Abstract
Median nerve injury is rarely associated with the humeral shaft fracture. A Sixty two year old woman with a displaced humeral shaft fracture, developed a symptomatic carpal tunnel syndrome after plating with a screw protruding medially. 16 months later, the implants were removed and the symptoms gradually improved without carpal tunnel release surgery. A double crush syndrome resulted due to the proximal compression by the medially protruding screw and the distal compression by carpal tunnel. The proximal decompression produced by removal of the screw led to relief of the symptoms.
Keywords: Carpal tunnel syndrome, double crush syndrome, humeral shaft fracture, median nerve
INTRODUCTION
Double crush syndrome is referrs to the coexistence of dual compressions along the course of a peripheral nerve. A proximal compression may lessen the ability of the nerve to withstand a distal one.1 When involving median nerve, the coexistence of carpal tunnel syndrome (CTS) and cervical radiculopathy is the type of double crush syndrome with the highest frequency.2 Except for the nerve roots, any other sites proximal to carpal tunnel along the median nerve can also serve as the proximal compression sites. We present a patient who developed a symptomatic CTS after plating of the humeral shaft fracture.
CASE REPORT
A 62 year old woman sustained a closed fracture of right humeral shaft resulting from a car accident (OTA 12A3). We performed the open reduction and internal fixation through an anterolateral approach under general anesthesia and placed a 4.5 mm dynamic compression plate on the lateral aspect of the humerus. The placement of the implants was good except that the tip of the most proximal screw protruding approximately 1 cm through the medial cortex [Figure 1]. During in-hospital treatment, the patient recovered without complaining any discomfort of the right hand. 4 weeks postoperatively, however, she began to feel tingling over the thumb, index and middle fingers of the right hand, which was worse at night. The symptoms gradually progressed with thumb-index finger pinch weakness. When coming to our clinics 3 months postoperatively, she presented a sensory deficit of those fingers. Both Tinel's sign over carpal tunnel and Phalen's test were positive, as well as atrophy of the thenar muscles. She did not experience such symptoms prior to surgery to the humerus fracture. The neurophysiological study confirmed the clinical suspicion of CTS, with a prolonged distal latency and low amplitude of compound muscle action potential, so did the sensory nerve [Figure 2]. The neurophysiological finding of the proximal median nerve and ipsilateral ulnar nerve was normal. The criteria for electro-diagnosis of CTS included: Distal median motor latency >4.4 ms; difference between distal motor latency of median and ulnar nerve >1.1 ms; difference between distal sensory latency of median and ulnar nerve >0.2 ms.3 Although a transient improvement was observed with night splint treatment, the symptoms recurred after a few weeks. A carpal tunnel decompression was therefore recommended but the patient refused.
Figure 1.

(a) Preoperative (b) postoperative radiographs of the humerus showing humeral shaft fracture. Note that the most proximal screw protrudes through the anteromedial cortex
Figure 2.
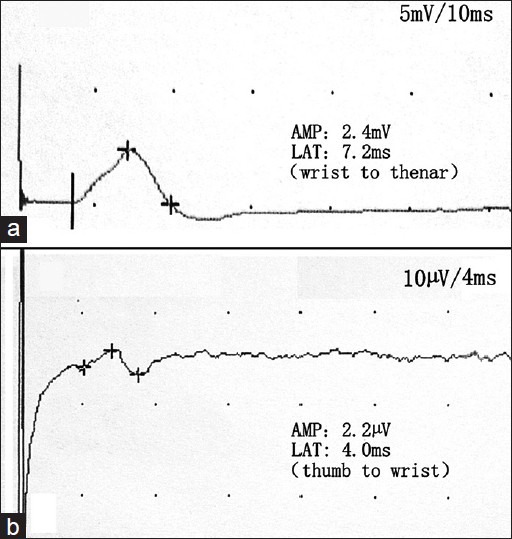
The right median nerve conduction study showed a low amplitude compound muscle action potential (a) and sensory nerve action potential (b) with a prolonged latency. For motor nerve study, recording electrode was over the abductor pollicis brevis muscle, with stimulation at the wrist radial to palmaris longus. For sensory nerve study, thumb was stimulated with ring electrode and response was recorded at the wrist. AMP, amplitude; LAT, latency
At 16 months postoperatively, the patient asked for removal of the implants. During the operation, we observed that the tip of the protruding screw twisted the median nerve with scar tissues. Extensive neurolysis around the median nerve was not performed, because we did not expect relief of symptoms of CTS after removal of the implants. At 2 weeks later, however, the patient experienced a significant relief of the tingling over fingers. At last review, 6 months after the implants removal, her sensations returned to near normal with full movement of the fingers. Although mild thenar atrophy was still present, the patient remained asymptomatic and denied additional carpal tunnel decompression surgery as she had no great difficulty in carrying out her daily activities.
DISCUSSION
A humeral shaft fracture is usually associated with radial nerve palsy, A review by Shao et al. reported an average rate of 11.8%.4 On the contrary, the injuries of the median nerve with fractures of the humeral shaft are extremely unusual, because it is protected from direct contact with bone by several muscles including the brachialis and coracobrachialis. Macnicol reported a case of the median nerve palsy after a humeral shaft fracture in a 10-year-old girl, who fell from a pony.5 Veilleux and Richardson also reported a case of median neuropathy associated with a humeral neck fracture.6
Our case developed a CTS 4 weeks after plating of the humeral shaft fracture. If it was not a coincidence, several potential causative factors might be involved in the presence of the CTS. The swelling of the limb after surgery might increase the pressure of carpal tunnel. The postoperative immobilization decreased the use of the muscle pump and caused an additional entrapment of the median nerve. However, the immobilization or swelling could not explain the rapid improvement of the numbness after removal of the implants. The clinical effects caused by intraoperative injuries, such as drilling, surgical stretch or compression, would usually be noticed immediately postoperative.
Therefore, we speculated that the symptoms of CTS were caused by the implants of the humeral shaft, i.e. a double crush syndrome might account for it. The theory of double crush syndrome emphasizes that the damage produced by the dual compression exceeds the additive damage caused by each low grade compression.2 Although there were still some controversies about the mechanism of coexistence of CTS and cervical radiculopathy, the theory of double crush syndrome had been proved in the model of dual compressions on a single nerve pathway.7,8 Regarding this case, the tip of a screw protruded 1 cm through the medial cortex at the middle of the humerus shaft after fracture plating, where the median nerve courses distally. It was extremely likely that the protruding screw produced a subclinical compression of the median nerve. The intraoperative exploration during the implants removal also observed the contact between the screw and nerve. Although the proximal compression was very slight, the susceptibility to compression of the median nerve might be increased at the carpal tunnel level. The scar formation surrounding the humerus limited the mobility of the nerve and resulted in further deterioration of the proximal compression. Ultimately, the additive effect of these factors converted a subclinical CTS into a clinically evident one and a double crush syndrome of the median nerve developed.
In management of double crush syndrome, whether proximal or distal compression should be treated first, is still controverial, given that there are few reported series with specific scrutiny of both conditions.9 In this case, it would have been more logical to do a carpal tunnel decompression if the patient agreed. However, most Chinese patients prefer to have the implants removed after the fracture. Interestingly, the symptoms also relieved after removal of the medially protruding screw. The relief of symptoms can be explained by decompression of the proximal median nerve. The incomplete recovery of the thenar atrophy may be related to the long period of the compression.
The report has some limitations. The picture of the screw entangling the nerve and causing nerve compression was not presented, as we did not expect that the implants removal could relieve the CTS symptoms. Furthermore, we did not record the picture of the affected hand evidencing CTS.
This study described a case of symptomatic CTS caused by the protruding screw in arm. Placement of any screw with excessive length should be avoided during the internal fixation of the humeral shaft fracture.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Upton AR, McComas AJ. The double crush in nerve entrapment syndromes. Lancet. 1973;2:359–62. doi: 10.1016/s0140-6736(73)93196-6. [DOI] [PubMed] [Google Scholar]
- 2.Osterman AL. The double crush syndrome. Orthop Clin North Am. 1988;19:147–55. [PubMed] [Google Scholar]
- 3.Sharma G. Detection of median nerve entrapment in the carpal tunnel by electrodiagnostic techniques. Calicut Med J. 2010;8:e3. [Google Scholar]
- 4.Shao YC, Harwood P, Grotz MR, Limb D, Giannoudis PV. Radial nerve palsy associated with fractures of the shaft of the humerus: A systematic review. J Bone Joint Surg Br. 2005;87:1647–52. doi: 10.1302/0301-620X.87B12.16132. [DOI] [PubMed] [Google Scholar]
- 5.Macnicol MF. Roentgenographic evidence of median-nerve entrapment in a greenstick humeral fracture. J Bone Joint Surg Am. 1978;60:998–1000. [PubMed] [Google Scholar]
- 6.Veilleux M, Richardson P. Proximal median neuropathy secondary to humeral neck fracture. Muscle Nerve. 2000;23:426–9. doi: 10.1002/(sici)1097-4598(200003)23:3<426::aid-mus15>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 7.Nemoto K, Matsumoto N, Tazaki K, Horiuchi Y, Uchinishi K, Mori Y. An experimental study on the “double crush” hypothesis. J Hand Surg Am. 1987;12:552–9. doi: 10.1016/s0363-5023(87)80207-1. [DOI] [PubMed] [Google Scholar]
- 8.Lo SF, Chou LW, Meng NH, Chen FF, Juan TT, Ho WC, et al. Clinical characteristics and electrodiagnostic features in patients with carpal tunnel syndrome, double crush syndrome, and cervical radiculopathy. Rheumatol Int. 2012;32:1257–63. doi: 10.1007/s00296-010-1746-1. [DOI] [PubMed] [Google Scholar]
- 9.Galarza M, Gazzeri R, Gazzeri G, Zuccarello M, Taha J. Cubital tunnel surgery in patients with cervical radiculopathy: Double crush syndrome? Neurosurg Rev. 2009;32:471–8. doi: 10.1007/s10143-009-0219-z. [DOI] [PubMed] [Google Scholar]


