Case Report
An otherwise healthy woman, age 67 years, presented in 2009 with the complaint of loose, nonbloody stools of 2 months’ duration. The patient reported having up to 6 bowel movements daily that sometimes occurred at night and were accompanied by lower abdominal cramping and urgency. The symptoms were not associated with food intake. The patient took aspirin but no other nonsteroidal anti-inflammatory drugs (NSAIDs). The symptoms were partially relieved by loperamide. Physical examination findings were unremarkable. Infectious causes as well as celiac disease were ruled out. A colonoscopy was planned for further evaluation.
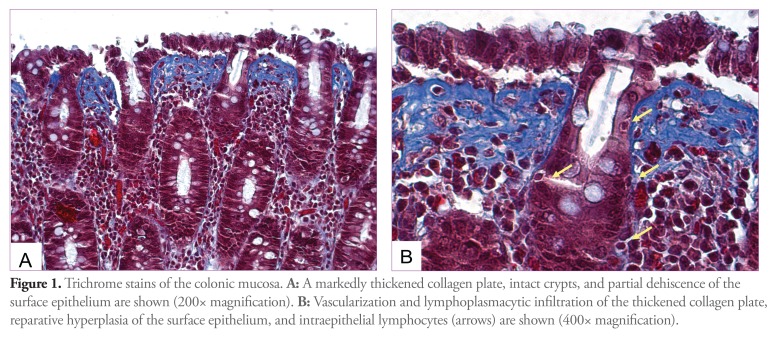
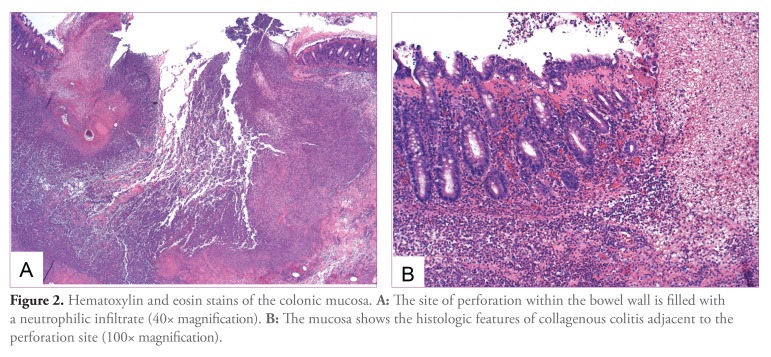
Prior to the colonoscopy, the patient was admitted to the hospital with abdominal pain, diarrhea, and rigors. A computed tomography scan of the abdomen revealed bowel wall thickening at the splenic flexure with pockets of extraluminal air and pneumatosis. There was no evidence of diverticular disease. The patient underwent partial colectomy and transverse colostomy with a mucus fistula. Surgical pathology revealed colonic mucosa with a thickened subepithelial collagen plate consistent with collagenous colitis (Figures 1 and 2).
Figure 1.
Trichrome stains of the colonic mucosa. A: A markedly thickened collagen plate, intact crypts, and partial dehiscence of the surface epithelium are shown (200x magnification). B: Vascularization and lymphoplasmacytic infiltration of the thickened collagen plate, reparative hyperplasia of the surface epithelium, and intraepithelial lymphocytes (arrows) are shown (400x magnification).
Figure 2.
Hematoxylin and eosin stains of the colonic mucosa. A: The site of perforation within the bowel wall is filled with a neutrophilic infiltrate (40x magnification). B: The mucosa shows the histologic features of collagenous colitis adjacent to the perforation site (100x magnification).
Postoperatively, the patient continued to have frequent loose stools from her ostomy. Endoscopic findings from a colonoscopy through the stoma in January 2010 were normal, but pathology again demonstrated collagenous colitis. In March 2010, the patient underwent takedown of her stoma and colo-colonic anastomosis. The patient continued to have frequent loose stools. She received 2 courses of budesonide in 2010 and was later treated with a short course of mesalamine. Her diarrhea resolved, and she now has formed daily bowel movements and no longer requires pharmacotherapy.
Discussion
Collagenous colitis is a relatively uncommon but increasingly diagnosed form of microscopic colitis. First described in 2 independent reports in 1976,1,2 it is characterized by a clinical syndrome of chronic or recurrent watery diarrhea and a grossly normal appearance of colonic mucosa on colonoscopy. The diagnosis is made histologically by the presence of increased intraepithelial lymphocytes and mixed inflammatory cells in the lamina propria and a pathognomonic appearance of a thickened subepithelial collagen band.3 This deposition of collagen distinguishes collagenous colitis from lymphocytic colitis (the other major subtype of microscopic colitis), although some researchers have suggested that the 2 entities may be part of the same spectrum of disease.4
Microscopic colitis most commonly affects women in their fifth and sixth decades of life.3-5 Several medications have been implicated as contributing factors, notably aspirin and other NSAIDs, histamine 2 receptor blockers, proton pump inhibitors, and certain selective serotonin reuptake inhibitors.6 Autoimmune conditions, including rheumatoid arthritis, thyroid disorders, and celiac disease, are associated with microscopic colitis.4 Family history and cigarette smoking also may be risk factors, and postinfectious and paraneoplastic cases have been described.3,4
The natural history of disease is typically benign, with intermittent periods of nonbloody, watery diarrhea that can resolve spontaneously, although some patients can have persistent symptoms.3-5,7 Symptoms may mimic irritable bowel syndrome, and a recent retrospective study suggested that microscopic colitis may be an underdiagnosed cause of chronic diarrhea.5
There are several treatment options, including discontinuation of potential triggering medications (noted above) or use of antidiarrheal medications, bismuth subsalicylate, mesalamine, or budesonide.3,4 A recent meta-analysis demonstrated the efficacy of budesonide in inducing clinical and histologic remission of microscopic colitis.8 Refractory disease can be treated with immunosuppressive drugs and, very rarely, surgery.4,9
Although uncommon, serious complications involving the integrity of the bowel wall have been reported in patients with collagenous colitis. Endoscopically apparent mucosal defects, including longitudinal tears and deeper “fractures,” have been described.10-13 Colonic perforation and peritonitis following barium enema or colonoscopy have been reported in several small case series.7,10-13 There are 2 previously reported cases of spontaneous colonic perforation in patients with collagenous colitis.14,15
The present case illustrates spontaneous perforation of the colon, a very rare complication of collagenous colitis. This is only the third such case reported in the literature. The patient did not have any other apparent risk factors for perforation, and the only findings at the time of laparotomy and on pathology were those consistent with collagenous colitis. Prior to the development of an acute abdomen necessitating partial colectomy, the patient had had the typical symptoms of microscopic colitis for 2 months.
Several recent case series have described colonic perforations and mucosal tears in patients with collagenous colitis undergoing colonoscopy or barium enema.7,10-16 Although descriptions of colonoscopic findings were not available in all cases and were normal in other cases, many of the reported perforations were associated with linear mucosal tears.7,11-13,16 Although these mucosal abnormalities were observed in all parts of the colon, a disproportionate number occurred in the right colon, which is consistent with the available evidence and suggests that collagenous colitis has a right-sided predilection.11,12 Interestingly, in the 2 previously reported cases of spontaneous perforation, as well as in the present case, perforation occurred in the left colon (Table).
Table.
Demographics of Reported Cases of Spontaneous Bowel Perforation in Patients with Collagenous Colitis
| Case | Patient age (yrs) | Comorbidities and risk factors | Medications | Location of perforation | Surgical outcome |
|---|---|---|---|---|---|
| Freeman HJ, et al14 | 37 | None | None | Sigmoid colon | Exploratory laparotomy, no resection |
| Bohr J, et al15 | 56 | Depression, tobacco use | Clomipramine, herbal colon cleanser | Splenic flexure/ descending colon | Segmental resection and anastomosis |
| Present case | 67 | None | Aspirin | Splenic flexure | Partial colectomy and transverse colostomy with subsequent anastomosis |
These recent descriptions of endoscopically visible mucosal defects in patients with collagenous colitis are of considerable interest; when observed, they raise the possibility of this diagnosis, which previously could only be made microscopically.
A recent review of this subject strove to categorize endoscopic findings from the small case series that make up the current body of knowledge and reported 4 patterns of mucosal abnormalities: pseudomembranes; an indistinct or crowded appearance of vasculature; mucosal abnormalities, such as red spots or nodularity; and a continuum of characteristic linear mucosal tears, including a “cat scratch” pattern and thicker scarred “fractures.”10 The authors of the review noted that such findings were only visible in a small percentage of cases of collagenous colitis and may not always be distinguishable from similar findings in other conditions10; however, their presence should alert endoscopists to the increased risk of complications, including perforation.10,11
Summary
Although rare, the risk of mucosal tearing and colonic perforation in patients with collagenous colitis represents a severe and life-threatening extreme of a continuum of illness typically thought of as benign. The present case serves to illustrate the importance of considering the diagnosis of collagenous colitis in patients with chronic non-bloody diarrhea, especially in the high-risk demographic of middle-aged and elderly women.
References
- 1.Freeman HJ, Weinstein WM, Shnitka TK, Wensel RH, Sartor VE. Watery diarrhea syndrome associated with a lesion of the colonic basement membrane (CD)-lamina propria (LP) interface. Ann R Coll Phys Surg Can. 1976;9:45. [Google Scholar]
- 2.Lindstrom CG. Collagenous colitis with watery diarrhea—a new entity? Pathol Eur. 1976;11:87–89. [PubMed] [Google Scholar]
- 3.Freeman HJ. Collagenous mucosal inflammatory diseases of the gastrointestinal tract. Gastroenterology. 2005;129:338–350. doi: 10.1053/j.gastro.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 4.Pardi DS, Kelly CP. Microscopic colitis. Gastroenterology. 2011;140:1155–1165. doi: 10.1053/j.gastro.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Mohamed N, Marais M, Bezuidenhout J. Microscopic colitis as a missed cause of chronic diarrhea. World J Gastroenterol. 2011;17:1996–2002. doi: 10.3748/wjg.v17.i15.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beaugerie L, Pardi DS. Review article: drug-induced microscopic colitis—proposal for a scoring system and review of the literature. Aliment Pharmacol Ther. 2005;22:277–284. doi: 10.1111/j.1365-2036.2005.02561.x. [DOI] [PubMed] [Google Scholar]
- 7.Freeman HJ. Complications of collagenous colitis. World J Gastroenterol. 2008;14:1643–1645. doi: 10.3748/wjg.14.1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chande N, Macdonald JK, McDonald JW. Interventions for treating microscopic colitis: a Cochrane Inflammatory Bowel Disease and Functional Bowel Disorders Review Group systematic review of randomized trials. Am J Gastroenterol. 2009;104:235–241. doi: 10.1038/ajg.2008.16. [DOI] [PubMed] [Google Scholar]
- 9.Williams RA, Gelfand DV. Total proctocolectomy and ileal pouch anal anastomosis to successfully treat a patient with collagenous colitis. Am J Gastroenterol. 2000;95:2147. doi: 10.1111/j.1572-0241.2000.02225.x. [DOI] [PubMed] [Google Scholar]
- 10.Koulaouzidis A, Saeed AA. Distinct colonoscopy findings of microscopic colitis: not so microscopic after all? World J Gastroenterol. 2011;17:4157–4165. doi: 10.3748/wjg.v17.i37.4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hussain Z, Kelly S, Clarke A, et al. Colonic perforation in collagenous colitis: a systematic review of a rare complication and guidance on management. Surg Endosc. 2010;24:2930–2934. doi: 10.1007/s00464-010-1086-y. [DOI] [PubMed] [Google Scholar]
- 12.Allende DS, Taylor SL. Bronner MP Colonic perforation as a complication of collagenous colitis in a series of 12 patients. Am J Gastroenterol. 2008;103:2598–2604. doi: 10.1111/j.1572-0241.2008.01998.x. [DOI] [PubMed] [Google Scholar]
- 13.Sherman A, Ackert JJ, Rajapaksa R, West AB, Owelty T. Fractured colon: an endoscopically distinctive lesion associated with colonic perforation following colonoscopy in patients with collagenous colitis. J Clin Gastroenterol. 2004;38:341–345. doi: 10.1097/00004836-200404000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Freeman HJ, James D, Mahoney C. Spontaneous peritonitis from perforation of the colon in collagenous colitis. Can J Gastroenterol. 2001;15:265–267. doi: 10.1155/2001/194837. [DOI] [PubMed] [Google Scholar]
- 15.Bohr J, Larsson LG, Eriksson S, et al. Colonic perforation in collagenous colitis: an unusual complication. Eur J Gastroenterol Hepatol. 2005;17:121–124. doi: 10.1097/00042737-200501000-00022. [DOI] [PubMed] [Google Scholar]
- 16.Wickbom A, Lindqvist M, Bohr J, et al. Colonic mucosal tears in collagenous colitis. Scand J Gastroenterol. 2006;41:726–729. doi: 10.1080/00365520500453473. [DOI] [PubMed] [Google Scholar]