Abstract
Introduction:
Diabetes is a chronic disease; it can cause serious complications. Diabetes self-management is essential for prevention of disease complications. This study was conducted to evaluate self-management promotion educational program intervention efficiency among diabetic patients in Iran and health belief model (HBM) was applied as a theoretical framework.
Materials and Methods:
Overall, 120 Type 2 diabetic patients referred to rural health centers in Gachsaran, Iran participated in this study as randomly divided into intervention and control group. This was a longitudinal randomized pre- and post-test series control group design panel study to implement a behavior modification based intervention to promotion self-management among diabetic patients. Cross-tabulation and t-test by using SPSS statistical package, version 16 was used for the statistical analysis.
Results:
Mean age was 55.07 years (SD = 9.94, range: 30-70). Our result shows significant improvements in average response for susceptibility, severity, benefit and self-management among intervention group. Additionally, after intervention, average response of the barrier to self-management was decreased among intervention group.
Conclusion:
Our result showed education program based on HBM was improve of self-management and seems implementing these programs can be effective in the and prevention of diabetes complications.
Keywords: Health belief model, self-management, Type 2 diabetic's patient
INTRODUCTION
Diabetes is the most common chronic disease with devastating complications, and the Middle East is expected to bear one of the greatest burdens of diabetes worldwide in the coming decades.[1] Type 2 diabetes can lead to complications such as heart disease, stroke, renal failure, amputation, and blindness.[2] It also presents a substantial socioeconomic and quality of life burden, mainly as a consequence of its chronic complications.[3] Diabetes is a main contributor to morbidity and mortality and generates enormous direct and indirect costs.[4] There are very different diabetes statistical records in Iran. It's estimated that prevalence of diabetes in population is about 2.3%.[5] Diabetes can be controlled by creating awareness of diabetes risk factors and symptoms, and counseling patients on diet, exercise, blood sugar monitoring, oral medication taking, and tablets or insulin use.[6] Control of diabetes requires the normalization of carbohydrate, protein, and fat metabolism.[7] Patient lifestyle and health behavior changes, and patient self-management in agreement with professional treatment guidance, are cornerstones of diabetes.[8] Diabetic Patients are expected to carry out daily self-management activities to help to avoid diabetes-related morbidity and mortality. Self-management is a basis of diabetes care, and it is believed that improving patient self-efficacy is a crucial pathway to improved self-management.[9] Educational programs are a significant demand on health care providers, requiring large blocks of time (generally uncompensated), specific training, teaching and communication skills, a supportive attitude, and a readiness to listen and negotiate. Therefore, effective education requires training in its delivery.[3] The American diabetes association estimates that the complications, and the costs of diabetes can be reduced dramatically by increasing awareness and improving prevention.[10] In order to understand and predict fulfillment, the patients’ attitude toward diabetes has been studied since more than twenty years by means of the health belief model (HBM).[11] At first, the HBM was designed to understand why people at risk to a disease did not contribute in the disease diagnosis program. According to the HBM, a subject is more likely to take a “health action” if he perceives; he is at risk; the disease is severe; health action is beneficial; understands limited barriers to the health action and receives a cue to get the health action.[12] So; people with diabetes will adhere to treatment plans if they be worried about their health and believe that they are susceptible to problems, diabetes could have serious consequences, and following medical recommendations will reduce threats, and believe that the benefits outweigh the costs of not adhering.[13] Becker and Janz[14] have urged researchers to use the HBM as a framework for understanding and enhancing patient adherence to the diabetes treatment regimen. They concluded that focusing on relevant identified attitudes, and beliefs will aid in the treatment of people with diabetes. Diabetes management and education programs have been shown to have a significant impact on improving health outcomes.[15] The purpose of this study is evaluating self-management promotion educational program intervention efficiency among Type 2 diabetic patients in Gachsaran, Iran during 2009 and HBM was applied as the theoretical framework.
MATERIALS AND METHODS
Participants
This study was conducted among Type 2 diabetics patient in Gachsaran, Iran. Four health centers randomly selected within all health centers in Gachsaran, Iran. Of the 406 Type 2 diabetic's patient enrolled at the four health centers, 120 (29.5%) patient participated in this study. Sixty participants as intervention and 60 as control groups were enrolled at the baseline survey, of who all were followed up after 2 month intervention. This study was conducted with approval from Tehran University of Medical Sciences’ institutional review board. Informed assent and consent were obtained from participants.
Measures
Prior to conducting the main project a pilot study was carried out. Initially, the relevant questionnaires were administered to 30 diabetic's patients who were similar to participants in the main study to obtain feedback about the clarity, length comprehensiveness, time of completion, and also internal reliability of the measures. Moreover, participants were instructed about how to fill questioners before gathering information. Participants responded to the standard writing questionnaire. Information was collected from an interview.
Questionnaire included three sections that comprised of 58 questions: Seven questions for demographic features; 36 questions for HBM variable; 15 questions about self-management behavior (including: Smoke use, physical activity, foot care, measurement of blood glucose, dietary intake, weight regular monitoring, and using medical advice).
Demographics
Background item was designed to gather information related to age (years), gender (men, women), job (housewife, farmer, unemployed, others), duration of diabetes (years), complications of diabetes (yes, no), educational status (elementary, guidance, diploma) and marital status (single, married, widow).
Health belief model variable
The items which assessed components of the HBM with use two standard questionnaires[16,17] and 36 items were composed under four major constructs, (1) perceived susceptibility; (2) perceived severity; (3) perceived benefit; (4) perceived barrier; (5) perceived self-efficacy. Four items were designed to measure perceived susceptibility (e.g. “I do not get diabetes complications”). Ten items were designed to measure perceived severity (e.g. “I think that diabetes is a serious disease”). Six items were designed to perceive benefit of self-efficacy to self-management (e.g. “Proper diabetic diet is effective for control blood sugar”). Ten items were designed to evaluate perceived barrier to self-management (e.g. “Diet for diabetics is annoying me”). Six items were designed to perceived self-efficacy to self-management (e.g. “How you sure the ability to diabetic diet?”). In order to facilitate respondents’ responses to the items, all items were standardized to a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). For self-efficacy scale, ranging from 1 (very little) to 5 (very much). Estimated reliability coefficients for each HBM constructs questionnaires were as follows: Severity (α = 0.69); susceptibility (α = 0.71); barrier (α = 0.62); benefit (α = 0.75); self-efficacy (α = 0.76), and knowledge (α = 0.66). These results demonstrated that questionnaires were internally consistent.
Procedure
This was a longitudinal randomized pre- and post-test series control group design panel study to implement a health education based intervention to improved self-management behaviors among a sample of Type 2 diabetic's patient recruited from four health centers randomly selected within all health centers in Gachsaran, Iran. After obtaining informed consent participants were enrolled in the study, a 58-item, structured questionnaire with the aforementioned measures was distributed to the patient to complete. Prior to the self-administration of the questionnaire, study staff explained the logistics of answering the different type of questions and clarified any concerns and questions that were raised by participants. Most participants have a low education, so data collection was based on an interview with them.
Educational program
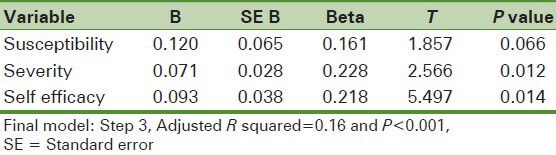
The course included 6 weekly teaching (a lecture and group discussion) units (45-60 min each). An educational program was adjusted based on HBM. For education needs assessment in participation linear regression analysis was performed. Our result showed susceptibility, severity, and self-efficacy were the best factor to prediction self-management [Table 1]. Thus, education programs were focused on these structures. The first and second teaching unit acquainted patients with the interactive group method, and education abut Type 2 diabetes complications (to improve patients’ susceptibility). The main topics discussed during the third teaching unit were foot care (to improve patients’ severity). The main topics discussed during the fourth teaching unit were regular physical activity (to improve patients’ self-efficacy). The fifth teaching unit were discussed about smoking complications in diabetic patients (to improve patients’ severity). The sixth teaching unit were discussed about nutrition and diet education (to improve patients’ self-efficacy).
Table 1.
Predictors of the health belief model variables in self-management among the participant
Educational planning for this study was based on active learning through educational intervention was attempted to patients actively participate in educational programs. Majority of participants in the study had low educational; therefore, a 2 h training session for their families was performed than the role of facilitator training.
Furthermore, training manual entitled “prevention of diabetic complications” by the research team designed to provide family intervention group patients were placed.
Statistical analysis
Analyses were conducted by using SPSS-16 and a probability level of 0.05 was used throughout. Chi-squared and t-test were employed to determine comparability of the intervention and control group.
RESULTS
Average of age was 55.07 years (SD = 9.94, range: 30-70). (Intervention group: 55.26 years and control group: 54.88 years). Regarding the educational status: 74.3% (n = 89) had elementary school, 27.7% guidance school (n = 20) and 9.2% (n = 11) had a diploma.
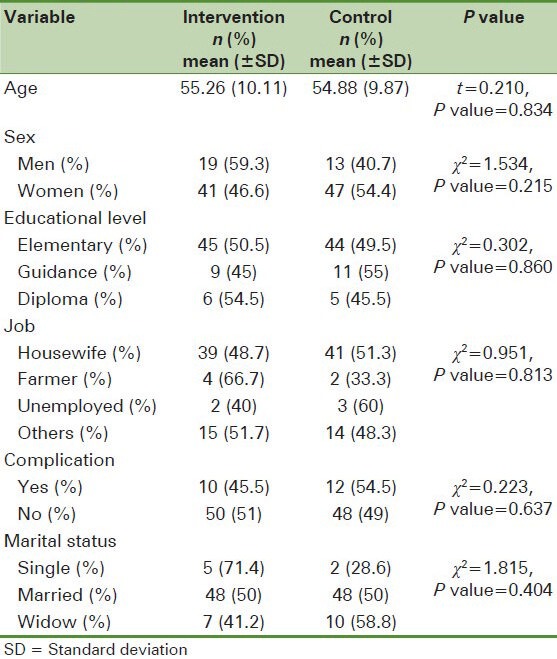
Table 2 shows not significant differences between two intervention and control groups in demographic characteristics (age, sex, educational level, disease duration, occupation, and marital status) of them before implementation of the educational program.
Table 2.
Pretest equivalency results for intervention and control groups
As can be seen in Table 1 for education needs assessment in participation linear regression analysis was performed to explain the variation in self-management, and our results showed on 3rd step the procedure stopped and the best model was selected, among the HBM constructs: Susceptibility, severity and self-efficacy were accounted for 16% of the self-management variation.
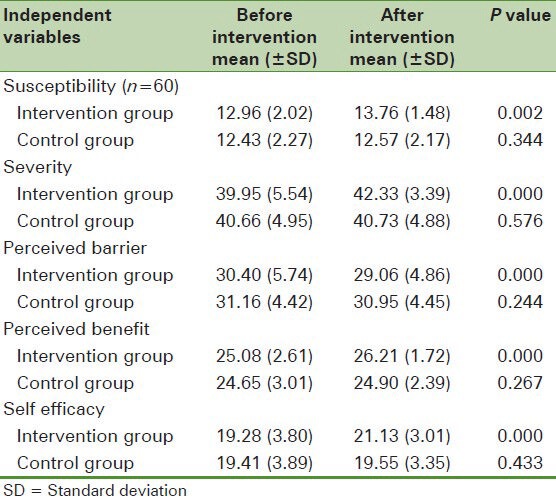
Table 3 indicates that there are significant improvements in average response for independent variables among Type 2 diabetic patient who were under intervention. As it shown in table average response for severity was 39.95 that it was increased to 42.33, susceptibility was 12.96 that it was increased to 13.76, benefit of self-management was 25.08 that it was increased to 26.21, self-efficacy was 19.28 that it was increased to 21.13 after intervention. Also average response to the barrier to self-management was 30.40 that it was decreased to 29.06 after intervention.
Table 3.
Average responses for health belief model variables about self-management before and after educational program
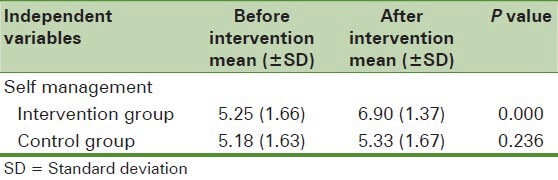
Additionally, Table 4 shows the result abut efficiency of self-management education program and our result show the average response for self-management improved from 5.25 to 6.90 after implementing educational program.
Table 4.
Average responses diabetes self-management behavior before and after educational program
DISCUSSION
The management of diabetes self-care is mainly related to the patients’ compliance. Hence, improvement of patients’ knowledge and their self-care skill is a fundamental strategy for controlling diabetes and its complications.[1] The aim of this study was to assess the effectiveness of a self-management education program among Type 2 diabetic patient. The HBM was conducted as a theoretical framework to assess educational need assessment among participants. Even though the duration of the educational intervention in this study was short, it was found significant improvements after manipulation. Analysis of the baseline and 2 months follow-up clearly demonstrated significant intervention effects on the participants’ severity, susceptibility, benefit, barrier, self-efficacy, and self-management among the intervention group.
Previous studies show that understanding the symptoms’ severity and susceptibility to these effects can lead to adopt a higher level of self-care among diabetic patients.[18,19] Our results show usefulness of the educational intervention program for increased susceptibility and severity among diabetic patients and consistent with similar studies.[16,20]
Aalto[21] and Bernal[22] reported a significant relationship between perceived benefits and perceived barriers and diabetes self-care behaviors our findings indicated that improve benefit and reduce barrier to self-management among participants, and these outcomes is consistent with similar studies.[5,16]
Also Bernal[22] reported presence in the diabetes education class is associated with perception of self-efficacy. In this regards our findings showed that education program could improve average response for participants’ self-efficacy.
One reason for the poor outcomes in individuals with diabetes is the lack of participation in the treatment of the disease. This participation is a key success factor in the treatment of diabetes that demands motivation, knowledge, and compliance to a difficult and complex lifetime regimen. Diabetes self-management education is a key element in preventing and treating diabetes,[3] and promotion of self-management the main objective of programs among diabetic patients.[16] Our result shows a significant increase in mean scores of self-management (6.06-7.25) among patient's intervention group, and it is similar to others study.[5,16]
Overall, findings of the current study supported that implementing the self-management education programs among Type 2 diabetic patient would be effective to improve self-management among them.
Although our study has several strengths, such as theory driven, interventional study, and educational program was adjusted based on educational need assessment the study are few limited. First, data collection was based on an interview with diabetic patients; this is maybe prone to recall bias. Second, the internal consistency the questionnaire was relatively low (α =0.62) for assessing perceived barrier to self-management. Focused on the specifically self-management behaviors and the use of other behavior change model in predicting health-related behaviors in Iranian patients recommended at future research.
ACKNOWLEDGMENTS
This article is a part of the research project supported by Tehran University of Medical Sciences. We would like to thank Deputy of Research of Tehran University of Medical Sciences for financial support of this study.
Footnotes
Source of Support: This research was supported by funding from the deputy of research of Tehran University of Medical Sciences [number research: 318].
Conflict of Interest: None declared
REFERENCES
- 1.Yekta Z, Pourali R, Aghassi MR, Ashragh N, Ravanyar L, Rahim Pour MY. Assessment of self-care practice and its associated factors among diabetic patients in Urban Area of Urmia, Northwest of Iran. J Res Health Sci. 2011;11:33–8. [PubMed] [Google Scholar]
- 2.Lawton J, Ahmad N, Hanna L, Douglas M, Hallowell N. ‘I can’t do any serious exercise’: Barriers to physical activity amongst people of Pakistani and Indian origin with Type 2 diabetes. Health Educ Res. 2006;21:43–54. doi: 10.1093/her/cyh042. [DOI] [PubMed] [Google Scholar]
- 3.Gagliardino JJ, Etchegoyen G PENDID-LA Research Group. A model educational program for people with type 2 diabetes: A cooperative Latin American implementation study (PEDNID-LA) Diabetes Care. 2001;24:1001–7. doi: 10.2337/diacare.24.6.1001. [DOI] [PubMed] [Google Scholar]
- 4.Baptiste-Roberts K, Gary TL, Beckles GL, Gregg EW, Owens M, Porterfield D, et al. Family history of diabetes, awareness of risk factors, and health behaviors among African Americans. Am J Public Health. 2007;97:907–12. doi: 10.2105/AJPH.2005.077032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hazavehei SM, Sharifirad G, Mohebi S. The effect of educational program based on health belief model on diabetic foot care. Int J Diabetes Dev Ctries. 2007;27:18–23. [Google Scholar]
- 6.Ratanasuwan T, Indharapakdi S, Promrerk R, Komolviphat T, Thanamai Y. Health belief model about diabetes mellitus in Thailand: The culture consensus analysis. J Med Assoc Thai. 2005;88:623–31. [PubMed] [Google Scholar]
- 7.Esscot-Stump S, Mahan LK. Krause's Food, Nutrition and Diet Therapy. 9th ed. Philadelphia: WB Saunders Company Publisher; 1996. Medical nutrition for diabetes mellitus and hypoglycaemia of nondiabetic origin; pp. 69–82. [Google Scholar]
- 8.van Dam HA, van der Horst FG, Knoops L, Ryckman RM, Crebolder HF, van den Borne BH. Social support in diabetes: A systematic review of controlled intervention studies. Patient Educ Couns. 2005;59:1–12. doi: 10.1016/j.pec.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29:823–9. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- 10.Pinto SL, Lively BT, Siganga W, Holiday-Goodman M, Kamm G. Using the Health Belief Model to test factors affecting patient retention in diabetes-related pharmaceutical care services. Res Social Adm Pharm. 2006;2:38–58. doi: 10.1016/j.sapharm.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Wens J, Vermeire E, Royen PV, Sabbe B, Denekens J. GPs’ perspectives of type 2 diabetes patients’ adherence to treatment: A qualitative analysis of barriers and solutions. BMC Fam Pract. 2005;6:20. doi: 10.1186/1471-2296-6-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wai CT, Wong ML, Ng S, Cheok A, Tan MH, Chua W, et al. Utility of the Health Belief Model in predicting compliance of screening in patients with chronic hepatitis B. Aliment Pharmacol Ther. 2005;21:1255–62. doi: 10.1111/j.1365-2036.2005.02497.x. [DOI] [PubMed] [Google Scholar]
- 13.Chapman KM, Ham JO, Liesen P, Winter L. Applying behavioral models to dietary education of elderly diabetic patients. J Nutr Educ. 1995;27:75–9. [Google Scholar]
- 14.Becker MH, Janz NK. The health belief model applied to understanding diabetes regimen compliance. Diabetes Educ. 1985;11:41–7. [Google Scholar]
- 15.Philis-Tsimikas A, Walker C, Rivard L, Talavera G, Reimann JO, Salmon M, et al. Improvement in diabetes care of underinsured patients enrolled in project dulce: A community-based, culturally appropriate, nurse case management and peer education diabetes care model. Diabetes Care. 2004;27:110–5. doi: 10.2337/diacare.27.1.110. [DOI] [PubMed] [Google Scholar]
- 16.Molaei TA, Eftekhar H, Mohammad K. Application of health belief model to behavior change of diabetic patients. Payesh. 2005;4:263–9. [Google Scholar]
- 17.Kartal A, Ozsoy SA. Validity and reliability study of the Turkish version of Health Belief Model Scale in diabetic patients. Int J Nurs Stud. 2007;44:1447–58. doi: 10.1016/j.ijnurstu.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 18.Daniel M, Messer LC. Perceptions of disease severity and barriers to self-care predict glycemic control in Aboriginal persons with type 2 diabetes mellitus. Chronic Dis Can. 2002;23:130–8. [PubMed] [Google Scholar]
- 19.Tan MY. The relationship of health beliefs and complication prevention behaviors of Chinese individuals with Type 2 Diabetes Mellitus. Diabetes Res Clin Pract. 2004;66:71–7. doi: 10.1016/j.diabres.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 20.Aljasem LI, Peyrot M, Wissow L, Rubin RR. The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Diabetes Educ. 2001;27:393–404. doi: 10.1177/014572170102700309. [DOI] [PubMed] [Google Scholar]
- 21.Aalto AM, Uutela A. Glycemic control, self-care behaviors, and psychosocial factors among insulin treated diabetics: A test of an extended health belief model. Int J Behav Med. 1997;4:191–214. doi: 10.1207/s15327558ijbm0403_1. [DOI] [PubMed] [Google Scholar]
- 22.Bernal H, Woolley S, Schensul JJ, Dickinson JK. Correlates of self-efficacy in diabetes self-care among Hispanic adults with diabetes. Diabetes Educ. 2000;26:673–80. doi: 10.1177/014572170002600415. [DOI] [PubMed] [Google Scholar]


