Abstract
The oblique retinacular ligament originates from the flexor tendon sheath, courses past the proximal interphalangeal joint, and merges with the lateral extensor tendon. There has been disagreement regarding the contribution of the oblique retinacular ligament to coordinated movements between the proximal and distal interphalangeal joints. Landsmeer postulated that it acts as a dynamic tenodesis that tightens with proximal interphalangeal joint extension causing obligatory distal interphalangeal joint extension. Studies have shown, however, that the oblique retinacular ligament is variably present and often attenuated, thus diminishing its presumed role in finger movement. Despite this, the concept of a checkrein linking interphalangeal joint motion heralded the development of effective and reproducible surgical interventions for swan-neck and mallet deformities. This paper examines the controversy regarding the existence of the oblique retinacular ligament, its plausible functionality, and clinical implications in the practice of hand surgery.
Introduction
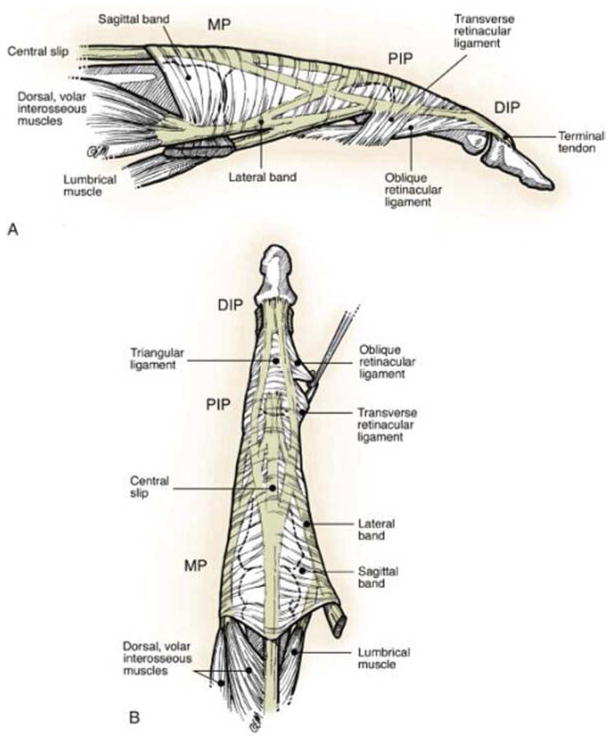
Finger extension occurs through a complex balance of intrinsic and extrinsic muscles with support from retinacular structures (1). A retinaculum is a fibrous band that acts to stabilize a tendon. Located in the finger, the oblique retinacular ligament (ORL) is believed to aid in stabilization of the proximal interphalangeal (PIP) joint. The ORL originates at the base of the proximal phalanx and courses obliquely past the PIP joint to terminate on the dorsum of the distal phalanx (Figure 1). Exploring the precise anatomy and function of this structure has interested anatomists and hand surgeons for decades.
Figure 1.
Drawing of the digital extensor mechanism with traction on the ORL. (Reprinted with permission from Strauch RJ. Extensor Tendon Injury. In: Green DP, Hotchkiss RN, Pederson WC ed. Green’s Operative Hand Surgery. 5th ed. New York, NY: Churchill Livingstone; 2005:163.)
Discovery of the ORL is credited to Josias Weitbrecht, a preeminent 18th century professor of anatomy, physiology, and medicine at the University of St. Petersburg in Russia. He reported its presence in his 1742 textbook entitled Syndesmology (2, 3, 4, 5). Weitbrecht labeled this structure “retinaculum tendini longi” owing to its tendinous, rather than ligamentous, role in hand function (6). Landsmeer in 1949 independently described the ORL in detail (7). His publications laid the framework for controversy regarding the presence, anatomy, function, and clinical implications of this fibrous structure.
Historically, there has been disagreement regarding the contribution of the ORL to coordinated movements between the PIP and distal interphalangeal (DIP) joints. Landsmeer believed the ORL acts as a dynamic tenodesis extending the DIP joint as the PIP is extended and relaxing with PIP flexion to enable full DIP flexion (8). Conversely, Harris and Kaplan felt the ORL contributes only to lateral stability of the PIP joint (3). Regardless of the true functionality of the ORL, an important byproduct has emerged from this debate. Using Landsmeer’s dynamic interphalangeal tenodesis theory, surgical procedures have been developed to address hand maladies such as swan-neck and mallet deformities. This paper examines the controversy surrounding the existence, anatomy, plausible functionality, and clinical implications of the ORL in the practice of hand surgery.
Anatomical Studies
The ORL contains fibers originating from medial and lateral volar-lateral ridge of the proximal phalanx and the flexor tendon sheath. These fibers coalesce immediately proximal to the PIP joint before coursing obliquely across the joint capsule (9, 10, 11, 12). Progressing distally and dorsally, the ORL merges with the lateral extensor tendon (at the proximal third of the middle phalanx) and inserts into the base of the distal phalanx (Figure 1) (11). By coursing palmar to the axis of rotation of the PIP joint, the ORL theoretically inhibits hyperextension of the middle phalanx through a checkrein action. Attaching dorsally on the distal phalanx enables the ORL to contribute to extension at the DIP joint when the ORL is placed under tension.
Dissections performed by surgeons and anatomists have identified the ORL as a distinct structure, though studies fail to show the ORL to be universally present on all fingers all the time. Ueba et al. found an ORL in 38 out of 40 uninjured cadaveric finger dissections (10 hands) (13). El-Gammal et al. found the ORL 95% (19/20) and 90% (18/20) of the time on the lateral and medial aspect of the index finger, respectively (this study centered on formulating a mathematical model for index finger motion, therefore characteristics of the ORL from other digits were not reported) (7). These findings contrast with work by Shrewsbury, Schweitzer, and Milford who were unable to easily or consistently identify the ORL in fresh-frozen and formalized specimens (11, 14, 15). Shrewsbury et al. identified “the presence of the ORL in the range of 40–50%” of dissected fingers. In 93% of their specimens there was an ORL on the medial side of the ring finger (11). Although identification of this ligament may depend on dissection expertise, the variable presence of the ORL has raised questions about its clinical function.
Ueba et al. made subjective thickness assessments and found the ORL on the medial side of the ring finger to be the most “robust.” These findings align with conclusions drawn by Shrewsbury et al. and Schweitzer et al (11, 14). The average thickness for all ORLs identified by Ueba et al. was ranked as a 3 out of 5, and designated as “thin” (where 0 is unidentifiable and 5 is thick) (13). Shrewsbury et al. offered more quantitative observations and found that the number of intratendinous fibers of the ORL ranged from 5 to 20 fibers, imparting a thickness of approximately 2mm and an average length of 15mm (11).
Biomechanical and Functional Studies of the ORL
The anatomical designs of the hand and finger are such that movements of the phalangeal joints are interdependent (16). These coordinated movements are appreciated when the radiocarpal joint is in passive flexion. This relaxes the long digital flexors and tightens the extrinsic extensors, thus placing the fingers in extension(1). Tension along the extensor tendon extends the PIP joint through the central band and the DIP joint through the lateral bands (1, 16, 17). The contribution from the ORL to extension of the DIP joint remains controversial.
Landsmeer postulated that extension of the distal phalanx occurs via the action of the common extensor through the lateral bands and by a dynamic interphalangeal tenodesis effect exerted by the ORL. He noted that “extension at the PIP joint implies corresponding extension of the DIP joint” and that when the ORL is placed “under tension it exerts a force on the terminal tendon, resulting in extension of the third phalanx” (16). Stated simply, with PIP joint extension, the ORL (which is volar to the PIP joint axis) is placed under tension causing DIP joint extension. With PIP joint flexion, the ORL becomes slack, allowing flexion of the DIP joint. In this respect, the ORL is dynamic because its tenodesis function (preventing flexion of the DIP joint with an extended PIP joint) is exerted only during extension of the PIP joint.
Based mostly on Landsmeer’s work, hand surgical dogma suggests that the ORL has a substantive role linking PIP and DIP joint movement. In 1969, Stack suggested that the ORL extends the DIP joint from full flexion of 90 degrees to 45 degrees of extension, whereas extension to 0 degrees is predominantly achieved by the lateral bands (18). He noted that, when the PIP joint is held forcibly in extension, there is sufficient laxity in the ORL to allow up to 45 degrees of flexion at the DIP joint (18). Bendz, in 1985, concurred that the ORL appears to be taut in this position (45 degrees of DIP joint flexion). As a result, further flexion at the DIP joint is prevented (19).
Harris and Schweitzer refuted this suggestion (3, 14). They felt the terminal tendon, not the ORL, is the structure primarily responsible for DIP joint extension through intrinsic muscles. Most convincingly, elegant work performed by Harris and Rutledge on cadavers showed that complete sectioning of the lateral bands, while sparing the ORL, led to a DIP joint extension lag of 70 degrees with the PIP joint in full extension (3). Conversely, transection of the ORL, while sparing the lateral bands, caused no perceptible extensor lag. Shrewsbury and Johnson made similar claims that excision of the ORL did not alter the coordinated motions of the interphalangeal joints (11).
Ueba et al. (13) sought objective data through biomechanical studies of flexion forces placed upon the DIP joint. They studied 40 fresh-frozen finger specimens with a focus on the ORL and its contribution to DIP and PIP joint mechanics. Their results showed the peak force required to flex the DIP joint was greater when the ORL was intact versus excised. The ORL contributed a maximum of 25% and 31% of the passive resistance to DIP joint flexion with the PIP joint at 0 and 30 degrees of flexion, respectively. They also concluded that an excised central slip resulted in a markedly decreased force required to flex the DIP joint. Practically speaking, the ORL presents a mild restraint upon flexion at the DIP joint with PIP joint extension. Based on Landsmeer’s original hypothesis, however, the ORL should exert its greatest resistance to flexion of the distal phalanx with the PIP joint at 0 degrees flexion (at which point the ORL would presumably be under greatest tension). Although Ueba et al. provide additional insight, a clear consensus understanding of the ORLs primary functionality is absent. Historically, those refuting Landsmeer’s original work have offered a simple alternative – the ORL functions to statically centralize the extensor mechanism and to reinforce lateral stability at the PIP joint (20).
Clinical Relevance
Because interphalangeal joint motion is interdependent, deformities at 1 joint will often have compensatory consequences at another. For example, a hyperextension deformity of the PIP joint causes laxity of the terminal extensor tendons leading to a DIP joint flexion deformity. Surgical correction may, as a result, require stabilization of the volar structures at the PIP joint and restoration of active DIP joint extension (20). Despite conflicting opinions regarding the ORL, the functional description offered by Landsmeer provided a novel foundation upon which to surgically address these deformities. The fundamental basis involves creating a checkrein fixed dorsal to the DIP joint axis and volar to the PIP joint axis. The surgically constructed band, therefore, prevents excessive extension at the PIP joint while aiding in extension of the DIP joint (20).
Swan-neck deformity
Pathological hyperextension of the PIP joint (swan-neck deformity) can be caused by laxity or disruption of the volar plate. This allows the lateral bands to converge as they slide dorsally over the inclined facets of the phalangeal condyles, perpetuating the hyperextension (1, 21). Littler, in 1967, concurred with Landsmeer’s tenodesis theory and stated that “a strong oblique retinacular ligament can be simulated using a lateral band” (1). He described surgical correction of PIP joint hyperextension by transferring a single lateral band volarly. This procedure involves sectioning a lateral band proximally at the musculotendinous junction with a tenodesis to the flexor sheath, leaving the terminal insertion intact. This translocation places the lateral band volar to the axis of rotation of the PIP joint thus preventing PIP joint hyperextension as the finger is extended (1). Littler’s procedure requires an intact terminal extensor insertion, however, and would not address a mallet deformity secondary to extensor rupture (20).
In 1978, Thompson, Littler, and Upton modified the original Littler procedure by creating a spiral ORL (SORL) reconstruction to address swan-neck and/or mallet deformities (Figure 2) (20). In brief, a free tendon graft (e.g. palmaris longus) is fixed on the dorsal aspect of the distal phalanx with a vertical drill hole and button. The tendon is then passed over the radial aspect of the phalanx spiraling volarly across the palmar aspect of the PIP joint. A transverse hole through the proximal phalanx is created and the free tendon is passed through from the contralateral (ulnar) side and fixed with a button. As this technique is extra-anatomic, it can be performed in patients with ruptured terminal extensors. Thompson, Littler, and Upton’s method differs from Littler’s original technique in that it avoids disruption of the lateral bands and tension adjustments can be made with the buttons. Although Thompson, Littler, and Upton did not explicitly state the reason for the spiral course of the graft, this route ensures the graft will remain dorsal to the DIP joint and volar to the PIP joint. While technically challenging, Thompson, Littler, and Upton reported successful operations in 10 patients with a variety of joint deformities. Three months postoperatively, 8 PIP joints and 7 DIP joints achieved maximum active extension to 0 degrees.
Figure 2.
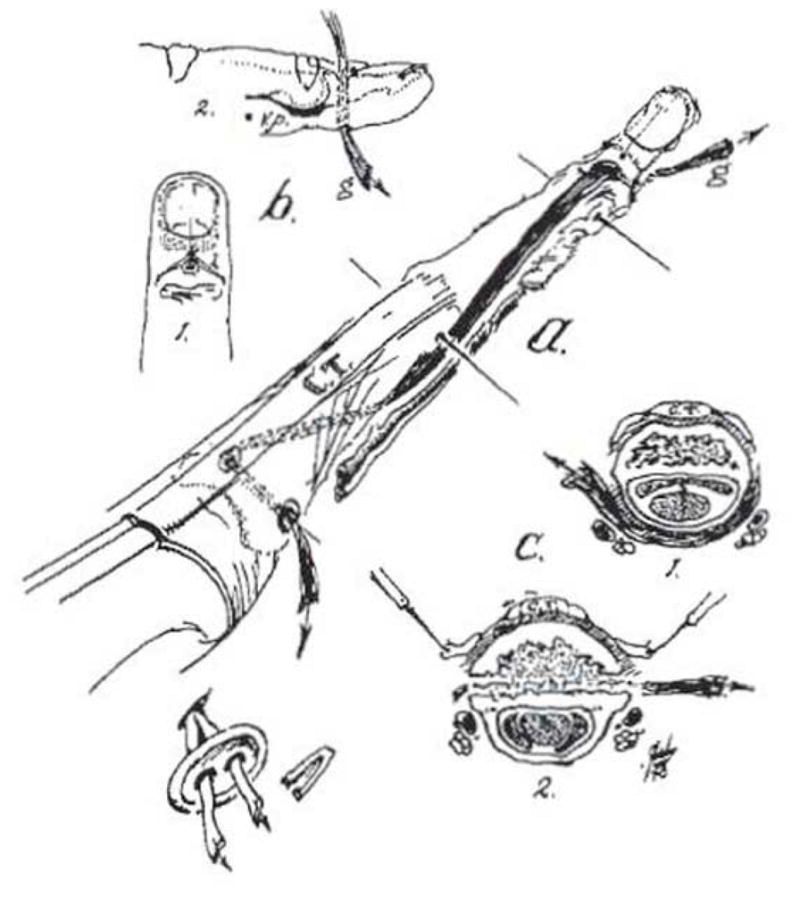
The SORL technique. The spiral course of the graft ensures a volar position at the PIP joint and dorsal position at the DIP joint (Reprinted with permission from Thompson JS, Littler JW, Upton J. The spiral oblique retinacular ligament (SORL). J Hand Surg Am. 1978;3(5):482–487.)
Mallet deformity
Mallet finger is a common injury resulting in a DIP joint flexion deformity and lack of voluntary DIP joint extension (1). Often there is terminal tendon incompetence and an unopposed flexor digitorum profundus. Volar plate or flexor digitorum superficialis laxity causing PIP joint hyperextension (swan-neck deformity), may also lead to mallet deformity by relaxing extensor mechanisms (1). Several techniques for surgical repair of mallet finger are currently available but have inconsistent results. These include tenorrhaphy, plication of elongated tendons, terminal tendon grafting, and release of the central slip from the middle phalanx (i.e. Fowler tenotomy) (22). In 1984, Kleinman and Petersen used Thompson, Littler, and Upton’s SORL concept to address passively correctable mallet deformities in 12 patients who sustained terminal tendon disruption. In contrast to the initially described bony fixation, the tendon graft was fixed at each end to soft tissue structures (Figure 3) (22). Correction of the deformity was successful in all 12 patients, with DIP joint extension restored to normal range in 9 patients while causing hyperextension (as much as +25 degrees) in the remaining 3.
Figure 3.
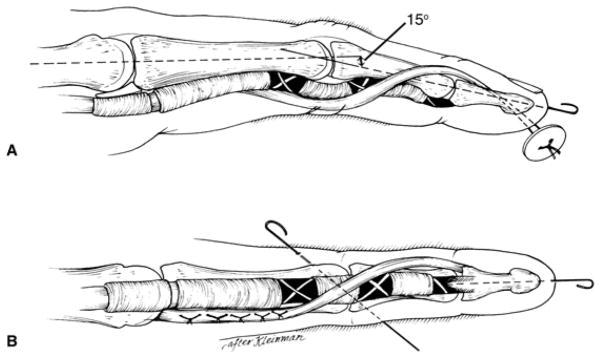
Kleinman and Petersen’s modification of Thompson’s SORL technique to address passively correctable mallet deformities (© 2005 American Academy of Orthopaedic Surgeons. Reprinted from the Journal of the American Academy of Orthopaedic Surgeons, Volume 13(5), pp. 336–344 with permission. This figure was adapted by the AAOS with permission from J Hand Surg (Am) 1984;9:399–404.
Other authors have successfully applied the SORL concept to address atypical mallet deformities. Kinoshita et al. used a free tendon graft to reconstruct the terminal tendon of a long finger after a free second-toe PIP joint transfer. One year following the transfer, the patient had a mallet deformity without active extension of the distal phalanx. A successful SORL procedure created a DIP joint in an anatomic alignment with the ability to flex from 0 to 50 degrees at 6 months postoperatively (23).
Contraction of the ORL
Dupuytren disease classically involves fibrous thickening and contracture of the palmar fascia. This affliction may cause fixed flexion or extension deformities at multiple joints when other connective tissues elements in the hand are involved (1, 17). Littler stated that Dupuytren disease involving the digital fascia resembles a contracted ORL (1). He referenced a manifestation of Dupuytren disease in the little finger that results in a PIP joint flexion contracture and a fixed extension of the terminal phalanx (boutonniere deformity). Though this posture of the digit appears consistent with ORL involvement, it is more likely secondary to soft tissue contraction as sequelae of cord progression. The relatively slow process eventually leads to lateral band displacement volarly causing PIP joint flexion and DIP joint extension.
Conclusion
One can draw the reasonable conclusion that the ORL plays a minor role linking DIP and PIP joint motion. This does not, however, undermine the importance of Landsmeer’s original dynamic interphalangeal tenodesis theory. His landmark research paved the way for Littler, Thompson, Upton, Kleinman, and others to develop surgical interventions aimed at correcting finger deformities commonly encountered in hand surgery. Surgical construction of a dynamic link between the PIP joint and DIP joint remains useful in the management of conditions such as swan-neck and mallet deformities. The presence and function of the ORL is controversial, but surgery directed at recreating its presumed role continues to provide successful outcomes.
Acknowledgments
Supported in part by grants from the National Institute on Aging and National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01 AR062066) and from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (2R01 AR047328-06) and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Littler JW. The finger extensor mechanism. Surg Clin North Am. 1967;47:415–432. doi: 10.1016/s0039-6109(16)38186-5. [DOI] [PubMed] [Google Scholar]
- 2.Kaplan EB. Functional and surgical anatomy of the hand. 2. Philadelphia, PA: J.B. Lippincott Co; 1965. pp. 42–43. [Google Scholar]
- 3.Harris C, Jr, Rutledge GL., Jr The functional anatomy of the extensor mechanism of the finger. J Bone Joint Surg. 1972;54A:713–726. [PubMed] [Google Scholar]
- 4.Ulrich F, Schmidt HM. Deep Ligaments of the interphalangeal joint of the thumb. Nato Adv Sci Inst Se. 1994;256:69–84. [Google Scholar]
- 5.Weitbrecht J. Syndesmology; or, A description of the ligaments of the human body, arranged in accordance with anatomical dissections and illustrated with figures drawn from fresh subjects. University of Otago; NZ: 1742. Retrieved August 2013. [Google Scholar]
- 6.Doyle JR, Botte MJ. Surgical Anatomy of the Hand and Upper Extremity. 1. Philadelphia, PA: Lippincott Williams & Wilkins; 2002. [Google Scholar]
- 7.el-Gammal TA, Steyers CM, Blair WF, et al. Anatomy of the oblique retinacular ligament of the index finger. J Hand Surg. 1993;18A:717–721. doi: 10.1016/0363-5023(93)90326-X. [DOI] [PubMed] [Google Scholar]
- 8.Kleinman WB, Petersen DP. Oblique retinacular ligament reconstruction for chronic mallet finger deformity. J Hand Surg. 1984;9:399–404. doi: 10.1016/s0363-5023(84)80231-2. [DOI] [PubMed] [Google Scholar]
- 9.Strauch RJ. Extensor Tendon Injury. In: Green DP, Hotchkiss RN, Pederson WC, editors. Green’s Operative Hand Surgery. 5. Vol. 163 New York, NY: Churchill Livingstone; 2005. [Google Scholar]
- 10.Davis TRC. Extensor Tendon Reconstruction after Chronic Injuries. In: Berger RA, Weiss APC, editors. Hand Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 11.Shrewsbury MM, Johnson RK. A systematic study of the oblique retinacular ligament of the human finger: its structure and function. J Hand Surg Am. 1977;2(3):194–199. doi: 10.1016/s0363-5023(77)80069-5. [DOI] [PubMed] [Google Scholar]
- 12.Tubiana R, Valentin P. The anatomy of the extensor apparatus of the fingers. Surg Clin N Amer. 1964;44:897. [PubMed] [Google Scholar]
- 13.Ueba H, Moradi N, Erne HC, et al. An anatomic and biomechanical study of the oblique retinacular ligament and its role in finger extension. J Hand Surg Am. 2011;36(12):1959–1964. doi: 10.1016/j.jhsa.2011.09.033. [DOI] [PubMed] [Google Scholar]
- 14.Schweitzer TP, Rayan GM. The terminal tendon of the digital extensor mechanism: Part I, anatomic study. J Hand Surg Am. 2004;29(5):898–902. doi: 10.1016/j.jhsa.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 15.Milford LW. Retaining Ligaments of the Digits of the Hand: Gross and Microscopic Anatomic Study. Philadelphia, PA: WB Saunders Co; 1968. [Google Scholar]
- 16.Landsmeer JM. The coordination of finger-joint motions. J Bone Joint Surg Am. 1963;45:1654–1662. [PubMed] [Google Scholar]
- 17.Haines RW. The extensor apparatus of the fingers. J Anat. 1951;85:251–259. [PMC free article] [PubMed] [Google Scholar]
- 18.Stack HG. Muscle function in the fingers. J Bone Joint Surg. 1962;44B:899–909. [Google Scholar]
- 19.Bendz P. The functional significance of the oblique retinacular ligament of Landsmeer. A review and new proposals. J Hand Surg Br. 1985;10(1):25–29. doi: 10.1016/s0266-7681(85)80009-7. [DOI] [PubMed] [Google Scholar]
- 20.Thompson JS, Littler JW, Upton J. The spiral oblique retinacular ligament (SORL) J Hand Surg Am. 1978;3(5):482–487. doi: 10.1016/s0363-5023(78)80144-0. [DOI] [PubMed] [Google Scholar]
- 21.Rockwell WB, Butler PN, Byrne BA. Extensor tendon: anatomy, injury and reconstruction. J Plast Recon Surg. 2000;106:1592–1603. doi: 10.1097/00006534-200012000-00024. [DOI] [PubMed] [Google Scholar]
- 22.Kleinman WB, Petersen DP. Oblique retinacular ligament reconstruction for chronic mallet finger deformity. J Hand Surg. 1984;9:399–404. doi: 10.1016/s0363-5023(84)80231-2. [DOI] [PubMed] [Google Scholar]
- 23.Kinoshita Y, Ogawa Y, Kojima T. Spiral oblique retinacular ligament (SORL) mallet correction in a finger with a proximal interphalangeal joint transferred from a toe. J Reconstr Microsurg. 1994;10(5):333–338. doi: 10.1055/s-2007-1006602. [DOI] [PubMed] [Google Scholar]