tomography and roentgenograph manifested satisfactory osseous fusion and cervical alignment. The patient underwent a corpectomy of C6 and an anterior interbody fusion with a titanium mesh cage spacer and bone grafting of autologous C6 vertebrae
Operative procedure
Patients were positioned supine on a radiolucent frame under general anesthesia. The patient's head was secured using Gardner-Wells tongs and 2 kg of traction was applied. Somatosensory-evoked potential monitoring was established to monitor spinal cord function through out the surgery. The transoral approach was used as described by Yin et al. and Ai et al.9,10 After a Codman transoral retractor was placed for exposure of the posterior pharynx, the posterior pharyngeal wall was incised vertically approximately 25-30 mm in the midline. After splitting the soft palate, the mucosa of the posterior pharynx was incised forming a lateral-based flap. The longitudinal muscles were split in the midline. The anterior arch of C1 and the anterior aspect of the lateral masses were exposed. To define the entry point for the screws, the lower margin and the medial edge of the lateral mass of C1 are palpated to determine the center of the lateral mass.11 Any soft tissue in the fracture line was removed. In order to achieve the reduction, plier was used during the surgery to approximate the C1 lateral masses by compressing at the outer walls bilateral [Figure 4]. Osteosynthesis of C1 was performed using reconstruction plates; iliac crest bone grafting was necessary to reconstruct anterior arch defects in patients with burst fractures [Figure 2B]. In five cases, C1 specific plate was applied on Axis (Medtronic Spine, Memphis, TN, USA), while in seven cases treatment AO reconstruction plates were applied (AO plate; Synthes Spine, USA). In all cases, we used 3-hole, 40-mm-length, 5-mm-width, 2-mm-thick plates. The length and diameter of screws used were 20-24 mm and 3.5 mm, respectively.
Figure 4.
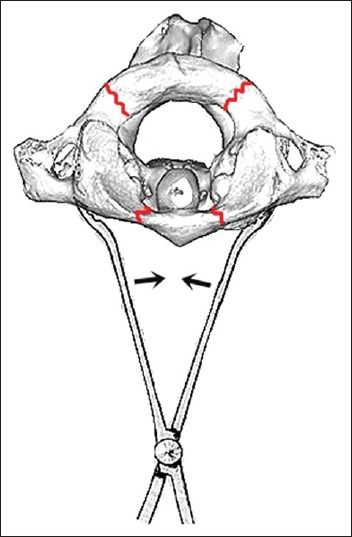
A line diagram showing plier is being used during surgery to achieve a reduction. Closure of the plier leads to approximation of the C1 lateral masses
Retrospective data included operative time (measured from the incision of the posterior pharyngeal wall to complete suture closure of the pharyngeal wall), clinicoradiological assessment and associated complications. Lateral, dynamic flexion/extension, anterior-posterior and open mouth odontoid radiographs of the upper cervical level were obtained at 3, 6 and 12 months postoperatively to assess union and alignment of C1-C2. 1 mm thin-slice CT scans with multiplanar reconstruction were used to assess bone healing and accuracy of screw placement and fracture reduction. Definitive fusion was identified by the formation of bridging bone across the fracture. The rotational capacity of the C1-C2 joints was measured by functional CT scans in the supine position as described by Koller et al.12 and patients were treated with therapy focusing on restoring rotation.
RESULTS
The patients were followed for average 16 months (range 12-28 months). All patients demonstrated clinical improvement. There were no postoperative complications in swallowing or speaking. The range of motion of the cervical spine was approximately physiologic. Average flexion 35° (range 28-40°), average extension 42° (range 30-48°). Lateral bending to the right and left averaged 30° and 28°, respectively (range 12-36° and 14-32° respectively) [Figure 2D]. The average postoperative rotation through the atlantoaxial joint, (evaluated by functional CT scan), was an arc of 60° (range 35-72°). The average composite lateral LMD was 7.0 mm before surgery (range 5-12 mm) and improved to 3.5 mm after surgery (range 1-6.5 mm) [Figure 2C]. The total average difference of the atlanto-dens interval in flexion extension after surgery was 1.0 mm (range 1-3 mm) [Table 1]. The average time was 100 min (range 80-120 min). The average intraoperative blood loss was 300 ml (range 100-500 ml) and the average fluoroscopic time was 60 s. No patient developed neurological deficit, arterial injury or other postoperative complication. At 6 months followup, roentgenograph and CT scan demonstrated satisfactory cervical alignment and osseous fusion in all the 12 patients [Figure 3B]. All screws were in a good position and no screws developed evidence of loosening or breakage. No C1-C2 instability was observed on flexion extension radiographs in any case [Figure 2C]. No patient went on to develop the previously described “cock-robin” deformity.
Table 1.
Clinical and radiographic results
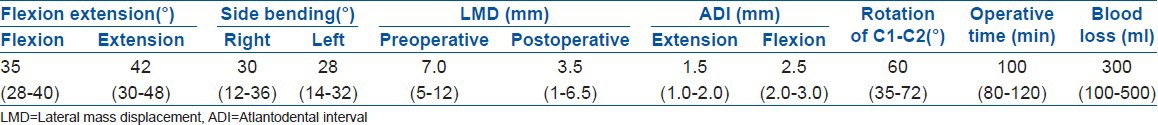
Figure 2B.
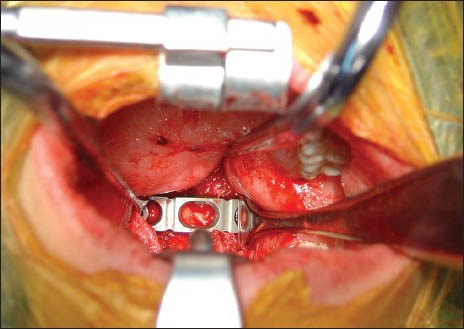
Transoral intraoperative view with the axis plate system, and bone grafting of autologous ilium were planted to anterior arch defect
DISCUSSION
Fractures of the atlas were originally described in the 1800s and further characterized through the classification systems given by Jefferson,13 Segal et al.,14 and Levine and Edwards.15 However, no single classification system can accurately describe the spectrum of atlas fractures seen in clinical practice. Most recent biomechanical studies of atlas fractures have concluded that these fractures are usually caused by axial loading through the occiput.16,17,18 Although there is agreement regarding treatment of stable Jefferson fractures, the optimal management of unstable Jefferson fractures remains controversial.6,19 The integrity of the transverse atlantal ligament (TAL) is the single most important factor in determining the method of treatment.20 Spence et al. reported a lateral mass spread >6.9 mm implied a disruption of the TAL.21 More recently, it has been proposed that MRI is a more sensitive indicator of TAL disruption than the “rule of Spence.” Based on a series of 39 patients with atlas and/or axis fractures who were evaluated with MRI, the authors reported that the use of standard cervical radiographs and the “rule of Spence” would have failed to identify 60% of fractures with associated disruption of the TAL.21 A recent report suggests that partial avulsion of the TAL can be sufficiently stabilized by surgical immobilization to allow union of the atlas fracture and healing of the avulsion.22
An unstable burst fracture of the atlas may result in atlantoaxial instability, even if properly treated.23 Patients on conservative management are often treated with initial reduction of the fracture with skeletal traction, followed by halo-vest immobilization. Advocates of surgical treatment cite high rates of nonunion and persistent neck pain as reasons to perform surgical stabilization.16,24,25 Neck pain is present in 20-80% of patients after external immobilization.14 Segal et al.14 reported 18 patients with atlas fractures were treated using the external immobilization. Of the five patients with isolated C1 fractures, nonunion of the fracture and poor clinical results were seen in three patients leading to conclusion that isolated anterior arch fractures often go onto nonunion with nonoperative treatment. Nonunion of isolated fractures of the atlas may occur in association with disruption of the transverse ligament, inadequate fracture reduction or absence of adequate cervical immobilization.26 Surgical immobilization has classically involved fusion from either the occiput to C2 or between C1 and C2 and posterior approaches offer the advantage of being a commonly performed approach with relatively low morbidity.27,28 However, the major disadvantage of C1-2 or C0-2 fusion is the loss of motion of the C1-2 and C0-1 joints and potentially accelerated degeneration of the subaxial cervical spine.8
Ideally, unstable atlas fractures would be treated with both stabilization of the atlas and maintenance of motion at the occipitocervical junction. Treatment strategies would involve limited fixation of the fracture to preserve the function of the atlantoaxial and atlanto-occipital joints while maintaining cervical alignment, possibly using either transoral limited internal fixation or limited posterior lateral mass fixation.8,16,22,25,29 C1 posterior osteosynthesis does expose the patient to the risks of vertebral artery and greater occipital nerve injury. The greater occipital nerve is at risk with a more cranial starting point for C1 lateral mass screws and the vertebral artery can be injured near the C1-2 joint,27,28 reduction via a posterior approach can be difficult to perform.8 Ruf et al.8 presented an innovative technique for function-preserving C1 osteosynthesis via a transoral approach, which was used successfully to treat six patients with high-grade C1 LMD using either compression plating or a screw-rod construct. No relevant C1-2 instability was observed on followup flexion extension radiographs. This technique however, is unsuitable for mounting a screw-rod instrumentation of more than 2 mm in thickness as the posterior pharyngeal soft tissue cannot completely cover the instrumentation, thus increasing the risk of wound infection.10,30
The transoral approach has some disadvantages, including the high rate of postoperative infection and the technical difficulty, which increases the postoperative complication rate to as high as 75%.31 Wound infection and dehiscence are common problems and observed in 9-22% of cases.32,33 Cerebrospinal fluid leaks, meningitis, neurological deficits and pseudomeningocele have also been reported. Breathing, swallowing and speech dysfunction may require gastrostomy and tracheostomy in 4% of patients.33 Velopharyngeal insufficiency is noted in about 40% of patients.32,33 Although commonly reported, we have yet to experience any of the aforementioned complications in our patients. Thorough preoperative oral cavity cleansing, establishing an ex-oral airway (tracheotomy), sterilization of the oral cavity, careful postoperative oral cavity nursing care, prophylactic antibiotics and maintenance of optimal nutritional support are all likely contributing factors.9,11
We consider anterior 1/4, posterior 1/4 or posterior 1/2 simple Jefferson fracture which are not combined with transverse ligament rupture to be stable fractures; injuries combined with transverse ligament ruptures should be treated as unstable fractures. During the surgery, skull traction via Gardner-Wells tongs contributes to achieving a partial reduction, which is of great importance during the surgery; complete reduction is rare during surgery. In our series, 12 patients underwent transoral limited internal fixation of the atlas using a pre bent steel plate and lateral mass screws to achieve a direct reduction of the lateral mass. A nearly anatomic reduction of the bony fragments could often be obtained. Fracture reduction restored the congruence of the atlanto-occipital and atlantoaxial joints, preventing the development of early arthrosis of these joints. Reduction through an anterior approach is facilitated by the fact that the center of the lateral masses is close to the anterior aspect of the atlas; the lever arm for reduction from an anterior approach is much shorter than it is from a posterior approach. All patients achieved fracture reduction, good cervical alignment and successful healing of the fracture; flexion/extension views demonstrated no loosening or breakage of screws and no C1-C2 instability. Patients improved clinically and cervical range of motion was adequately preserved as demonstrated by functional CT scan as described by Koller et al.12 Indications for this surgical approach include isolated atlas anterior 3/4 Jefferson fracture, anterior 1/2 Jefferson fracture and semi-ring Jefferson fracture. Abeloos et al.7 pointed out that patients with isolated atlas fractures without ligament injury, which do not heal after conservative treatment, isolated atlas fractures associated with C1 LMD and type II transverse ligament injury are also candidates for surgical intervention. A contraindication to this treatment approach is atlantoaxial or atlanto-occipital joint instability, such as seen in an isolated atlas fracture combined with type I ligament injury, which should be treated with C1-C2 or C0-C2 fusion. Special attention must be paid to the importance of characterizing the type of transverse ligament injury when making treatment decisions.2,20 Moreover, the technical nature of this procedure provides an additional challenge to the treating surgeon.
To conclude, transoral osteosynthesis using an anterior arch plate and lateral mass screws for treating unstable Jefferson fractures, which allows maintenance of rotatory mobility in the C1-C2 joint and restoration of congruency in the atlanto-occipital and atlantoaxial joints is a viable option. The procedure is able to achieve an anatomic reconstruction of the atlas and a reliable bony fusion of the fragments with a low morbidity rate.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.An HS. Cervical spine trauma. Spine (Phila Pa 1976) 1998;23:2713–29. doi: 10.1097/00007632-199812150-00011. [DOI] [PubMed] [Google Scholar]
- 2.Dickman CA, Sonntag VK. Injuries involving the transverse atlantal ligament: Classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery. 1997;40:886–7. doi: 10.1097/00006123-199704000-00061. [DOI] [PubMed] [Google Scholar]
- 3.Guiot B, Fessler RG. Complex atlantoaxial fractures. J Neurosurg. 1999;91:139–43. doi: 10.3171/spi.1999.91.2.0139. [DOI] [PubMed] [Google Scholar]
- 4.Gleizes V, Jacquot FP, Signoret F, Feron JM. Combined injuries in the upper cervical spine: Clinical and epidemiological data over a 14-year period. Eur Spine J. 2000;9:386–92. doi: 10.1007/s005860000153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kontautas E, Ambrozaitis KV, Kalesinskas RJ, Spakauskas B. Management of acute traumatic atlas fractures. J Spinal Disord Tech. 2005;18:402–5. doi: 10.1097/01.bsd.0000177959.49721.3b. [DOI] [PubMed] [Google Scholar]
- 6.Haus BM, Harris MB. Case report: Nonoperative treatment of an unstable Jefferson fracture using a cervical collar. Clin Orthop Relat Res. 2008;466:1257–61. doi: 10.1007/s11999-008-0143-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Payer M, Luzi M, Tessitore E. Posterior atlanto-axial fixation with polyaxial C1 lateral mass screws and C2 pars screws. Acta Neurochir (Wien) 2009;151:223–9. doi: 10.1007/s00701-009-0198-4. [DOI] [PubMed] [Google Scholar]
- 8.Ruf M, Melcher R, Harms J. Transoral reduction and osteosynthesis C1 as a function-preserving option in the treatment of unstable Jefferson fractures. Spine (Phila Pa 1976) 2004;29:823–7. doi: 10.1097/01.brs.0000116984.42466.7e. [DOI] [PubMed] [Google Scholar]
- 9.Yin Q, Ai F, Zhang K, Chang Y, Xia H, Wu Z, et al. Irreducible anterior atlantoaxial dislocation: One-stage treatment with a transoral atlantoaxial reduction plate fixation and fusion. Report of 5 cases and review of the literature. Spine (Phila Pa 1976) 2005;30:E375–81. doi: 10.1097/01.brs.0000168374.84757.d5. [DOI] [PubMed] [Google Scholar]
- 10.Ai F, Yin Q, Wang Z, Xia H, Chang Y, Wu Z, et al. Applied anatomy of transoral atlantoaxial reduction plate internal fixation. Spine (Phila Pa 1976) 2006;31:128–32. doi: 10.1097/01.brs.0000195159.04197.21. [DOI] [PubMed] [Google Scholar]
- 11.Hu Y, Ma W, Xu R. Transoral osteosynthesis C1 as a function-preserving option in the treatment of bipartite atlas deformity: A case report. Spine (Phila Pa 1976) 2009;34:E418–21. doi: 10.1097/BRS.0b013e3181a0ff2f. [DOI] [PubMed] [Google Scholar]
- 12.Koller H, Acosta F, Forstner R, Zenner J, Resch H, Tauber M, et al. C2-fractures: Part II. A morphometrical analysis of computerized atlantoaxial motion, anatomical alignment and related clinical outcomes. Eur Spine J. 2009;18:1135–53. doi: 10.1007/s00586-009-0901-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jefferson G. Fractures of the atlas vertebra: Report of four cases, and a review of those previously recorded. Br J Surg. 1920;7:407–22. [Google Scholar]
- 14.Segal LS, Grimm JO, Stauffer ES. Nonunion of fractures of the atlas. J Bone Joint Surg Am. 1987;69:1423–34. [PubMed] [Google Scholar]
- 15.Levine AM, Edwards CC. Traumatic lesions of the occipitoatlantoaxial complex. Clin Orthop Relat Res. 1989;239:53–68. [PubMed] [Google Scholar]
- 16.Chung SK, Park JT, Lim J, Park J. Open posterior reduction and stabilization of a C1 burst fracture using mono-axial screws. Spine (Phila Pa 1976) 2011;36:E301–6. doi: 10.1097/BRS.0b013e31820644cd. [DOI] [PubMed] [Google Scholar]
- 17.Kakarla UK, Chang SW, Theodore N, Sonntag VK. Atlas fractures. Neurosurgery. 2010;66:60–7. doi: 10.1227/01.NEU.0000366108.02499.8F. [DOI] [PubMed] [Google Scholar]
- 18.Koller H, Resch H, Tauber M, Zenner J, Augat P, Penzkofer R, et al. A biomechanical rationale for C1-ring osteosynthesis as treatment for displaced Jefferson burst fractures with incompetency of the transverse atlantal ligament. Eur Spine J. 2010;19:1288–98. doi: 10.1007/s00586-010-1380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hein C, Richter HP, Rath SA. Atlantoaxial screw fixation for the treatment of isolated and combined unstable jefferson fractures-experiences with 8 patients. Acta Neurochir (Wien) 2002;144:1187–92. doi: 10.1007/s00701-002-0998-2. [DOI] [PubMed] [Google Scholar]
- 20.Dickman CA, Greene KA, Sonntag VK. Injuries involving the transverse atlantal ligament: Classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery. 1996;38:44–50. doi: 10.1097/00006123-199601000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Spence KF, Jr, Decker S, Sell KW. Bursting atlantal fracture associated with rupture of the transverse ligament. J Bone Joint Surg Am. 1970;52:543–9. [PubMed] [Google Scholar]
- 22.Jo KW, Park IS, Hong JT. Motion-preserving reduction and fixation of C1 Jefferson fracture using a C1 lateral mass screw construct. J Clin Neurosci. 2011;18:695–8. doi: 10.1016/j.jocn.2010.08.033. [DOI] [PubMed] [Google Scholar]
- 23.Dvorak MF, Johnson MG, Boyd M, Johnson G, Kwon BK, Fisher CG. Long term health-related quality of life outcomes following Jefferson-type burst fractures of the atlas. J Neurosurg Spine. 2005;2:411–7. doi: 10.3171/spi.2005.2.4.0411. [DOI] [PubMed] [Google Scholar]
- 24.Abeloos L, De Witte O, Walsdorff M, Delpierre I, Bruneau M. Posterior osteosynthesis of the atlas for nonconsolidated Jefferson fractures: A new surgical technique. Spine (Phila Pa 1976) 2011;36:E1360–3. doi: 10.1097/BRS.0b013e318206cf63. [DOI] [PubMed] [Google Scholar]
- 25.Li L, Teng H, Pan J, Qian L, Zeng C, Sun G, et al. Direct posterior c1 lateral mass screws compression reduction and osteosynthesis in the treatment of unstable jefferson fractures. Spine (Phila Pa 1976) 2011;36:E1046–51. doi: 10.1097/BRS.0b013e3181fef78c. [DOI] [PubMed] [Google Scholar]
- 26.Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Zhang Y, et al. Direct repair of displaced anterior arch fracture of the atlas under microendoscopy: Experience with seven patients. Eur Spine J. 2012;21:347–51. doi: 10.1007/s00586-011-1965-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Conroy E, Laing A, Kenneally R, Poynton AR. C1 lateral mass screw-induced occipital neuralgia: A report of two cases. Eur Spine J. 2010;19:474–6. doi: 10.1007/s00586-009-1178-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stulík J, Klézl Z, Sebesta P, Kryl J, Vyskocil T. Occipitocervical fixation: Long term followup in fifty-seven patients. Acta Chir Orthop Traumatol Cech. 2009;76:479–86. [PubMed] [Google Scholar]
- 29.Bransford R, Chapman JR, Bellabarba C. Primary internal fixation of unilateral C1 lateral mass sagittal split fractures: A series of 3 cases. J Spinal Disord Tech. 2011;24:157–63. doi: 10.1097/BSD.0b013e3181e12419. [DOI] [PubMed] [Google Scholar]
- 30.Hu Y, Yang S, Xie H, He X, Xu R, Ma W, et al. The anatomic study on replacement of artificial atlanto-odontoid joint through transoral approach. J Huazhong Univ Sci Technolog Med Sci. 2008;28:327–32. doi: 10.1007/s11596-008-0322-3. [DOI] [PubMed] [Google Scholar]
- 31.Jones DC, Hayter JP. The superiorly based pharyngeal flap: A modification of the transoral approach to the upper cervical spine. Br J Oral Maxillofac Surg. 1997;35:368–9. doi: 10.1016/s0266-4356(97)90412-5. [DOI] [PubMed] [Google Scholar]
- 32.Al-Holou WN, Park P, Wang AC, Than KD, Marentette LJ. Modified trans-oral approach with an inferiorly based flap. J Clin Neurosci. 2010;17:464–8. doi: 10.1016/j.jocn.2009.08.015. [DOI] [PubMed] [Google Scholar]
- 33.Kingdom TT, Nockels RP, Kaplan MJ. Transoral-transpharyngeal approach to the craniocervical junction. Otolaryngol Head Neck Surg. 1995;113:393–400. doi: 10.1016/S0194-59989570074-9. [DOI] [PubMed] [Google Scholar]


