Abstract
Recent changes in the global climate system have resulted in excess mortality and morbidity, particularly among susceptible individuals with preexisting cardiopulmonary disease. These weather patterns are projected to continue and intensify as a result of rising CO2 levels, according to the most recent projections by climate scientists. In this Pulmonary Perspective, motivated by the American Thoracic Society Committees on Environmental Health Policy and International Health, we review the global human health consequences of projected changes in climate for which there is a high level of confidence and scientific evidence of health effects, with a focus on cardiopulmonary health. We discuss how many of the climate-related health effects will disproportionally affect people from economically disadvantaged parts of the world, who contribute relatively little to CO2 emissions. Last, we discuss the financial implications of climate change solutions from a public health perspective and argue for a harmonized approach to clean air and climate change policies.
Keywords: climate change, air pollution, cardiovascular health, pulmonary health
In the past several decades, an accumulation of scientific evidence has shown that climate change is not only an environmental and economic problem but also a human health problem of enormous proportions. Some of the most well-described human health consequences of climate change are the exacerbation of preexisting cardiopulmonary disease. The American Thoracic Society, whose mission is to improve health worldwide by advancing research, clinical care, and public health in respiratory disease and critical illness, is concerned about the implications of climate change for global public health, especially cardiopulmonary health.
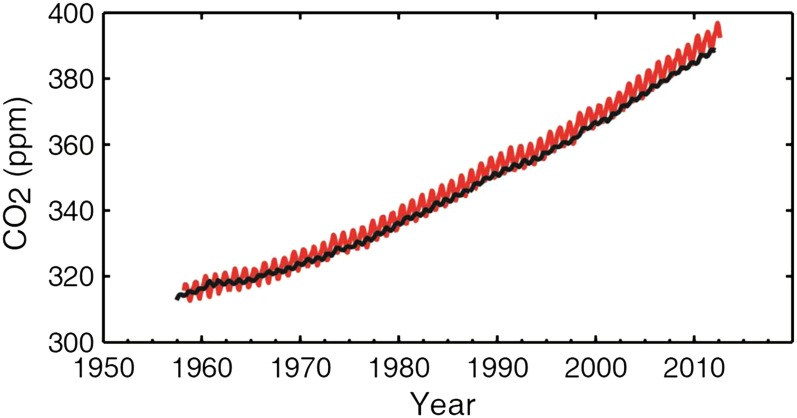
As early as 1896 it was found that carbon dioxide in the Earth’s atmosphere causes an imbalance between infrared light–transmitting and –absorbing properties and an increased back-radiation effect in the atmosphere that elevates the temperature at the surface and in the lower atmosphere (1). Human activities that burn fossil fuels release additional CO2 into the atmosphere. CO2 levels have risen dramatically since industrialization and continue to rise at alarming rates (Figure 1). The 2013 Intergovernmental Panel on Climate Change (IPCC) report concluded that CO2 concentrations have risen by 40% since preindustrial times, primarily due to fossil fuel emissions, and have reached levels “unprecedented in at least the last 800,000 years” (2). Other human activities release other greenhouse gases with similar effects, including methane, nitrous oxide, and sulfur dioxide, in addition to naturally occurring ozone and water vapor. Particulate black carbon is released from fossil fuel, biomass, and forest burning and directly absorbs solar radiation, which warms surface temperatures, and also deposits on snow and ice, which reduces the reflectivity of snow and further contributes to global warming (3).
Figure 1.
Atmospheric CO2 from Mauna Loa, Hawaii (red) and South Pole (black) since 1958. Reprinted by permission from Reference 2.
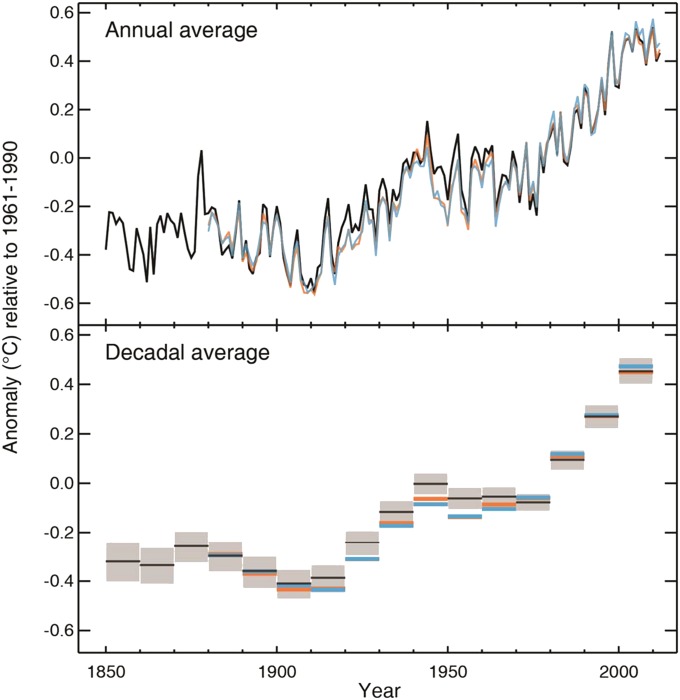
There is no dispute among climate scientists that the Earth’s climate system is warming. Figure 2 shows globally averaged surface and ocean temperatures since 1850 (relative to 1961–1990 levels) and illustrates the global warming trend since the 1950s. The 2013 IPCC report concluded that global warming is “unequivocal” and that with 95 to 100% certainty, the observed warming since the 1950s is primarily due to human activity (2). Global temperatures rose 0.6 to 0.7°C from 1951 to 2010, of which 0.5 to 1.3°C is attributed to greenhouse gases, −0.6 to 0.1°C from other human emissions including the cooling effect of aerosols, −0.1 to 0.1°C from natural forcings, and −0.1 to 0.1°C from internal variability (2).
Figure 2.
Observed globally averaged combined land and ocean surface temperature anomaly from 1850 to 2012 from three datasets used by the Intergovernmental Panel on Climate Change. Bottom panel: decadal mean values including the estimate of uncertainty for one dataset (black). Reprinted by permission from Reference 2.
Disruption of the global climate promotes extreme weather patterns that harm human health. These include heat waves, droughts, thunderstorms and heavier precipitation, and hurricanes and tropical cyclones. Secondary consequences of these changes include worsening air quality (due to high temperatures, forest fires, and dust storms), floods, and desertification.
Environmental Air Pollution and Climate Change
The primary outdoor air pollutants associated with climate change that are of particular relevance to cardiopulmonary health are black carbon, ozone, and particulate matter. Black carbon is released from fossil fuel combustion (including diesel, coal, and fuel), cooking with biomass fuels (which is widespread in the developing world), and the burning of forest and crop residue for agricultural purposes. Black carbon has been identified as an important climate-forcing emission along with CO2 (3), and has climate-forcing effects that last for decades (compared with centuries for CO2). In addition to its effects on climate, black carbon is an air pollutant (a constituent of fine particulate matter) with well-described respiratory and cardiovascular health effects at increased concentrations, including worsening of preexisting cardiovascular disease (4), worsening lung function (5), and increases in chronic obstructive pulmonary disease (COPD) hospitalization and mortality (6) and total and cardiovascular mortality (7). Household air pollution, consisting of black carbon smoke from indoor cooking particularly in the developing world, has been ranked as the third largest contributor to the global burden of disease, largely because of its associations with childhood respiratory infections, COPD in women, and cardiovascular disease in men (8).
Ground-level ozone is an air pollutant that is formed through atmospheric reactions of nitrogen oxides and volatile organic compounds (both emitted by motor vehicles and fossil fuel burning) in the presence of sunlight. Ozone formation increases on sunny, cloudless days and at higher temperatures (9). The frequency and intensity of ozone episodes during summer months are projected to increase as a result of rising temperatures (10, 11). Some recent heat waves have been associated with ozone levels that exceeded air quality standards (12).
Short-term elevations in ozone have been associated with increases in all-cause mortality in relatively polluted Latin American cities (13) and in less-polluted cities in Western Europe and North America (14). The deadly heat wave of 2003 in Europe was associated with high levels of ozone that are believed to have contributed to excess mortality in addition to the mortality caused by the heat itself (12, 15). Ozone has also been found to exacerbate preexisting respiratory diseases in both children and adults. Because ozone is a respiratory irritant that causes bronchial inflammation and hyperresponsiveness (16, 17), people with preexisting obstructive lung disease are particularly susceptible to adverse respiratory effects of ozone. A substantial body of evidence has shown that modest short-term increases in ground-level ozone increase risk of acute care visits and hospitalization for asthma (18–21) and COPD (22, 23). Ozone exposure has been associated with deterioration in asthma control in studies in the United States and Europe, resulting in increased medication use and missed school and work days (24–26). There is emerging evidence that obesity may increase susceptibility to respiratory effects of ozone exposure, which is concerning given the increasing prevalence of obesity in many parts of the world (27, 28).
Climate change is expected to contribute to dangerous elevations in particulate matter by fostering conditions favorable to forest fires and, in some arid parts of the world, promoting sand storms. Climate models indicate that with 1°C of warming, wildland fire risk may increase two- to sixfold over the 1950 to 2003 baseline in most of the continental United States west of the Mississippi (29). Although forest fires may ignite in only certain regions, their smoke plumes may extend over great distances. During the Russian heat wave of 2010, for instance, smoke from more than 500 wildfires stretched across more than 1,800 miles—roughly the distance from San Francisco to Chicago (30). Studies in the United States, Europe, and Australia have associated exposure to wildland fire smoke with asthma and COPD exacerbations and hospitalizations (31, 32), congestive heart failure events (33), and overall mortality (34).
Rising temperatures and increasing frequency of droughts are projected to increase desertification in areas with dry climates (35). Desertification and droughts promote dust storms (36), which are public health hazards, particularly for people with pulmonary disease. Desert dust particles contain quartz, which has been found to cause airway inflammation in animal studies (37, 38). Exposure to airborne dust particles transported from regional deserts (in some cases more than 4,000 km away) has been associated with increases in cardiovascular and respiratory mortality (39), cardiopulmonary emergency room visits (40), stroke (41), and admissions for asthma (42) and pneumonia (43) in studies from Spain, Taiwan, and California.
Particulate matter emissions tend to increase during heat waves in regions where electricity is supplied by coal-fired power plants, as a consequence of increased electrical energy use for cooling. There is evidence that high temperatures and particulate matter interact to cause greater mortality than would be expected for the same level of particulate matter at cooler temperatures, even in developed countries where particulate levels are relatively low (44–46). Particulate matter concentrations have declined substantially in the developed world in recent decades as a result of air quality regulations and tightening emissions standards. Even if average particulate matter concentrations continue to decrease in the future, the relative toxicity of particulate matter may rise during higher temperature periods because of this interaction.
Aeroallergen (Pollen) and Climate Change
Higher levels of CO2 and a warming climate are likely to worsen the global burden of allergic disease, which has been increasing in prevalence in the industrialized world for more than 50 years (47). Worldwide, between 10 and 30% of people suffer periodically from allergic rhinitis, and up to 40% are sensitized (by the presence of IgE antibodies) to environmental proteins (47). Warmer temperatures lengthen the pollen season in temperate climates because plants bloom earlier in the spring. Between 1995 and 2009, the pollen season lengthened 13 to 27 days above 44 degrees north in the United States (48). Higher levels of CO2 in the atmosphere have been found to increase pollen productivity and the allergic potency (relative allergen protein content) of pollen (49, 50). Extreme weather events involving high winds, heavy precipitation, and thunderstorms, which may increase in incidence over mid-latitudes due to climate change (2), may also contribute to large sudden bursts of allergen release (51, 52).
Higher pollen concentrations have been associated with increased prevalence of allergic sensitization (53) and increased healthcare use for allergic disease, measured in terms of over-the-counter allergy medication use (54), and emergency department (ED) and physician office visits for allergic disease (55, 56). Longer, more potent allergy seasons are likely to be especially detrimental to people with asthma. Experimental studies have found reduced lung function and increased pulmonary inflammation in subjects with asthma exposed to pollen (57, 58). Numerous studies in temperate climates have found increases in asthma and wheeze-related ED visits in association with high pollen concentrations (59–62). Some studies have linked asthma outbreaks to thunderstorms with peaks in allergen release (51, 52, 63). There may be adverse synergistic effects of increases in both air pollution and pollen for people with allergy and/or allergic asthma. Higher levels of particulate matter and ozone lower the bronchoconstrictive threshold to environmental allergens such as pollen and increase the subsequent production of IgE and cytokines, which may promote allergic respiratory disease (16, 64–66).
Increases in allergen exposure may also result in health effects beyond allergic disease. At least one study identified an increase in cardiovascular and respiratory mortality in association with higher pollen levels, a concerning finding that deserves further scientific investigation (67).
Extreme Weather
Climate change is likely to increase the frequency and intensity of a number of “extreme” weather events, including heat waves, hurricanes and tropical storms, and droughts. These changes have already been reported in recent decades (2). The 2013 IPCC report projects with 90 to 100% certainty that in the late 21st century there will an increase in heat waves over most land areas, an increase in the intensity and frequency of heavy precipitation over mid-latitudes and wet tropical areas, and an increase in the frequency and/or magnitude of extremely high sea levels (which may result in floods). The confidence levels for an increase in drought on a regional to global scale (66–100%) and increased tropical cyclone activity (>50–100%) in the late-21st century are lower (2).
Heat waves have well-documented adverse health effects. It is therefore highly concerning that climate models project up to a 50% increase in the frequency in the hottest (ie, the top 5th percentile based on historical records) days by midcentury (68, 69). Extreme heat increases all-cause mortality. The heat wave that hit western Europe in August 2003 resulted in an excess of 15,000 deaths in France alone (70). Studies have found that the elderly and those with chronic respiratory or cardiovascular disease are particularly susceptible to heat-related death (71, 72). Some of these deaths are due to a “harvesting effect,” or short-term mortality displacement, wherein people who would have died within 1 to 2 months die a few weeks earlier. However, only 30 to 40% of the estimated deaths from recent heat waves in the United States have been attributed to a harvesting effect, and the remainder constitute actual life-years lost (73). A study of the 2003 heat wave mortality in France found no evidence of harvesting (70). As average temperatures increase, populations will adjust to a higher temperature range, but they will continue to be vulnerable at temperature extremes (74).
Extreme heat events are associated with exacerbations of respiratory and cardiovascular disease. Hot, humid days trigger asthma symptoms and have been shown to increase airway resistance, most likely by stimulating airway C-fiber nerves (75, 76). Studies in the United States have associated acute increases in temperature and humidity with increased ED visits and hospitalizations for asthma in children (77) and adults (78). A case-crossover study in England and Wales examining hourly temperature and incidence of myocardial infarction found that higher ambient temperatures above a threshold of 20°C were associated with an increased risk of myocardial infarction 1 to 6 hours after exposure (80). There is also evidence that extreme heat may trigger exacerbations of congestive heart failure (79).
Warming temperatures cause an intensification of the water cycle that increases the frequency of both droughts and floods and promotes storm formation. Hot temperatures increase the rate of evaporation of moisture in the soil, resulting in droughts. Warmer air also holds more moisture, leading to heavier precipitation and floods. Additionally, high sea surface temperatures increase wind velocities, which promotes storms. Tropical storms will only form in the presence of warm ocean waters of at least 26.5°C to a minimum depth of 50 m (81). The melting of sea ice and a rising sea level also increase the vulnerability of coastal areas to storm surges. The IPCC projects a rise in the sea level of 0.3 to 0.8 m by 2100 compared with 1986 to 2005 levels and a rise in sea surface temperatures by up to 2°C (2).
Although extreme weather events such as droughts, floods, and storms are low-probability events, the human health costs of any one event can be catastrophic. In 2011 in the United States, there were 14 weather-related disasters costing more than $1 billion in damages, which was a national record (82). Hurricane Katrina killed more than 1,300 people and displaced approximately 30,000 persons (83). Though the United States ranks first among the world’s nations in terms of the frequency of coastal hurricanes, there are many regions of the world that are much less equipped to manage these natural disasters and suffer greater loss of life (81). In 1999, for example, 30,000 people died as a result of storms followed by floods and landslides in Venezuela (84). South Asia and Latin America have been identified as the most vulnerable areas to floods and tropical cyclones in terms of the human death toll and number of people affected (85). Studies of recent storms have identified drowning and severe injuries as the most common cause of death (85). The decreased sanitation and crowding after storms and floods promote the spread of infectious respiratory disease, and damage to the healthcare infrastructure, including disruption of electricity to clinics, hospitals, and intensive care units, impairs virtually every dimension of public health (81).
Desertification and droughts are a major public health concern for arid climates. Malnutrition is one of the top global health challenges, and climate change further threatens the ability of low-resource areas to maintain adequate food production. The WHO ranked malnutrition as the largest global health problem associated with climate change (86). The risk of drought-related health effects depends on the severity of the drought and resources to mitigate impacts of the drought (87). Sub-Saharan Africa and South Asia, whose food supplies are already limited, are anticipated to have the largest reductions in food supply as a result of climate change (88). A large proportion of global deaths from pneumonia in children under the age of 5 years are attributed to malnutrition (89), and pediatric pneumonia deaths in low resource arid climates may rise as a result of an increasing frequency of droughts.
Climate Change Solutions
The intent of this review is to describe how climate change is anticipated to affect global cardiopulmonary health and not to provide a comprehensive discussion of mitigation solutions. However, it is important to note that there is hope. The worst climate change scenarios may be avoidable with aggressive policy measures. The international community has agreed to a goal of limiting global warming to 2°C above preindustrial levels, based on evidence that further warming would be extremely difficult for contemporary societies to tolerate and concern that a “tipping point” could be reached after which there could be abrupt or even irreversible climate shifts (90, 91). Reaching this target will require dramatic (70%) reductions in cumulative greenhouse gas emissions between 2010 and 2100 compared with a baseline scenario, according to the climate model scenario selected by the IPCC that evaluated this target (2, 92). Is this achievable? A motivational success story is the Clean Air Act of 1970. The United States reduced most primary pollutants by more than two-thirds despite a growing population and economy. The public health benefits of the Clean Air Act have been substantial. A recent study attributed 15% of the increase in U.S. life expectancy in the 1980s and 1990s to improvements in particulate air pollution (93). The EPA estimates a return of $30 for every dollar spent on reducing air pollution through the Clean Air Act (94). Climate change policy can be such a success story, too.
Perhaps the largest problem with climate as a policy issue compared with air pollution is that many of the most devastating consequences of climate change, such as rising sea levels and desertification, occur incrementally over the course of decades, and policymakers tend to discount events that occur further into the future, preferring to react to what affects people “here and now” (95). Though the consequences of CO2 emissions are not always immediate, the air pollutants including particulate matter and black carbon that are emitted along with CO2 when fossil fuels and biomass are burned have immediate adverse cardiopulmonary health effects. A recent analysis compared the costs of reducing global greenhouse gas emissions according to one of the intermediate-level mitigation scenarios selected by the IPCC to the cardiopulmonary mortality benefits of reduced air pollution emissions that will accompany the reduction in CO2 emissions (96). The study found that the health benefits of cleaner air will exceed the cost of the proposed mitigation measures. These health benefits were projected to be gained immediately and locally by the regions that reduce their CO2 emissions, unlike the health benefits of the reduced CO2 itself, which are more delayed and global. Other cost–benefit analyses assessing the outdoor air pollution cobenefits of greenhouse gas emissions reductions have found similar results (97). There are also substantial and immediate cardiopulmonary health benefits of reducing indoor black carbon emissions through the introduction of cook stoves in the developing world (98). These cost–benefit analyses do not even consider the many other long-term global health benefits of mitigating climate change itself, including benefits of avoiding high temperatures, storms, floods, and droughts as discussed above. Given the enormous and immediate health benefits of the cleaner air that results from reduced fossil fuel and biomass combustion, a case can be made for harmonizing clean air and climate change policy, so that they each consider the other when one is being set (95). Public health benefits will be maximized by selecting climate mitigation measures that also minimize toxic air pollution emissions (e.g., focusing on coal and diesel emissions) and selecting air pollution measures that minimize CO2 emissions (e.g., reducing or eliminating coal emissions rather than applying scrubbers to remove particulate matter) (95).
In 2010, parties to the United Nations Framework Convention on Climate Change, which included the Obama Administration, agreed to a goal of limiting growth in CO2 emissions to a corresponding temperature increase limit of 2°C above preindustrial levels. It was suggested at the World Economic Forum that achieving this goal would require a global investment in clean energy of about $500 billion per year by 2020. In 2009, only $145 billion in public and private investment was spent on clean energy, a far cry from what is needed. The 2013 United Nations report on the 2°C target concluded that achieving the emissions goal is still possible with existing policy options—the major barrier is insufficient political will (99). Reducing CO2 emissions will require investment in multiple strategies, including the use of alternative energy sources, improved power plant efficiency, a reduction in coal-based power production in favor of natural gas and other alternatives, transportation strategies to reduce single-occupancy vehicle driving, advanced clean vehicles with improved fuel efficiency (such as plug-in–hybrid, battery electric, and fuel cell vehicles), modified construction to reduce the energy use of buildings, development of carbon sinks (such as forests and carbon capture and storage technology), and foreign aid to help lower-income countries achieve these goals. Efforts to reduce emissions of short-lived climate-forcing agents such as methane and black carbon will be particularly important toward reducing the rapid trajectory of global warming in the near term (7). The technology for most of these climate mitigation solutions already exists on an industrial scale (100). The global policy solution should also give low-resource countries a voice in initiatives to reduce greenhouse gas emissions, as they are disproportionately affected by the health consequences of climate change yet contribute relatively little to CO2 emissions.
Conclusions
Climate change is a growing public health problem of enormous proportions. The American Thoracic Society has identified climate change as an urgent issue facing our clinical profession, our research community, and our patients around the world, because people with cardiopulmonary disease are among the most susceptible to death and disease as a result of climate change. We need a paradigm shift to foster the magnitude of political will and investment required to solve this problem. Yet this is a problem that can be mitigated with existing tools. The value of the immediate cardiopulmonary health benefits of reducing emissions of CO2 and its associated air pollutants will outweigh the costs of mitigation. The long-term health benefits of avoiding mortality and morbidity due to temperature extremes, air pollution, pollen, floods, droughts, storms, desertification, and malnutrition justify climate change mitigation not only from an economic standpoint but also from a moral one.
Acknowledgments
Acknowledgment
The authors thank Gary Ewart of the American Thoracic Society and members of the Environmental Health Policy Committee and International Health Committee for their contributions to this manuscript.
Footnotes
Supported by the National Institute of Environmental Health Sciences grant 1F32ES023352-01 (M.B.R.), the National Heart, Lung, and Blood Institute grant T32HL007374 (M.B.R.), the California Air Resources Board (J.R.B.), the New York University–National Institute of Environmental Health Sciences Center of Excellence Grant ES00260 (G.D.T.), the California National Primate Research Center grant P51 OD0011107 (K.E.P.), and the National Institute for Occupational Safety and Health grant U54 OH007550 (K.E.P.).
Originally Published in Press as DOI: 10.1164/rccm.201310-1924PP on January 8, 2014
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.IPCC Working Group I. Summary for policymakers. In: Stocker TF, Qin D, Plattner G-K, Tignor M, Allen SK, Boschung J, Nauels A, Xia Y, Bex V, Midgley PM, editors. Climate change 2013: the physical science basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. New York: Cambridge University Press; 2013
- 2.Arrhenius S. On the influence of carbonic acid in the air upon the temperature of the ground. Philosophical Magazine and Journal of Science. 1896;41:237–276. [Google Scholar]
- 3.Bond TC, Doherty SJ, Fahey DW, Forster PM, Berntsen T, DeAngelo BJ, Flanner MG, Ghan S, Kärcher B, Koch D, et al. Bounding the role of black carbon in the climate system: a scientific assessment. J Geophys Res Atmos. 2013;118:5380–5552. [Google Scholar]
- 4.Nichols JL, Owens EO, Dutton SJ, Luben TJ. Systematic review of the effects of black carbon on cardiovascular disease among individuals with pre-existing disease. Int J Public Health. 2013;58:707–724. doi: 10.1007/s00038-013-0492-z. [DOI] [PubMed] [Google Scholar]
- 5.Franco Suglia S, Gryparis A, Schwartz J, Wright RJ. Association between traffic-related black carbon exposure and lung function among urban women. Environ Health Perspect. 2008;116:1333–1337. doi: 10.1289/ehp.11223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gan WQ, FitzGerald JM, Carlsten C, Sadatsafavi M, Brauer M. Associations of ambient air pollution with chronic obstructive pulmonary disease hospitalization and mortality. Am J Respir Crit Care Med. 2013;187:721–727. doi: 10.1164/rccm.201211-2004OC. [DOI] [PubMed] [Google Scholar]
- 7.Smith KR, Jerrett M, Anderson HR, Burnett RT, Stone V, Derwent R, Atkinson RW, Cohen A, Shonkoff SB, Krewski D, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: health implications of short-lived greenhouse pollutants. Lancet. 2009;374:2091–2103. doi: 10.1016/S0140-6736(09)61716-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bloomer BJ, Stehr JW, Piety CA, Salawitch RJ, Dickerson RR. Observed relationships of ozone air pollution with temperature and emissions. Geophys Res Lett. 2009;36:L09803. [Google Scholar]
- 10.Knowlton K, Rosenthal JE, Hogrefe C, Lynn B, Gaffin S, Goldberg R, Rosenzweig C, Civerolo K, Ku J-Y, Kinney PL. Assessing ozone-related health impacts under a changing climate. Environ Health Perspect. 2004;112:1557–1563. doi: 10.1289/ehp.7163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murazaki K, Hess P. How does climate change contribute to surface ozone change over the United States? J Geophys Res. 2006;111:D05301. [Google Scholar]
- 12.Doherty RM, Heal MR, Wilkinson P, Pattenden S, Vieno M, Armstrong B, Atkinson R, Chalabi Z, Kovats S, Milojevic A, Stevenson DS. Current and future climate- and air pollution-mediated impacts on human health. Environ Health. 2009;8:S8. doi: 10.1186/1476-069X-8-S1-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romieu I, Gouveia N, Cifuentes LA, de Leon AP, Junger W, Vera J, Strappa V, Hurtado-Díaz M, Miranda-Soberanis V, Rojas-Bracho L, et al. Multicity study of air pollution and mortality in Latin America (the ESCALA study) Res Rep Health Eff Inst. 2012:5–86. [PubMed] [Google Scholar]
- 14.Peng RD, Samoli E, Pham L, Dominici F, Touloumi G, Ramsay T, Burnett RT, Krewski D, Le Tertre A, Cohen A, et al. Acute effects of ambient ozone on mortality in Europe and North America: results from the APHENA study. Air Qual Atmos Health. 2013;6:445–453. doi: 10.1007/s11869-012-0180-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Filleul L, Cassadou S, Médina S, Fabres P, Lefranc A, Eilstein D, Le Tertre A, Pascal L, Chardon B, Blanchard M, et al. The relation between temperature, ozone, and mortality in nine French cities during the heat wave of 2003. Environ Health Perspect. 2006;114:1344–1347. doi: 10.1289/ehp.8328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alexis NE, Lay JC, Hazucha M, Harris B, Hernandez ML, Bromberg PA, Kehrl H, Diaz-Sanchez D, Kim C, Devlin RB, et al. Low-level ozone exposure induces airways inflammation and modifies cell surface phenotypes in healthy humans. Inhal Toxicol. 2010;22:593–600. doi: 10.3109/08958371003596587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song H, Tan W, Zhang X. Ozone induces inflammation in bronchial epithelial cells. J Asthma. 2011;48:79–83. doi: 10.3109/02770903.2010.529224. [DOI] [PubMed] [Google Scholar]
- 18.Moore K, Neugebauer R, Lurmann F, Hall J, Brajer V, Alcorn S, Tager I. Ambient ozone concentrations cause increased hospitalizations for asthma in children: an 18-year study in Southern California. Environ Health Perspect. 2008;116:1063–1070. doi: 10.1289/ehp.10497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glad JA, Brink LL, Talbott EO, Lee PC, Xu X, Saul M, Rager J. The relationship of ambient ozone and PM(2.5) levels and asthma emergency department visits: possible influence of gender and ethnicity. Arch Environ Occup Health. 2012;67:103–108. doi: 10.1080/19338244.2011.598888. [DOI] [PubMed] [Google Scholar]
- 20.Babin S, Burkom H, Holtry R, Tabernero N, Davies-Cole J, Stokes L, Dehaan K, Lee D. Medicaid patient asthma-related acute care visits and their associations with ozone and particulates in Washington, DC, from 1994-2005. Int J Environ Health Res. 2008;18:209–221. doi: 10.1080/09603120701694091. [DOI] [PubMed] [Google Scholar]
- 21.Babin SM, Burkom HS, Holtry RS, Tabernero NR, Stokes LD, Davies-Cole JO, DeHaan K, Lee DH. Pediatric patient asthma-related emergency department visits and admissions in Washington, DC, from 2001–2004, and associations with air quality, socio-economic status and age group. Environ Health. 2007;6:9. doi: 10.1186/1476-069X-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ko FWS, Tam W, Wong TW, Chan DPS, Tung AH, Lai CKW, Hui DSC. Temporal relationship between air pollutants and hospital admissions for chronic obstructive pulmonary disease in Hong Kong. Thorax. 2007;62:780–785. doi: 10.1136/thx.2006.076166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brunekreef B, Holgate ST. Air pollution and health. Lancet. 2002;360:1233–1242. doi: 10.1016/S0140-6736(02)11274-8. [DOI] [PubMed] [Google Scholar]
- 24.Jacquemin B, Kauffmann F, Pin I, Le Moual N, Bousquet J, Gormand F, Just J, Nadif R, Pison C, Vervloet D, et al. Epidemiological study on the Genetics and Environment of Asthma (EGEA) Air pollution and asthma control in the Epidemiological study on the Genetics and Environment of Asthma. J Epidemiol Community Health. 2012;66:796–802. doi: 10.1136/jech.2010.130229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meng Y-Y, Wilhelm M, Rull RP, English P, Ritz B. Traffic and outdoor air pollution levels near residences and poorly controlled asthma in adults. Ann Allergy Asthma Immunol. 2007;98:455–463. doi: 10.1016/S1081-1206(10)60760-0. [DOI] [PubMed] [Google Scholar]
- 26.Thurston GD, Lippmann M, Scott MB, Fine JM. Summertime haze air pollution and children with asthma. Am J Respir Crit Care Med. 1997;155:654–660. doi: 10.1164/ajrccm.155.2.9032209. [DOI] [PubMed] [Google Scholar]
- 27.Alexeeff SE, Litonjua AA, Suh H, Sparrow D, Vokonas PS, Schwartz J. Ozone exposure and lung function: effect modified by obesity and airways hyperresponsiveness in the VA normative aging study. Chest. 2007;132:1890–1897. doi: 10.1378/chest.07-1126. [DOI] [PubMed] [Google Scholar]
- 28.Shore SA, Rivera-Sanchez YM, Schwartzman IN, Johnston RA. Responses to ozone are increased in obese mice. J Appl Physiol (1985) 2003;95:938–945. doi: 10.1152/japplphysiol.00336.2003. [DOI] [PubMed] [Google Scholar]
- 29.Solomon S, Battisti DS, Doney SC, Hayhoe K, Held I, Al E.Climate stabilization targets: emissions, concentrations, and impacts over decades to millennia. Washington, D.C.: National Academy Press; 2011 [Google Scholar]
- 30.NASAFires and smoke in Russia. Earth Observatory 2010 [Google Scholar]
- 31.Henderson SB, Johnston FH. Measures of forest fire smoke exposure and their associations with respiratory health outcomes. Curr Opin Allergy Clin Immunol. 2012;12:221–227. doi: 10.1097/ACI.0b013e328353351f. [DOI] [PubMed] [Google Scholar]
- 32.Rappold AG, Stone SL, Cascio WE, Neas LM, Kilaru VJ, Carraway MS, Szykman JJ, Ising A, Cleve WE, Meredith JT, et al. Peat bog wildfire smoke exposure in rural North Carolina is associated with cardiopulmonary emergency department visits assessed through syndromic surveillance. Environ Health Perspect. 2011;119:1415–1420. doi: 10.1289/ehp.1003206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rappold AG, Cascio WE, Kilaru VJ, Stone SL, Neas LM, Devlin RB, Diaz-Sanchez D. Cardio-respiratory outcomes associated with exposure to wildfire smoke are modified by measures of community health. Environ Health. 2012;11:71. doi: 10.1186/1476-069X-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hänninen OO, Salonen RO, Koistinen K, Lanki T, Barregard L, Jantunen M. Population exposure to fine particles and estimated excess mortality in Finland from an East European wildfire episode. J Expo Sci Environ Epidemiol. 2009;19:414–422. doi: 10.1038/jes.2008.31. [DOI] [PubMed] [Google Scholar]
- 35.UNESCOWorld Water Development Report, 4th Edition, World Water Assessment Programme. 2012 [accessed 2014 Feb 13]. Available from: http://www.unesco.org/new/en/natural-sciences/environment/water/wwap/wwdr/wwdr4–2012/
- 36.Goudie AS, Middleton NJ. The changing frequency of dust storms through time. Clim Change. 1992;20:197–225. [Google Scholar]
- 37.Ichinose T, Yoshida S, Sadakane K, Takano H, Yanagisawa R, Inoue K, Nishikawa M, Mori I, Kawazato H, Yasuda A, et al. Effects of Asian sand dust, Arizona sand dust, amorphous silica and aluminum oxide on allergic inflammation in the murine lung. Inhal Toxicol. 2008;20:685–694. doi: 10.1080/08958370801935133. [DOI] [PubMed] [Google Scholar]
- 38.Murphy SA, BéruBé KA, Pooley FD, Richards RJ. The response of lung epithelium to well characterised fine particles. Life Sci. 1998;62:1789–1799. doi: 10.1016/s0024-3205(98)00141-6. [DOI] [PubMed] [Google Scholar]
- 39.Perez L, Tobías A, Querol X, Pey J, Alastuey A, Díaz J, Sunyer J. Saharan dust, particulate matter and cause-specific mortality: a case-crossover study in Barcelona (Spain) Environ Int. 2012;48:150–155. doi: 10.1016/j.envint.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 40.Chan C-C, Chuang K-J, Chen W-J, Chang W-T, Lee C-T, Peng C-M. Increasing cardiopulmonary emergency visits by long-range transported Asian dust storms in Taiwan. Environ Res. 2008;106:393–400. doi: 10.1016/j.envres.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 41.Yang C-Y, Chen Y-S, Chiu H-F, Goggins WB. Effects of Asian dust storm events on daily stroke admissions in Taipei, Taiwan. Environ Res. 2005;99:79–84. doi: 10.1016/j.envres.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 42.Kanatani KT, Ito I, Al-Delaimy WK, Adachi Y, Mathews WC, Ramsdell JW Toyama Asian Desert Dust and Asthma Study Team. Desert dust exposure is associated with increased risk of asthma hospitalization in children. Am J Respir Crit Care Med. 2010;182:1475–1481. doi: 10.1164/rccm.201002-0296OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cheng M-F, Ho S-C, Chiu H-F, Wu T-N, Chen P-S, Yang C-Y. Consequences of exposure to Asian dust storm events on daily pneumonia hospital admissions in Taipei, Taiwan. J Toxicol Environ Health A. 2008;71:1295–1299. doi: 10.1080/15287390802114808. [DOI] [PubMed] [Google Scholar]
- 44.Qian Z, He Q, Lin H-M, Kong L, Bentley CM, Liu W, Zhou D. High temperatures enhanced acute mortality effects of ambient particle pollution in the “oven” city of Wuhan, China. Environ Health Perspect. 2008;116:1172–1178. doi: 10.1289/ehp.10847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ren C, Williams GM, Tong S. Does particulate matter modify the association between temperature and cardiorespiratory diseases? Environ Health Perspect. 2006;114:1690–1696. doi: 10.1289/ehp.9266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Katsouyanni K, Pantazopoulou A, Touloumi G, Tselepidaki I, Moustris K, Asimakopoulos D, Poulopoulou G, Trichopoulos D. Evidence for interaction between air pollution and high temperature in the causation of excess mortality. Arch Environ Health. 1993;48:235–242. doi: 10.1080/00039896.1993.9940365. [DOI] [PubMed] [Google Scholar]
- 47.Pawankar R, Canonica GW, Holgate ST, Lockey RF.WAO White Book on Allergy 2011–2012. Milwaukee, WI: World Allergy Organization; 2011 [accessed 2014 Feb 13]. Available from: http://www.worldallergy.org/publications/wao_white_book.pdf
- 48.Ziska L, Knowlton K, Rogers C, Dalan D, Tierney N, Elder MA, Filley W, Shropshire J, Ford LB, Hedberg C, et al. Recent warming by latitude associated with increased length of ragweed pollen season in central North America. Proc Natl Acad Sci USA. 2011;108:4248–4251. doi: 10.1073/pnas.1014107108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wolf J, O’Neill NR, Rogers CA, Muilenberg ML, Ziska LH. Elevated atmospheric carbon dioxide concentrations amplify Alternaria alternata sporulation and total antigen production. Environ Health Perspect. 2010;118:1223–1228. doi: 10.1289/ehp.0901867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wayne P, Foster S, Connolly J, Bazzaz F, Epstein P. Production of allergenic pollen by ragweed (Ambrosia artemisiifolia L.) is increased in CO2-enriched atmospheres. Ann Allergy Asthma Immunol. 2002;88:279–282. doi: 10.1016/S1081-1206(10)62009-1. [DOI] [PubMed] [Google Scholar]
- 51.Wardman AED, Stefani D, MacDonald JC. Thunderstorm-associated asthma or shortness of breath epidemic: a Canadian case report. Can Respir J. 2002;9:267–270. doi: 10.1155/2002/728257. [DOI] [PubMed] [Google Scholar]
- 52.Packe GE, Ayres JG. Asthma outbreak during a thunderstorm. Lancet. 1985;2:199–204. doi: 10.1016/s0140-6736(85)91510-7. [DOI] [PubMed] [Google Scholar]
- 53.Porsbjerg C, Linstow ML, Nepper-christensen SC, Rasmussen A, Korsgaard J, Nolte H, Backer V Greenlandic Population Study Group. Allergen sensitization and allergen exposure in Greenlander Inuit residing in Denmark and Greenland. Respir Med. 2002;96:736–744. doi: 10.1053/rmed.2002.1341. [DOI] [PubMed] [Google Scholar]
- 54.Sheffield PE, Weinberger KR, Ito K, Matte TD, Mathes RW, Robinson GS, Kinney PL. The association of tree pollen concentration peaks and allergy medication sales in New York City: 2003–2008. ISRN allergy. 2011;2011:537194. doi: 10.5402/2011/537194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cakmak S, Dales RE, Burnett RT, Judek S, Coates F, Brook JR. Effect of airborne allergens on emergency visits by children for conjunctivitis and rhinitis. Lancet. 2002;359:947–948. doi: 10.1016/S0140-6736(02)08045-5. [DOI] [PubMed] [Google Scholar]
- 56.Villeneuve PJ, Doiron M-S, Stieb D, Dales R, Burnett RT, Dugandzic R. Is outdoor air pollution associated with physician visits for allergic rhinitis among the elderly in Toronto, Canada? Allergy. 2006;61:750–758. doi: 10.1111/j.1398-9995.2006.01070.x. [DOI] [PubMed] [Google Scholar]
- 57.Higgins BG, Francis HC, Yates C, Warburton CJ, Fletcher AM, Pickering CA, Woodcock AA. Environmental exposure to air pollution and allergens and peak flow changes. Eur Respir J. 2000;16:61–66. doi: 10.1034/j.1399-3003.2000.16a11.x. [DOI] [PubMed] [Google Scholar]
- 58.Boulet L-P, Turcotte H, Boutet M, Montminy L, Laviolette M. Influence of natural antigenic exposure on expiratory flows, methacholine responsiveness, and airway inflammation in mild allergic asthma. J Allergy Clin Immunol. 1993;91:883–893. doi: 10.1016/0091-6749(93)90346-h. [DOI] [PubMed] [Google Scholar]
- 59.Darrow LA, Hess J, Rogers CA, Tolbert PE, Klein M, Sarnat SE. Ambient pollen concentrations and emergency department visits for asthma and wheeze. J Allergy Clin Immunol. 2012;130:630–638. doi: 10.1016/j.jaci.2012.06.020. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Héguy L, Garneau M, Goldberg MS, Raphoz M, Guay F, Valois M-F. Associations between grass and weed pollen and emergency department visits for asthma among children in Montreal. Environ Res. 2008;106:203–211. doi: 10.1016/j.envres.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 61.Zhong W, Levin L, Reponen T, Hershey GK, Adhikari A, Shukla R, LeMasters G. Analysis of short-term influences of ambient aeroallergens on pediatric asthma hospital visits. Sci Total Environ. 2006;370:330–336. doi: 10.1016/j.scitotenv.2006.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Erbas B, Akram M, Dharmage SC, Tham R, Dennekamp M, Newbigin E, Taylor P, Tang MLK, Abramson MJ. The role of seasonal grass pollen on childhood asthma emergency department presentations. Clin Exp Allergy. 2012;42:799–805. doi: 10.1111/j.1365-2222.2012.03995.x. [DOI] [PubMed] [Google Scholar]
- 63.Newson R, Strachan D, Archibald E, Emberlin J, Hardaker P, Collier C. Effect of thunderstorms and airborne grass pollen on the incidence of acute asthma in England, 1990-94. Thorax. 1997;52:680–685. doi: 10.1136/thx.52.8.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Leikauf GD. Hazardous air pollutants and asthma. Environ Health Perspect. 2002;110:505–526. doi: 10.1289/ehp.02110s4505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Diaz-Sanchez D, Garcia MP, Wang M, Jyrala M, Saxon A. Nasal challenge with diesel exhaust particles can induce sensitization to a neoallergen in the human mucosa. J Allergy Clin Immunol. 1999;104:1183–1188. doi: 10.1016/s0091-6749(99)70011-4. [DOI] [PubMed] [Google Scholar]
- 66.Jörres R, Nowak D, Magnussen H. The effect of ozone exposure on allergen responsiveness in subjects with asthma or rhinitis. Am J Respir Crit Care Med. 1996;153:56–64. doi: 10.1164/ajrccm.153.1.8542163. [DOI] [PubMed] [Google Scholar]
- 67.Brunekreef B, Hoek G, Fischer P, Spieksma FT. Relation between airborne pollen concentrations and daily cardiovascular and respiratory-disease mortality. Lancet. 2000;355:1517–1518. doi: 10.1016/S0140-6736(00)02168-1. [DOI] [PubMed] [Google Scholar]
- 68.Duffy PB, Tebaldi C. Increasing prevalence of extreme summer temperatures in the US. Clim Change. 2012;111:487–495. [Google Scholar]
- 69.Meehl GA, Tebaldi C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science. 2004;305:994–997. doi: 10.1126/science.1098704. [DOI] [PubMed] [Google Scholar]
- 70.Fouillet A, Rey G, Laurent F, Pavillon G, Bellec S, Guihenneuc-Jouyaux C, Clavel J, Jougla E, Hémon D. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health. 2006;80:16–24. doi: 10.1007/s00420-006-0089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stafoggia M, Forastiere F, Agostini D, Caranci N, de’Donato F, Demaria M, Michelozzi P, Miglio R, Rognoni M, Russo A, et al. Factors affecting in-hospital heat-related mortality: a multi-city case-crossover analysis. J Epidemiol Community Health. 2008;62:209–215. doi: 10.1136/jech.2007.060715. [DOI] [PubMed] [Google Scholar]
- 72.Medina-Ramón M, Zanobetti A, Cavanagh DP, Schwartz J. Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect. 2006;114:1331–1336. doi: 10.1289/ehp.9074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet. 2006;367:859–869. doi: 10.1016/S0140-6736(06)68079-3. [DOI] [PubMed] [Google Scholar]
- 74.Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155:80–87. doi: 10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
- 75.Hayes D, Jr, Collins PB, Khosravi M, Lin R-L, Lee L-Y. Bronchoconstriction triggered by breathing hot humid air in patients with asthma: role of cholinergic reflex. Am J Respir Crit Care Med. 2012;185:1190–1196. doi: 10.1164/rccm.201201-0088OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Aitken ML, Marini JJ. Effect of heat delivery and extraction on airway conductance in normal and in asthmatic subjects. Am Rev Respir Dis. 1985;131:357–361. doi: 10.1164/arrd.1985.131.3.357. [DOI] [PubMed] [Google Scholar]
- 77.Mireku N, Wang Y, Ager J, Reddy RC, Baptist AP. Changes in weather and the effects on pediatric asthma exacerbations. Ann Allergy Asthma Immunol. 2009;103:220–224. doi: 10.1016/S1081-1206(10)60185-8. [DOI] [PubMed] [Google Scholar]
- 78.Lin S, Luo M, Walker RJ, Liu X, Hwang SA, Chinery R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20:738–746. doi: 10.1097/EDE.0b013e3181ad5522. [DOI] [PubMed] [Google Scholar]
- 79.Lim Y-H, Hong Y-C, Kim H. Effects of diurnal temperature range on cardiovascular and respiratory hospital admissions in Korea. Sci Total Environ. 2012;417-418:55–60. doi: 10.1016/j.scitotenv.2011.12.048. [DOI] [PubMed] [Google Scholar]
- 80.Bhaskaran K, Armstrong B, Hajat S, Haines A, Wilkinson P, Smeeth L. Heat and risk of myocardial infarction: hourly level case-crossover analysis of MINAP database. BMJ. 2012;345:e8050. doi: 10.1136/bmj.e8050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shultz JM, Russell J, Espinel Z. Epidemiology of tropical cyclones: the dynamics of disaster, disease, and development. Epidemiol Rev. 2005;27:21–35. doi: 10.1093/epirev/mxi011. [DOI] [PubMed] [Google Scholar]
- 82.National Oceanic and Atmospheric Administration (NOAA), National Climatic Data Center. Billion-dollar weather/climate disasters. 2011 [accessed 2014 Feb 13]. Available from: http://www.ncdc.noaa.gov/billions/
- 83.Jenkins JL, McCarthy M, Kelen G, Sauer LM, Kirsch T. Changes needed in the care for sheltered persons: a multistate analysis from Hurricane Katrina. Am J Disaster Med. 2009;4:101–106. [PubMed] [Google Scholar]
- 84.IFRC (International Federation of Red Cross and Red Crescent Societies)World Disaster Report 2002. Geneva, Switzerland: 2002 [Google Scholar]
- 85.Parry ML, Canziani OF, Palutikof JP, van der Linden PJ, Hanson CE.editors. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK: Cambridge University Press; 2007
- 86.Campbell-Lendrum DH, Corvalán CF, Prüss–Ustün A.How much disease could climate change cause? In: McMichael AJ, Campbell-Lendrum DH, Corvalan CF, Ebi KL, Githeko AK, Scheraga JD, Woodward A, editors. Climate change and human health - risks and response. Geneva, Switzerland: World Health Organization; 2003. pp. 133–158
- 87.Stanke C, Kerac M, Prudhomme C, Medlock J, Murray V. Health effects of drought: a systematic review of the evidence. PLoS Curr. 2013;5:5. doi: 10.1371/currents.dis.7a2cee9e980f91ad7697b570bcc4b004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cline W.Global warming and agriculture impact estimates by country. Washington, DC: Center for Global Development and Peterson Institute for International Economics; 2007 [Google Scholar]
- 89.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lenton TM, Held H, Kriegler E, Hall JW, Lucht W, Rahmstorf S, Schellnhuber HJ. Tipping elements in the Earth’s climate system. Proc Natl Acad Sci USA. 2008;105:1786–1793. doi: 10.1073/pnas.0705414105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Richardson K, Steffen W, Schellnhuber HJ, Alcamo J, Barker T, Kammen DM, Leemans R, Liverman D, Munasinghe M, Osman-Elasha B, et al. Synthesis report from the Congress: climate change – global risks, challenges, and decisions. Copenhagen: University of Copenhagen; 2009 [Google Scholar]
- 92.van Vuuren DP, Stehfest E, den Elzen MGJ, Kram T, van Vliet J, Deetman S, Isaac M, Klein Goldewijk K, Hof A, Mendoza Beltran A, et al. RCP2.6: exploring the possibility to keep global mean temperature increase below 2°C. Clim Change. 2011;109:95–116. [Google Scholar]
- 93.Pope CA, III, Ezzati M, Dockery DW. Fine-particulate air pollution and life expectancy in the United States. N Engl J Med. 2009;360:376–386. doi: 10.1056/NEJMsa0805646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.EPAThe benefits and costs of the Clean Air Act from 1990 to 2020: Summary report. Research Triangle Park, NC: Environmental Protection Agency. 2011 [Google Scholar]
- 95.Thurston GD. Mitigation policy: health co-benefits. Nature Climate Change. 2013;3:863–864. [Google Scholar]
- 96.West JJ, Smith SJ, Silva RA, Naik V, Zhang Y, Adelman Z, Fry MM, Anenberg S, Horowitz LW, Lamarque J-F. Co-benefits of mitigating global greenhouse gas emissions for future air quality and human health. Nature Climate Change. 2013;3:885–889. doi: 10.1038/NCLIMATE2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Markandya A, Armstrong BG, Hales S, Chiabai A, Criqui P, Mima S, Tonne C, Wilkinson P. Public health benefits of strategies to reduce greenhouse-gas emissions: low-carbon electricity generation. Lancet. 2009;374:2006–2015. doi: 10.1016/S0140-6736(09)61715-3. [DOI] [PubMed] [Google Scholar]
- 98.Wilkinson P, Smith KR, Davies M, Adair H, Armstrong BG, Barrett M, Bruce N, Haines A, Hamilton I, Oreszczyn T, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: household energy. Lancet. 2009;374:1917–1929. doi: 10.1016/S0140-6736(09)61713-X. [DOI] [PubMed] [Google Scholar]
- 99.UNEPThe Emissions Gap Report 2013. Nairobi: United Nations Environment Programme (UNEP); 2013 [Google Scholar]
- 100.Pacala S, Socolow R. Stabilization wedges: solving the climate problem for the next 50 years with current technologies. Science. 2004;305:968–972. doi: 10.1126/science.1100103. [DOI] [PubMed] [Google Scholar]