Abstract
Background
Current guidelines for evaluating cleft palate treatments are mostly based on two-dimensional (2D) evaluation, but three-dimensional (3D) imaging methods to assess treatment outcome are steadily rising.
Objective
To identify 3D imaging methods for quantitative assessment of soft tissue and skeletal morphology in patients with cleft lip and palate.
Data sources
Literature was searched using PubMed (1948–2012), EMBASE (1980–2012), Scopus (2004–2012), Web of Science (1945–2012), and the Cochrane Library. The last search was performed September 30, 2012. Reference lists were hand searched for potentially eligible studies. There was no language restriction.
Study selection
We included publications using 3D imaging techniques to assess facial soft tissue or skeletal morphology in patients older than 5 years with a cleft lip with/or without cleft palate. We reviewed studies involving the facial region when at least 10 subjects in the sample size had at least one cleft type. Only primary publications were included.
Data extraction
Independent extraction of data and quality assessments were performed by two observers.
Results
Five hundred full text publications were retrieved, 144 met the inclusion criteria, with 63 high quality studies. There were differences in study designs, topics studied, patient characteristics, and success measurements; therefore, only a systematic review could be conducted. Main 3D-techniques that are used in cleft lip and palate patients are CT, CBCT, MRI, stereophotogrammetry, and laser surface scanning. These techniques are mainly used for soft tissue analysis, evaluation of bone grafting, and changes in the craniofacial skeleton. Digital dental casts are used to evaluate treatment and changes over time.
Conclusion
Available evidence implies that 3D imaging methods can be used for documentation of CLP patients. No data are available yet showing that 3D methods are more informative than conventional 2D methods. Further research is warranted to elucidate it.
Systematic review registration
International Prospective Register of Systematic Reviews, PROSPERO CRD42012002041
Introduction
Patients with cleft lip and palate (CLP) are treated for an extended period of time. They often undergo several types of surgery as well as other treatment procedures by specialists collaborating with interdisciplinary teams from infancy until adulthood. The surgical procedures are necessary to reconstruct the anatomy of the alveolar arch and the face, and to restore the functions of the palate, lip muscles, and nose. Although treatment improves function and esthetics, it potentially can lead to tissue distortion and have a negative effect on craniofacial growth [1]. This may lead to less optimal facial esthetics along with negative psychosocial effects on a patient’s well-being [2], [3].
Many treatment protocols exist for the management of patients with CLP. Therefore, evaluating the results of treatment becomes more and more important. The Eurocleft study [4] evaluated treatment outcomes in Europe in the 1990s and recently the Americleft study [5], [6]–[9] examined treatment outcome in the US. Both studies proposed documentation and record taking for evaluation of treatment outcomes at certain time points, while they leave liberty for records at other time points. For record taking it appears that the first most complete data records are generally not documented earlier than age 5 [4], [5]. At this age, some records, especially dental casts, have a predictive value for growth and further treatment [10], [11].
It is expected that the majority of cleft palate treatment teams will use newly introduced three dimensional (3D) imaging technology to assess their treatment results. An increasing number of papers have been published regarding 3D evaluation of facial morphology and treatment outcomes in patients with clefts. Pharyngeal space is assessed with magnetic resonance imaging (MRI), computed tomography (CT), or cone beam computed tomography (CBCT). Results of bone grafting are evaluated with CT or CBCT. The jaw relationship, dental and alveolar arch, and the effects of surgery are examined with digital models and CBCT. The guidelines derived from Eurocleft, and later from Americleft, are still based on two-dimensional (2D) evaluation, except for dental casts, which are 3D by nature. Further evaluation may be needed to determine whether guidelines are necessary for the newer craniofacial imaging technologies.
A recent systematic review [12] about methods to quantify soft-tissue based facial growth and treatment outcomes in children younger than 6 years of age concluded that stereophotogrammetry seems to be the best method to longitudinally assess facial growth in these children. Studies on infants with CLP using 3D imaging techniques have been performed mainly to evaluate lip changes after surgery [13]–[15] and the effect of nasoalveolar molding [16].
A systematic review of existing 3D technologies for assessing treatment outcome in patients with CLP would provide clues for evaluating treatment effects and planning, as well as a comparison of treatment possibilities. Therefore, the objective of this systematic review was to identify 3D imaging methods that enable a quantitative analysis of facial soft tissues, velopharyngeal function and airway, skeletal morphology, and dentition in patients with cleft lip and palate.
Methods
Protocol and Registration
Inclusion criteria and methods of analysis were specified in advance and registered as a protocol in the International Prospective Register of Systematic Reviews, PROSPERO (http://www.crd.york.ac.uk/Prospero/). The registration number is: CRD42012002041. The protocol for this systematic review and supporting PRISMA checklist are available as supporting information; see Checklist S1 and Protocol S1.
Eligibility Criteria
Primary publications eligible for inclusion were those using 3D imaging techniques for assessing facial soft tissue or skeletal morphology in CLP patients. Further inclusion criteria were 1) cleft lip with or without cleft palate; 2) sample size larger than 10 for at least one cleft type; 3) patients 5 years of age or older; and 4) publications with quantitative assessment. Patients 5 years and older were included, because it appears that the first most complete data records are generally not documented earlier than age 5 [4], [5]. Exclusion criteria were: 1) craniofacial syndromes; 2) imaging only of neurocranium; 3) injury and trauma; 4) use of only 2D imaging techniques; and 5) reviews, expert opinions, letters, and case reports.
No restrictions were made for language, publication date, and publication status.
Information Resources
To identify publications, literature was searched until September 2012 using PubMed (1948–2012), EMBASE (1980–2012), Scopus (2004–2012), Web of Science (1945–2012), and the Cochrane Library. The last search was performed September 30th, 2012. Reference lists of identified manuscripts were then hand searched for potentially eligible studies. Digital full text publications were retrieved from licensed digital publishers and paper publications were retrieved from the university library. Authors were contacted when publications could not be retrieved. Gray literature was not searched.
Search Strategy
A search strategy and list of terms were developed and databases were selected with the help of a senior librarian specialized in health sciences. Medical subject headings and text words in the title and abstract were used for the search strategy in PubMed (Table 1) and search strategies for other databases were derived from this approach.
Table 1. PubMed search strategy.
| (((((((((4D[tiab] OR 4-dimensional[tiab])) OR (Four Dimensional Computed Tomography[tiab]))) OR (((((Tomography, X-Ray Computed[Mesh] OR Tomography, X-Ray Computed[tiab])) OR (Computed Tomographic[tiab] OR CT[tiab] OR volumetric CT[tiab])) OR (Cone Beam Computed Tomography[tiab] OR CBCT[tiab] OR Spiral Cone Beam Computed Tomography[tiab])) OR (Four Dimensional Computed Tomography[tiab]))) OR (((Photogrammetry[Mesh] OR Photogrammetry[tiab])) OR (stereophotogrammetr*[tiab]))) OR (((((computed tomography[tiab])) OR (computer assisted tomography[tiab]))) OR (((((Tomography, X-Ray Computed[Mesh] OR Tomography, X-Ray Computed[tiab])) OR (Computed Tomographic[tiab] OR CT[tiab] OR volumetric CT[tiab])) OR (Cone Beam Computed Tomography[tiab] OR CBCT[tiab] OR Spiral Cone Beam Computed Tomography[tiab])) OR (Four Dimensional Computed Tomography[tiab])))) OR (((Magnetic Resonance Imaging[Mesh] OR Magnetic Resonance Imaging[tiab] OR Magnetic Resonance Image[tiab] OR Magnetic Resonance Images[tiab])) OR (MRI[tiab]))) OR (((((Imaging, Three-Dimensional[Mesh] OR Imaging, Three-Dimensional[tiab])) OR (3D[tiab] OR three dimensional[tiab])) OR (3D[tiab] AND (image[tiab] OR images[tiab] OR imaging[tiab]))) OR (3D image[tiab] OR 3D images[tiab] OR 3D imaging[tiab]))) AND ((((cleft lip[Mesh] OR cleft lip[tiab])) OR (cleft palate[Mesh] OR cleft palate[tiab])) OR ((((CLP[tiab])) OR (UCLP[tiab])) OR (BCLP[tiab]))) |
The terms used in the search strategy were:
1- Concerning cleft lip and palate: Cleft lip, cleft palate, CLP, UCLP, BCLP
2-Three dimensional: Imaging three-dimensional, 3D, three dimensional, image, images, imaging, 3D image, 3D images, 3D imaging
3- CT: Tomography, X-ray computed, computed tomographic, CT, volumetric CT, computed tomography, computer assisted tomography
4- CBCT: Cone beam computed tomography, CBCT, spiral cone beam computed tomography
5- Photos: Photogrammetry, stereophotogrammetr*
6- MRI: Magnetic resonance imaging, magnetic resonance image*, MRI
7- 4D: 4D, 4-dimensional, four dimensional computed tomography
8- Ultrasound: Ultrasonography, echography
The title and abstract of studies were first independently screened by two reviewers (YC and MK). The reviewers were chosen based on their experience of 3D-techniques and cleft lip and palate treatment. Disagreements were resolved by discussion and consensus. After review of only the abstracts, they were scored as” included”, “excluded”, or “unclear”. Then, the full text was retrieved for included articles and articles with unclear abstracts. Full text assessments were performed independently by the same two reviewers. Disagreements were resolved by discussion and consensus. All studies were categorized by the method of imaging used.
Quality Assessment
The included studies were evaluated according to the quality assessment instrument used by Gordon et al [17]. This instrument includes an assessment of study bias and criteria, as shown in Table 2. Two reviewers utilized the quality assessment instrument (QAI) independent of each other (MK and YC). After that, disagreements were resolved by discussion and consensus. When no consensus could be reached, a senior researcher (PF) experienced with this QAI and also familiar with cleft lift and palate treatment made the final decision.
Table 2. Quality assessment instrument.
I. Study design (7
 )
)
|
A. Objective–objective clearly formulated ( ) ) |
B. Sample size–considered adequate ( ) ) |
C. Sample size–estimated before collection of data ( ) ) |
D. Selection criteria–clearly described ( ) ) |
E. Baseline characteristics–similar baseline characteristics ( ) ) |
F. Timing–prospective ( ) ) |
G. Randomization–stated ( ) ) |
II. Study measurements (3
 )
)
|
H. Measurement method–appropriate to the objective ( ) ) |
I. Blind measurement–blinding ( ) ) |
J. Reliability–adequate level of agreement ( ) ) |
III. Statistical analysis (5
 )
)
|
K. Dropouts–dropouts included in data analysis ( ) ) |
L. Statistical analysis–appropriate for data ( ) ) |
M. Confounders–confounders included in analysis ( ) ) |
N. Statistical significance level–P value stated ( ) ) |
O. Confidence intervals provided ( )Maximum number of )Maximum number of  s = 15 s = 15 |
(Gordon JM, Rosenblatt M, Witmans M, Carey JP, Heo G, Major PW, et al. Rapid palatal expansion effects on nasal airway dimensions as measured by acoustic rhinometry. A systematic review. Angle Orthod. 2009;79(5): 1000–1007.).
A checkmark was scored when a criterion was fulfilled. Depending on the study design, a maximum of 15 criteria could be scored. When certain criteria were not applicable for the study design, less than 15 criteria were scored and the non-applicable criteria were not used for assessing the overall study quality. Study quality was expressed as the number of criteria fulfilled divided by the total number of applicable criteria multiplied by 100. The studies were grouped according to the method of imaging. In cases where criteria were not applicable to the study design, the scoring was marked with a dot. Arbitrarily, a cut-off of 60% or higher was graded (after evaluation of the data) as good quality and below 60% was graded as poor quality [18].
Statistics
Cohens’s kappa statistics were used to assess the inter-observer reliability of the selection of articles based on the full text. The inter-rater reliability of the quality assessment was calculated using kappa statistics on 23 randomly selected articles scored by two reviewers (MK and YC). The strength of agreement was defined according to Landis and Koch [19]: poor (kappa <0.20), fair (kappa = 0.21–0.40), moderate (kappa = 0.41–0.60), good (kappa = 0.61–0.80), and very good (kappa = 0.81–1.00). Fisher’s exact test was performed to test for differences in quality between groups of methods with a cut-off score of 60% for the QAI. SPSS version 19.0 was used.
Results
Study Selection
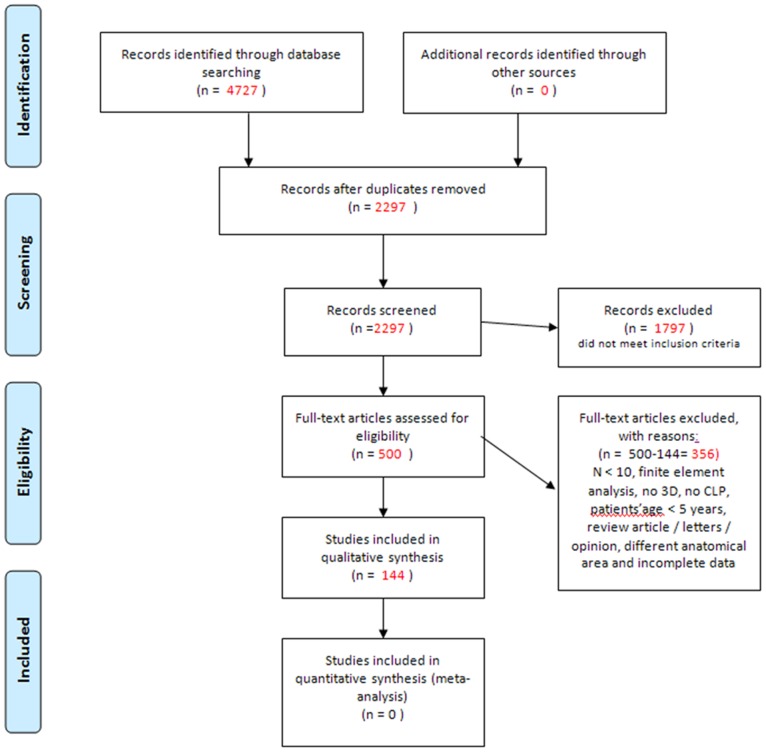
The inter-observer kappa for the reliability of study selection based on the full text was 0.76, which qualified as good [19]. The searches in PubMed, EMBASE, Cochrane Library, Web of Science, and Scopus yielded a total of 4727 citations and the hand search provided no additional publications. After adjusting for duplicates, the title and abstract of 2297 citations were screened. After this screening, 1797 articles were excluded because they did not meet the inclusion criteria. The full text was assessed for the 500 remaining articles. All of these articles were retrieved. All, except 2, articles were available in e-journals. Two articles were retrieved by contacting the author. Reasons for excluding studies after full text assessment were: different anatomical region; articles were letters, opinions, or reviews; and the studies applying finite element models. A total of 144 studies met the inclusion criteria. The PRISMA flow diagram is shown in Figure 1. Of the 144 included studies for this review, 49 used CT as a 3D imaging modality, 23 used CBCT, 21 studies involved 3D stereophotogrammetry, 26 studies used laser surface scanning (including n = 5 3D digital dental casts), 7 used MRI, and another method of 3D analysis was used in 18 studies [10], [11], [20]–[159].
Figure 1. PRISMA flow chart of the study selection process.
Quality Assessment of Studies
The inter-rater reliability for all 15 criteria of the QAI were between −0.42 and 1 (inter-observer kappa). The kappa’s for the different criteria (A to O) were: A = 1; B = 0.76; C = 1; D = 0; E = 0.39; F = 0.6; G = 0.52; H = −0.42; I = 0.28; J = 0.48; K = 0.64; L = 0.34; M = 0.67; N = 0.73; and O = 0.46. Eight of 15 criteria had a kappa of 0.50 or higher. The inter-rater reliability for criteria D (selection criteria – clearly described) and H (measurement method – appropriate to the objective) were below 0.20 with the reviewers disagreeing on 3 out of 23 articles.
The assessment of the methodological quality of all reviewed studies resulted in scores ranging from 8% to 92%. Of the 144 included studies, 63 (43.8%) qualified as good according to a methodological quality score ≥60% (Tables 3 to 8). Complete score summaries for the different imaging techniques are shown in Tables S1 to S6. Fisher’s exact test (p = 0.232) showed no statistically significant difference in the number of studies with good methodological quality among the groups of methods. The numbers of good (score >60%) and low quality studies were comparable for each method.
Table 3. Methodological quality scores of CT studies with an overall quality score of ≥60%.
| First author | Year | Topic | Study design | Measure | Statistics | Score | ||||||||||||
| A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | ||||
| Ras | 1997 | sagittal position maxilla |

|

|
o |

|

|
o | . |

|
. |

|
. |

|

|

|
o | 75% |
| Van der Meij | 2001 | bone graft quantity |

|

|
o |

|

|
o | . |

|
. |

|

|

|
o |

|
o | 69% |
| Kawakami | 2003 | bone graft height, density |

|
o | o |

|

|
o | . |

|
. |

|

|

|

|

|
o | 69% |
| Van der Meij | 2003 | bone graft |

|

|
o |

|

|
o | . |

|
. | o |

|

|

|

|

|
77% |
| Kita | 2004 | need bone graft |

|

|
o |

|

|
o | . |

|
. | o |

|

|

|

|

|
77% |
| Schliephake | 2006 | maxillary arch width |

|

|
o |

|

|
o | . |

|
. | o |

|

|
o |

|
o | 62% |
| Kim | 2008 | bone graft size, volume |

|
o | o |

|

|

|
. |

|
. |

|

|

|

|

|
o | 77% |
| Suri | 2008 | midface, maxilla |

|
o | o |

|

|
o | . |

|
. |

|
. |

|

|

|
o | 66% |
| Alonso | 2010 | bone graft size, volume |

|
o | o | o |

|

|

|

|

|

|

|

|

|

|
o | 73% |
| Saijo | 2010 | ossification pal suture |

|

|
o |

|

|
o | . |

|
. | o | . |

|
. |

|
. | 70% |
| Lee | 2011 | pterygomaxillary region |

|
o | o |

|

|
o | . |

|
o |

|
. |

|

|

|
o | 62% |
| Li | 2011 | maxilla |

|

|
o |

|

|
o | . |

|
. |

|
. |

|

|

|
o | 75% |
| Tulunoglu | 2011 | cephalometry 2d vs 3D |

|
o | o |

|

|
o | . |

|
. |

|
. |

|
. |

|
o | 63% |
| Choi | 2012 | ossification pal suture |

|

|
o |

|

|
o | . |

|
. | o | . |

|

|

|
o | 67% |
| Seike | 2012 | bone graft size, density |

|

|
o |

|
. | o | . |

|
. | o | . |

|
. |

|
o | 60% |
| Ye | 2012 | palatal shelf elevation |

|

|
o |

|

|
o | . |

|
. |

|

|

|
o |

|
o | 69% |
 = Fulfilled satisfactorily the methodological criteria;
= Fulfilled satisfactorily the methodological criteria;
o = Did not fulfill the methodological criteria;
. = Not applicable.
Table 8. Methodological quality scores of other studies with an overall quality score of ≥60%.
| First author | Year | Topic | Study design | Measure | Statistics | Score | ||||||||||||
| A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | ||||
| Kilpelainen | 1996 | asymmetry palate |

|

|
o |

|

|
o | . |

|
. | o | . |

|

|

|
o | 67% |
| Russell | 2001 | Nose |

|

|
o |

|
. | o | . |

|
. |

|
. |

|

|

|
o | 73% |
| Smahel | 2003 | Palate |

|

|
o |

|

|
o | . |

|
. |

|
. |

|
. |

|
o | 73% |
| Smahel | 2004 | Palate |

|

|
o |

|

|
o | . |

|
. |

|
. |

|
. |

|
o | 73% |
| Bilwatsch | 2006 | Nose |

|
o | o |

|

|
o | . |

|
. |

|
. |

|

|

|
o | 67% |
| Stauber | 2008 | Nose |

|

|
o | o | . | o | . |

|
. |

|
. |

|

|

|
o | 64% |
| Krey | 2009 | dental arches |

|

|
o |

|

|
o | . |

|
. | o | . |

|
. |

|
o | 64% |
| Trotman | 2010 | Lips |

|

|

|

|

|

|
o |

|
. | . | . |

|
o |

|
o | 75% |
| Russell | 2011 | Nose |

|

|
o |

|

|
o | . |

|

|
o | . |

|

|

|
o | 69% |
 = Fulfilled satisfactorily the methodological criteria;
= Fulfilled satisfactorily the methodological criteria;
o = Did not fulfill the methodological criteria;
. = Not applicable.
CT scanning was the most commonly applied method for 3D imaging of the head in patients with clefts (N = 49 studies; Table 3 and Table S1) [20]–[68]. CT scanning was mainly used to evaluate the results of bone grafting of the alveolar cleft. In addition, the technique was utilized to evaluate bone formation in the palatal cleft, nasal and sinus deformities, and the effects of surgery on the maxilla. The mean methodological score was 54% (range 25–77%). Sixteen (32,7%) of 49 studies [22], [27], [33]–[35], [41], [46], [48], [51], [53], [56]–[58], [61], [64], [66] had a good methodological quality (score of 60% or higher) and the highest score was 77%.
CBCT (N = 23 studies; Table 4 and Table S2) was also used to evaluate the results of bone grafting and to assess the amount of bone needed [69]–[91]. Yet, in the majority of the studies other structures were also assessed such as the pharyngeal airway, canines, alveolar bone adjacent to the cleft, mandible, and nasal morphology. The mean methodological score was 58% (range 18–85%). Of all 23 studies, 11 (47.8%) had a good quality score with the highest score being 85% [73–73,77–79,81,84,85,89,91].
Table 4. Methodological quality scores of CBCT studies with an overall quality score of ≥60%.
| First author | Year | Topic | Study design | Measure | Statistics | Score | ||||||||||||
| A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | ||||
| Dickinson | 2008 | bone graft |

|
o | o |

|

|

|

|

|

|

|

|

|
. |

|
o | 79% |
| Nagasao | 2008 | nasal septum |

|

|
o |

|

|
o | . |

|
. |

|
. |

|

|

|
o | 75% |
| Oberoi | 2009 | bone graft volume |

|
o | o |

|

|

|
. |

|
. |

|

|

|

|

|

|
85% |
| Oberoi | 2010 | canine |

|
o | o |

|

|
o | . |

|
. |

|

|

|
. |

|

|
75% |
| Shirota | 2010 | bone graft volume |

|
o | o |

|
. | o | . |

|

|

|
. |

|

|

|
o | 67% |
| Li, F. | 2011 | maxilla |

|

|
o |

|

|
o | o |

|
. |

|

|

|
. |

|
o | 69% |
| Veli | 2011 | Mandible |

|
o | o |

|

|
o | . |

|
o |

|
. |

|
. |

|

|
67% |
| Leenarts | 2012 | dental arches (Goslon) |

|
o | o |

|

|
o | . |

|
. |

|
. |

|
. |

|

|
73% |
| Li | 2012 | Nose |

|
o | o |

|

|
o | . |

|
. |

|
. |

|
. |

|
o | 63% |
| Trindade-Suedam | 2012 | bone graft |

|

|
o |

|

|

|
. |

|
. |

|
. |

|

|

|
o | 83% |
| Zhou | 2013 | tooth length |

|

|

|

|
o | o | . |

|
o |

|
. |

|
o |

|

|
69% |
 = Fulfilled satisfactorily the methodological criteria;
= Fulfilled satisfactorily the methodological criteria;
o = Did not fulfill the methodological criteria;
. = Not applicable.
MRI (N = 7 studies; Table 5 and Table S3) was utilized for speech assessments. The velopharyngeal space before and after palatal repair was studied as well as mobility of the lateral pharyngeal wall and the velum [92]–[98]. The mean methodological score was 40% (range 8–69%). The highest quality score was 69% and two studies (28.6%) had good methodological quality [97], [98].
Table 5. Methodological quality scores of MRI studies with an overall quality score of ≥60%.
| First author | Year | Topic | Study design | Measure | Statistics | Score | ||||||||||||
| A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | ||||
| Tian | 2010 | velopharyngeal space after palatal repair |

|
o | o |

|

|
o | . |

|
. |

|

|

|
o |

|

|
69% |
| Tian | 2010 | velopharyngeal motion after palatal repair |

|
o | o |

|

|
o | . |

|
. |

|

|

|
o |

|
o | 62% |
 = Fulfilled satisfactorily the methodological criteria;
= Fulfilled satisfactorily the methodological criteria;
o = Did not fulfill the methodological criteria;
. = Not applicable.
Thirteen (61.9%) [100], [103], [105], [107]–[111], [114], [116], [118], [119] of the 21 studies [99]–[119] using stereophotogrammetry (Table 6 and Table S4) had good quality methodological scores and 92% was the highest score. The mean methodological score was 64% (range 30–92%). Stereophotogrammetry was used for asymmetry assessment of the face, nose, and lips as well as for soft tissue changes after bone grafting or treatment with a Delaire protraction appliance. It was also used for treatment evaluation of lip repair.
Table 6. Methodological quality scores of stereophotogrammetry studies with an overall quality score of ≥60%.
| First author | Year | Topic | Study design | Measure | Statistics | Score | ||||||||||||
| A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | ||||
| Ras | 1994 | facial asymmetry |

|

|
o |

|
o | o | . |

|
. |

|
. |

|

|

|
o | 67% |
| Al-Omari | 2003 | facial deformity scoring |

|

|
o |

|
. | o | . |

|
. |

|
. |

|
. |

|

|
80% |
| Devlin | 2007 | nasal symmetry |

|
o | o |

|
. | o | . |

|
. |

|
. |

|
. |

|
o | 60% |
| Bugaighis | 2010 | facial shape |

|

|

|

|

|

|
. |

|
. |

|
. |

|

|

|
o | 92% |
| Hoefert | 2010 | soft tissue changes face |

|
o | o |

|

|

|
. |

|
. | o |

|

|
o |

|

|
69% |
| Hoefert | 2010 | soft tissue changes face |

|

|
o |

|

|
o | . |

|
. |

|

|
O | . | . | . | 70% |
| Tanikawa | 2010 | Lips |

|

|
o |

|
. | o | . |

|
. |

|
. |

|
o |

|
o | 64% |
| Van Loon | 2010 | Nose |

|

|
o |

|
o | o | . |

|
. |

|
. |

|

|

|

|
75% |
| Clark | 2011 | Lips |

|

|
o |

|

|
o | . |

|

|
o |

|

|

|

|
o | 71% |
| Kau | 2011 | maxilla/lip after bone graft |

|
o | o |

|
o |

|
. |

|

|
o | . |

|

|
o |

|
62% |
| Sander | 2011 | Nose |

|

|
o |

|

|

|
. |

|
o |

|

|

|

|

|
o | 79% |
| Zreaqat | 2012 | lips, eyes, nose, chin with controls |

|

|
o |

|

|
o | . |

|
. |

|
. |

|

|

|

|
77% |
| Millar | 2013 | facial asymmetry and scars |

|

|

|
o |

|
o | . |

|
. | o | . |

|

|

|
o | 67% |
 = Fulfilled satisfactorily the methodological criteria;
= Fulfilled satisfactorily the methodological criteria;
o = Did not fulfill the methodological criteria;
. = Not applicable.
Laser scanners (N = 24; Table 7 and Table S5) were used for scanning faces to assess asymmetries and to evaluate changes of the nose, lips, and facial soft tissue before and after surgery [6], [7], [120]–[141]. They were also used to reconstruct digital dental models. The dental models were used to study palatal morphology and dental arch relationships. The dental arch relationship scores on 3D models were compared with plaster cast scores and 2D pictures to evaluate if digital dental models can be used for inter-center studies concerning treatment outcome. The mean methodological score was 58% (range 23–78%). Eleven (45.8%) of 24 studies [6], [7], [122]–[125], [129]–[131], [140], [141] had a good methodological quality and the highest score was 78%.
Table 7. Methodological quality scores of laser surface scanning studies with an overall quality score of ≥60%.
| First author | Year | Topic | Study design | Measure | Statistics | Score | ||||||||||||
| A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | ||||
| Bennun | 1999 | Nose |

|

|
o |

|

|

|

|

|
o | O | . |

|

|

|
o | 71% |
| Duffy | 2000 | chin, nose, lips |

|
o | o |

|

|
o | . |

|
. |

|
. |

|
. |

|
o | 64% |
| Honda | 2002 | maxillofacial morphology |

|

|
o |

|

|
o | . |

|
. |

|

|

|

|

|
o | 77% |
| Mori | 2005 | nose, lips |

|

|
o |

|

|
o | . |

|
. | O | . |

|
. |

|
o | 64% |
| Meyer-Marcotty | 2009 | asymmetry face lay vs specialist |

|

|
o |

|

|
o | . |

|
. |

|
. |

|
. |

|
o | 73% |
| Smahel | 2009 | palatal morph |

|

|
o |

|

|
o | . |

|
. |

|
. |

|
. |

|
o | 73% |
| Meyer-Marcotty | 2010 | Face |

|
o | o |

|

|
o |

|

|
. |

|
. |

|

|

|
o | 69% |
| Asquith | 2012 | dental arches (5-yr-olds' index) |

|

|
o | o | . | o | . |

|

|

|
. |

|

|

|
o | 67% |
| Chawla | 2012 | dental arches (5-yr-olds' index) |

|

|
o |

|
. | o | . |

|

|

|
. |

|
. | . | . | 78% |
| Dogan | 2012 | dental arches (Goslon) |

|

|
o |

|
. | o | . |

|

|

|
. |

|
. | . | . | 78% |
| Chawla | 2013 | dental arches (5-yr-olds' index) |

|

|
o |

|

|
o | . |

|
. |

|
. |

|
. | . | . | 78% |
 = Fulfilled satisfactorily the methodological criteria;
= Fulfilled satisfactorily the methodological criteria;
o = Did not fulfill the methodological criteria;
. = Not applicable.
Various other methods (Table 8 and Table S6) were used that provide 3D coordinates of anatomical structures [142]–[159], like structured lights to create Moiré patterns, reflex microscopy, electromagnetic digitizers, and video tracking. Several studies evaluated palatal morphology, other studies looked at facial asymmetry, nasal asymmetry, and nasal and lip esthetics. One study measured the effect of nasoalveolar molding on the nose [144]. The mean methodological score was 62% (range 36–75%). The highest quality score in this group was 75% and nine of 18 studies (50%) had a good methodological quality [143], [148], [153]–[159].
Reliability
Scores for reliability and measurement errors of the studies with good methodological quality (score >60%) are shown in Table 9. The majority of the studies reported inter- and intra-rater reliability and the methods used to assess these factors were appropriate for the measurements performed. However, the magnitude of the random error was reported only in a minority of studies.
Table 9. Reliability of methods for 3D imaging in cleft lip and palate patients in studies with good methodological quality.
| first author | Year | Topic | raters | subjects/objects included in error analysis | duplicate measurements | reliability corr coeff | systematic error determined | Randomerror | weighted kappa |
| CT | |||||||||
| Ras | 1997 | maxilla, position(mm) | 2 | 17 | 2 | y | |||
| van der Meij | 2001 | bone graft quantity, surface (mm2) | 1 | 1 | 10 | 1.95%* | |||
| Kawakami | 2003 | bone graft density (grading scale) | 1 | 19 | 2 | 0.99 | y | ||
| van der Meij | 2003 | bone graft, surface (mm2) | – | – | – | ||||
| Kita | 2004 | bone graft, need (grading scale) | 2 | 24 | 0 | ||||
| Schliephake | 2006 | maxillary arch width (mm) | – | – | – | ||||
| Kim | 2008 | bone graft, volume(mm3) | 1 | 15 | 2 | y | |||
| 2 | 15 | 2 | y | ||||||
| Suri | 2008 | midface (mm) | 1 | 3 | 3 | y | |||
| Alonso | 2010 | bone graft, bone fill (%) | 1 | 16 | 2 | y | |||
| Saijo | 2010 | pal suture, ossification (mm) | – | – | – | ||||
| Lee | 2011 | pterygomaxillary region (mm) | – | 10 | 2 | y | 0.4 | ||
| Li | 2011 | maxilla (mm) | 1 | – | 2 | y | |||
| Tulunoglu | 2011 | cephalometry 3D (mm, degrees) | 1 | 15 | 2 | 0.88–0.99 | |||
| Choi | 2012 | pal suture, ossification (mm) | – | – | – | ||||
| Seike | 2012 | bone graft, size (mm), bone graft, density (mg Calcium) | – | – | – | ||||
| Ye | 2012 | maxillary arch width (mm) | 1 | 30 | 3 | 0.84 | |||
| CBCT | |||||||||
| Dickinson | 2008 | bone graft (grading system) | 3 | – | - | 1.9%* | |||
| Nagasao | 2008 | nasal septum (mm) | – | – | – | ||||
| Oberoi | 2009 | bone graft, bone fill (%) | 1 | 5 | 2 | >0.9 | |||
| 2 | 5 | 2 | >0.9 | ||||||
| Oberoi | 2010 | Canine, eruption (mm) | 2 | 10 | 2 | 0.3–1.03 | |||
| Shirota | 2010 | bone graft, volume(cm3) | 1 | 13 | 3 | ||||
| Li, F | 2011 | Maxilla, position (mm) | 1 | 20 | 2 | 0.98 | |||
| Veli | 2011 | Mandible (mm, mm3) | – | 15 | 2 | y | |||
| Leenarts | 2012 | dental arch relationship (1–5 Goslon grading scale) | 4 | 26 | 2 | 0.83–0.97 | y | 0.18–0.45 | 0.72–0.93 |
| Li | 2012 | Nose, angles (degrees) | 2 | 16 | 2 | 0.98–0.99 | |||
| 1 | 16 | 2 | 0.94–0.99 | ||||||
| Trindade–Suedam | 2012 | bone graft, presence of bone (grading scale) | 3 | –– | 2 | y | |||
| Zhou | 2013 | Teeth movement (mm) | 1 | 20 | 2 | 2%* | |||
| MRI | |||||||||
| Tian | 2010 | velopharyngeal space(mm) | 1 | 2 | 2 | 0.92–0.99 | |||
| 2 | 2 | 2 | 0.89–0.98 | ||||||
| Tian | 2010 | velopharyngeal motion (mm, ratios) | 1 | 6 | 2 | 0.92–0.99 | |||
| 2 | 6 | 2 | 0.89–0.98 | ||||||
| Stereophotogrammetry | |||||||||
| Ras | 1994 | face, asymmetry (mm) | 1 | 10 | 4 | y | |||
| Al–Omari | 2003 | face, deformity scoring (rating scale) | 10 | 31 | 2 | 0.42–0.72 | |||
| Devlin | 2007 | nose, symmetry (mm) | 1 | 1 | 10 | 0.46 | |||
| Bugaighis | 2010 | face, shape (mm) | – | – | – | 0.5 | |||
| Hoefert | 2010 | face, controls (mm) | 1 | 7 | 10 | ||||
| CLP (mm) | 1 | 22 | 10 | ||||||
| Hoefert | 2010 | face (mm) | 1 | 29 | 10 | 0.31–0.55 | |||
| Tanikawa | 2010 | lips (mm) | 1 | 10 | 2 | ||||
| van Loon | 2010 | Nose, volume (mm3) | 1 | 12 | 2 | 0.97–1.00 | y | 55.68–129.86 | |
| 2 | 12 | 2 | 0.96–1.00 | y | 56.32–147.40 | ||||
| Clark | 2011 | lips (mm) | – | – | – | ||||
| Kau | 2011 | maxilla/lip (mm) | – | – | – | ||||
| Sander | 2011 | Nose (mm) | 1 | 9 | 3 | 0.99 | |||
| Zreaqat | 2012 | face (mm) | 1 | 20 | 2 | 0.97–0.98 | |||
| Millar | 2013 | facial asymmetry, scars (algorithm score, ratios, scale) | – | – | – | ||||
| Laser surface scanning | |||||||||
| Bennun | 1999 | Nose (mm) | – | – | – | ||||
| Duffy | 2000 | chin, nose, lips (mm) | 2 | 16 | 2 | 0.47–5.4%* | |||
| Honda | 2002 | Maxillary dental arch (mm, mm2, degrees) | – | – | – | ||||
| Mori | 2005 | nose, lips (mm, degrees) | – | – | – | ||||
| Meyer–Marcotty | 2009 | Face, asymmetry (mm) | – | – | 2 | <0.006 | |||
| Smahel | 2009 | palate (mm) | – | – | – | >0.98 | 0.03–2.45 | ||
| Meyer–Marcotty | 2010 | Face (mm) | – | – | 2 | <0.006 | |||
| Chawla | 2012 | dental arches (1–5grading scale of 5-yr-olds' index) | 7 | 45 | 2 | 0.67–0.88 | |||
| Asquith | 2012 | dental arches (1–5 grading scale of 5-yr-olds' index) | 3 | 30 | 2 | 062–0.83 | |||
| Dogan | 2012 | dental arches (1–5 Goslon grading scale) | 2 | 70 | 3 | 0.82–0.96 | |||
| Chawla | 2013 | dental arches (1–5grading scale of 5-yr-olds' index) | 3 | 45 | 2 | 0.74–0.83 | |||
| Other | |||||||||
| Kilpelainen | 1996 | palate (mm, degrees) | – | – | – | ||||
| Russell | 2001 | Nose (degrees, VAS scale) | 6 | 28 | 1 | 0.74 | |||
| Smahel | 2003 | Palate (mm, mm2) | 1 | – | 2 | >0.95 | 0.03 | ||
| Smahel | 2004 | Palate (mm, mm2) | 1 | – | 2 | >0.95 | 0.03 | ||
| Bilwatsch | 2006 | nose (mm, degrees) | – | 22 | 2 | y | <1mm, <1.50 | ||
| Stauber | 2008 | nose (mm, degrees) | – | 40 | 2 | y | <1mm, <1.50 | ||
| Krey | 2009 | dental arches (mm) | – | – | – | ||||
| Trotman | 2010 | Lips, distances and movements (mm) | – | – | – | ||||
| Russell | 2011 | Nose (VAS), | 6 | 48 | 1 | 0.74 | |||
* = maximum of variable of landmark/distance reproducibility.
Discussion
The number of publications listed in PubMed on 3D-imaging in CLP patients is steadily rising. A wide variety of different 3D imaging techniques and evaluation methods are used for the craniofacial skeleton and surrounding soft tissues. Below, we discuss the results of this systematic review concerning the 3D-techniques for facial soft tissues, velopharyngeal function and the airway, the craniofacial skeleton, and dentition.
Soft Tissue Analysis
The majority of the studies concerning soft tissues that had a methodological quality ≥60% were performed with laser surface scanning (Table 6) or stereophotogrammetry (Table 7). However, only a few studies reported the magnitude of the measurement error (Table 9). The maximum reported error for soft tissue measurements with 3D-stereophotogrammetry and laser surface scanning was 0.55 mm [109]. Bilwatsch [155] and Stauber [156] used an optical 3D sensor to acquire facial surface data (Table 8) and they reported a measurement error <1 mm. Only one study reported a measurement error for volume measurements of the nose, with a maximum of 147.40 mm3 [111].
Based on the measurement errors in the good quality studies, laser surface scanning and 3D stereophotogrammetry seem to be reliable methods for quantitatively measuring asymmetry and 3-dimensional changes in soft tissues after treatment. For qualitative scoring of asymmetry and esthetics using an expert panel, it is necessary to familiarize the panel members with 3D-stereophotogrammetrical images prior to the scoring task [103]. Dynamic 4D-assessment of soft tissues can register functional repair, but this technique still is in its infancy as only 1 high quality study was found [158].
Velopharyngeal Function and the Airway
CT and CBCT were used to assess the bony structures of the nose and development of sinuses. Some CBCT and CT studies examined the distances and volumes of the pharyngeal airway space [28], [60], [82], [90]. None of these studies had a high quality score; therefore, we are not able to draw conclusions on the value of CT and CBCT for measuring the airway space in CLP. In two high quality studies, MRI was used to evaluate velopharyngeal function at rest and during phonation, but the random error was not reported [97], [98]. This may indicate that MRI is an adequate, although expensive, technique for measuring the space and motion of the pharyngeal airway.
Craniofacial Skeleton
CT and CBCT are mainly used for planning orthognathic surgery before and after treatment and for assessing anatomical differences in the nose [47], [56], [79], [81], [85]. These techniques are also used for treatment planning and measuring the results of bone grafting [30], [33]–[35], [46], [64], [73], [75], [77], [78], [89]. Most studies report that no systematic measurement error was present, but the magnitude of the random error was hardly ever reported.
CBCT is a recent radiological technique that became more widely available for imaging the craniofacial region after 2005. CT, which has a much higher radiation dose, was the most commonly used technique for 3D-imaging before CBCT. The SEDENTEXCT Consortium stated, in regards to the radiation dose, that ‘’the application of CBCT in cleft lip and palate patients was found to be the simplest to support’’ in dentistry [160]. They further stated that CBCT may be preferred in situations where CT scanning is currently used for the assessment of cleft lip and palate. The few studies concerning CT or CBCT that reported the reliability showed an acceptable measurement error for both techniques. Therefore, CBCT imaging could be the preferred method for assessing bone volume, as well as for surgical planning, since it has a lower radiation dose than CT scanning. However, further investigation is necessary to determine the influence of this new 3D facial imaging modality on treatment planning, treatment outcome, and treatment evaluation.
Dentition
Laser surface scanning, CT, CBCT, or moiré photography are used for reconstruction of digital dental casts from plaster casts or from scanning of the impressions [6], [7], [41], [66], [84], [130], [140]–[142], [153], [154], [157]. The majority of these studies reported good reliability. Some studies compared digital models, plaster models, and 2D photographs to assess if digital models can be used to assess outcome and future treatment expectations with the GOSLON yardstick or the 5-year olds’ index [84], [140], [141]. When overlooking the measurement errors in the high quality studies, it seems that digital models obtained with the aid of 3D imaging are a valid alternative for plaster models when assessing treatment outcome with a yardstick as well as for assessment of arch width and palatal morphology.
The dentition has also been studied with CT and CBCT. The bone height of teeth next to the bone graft, eruption, and dental abnormalities have been studied [77], [79], [91] and good reliability was reported. Although the SEDENTEXCT statement [160] includes CLP as one of the few justified reasons for a CBCT in dentistry, there are currently no studies that confirm changes in the diagnosis lead to better treatment planning or outcome in CLP patients when three-dimensional X-rays were used instead of 2D X-rays [18]–[160]. Therefore, the cost benefit of 3D radiology in this situation should be considered.
Limitations of this Systematic Review
The methodological qualities of the selected articles were assessed according to a scoring system repeatedly used in systematic reviews in orthodontics, which was originally developed by Lagravere [161] and later adapted by Gordon [17]. The method is mainly used for assessing the quality of prospective randomized studies. Only 63 out of 142 studies qualified as being of good methodological quality. The studies were mostly retrospective with relatively small sample sizes and often used descriptive outcome variables. Some criteria used for this study (Table 2), such as the estimation of appropriate sample size before data collection (C), prospective study design (F), randomization (G), and blinding (I), which are all are crucial criteria for high quality studies, were rarely scored as being fulfilled satisfactorily in our systematic review. This was partly due to the patient populations, which make blinding as well as randomization difficult. These were limitations inherent to the scoring system used. Yet, we decided to use this scoring system for the assessment of methodological quality of non-randomized studies [162] as there is no other obvious candidate for assessing these type of studies [162]. Other quality assessment instruments, like the Newcastle-Ottawa scale [162] or Jadad scale [163], [164], used for retrospective studies produce highly arbitrary results [162], [163]. There is still a need for a validated quality assessment instrument that is applicable for a wide range of study designs.
The range of inter-observer kappa values for the quality assessment score was −0.42 to 1.0, indicating strengths of agreement from extremely poor to almost perfect. The low kappa values for criteria D (selection criteria) and H (measurement method) in the quality assessment can be explained by the kappa value being influenced by trait prevalence. A single disagreement in scoring between two observers could determine whether the kappa value is 1.0 or 0.0. The absence of adequate instructions for the QAI may lead to different interpretations of the data. In addition, difficulties in interpretation of the data due to its presentation and a lack of information concerning methodology in the published papers may explain the wide range in inter-rater kappa scores.
Conclusions
CT, CBCT, MRI, stereophotogrammetry, and laser surface scanning are the most frequently used 3D techniques in cleft lip and palate patients. These techniques are mainly used for soft tissue analysis, evaluation of bone grafting, and changes in the craniofacial skeleton. MRI seems to be a reliable, although expensive method to determine velopharyngeal function. Digital dental casts are used to evaluate treatment and changes over time. Available evidence implies that 3D imaging methods can be used for documentations of CLP patients. However, there is no data yet showing that 3D methods are more informative than conventional 2D methods. Further research is warranted to elucidate this and to enable the development of new guidelines for documentation and record taking in cleft lip and palate patients.
Supporting Information
Methodological quality scores of CT studies.
(DOCX)
Methodological quality scores of CBCT studies.
(DOCX)
Methodological quality scores of MRI studies.
(DOCX)
Methodological quality scores of stereophotogrammetry studies.
(DOCX)
Methodological quality scores of laser surface scanning studies.
(DOCX)
Methodological quality scores of other studies.
(DOCX)
PRISMA checklist.
(DOCX)
Protocol for the systematic review as registered in PROSPERO (registration number: CRD42012002041).
(PDF)
Acknowledgments
We are grateful to our librarian of health sciences, Elmie Peters, for her support in the development of the search strategies.
Funding Statement
These authors have no support or funding to report.
References
- 1.Kuijpers-Jagtman AM, Long RE (2000) The Influence of surgery and orthopedic treatment on maxillofacial growth and maxillary arch development in patients treated for orofacial clefts. Cleft Pal Craniofac J 37: 527[1] –527[12].
- 2. Bos A, Prahl C (2011) Oral health-related quality of life in Dutch children with cleft lip and/or palate. Angle Orthod 81: 865–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wehby GL, Cassel CH (2010) The impact of orofacial clefts on quality of life and healthcare use and costs. Oral Dis 16;3–10. [DOI] [PMC free article] [PubMed]
- 4.Shaw WC, Semb G, Nelson P, Brattström V, Mølstred K, et al.. (2000) The Eurocleft Project 1996–2000. IOS Press, Amsterdam.
- 5.American Cleft Palate Association (2009) Guidelines for team evaluation American Cleft Palate Association. Available: http://www.acpa-cpf.org/uploads/site/Parameters_Rev_2009.pdf. Accessed 2014 Mar 16.
- 6. Long RE Jr, Hathaway R, Daskalogiannakis J, Mercado A, Russell K, et al. (2011) The Americleft study: an inter-center study of treatment outcomes for patients with unilateral cleft lip and palate part 1. Principles and study design. Cleft Palate Craniofac J 48: 239–243. [DOI] [PubMed] [Google Scholar]
- 7. Hathaway R, Daskalogiannakis J, Mercado A, Russell K, Long RE Jr, et al. (2011) The Americleft study: an inter-center study of treatment outcomes for patients with unilateral cleft lip and palate part 2. Dental arch relationships. Cleft Palate Craniofac J 48: 244–251. [DOI] [PubMed] [Google Scholar]
- 8. Mercado A, Russell K, Hathaway R, Daskalogiannakis J, Sadek H, et al. (2011) The Americleft study: an inter-center study of treatment outcomes for patients with unilateral cleft lip and palate part 4. Nasolabial aesthetics. Cleft Palate Craniofac J 48: 259–264. [DOI] [PubMed] [Google Scholar]
- 9. Russell K, Long RE Jr, Hathaway R, Daskalogiannakis J, Mercado A, et al. (2011) The Americleft study: an inter-center study of treatment outcomes for patients with unilateral cleft lip and palate part 5. General discussion and conclusions. Cleft Palate Craniofac J 48: 265–270. [DOI] [PubMed] [Google Scholar]
- 10. Asquith J, McIntyre G (2012) Dental arch relationships on three-dimensional digital study models and conventional plaster study models for patients with unilateral cleft lip and palate. Cleft Palate Craniofac J 49: 530–4. [DOI] [PubMed] [Google Scholar]
- 11. Chawla O, Deacon SA, Atack NE, Ireland AJ, Sandy JR (2011) The 5-year-olds' Index: determining the optimal format for rating dental arch relationships in unilateral cleft lip and palate. Eur J Orthod 2012 34: 768–72. [DOI] [PubMed] [Google Scholar]
- 12. Brons S, van Beusichem ME, Bronkhorst EM, Draaisma J, Bergé SJ, et al. (2012) Methods to quantify soft-tissue based facial growth and treatment outcomes in children: a systematic review. PLoS ONE 7: e41898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ayoub A, Garrahy A, Millett D, Bowman A, Siebert JP, et al. (2011) Three-dimensional assessment of early surgical outcome in repaired unilateral cleft lip and palate: Part 1. Nasal changes. Cleft Palate Craniofac J 48: 571–577. [DOI] [PubMed] [Google Scholar]
- 14. Ayoub A, Bell A, Simmons D, Bowman A, Brown D, et al. (2011) Three-dimensional assessment of early surgical outcome in repaired unilateral cleft lip and palate: part 2. Lip changes. Cleft Palate Craniofac J 48: 578–583. [DOI] [PubMed] [Google Scholar]
- 15. van Loon B, Reddy SG, van Heerbeek N, Ingels KJ, Maal TJ, et al. (2011) 3D stereophotogrammetric analysis of lip and nasal symmetry after primary cheiloseptoplasty in complete unilateral cleft lip repair. Rhinology 49: 546–553. [DOI] [PubMed] [Google Scholar]
- 16. Simanca E, Morris D, Zhao L, Reisberg D, Viana G (2011) Measuring progressive soft tissue change with nasoalveolar molding using a three-dimensional system. J Craniofac Surg 22: 1622–1625. [DOI] [PubMed] [Google Scholar]
- 17. Gordon JM, Rosenblatt M, Witmans M, Carey JP, Heo G, et al. (2009) Rapid palatal expansion effects on nasal airway dimensions as measured by acoustic rhinometry. A systematic review. Angle Orthod 79: 1000–1007. [DOI] [PubMed] [Google Scholar]
- 18. van Vlijmen OJ, Kuijpers MA, Bergé SJ, Schols JG, Maal TJ, et al. (2012) Evidence supporting the use of cone-beam computed tomography in orthodontics. J Am Dent Assoc 143: 241–52. [DOI] [PubMed] [Google Scholar]
- 19. Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33: 159–174. [PubMed] [Google Scholar]
- 20. Dado DV, Rosenstein SW, Alder ME, Kernahan DA (1997) Long-term assessment of early alveolar bone grafts using three-dimensional computer-assisted tomography: a pilot study. Plast Reconstr Surg 99: 1840–1845. [DOI] [PubMed] [Google Scholar]
- 21. McCance AM, Moss JP, Fright WR, Linney AD, James DR, et al. (1997) Three-dimensional analysis techniques–Part 4: Three-dimensional analysis of bone and soft tissue to bone ratio of movements in 24 cleft palate patients following Le Fort I osteotomy: a preliminary report. Cleft Palate Craniofac J 34: 58–62. [DOI] [PubMed] [Google Scholar]
- 22. Ras F, van Aalten L, Janse A, Mobers S, Prahl-Andersen B (1997) Sagittal position of the left and right maxillary segment in children with cleft lip and palate. Cleft Palate Craniofac J 34: 438–442. [DOI] [PubMed] [Google Scholar]
- 23. Rosenstein SW, Long RE Jr, Dado DV, Vinson B, Alder ME (1997) Comparison of 2-D calculations from periapical and occlusal radiographs versus 3-D calculations from CAT scans in determining bone support for cleft-adjacent teeth following early alveolar bone grafts. Cleft Palate Craniofac J 34: 199–205. [DOI] [PubMed] [Google Scholar]
- 24. Santiago PE, Grayson BH, Cutting CB, Gianoutsos MP, Brecht LE, et al. (1998) Reduced need for alveolar bone grafting by presurgical orthopedics and primary gingivoperiosteoplasty. Cleft Palate Craniofac J 35: 77–80. [DOI] [PubMed] [Google Scholar]
- 25. Denny AD, Talisman R, Bonawitz SC (1999) Secondary alveolar bone grafting using milled cranial bone graft: A retrospective study of a consecutive series of 100 patients. Cleft Palate Craniofac J 36: 144–153. [DOI] [PubMed] [Google Scholar]
- 26. Honma K, Kobayashi T, Nakajima T, Hayasi T (1999) Computed tomographic evaluation of bone formation after secondary bone grafting of alveolar clefts. J Oral Maxillofac Surg 57: 1209–1213. [DOI] [PubMed] [Google Scholar]
- 27. Suzuki H, Yamaguchi T, Furukawa M (1999) Rhinologic computed tomographic evaluation in patients with cleft lip and palate. Arch Otolaryngol Head Neck Surg 125: 1000–1004. [DOI] [PubMed] [Google Scholar]
- 28. Suzuki H, Yamaguchi T, Furukawa M (2000) Maxillary sinus development and sinusitis in patients with cleft lip and palate. Auris Nasus Larynx 27: 253–256. [DOI] [PubMed] [Google Scholar]
- 29. Tai CC, Sutherland IS, McFadden L (2000) Prospective analysis of secondary alveolar bone grafting using computed tomography. J Oral Maxillofac Surg 58: 1241–1249. [DOI] [PubMed] [Google Scholar]
- 30. Van der Meij AJ, Baart JA, Prahl-Andersen B, Valk J, Kostense PJ, et al. (2001) Bone volume after secondary bone grafting in unilateral and bilateral clefts determined by computed tomography scans. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 92: 136–141. [DOI] [PubMed] [Google Scholar]
- 31. Kolbenstvedt A, Aalokken TM, Arctander K, Johannessen S (2002) CT appearances of unilateral cleft palate 20 years after bone graft surgery. Acta radiologica 43: 567–570. [DOI] [PubMed] [Google Scholar]
- 32. Raphaël B, Morand B, Bettega G, Lesne C, Lesne V (2002) Alveolar and hard palate repair by tibial periosteal graft in complete unilateral cleft lip and palate. Long-term follow-up about 51 clinical cases. Ann Chir Plast Esthet 47: 196–203. [DOI] [PubMed] [Google Scholar]
- 33. Kawakami S, Hiura K, Yokozeki M, Takahashi T, Seike T, et al. (2003) Longitudinal Evaluation of Secondary Bone Grafting into the Alveolar Cleft. Cleft Palate Craniofac J 40: 569–576. [DOI] [PubMed] [Google Scholar]
- 34. van der Meij AW, Baart JA, Prahl-Andersen B, Kostense PJ, van der SijpJR, et al. (2003) Outcome of bone grafting in relation to cleft width in unilateral cleft lip and palate patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 96: 19–25. [DOI] [PubMed] [Google Scholar]
- 35. Kita H, Kochi S, Kamiya N, Yamada A, Mitani H (2004) Alveolar ridge notching as a predictor for secondary bone grafting in incomplete alveolar clefts. Cleft Palate Craniofac J 41: 36–41. [DOI] [PubMed] [Google Scholar]
- 36. Arctander K, Kolbenstvedt A, Aalokken TM, Abyholm F, Froslie KF (2005) Computed tomography of alveolar bone grafts 20 years after repair of unilateral cleft lip and palate. Scand J Plast Reconstr Surg Hand Surg 39: 11–14. [DOI] [PubMed] [Google Scholar]
- 37. Iino M, Ishii H, Matsushima R, Fukuda M, Hamada Y, et al. (2005) Comparison of intraoral radiography and computed tomography in evaluation of formation of bone after grafting for repair of residual alveolar defects in patients with cleft lip and palate. Scand J Plast Reconstr Surg Hand Surg 39: 15–21. [DOI] [PubMed] [Google Scholar]
- 38. Yin N, Ma L, Zhang Z (2005) Bone regeneration in the hard palate after cleft palate surgery. Plast Reconstr Surg 115: 1239–1244. [DOI] [PubMed] [Google Scholar]
- 39. Chowdhury SKR, Menon PS, Vasant MR, Jayan B, Dhiman RK, et al. (2006) Secondary and delayed bone grafting in alveolar and anterior palatal clefts. Med J Armed Forces India 62: 231–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Feichtinger M, Mossbock R, Karcher H (2006) Evaluation of bone volume following bone grafting in patients with unilateral clefts of lip, alveolus and palate using a CT-guided three-dimensional navigation system. J Craniomaxillofac Surg 34: 144–149. [DOI] [PubMed] [Google Scholar]
- 41. Schliephake H, Donnerstag F, Berten JL, Lonquist N (2006) Palate morphology after unilateral and bilateral cleft lip and palate closure. Int J Oral Maxillofac Surg 35: 25–30. [DOI] [PubMed] [Google Scholar]
- 42. Feichtinger M, Mossbock R, Karcher H (2007) Assessment of bone resorption after secondary alveolar grafting using three-dimensional computed tomography: A three-year study. Cleft Palate Craniofac J 44: 142–148. [DOI] [PubMed] [Google Scholar]
- 43. Herford AS, Boyne PJ, Rawson R, Williams RP (2007) Bone morphogenetic protein-induced repair of the premaxillary cleft. J Oral Maxillofac Surg 65: 2136–2141. [DOI] [PubMed] [Google Scholar]
- 44. Ozawa T, Omura S, Fukuyama E, Matsui Y, Torikai K, et al. (2007) Factors influencing secondary alveolar bone grafting in cleft lip and palate patients: prospective analysis using CT image analyzer. Cleft Palate Craniofac J 44: 286–291. [DOI] [PubMed] [Google Scholar]
- 45. Feichtinger M, Zemann W, Mossbock R, Karcher H (2008) Three-dimensional evaluation of secondary alveolar bone grafting using a 3D- navigation system based on computed tomography: a two-year follow-up. Br J Oral Maxillofac Surg 46: 278–282. [DOI] [PubMed] [Google Scholar]
- 46. Kim KR, Kim S, Baek SH (2008) Change in grafted secondary alveolar bone in patients with UCLP and UCLA. Angle Orthod 78: 631–640. [DOI] [PubMed] [Google Scholar]
- 47. Nagasao T, Miyamoto J, Yasuda S, Ogata H, Imanishi Y, et al. (2008) An anatomical study of the three-dimensional structure of the nasal septum in patients with alveolar clefts and alveolar-palatal clefts. Plast Reconstr Surg 121: 2074–2083. [DOI] [PubMed] [Google Scholar]
- 48. Suri S, Utreja A, Khandelwal N, Mago SK (2008) Craniofacial Computerized Tomography Analysis of the midface of patients with repaired complete unilateral cleft lip and palate. Am J Orthod Dentofac Orthop 134: 418–429. [DOI] [PubMed] [Google Scholar]
- 49. Nagasao T, Miyamoto J, Konno E, Ogata H, Nakajima T, et al. (2009) Dynamic analysis of the effects of upper lip pressure on the asymmetry of the facial skeleton in patients with unilateral complete cleft lip and palate. Cleft Palate Craniofac J 46: 154–160. [DOI] [PubMed] [Google Scholar]
- 50. Nagasao T, Ogata H, Miyamoto J, Jiang H, Kaneko T, et al. (2009) Alveolar bone grafting for patients with unilateral complete alveolar and palatal clefts improves the bony structure of the nose. Cleft Palate Craniofac J 46: 9–18. [DOI] [PubMed] [Google Scholar]
- 51. Alonso N, Tanikawa DY, Freitas RS, Canan L Jr, Ozawa TO, et al. (2010) Evaluation of maxillary alveolar reconstruction using a resorbable collagen sponge with recombinant human bone morphogenetic protein-2 in cleft lip and palate patients. Tissue engineering Part C, Methods 16: 1183–1189. [DOI] [PubMed] [Google Scholar]
- 52. Mikoya T, Inoue N, Matsuzawa Y, Totsuka Y, Kajii TS, et al. (2010) Monocortical mandibular bone grafting for reconstruction of alveolar cleft. Cleft Palate Craniofac J 47: 454–46. [DOI] [PubMed] [Google Scholar]
- 53. Saijo H, Mori Y, Fujihara H, Kanno Y, Chikazu D, et al. (2010) Evaluation and analysis of formation of bone at the palate in patients with cleft lip and palate after palatoplasty based on computed tomograms and three-dimensional data. Scand J Plast Reconstr Surg Hand Surg 44: 21–25.8. [DOI] [PubMed] [Google Scholar]
- 54. Ye B, Ruan C, Hu J, Yang Y, Ghosh A, et al. (2010) A comparative study on dental-arch morphology in adult unoperated and operated cleft palate patients. J Craniofac Surg 21: 811–815. [DOI] [PubMed] [Google Scholar]
- 55. Chen PKT, Por YC, Liou EJW, Chang FCS (2011) Maxillary distraction osteogenesis in the adolescent cleft patient: Three-dimensional computed tomography analysis of linear and volumetric changes over five years. Cleft Palate Craniofac J 48: 445–454. [DOI] [PubMed] [Google Scholar]
- 56. Lee SH, Lee SH, Mori Y, Minami K, Park HS, et al. (2011) Evaluation of pterygomaxillary anatomy using computed tomography: are there any structural variations in cleft patients? J Oral Maxillofac Surg 69: 2644–2649. [DOI] [PubMed] [Google Scholar]
- 57. Li H, Yang Y, Chen Y, Wu Y, Zhang Y, et al. (2011) Three-dimensional reconstruction of maxillae using spiral computed tomography and its application in postoperative adult patients with unilateral complete cleft lip and palate. J Oral Maxillofac Surg 69: e549–e557. [DOI] [PubMed] [Google Scholar]
- 58. Tulunoglu O, Esenlik E, Gulsen A, Tulunoglu I (2011) A comparison of three-dimensional and two-dimensional cephalometric evaluations of children with cleft lip and palate. Eur J Dent 5: 451–458. [PMC free article] [PubMed] [Google Scholar]
- 59. Agarwal R, Parihar A, Mandhani PA, Chandra R (2012) Three-Dimensional Computed Tomographic Analysis of the Maxilla in Unilateral Cleft Lip and Palate: Implications for Rhinoplasty. J Craniofac Surg 23: 1338–42. [DOI] [PubMed] [Google Scholar]
- 60. Aras I, Olmez S, Dogan S (2012) Comparative Evaluation Of Nasopharyngeal Airways Of Unilateral Cleft Lip And Palate Patients using 3 Dimensional And 2 Dimensional Methods. Cleft Palate Craniofac J 49: e75–81. [DOI] [PubMed] [Google Scholar]
- 61. Choi J, Kwon GY, Kim S, Choi TH (2012) The long-term changes of hard palatal bony cleft defects after palatoplasty in unilateral complete cleft lip and palate. J Plast Reconstr Aesthet Surg 65: 1461–7. [DOI] [PubMed] [Google Scholar]
- 62. Hegab AF (2012) Closure of the alveolar cleft by bone segment transport using an intraoral tooth-borne custom-made distraction device. J Oral Maxillofac Surg 70: e337–348. [DOI] [PubMed] [Google Scholar]
- 63. Rychlik D, Wojcicki P (2012) Bone graft healing in alveolar osteoplasty in patients with unilateral lip, alveolar process, and palate clefts. J Craniof Surg 23: 118–123. [DOI] [PubMed] [Google Scholar]
- 64. Seike T, Hashimoto I, Matsumoto K, Tanaka E, Nakanishi H (2012) Early postoperative evaluation of secondary bone grafting into the alveolar cleft and its effects on subsequent orthodontic treatment. J Med Invest 59: 152–165. [DOI] [PubMed] [Google Scholar]
- 65. Wu Y, Yang Y, Chen Y, Zhang Y, Wang GM (2013) Measurement and Evaluation of Alar Base in Unilateral Secondary Lip Nasal Deformities by Three-dimensional Computed Tomography. Cleft Palate Craniofac J 50: 696–703. [DOI] [PubMed] [Google Scholar]
- 66. Ye B, Ruan C, Hu J, Yang Y, Thomas J, et al. (2012) A comparative study on the measurements of palatal shelf area and gradient for adult patients with unoperated cleft palate. Cleft Palate Craniofac J 49: 561–5. [DOI] [PubMed] [Google Scholar]
- 67. Yoshida S, Suga K, Nakano Y, Sakamoto T, Takaki T, et al. (2013) Postoperative Evaluation of Grafted Bone in Alveolar Cleft Using Three-Dimensional Computed Data.". Cleft Palate Craniofac J 50: 671–7. [DOI] [PubMed] [Google Scholar]
- 68. Zhang Y, Yang YS, Wu YL, Liang Y, Wang GM (2012) Measurement of the volume absorption of alveolar bone grafting. Shanghai Kou Qiang Yi Xue 21: 308–311. [PubMed] [Google Scholar]
- 69. Yin N, Ma L, Yang B (2001) The bone regeneration in cleft palate after surgical repair (a prelimilnary observation). Chin J Stomatol 36: 133–135. [PubMed] [Google Scholar]
- 70. Hamada Y, Kondoh T, Noguchi K, Iino M, Isono H, et al. (2005) Application of limited cone beam computed tomography to clinical assessment of alveolar bone grafting: A preliminary report. Cleft Palate Craniofac J 42: 128–137. [DOI] [PubMed] [Google Scholar]
- 71. Korbmacher H, Kahl-Nieke B, Schöllchen M, Heiland M (2007) Value of two cone-beam computed tomography systems from an orthodontic point of view. J Orofac Orthop 68: 278–89. [DOI] [PubMed] [Google Scholar]
- 72. Miyamoto J, Nagasao T, Nakajima T, Ogata H (2007) Cone beam computed evaluation of cleft lip bony depression of piriform margin and nasal deformity with tomography: "Retruded-like" appearance and anteroposterior position of the Alar base. Plast Reconstr Surg 120: 1612–1620. [DOI] [PubMed] [Google Scholar]
- 73. Dickinson BP, Ashley RK, Wasson KL, O'Hara C, Gabbay J, et al. (2008) Reduced morbidity and improved healing with bone morphogenic protein-2 in older patients with alveolar cleft defects. Plast Reconstr Surg 121: 209–217. [DOI] [PubMed] [Google Scholar]
- 74. Nagasao T, Miyamoto J, Hikosaka M, Yoshikawa K, Ishii N, et al. (2008) A new method to quantify subtle morphological deformities in nasal profile curvatures and its application for analysis of unilateral cleft lip noses. J Craniomaxillofac Surg 36: 321–334. [DOI] [PubMed] [Google Scholar]
- 75. Oberoi S, Chigurupati R, Gill P, Hoffman WY, Vargervik K (2009) Volumetric assessment of secondary alveolar bone grafting using cone beam computed tomography. Cleft Palate Craniofac J 46: 503–511. [DOI] [PubMed] [Google Scholar]
- 76. Miyamoto J, Nakajima T (2010) Anthropometric evaluation of complete unilateral cleft lip nose with cone beam CT in early childhood. J Plast Reconstr Aesthet Surg 63: 9–14. [DOI] [PubMed] [Google Scholar]
- 77. Oberoi S, Gill P, Chigurupati R, Hoffman WY, Hatcher DC, et al. (2010) Three-dimensional assessment of the eruption path of the canine in individuals with bone-grafted alveolar clefts using cone beam computed tomography. Cleft Palate Craniofac J 47: 507–512. [DOI] [PubMed] [Google Scholar]
- 78. Shirota T, Kurabayashi H, Ogura H, Seki K, Maki K, et al. (2010) Analysis of bone volume using computer simulation system for secondary bone graft in alveolar cleft. Int J Oral Maxillofac Surg 39: 904–908. [DOI] [PubMed] [Google Scholar]
- 79.Li F, Wang JG (2011) Measurement of tooth length of upper canines in complete unilateral cleft lip and palate patients with cone-beam computed tomography. Hua Xi Kou Qiang Yi Xue Za Zhi 29: 161–163, 167. [PubMed]
- 80. Contreras V, Carrasco-Labra A, Andrews N, Brignardello-Petersen R, Pantoja R (2011) Morphological study of the inferior meatus in three planes in patients with operated unilateral clefts. J Maxilo 33: 105–108. [Google Scholar]
- 81. Veli I, Uysal T, Ucar FI, Eruz M, Ozer T (2011) Cone-beam computed tomography assessment of mandibular asymmetry in unilateral cleft lip and palate patients. Korean J Orthod 41: 431–439. [Google Scholar]
- 82. Cheung T, Oberoi S (2012) Three dimensional assessment of the pharyngeal airway in individuals with non-syndromic cleft lip and palate. PLoS ONE 7: e43405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Garib DG, Yatabe MS, Ozawa TO, da Silva Filho OG (2012) Alveolar bone morphology in patients with bilateral complete cleft lip and palate in the mixed dentition: cone beam computed tomography evaluation. Cleft Palate Craniofac J 49: 208–14. [DOI] [PubMed] [Google Scholar]
- 84. Leenarts CMR, Bartzela TN, Bronkhorst EM, Semb G, Shaw WC, et al. (2012) Photographs of dental casts or digital models: Rating dental arch relationships in bilateral cleft lip and palate. Int J Oral Maxillofac Surg 41: 180–185. [DOI] [PubMed] [Google Scholar]
- 85. Li JT, Shi B, Liu K, Zheng Q (2012) A preliminary study on the hard-soft tissue relationships among unoperated secondary unilateral cleft nose deformities. Oral Surg Oral Med Oral Pathol Oral Radiol 113: 300–307. [DOI] [PubMed] [Google Scholar]
- 86. Miyamoto J, Miyamoto S, Nagasao T, Nakajima T, Kishi K (2012) Anthropometric evaluation of bilateral cleft lip nose with cone beam computed tomography in early childhood: Estimation of nasal tip collapse. J Plast Reconstr Aesthet Surg 65: 169–74. [DOI] [PubMed] [Google Scholar]
- 87. Padricelli G, Monsurro A, Grassia V, Perillo L (2012) The frequency of dental anomalies in subjects with cleft lip and palate. Mondo Ortodontico 37: 46–55. [Google Scholar]
- 88. Quereshy FA, Barnum G, Demko C, Horan M, Palomo JM, et al. (2012) Use of cone beam computed tomography to volumetrically assess alveolar cleft defects-preliminary results. J Oral Maxillofac Surg 70: 188–191. [DOI] [PubMed] [Google Scholar]
- 89. Trindade-Suedam IK, da Silva Filho OG, Carvalho RM, de Souza Faco RA, Calvo AM, et al. (2012) Timing of alveolar bone grafting determines different outcomes in patients with unilateral cleft palate. J Craniofac Surg 23: 1283–1286. [DOI] [PubMed] [Google Scholar]
- 90.Yoshihara M, Terajima M, Yanagita N, Hyakutake H, Kanomi R, et al.. (2012) Three-dimensional analysis of the pharyngeal airway morphology in growing Japanese girls with and without cleft lip and palate. Am J Orthod Dentofac Orthop 141(4 SUPPL): S92–S101. [DOI] [PubMed]
- 91. Zhou W, Li W, Lin J, Liu D, Xie X, et al. (2013) Tooth Lengths of the Permanent Upper Incisors in Patients with Cleft Lip and Palate Determined with Cone Beam Computed Tomography. Cleft Palate Craniofac J 50: 88–95. [DOI] [PubMed] [Google Scholar]
- 92. Yamawaki Y, Nishiniura Y, Suzuki Y (1999) Eustachian tube cartilage and medial movement of lateral pharyngeal wall on phonation. Plast Reconstr Surg 104: 350–356. [DOI] [PubMed] [Google Scholar]
- 93. Ozgur F, Tuncbilek G, Cila A (2000) Evaluation of velopharyngeal insufficiency with magnetic resonance imaging and nasoendoscopy. Ann Plast Surg 44: 8–13. [DOI] [PubMed] [Google Scholar]
- 94. Vadodaria S, Goodacre TE, Anslow P (2000) Does MRI contribute to the investigation of palatal function? Br J Plast Surg 53: 191–199. [DOI] [PubMed] [Google Scholar]
- 95. Sehhati-Chafai-Leuwer S, Wenzel S, Bschorer R, Seedorf H, Kucinski T, et al. (2006) Pathophysiology of the Eustachian tube - relevant new aspects for the head and neck surgeon. J Craniomaxillofac Surg. 34: 351–4. [DOI] [PubMed] [Google Scholar]
- 96. Atik B, Bekerecioglu M, Tan O, Etlik O, Davran R, et al. (2008) Evaluation of dynamic magnetic resonance imaging in assessing velopharyngeal insufficiency during phonation. J Craniofac Surg 19: 566–572. [DOI] [PubMed] [Google Scholar]
- 97. Tian W, Yin H, Li Y, Zhao S, Zheng Q, Shi B (2010) Magnetic resonance imaging assessment of velopharyngeal structures in Chinese children after primary palatal repair. J Craniofac Surg 21: 568–77. [DOI] [PubMed] [Google Scholar]
- 98. Tian W, Li Y, Yin H, Zhao SF, Li S, et al. (2010) Magnetic resonance imaging assessment of velopharyngeal motion in Chinese children after primary palatal repair. J Craniofac Surg 21: 578–587. [DOI] [PubMed] [Google Scholar]
- 99. Ras F, Habets LLMH, Van Ginkel FC, Prahl-Andersen B (1994) Facial left-right dominance in cleft lip and palate: Three-dimension evaluation. Cleft Palate Craniofac J 31: 461–465. [DOI] [PubMed] [Google Scholar]
- 100. Ras F, Habets LLMH, Van Ginkel FC, Prahl-Andersen B (1994) Three-dimensional evaluation of facial asymmetry in cleft lip and palate. Cleft Palate Craniofac J 31: 116–121. [DOI] [PubMed] [Google Scholar]
- 101. Ras F, Habets LL, van Ginkel FC, Prahl-Andersen B (1995) Method for quantifying facial asymmetry in three dimensions using stereophotogrammetry. Angle Orthod 65: 233–9. [DOI] [PubMed] [Google Scholar]
- 102. Ras F, Habets LLMH, Van Ginkel FC, Prahl-Andersen B (1995) Longitudinal study on three-dimensional changes of facial asymmetry in children between 4 to 12 years of age with unilateral cleft lip and palate. Cleft Palate Craniofac J 32: 463–468. [DOI] [PubMed] [Google Scholar]
- 103. Al-Omari I, Millett DT, Ayoub A, Bock M, Ray A, et al. (2003) An appraisal of three methods of rating facial deformity in patients with repaired complete unilateral cleft lip and palate. Cleft Palate Craniofac J 40: 530–537. [DOI] [PubMed] [Google Scholar]
- 104.Proff P, Weingartner J, Rottner K, Bayerlein T, Schoebel S, et al.. (2006) Functional 3-D analysis of patients with unilateral cleft of lip, alveolus and palate (UCLAP) following lip repair. J Cranio Maxillofac Surg (SUPPL. 2): 26–30. [DOI] [PubMed]
- 105. Devlin MF, Ray A, Raine P, Bowman A, Ayoub AF (2007) Facial symmetry in unilateral cleft lip and palate following alar base augmentation with bone graft: a three-dimensional assessment. Cleft Palate Craniofac J 44: 391–395. [DOI] [PubMed] [Google Scholar]
- 106. Grewal NS, Kawamoto HK, Kumar AR, Correa B, Desrosiers AE 3rd, et al. (2009) Correction of secondary cleft lip deformity: the whistle flap procedure. Plast Reconstr Surg 124: 1590–1598. [DOI] [PubMed] [Google Scholar]
- 107. Bugaighis I, O'Higgins P, Tiddeman B, Mattick C, Ben Ali O, et al. (2010) Three-dimensional geometric morphometrics applied to the study of children with cleft lip and/or palate from the North East of England. Eur J Orthod 32: 514–521. [DOI] [PubMed] [Google Scholar]
- 108. Hoefert CS, Bacher M, Herberts T, Krimmel M, Reinert S, et al. (2010) 3D soft tissue changes in facial morphology in patients with cleft lip and palate and class III mal occlusion under therapy with rapid maxillary expansion and delaire facemask. J Orofac Orthop 71: 136–151. [DOI] [PubMed] [Google Scholar]
- 109. Hoefert CS, Bacher M, Herberts T, Krimmel M, Reinert S, et al. (2010) Implementing a superimposition and measurement model for 3D sagittal analysis of therapy-induced changes in facial soft tissue: a pilot study. J Orofac Orthop 71: 221–234. [DOI] [PubMed] [Google Scholar]
- 110. Tanikawa C, Takada K, van Aalst J, Trotman CA (2010) Objective three-dimensional assessment of lip form in patients with repaired cleft lip. Cleft Palate Craniofac J 47: 611–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. van Loon B, Maal TJ, Plooij JM, Ingels KJ, Borstlap WA, et al. (2010) 3D Stereophotogrammetric assessment of pre- and postoperative volumetric changes in the cleft lip and palate nose. Int J Oral Maxillofac Surg 39: 534–540. [DOI] [PubMed] [Google Scholar]
- 112. Ayoub A, Bell A, Simmons D, Bowman A, Brown D, et al. (2011) 3D Assessment of Lip Scarring and Residual Dysmorphology Following Surgical Repair of Cleft Lip and Palate: A Preliminary Study. Cleft Palate Craniofac J 48: 379–387. [DOI] [PubMed] [Google Scholar]
- 113. Clark SL, Teichgraeber JF, Fleshman RG, Shaw JD, Chavarria C, et al. (2011) "Long-term treatment outcome of presurgical nasoalveolar molding in patients with unilateral cleft lip and palate.". J Craniofac Surg 22: 333–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Kau CH, Medina L, English JD, Xia J, Gateno J, et al. (2011) A comparison between landmark and surface shape measurements in a sample of cleft lip and palate patients after secondary alveolar bone grafting. Orthodontics (Chic.) 12: 188–195. [PMC free article] [PubMed] [Google Scholar]
- 115. Krimmel M, Schuck N, Bacher M, Reinert S (2011) Facial surface changes after cleft alveolar bone grafting. J Oral Maxillofac Surg 69: 80–83. [DOI] [PubMed] [Google Scholar]
- 116. Sander M, Daskalogiannakis J, Tompson B, Forrest C (2011) Effect of alveolar bone grafting on nasal morphology, symmetry, and nostril shape of patients with unilateral cleft lip and palate. Cleft Palate Craniofac J 48: 20–27. [DOI] [PubMed] [Google Scholar]
- 117. Oh TS, Choi JW, Koh KS (2011) Upper lip asymmetry perception using three-dimensional anthropometry in patients with unilateral cleft lip deformity. J Craniofac Surg 22: 2080–2083. [DOI] [PubMed] [Google Scholar]
- 118. Zreaqat M, Hassan R, Halim AS (2012) Facial dimensions of Malay children with repaired unilateral cleft lip and palate: A three dimensional analysis. Int J Oral Maxillofac Surg 41: 783–788. [DOI] [PubMed] [Google Scholar]
- 119. Millar K, Bell A, Bowman A, Brown D, Lo TW, et al. (2013) Psychological status as a function of residual scarring and facial asymmetry after surgical repair of cleft lip and palate. Cleft Palate Craniofac J 50(2): 150–7. [DOI] [PubMed] [Google Scholar]
- 120. Stewart A, McCance AM, James DR, Moss JP (1996) Three-dimensional nasal changes following maxillary advancement in cleft patients. Int J Oral Maxillofac Surg 25: 171–177. [DOI] [PubMed] [Google Scholar]
- 121. McCance AM, Moss JP, Fright WR, Linney AD, James DR (1997) Three-dimensional analysis techniques - Part 1: Three-dimensional soft- tissue analysis of 24 adult cleft palate patients following Le Fort I maxillary advancement: A preliminary report. Cleft Palate Craniofac J 34: 36–45. [DOI] [PubMed] [Google Scholar]
- 122. Bennun RD, Perandones C, Sepliarsky VA, Chantiri SN, Ines Ulfe Aguirre M, et al. (1999) Nonsurgical correction of nasal deformity in unilateral complete cleft lip: A 6-year follow-up. Plast Reconstr Surg 104: 616–630. [DOI] [PubMed] [Google Scholar]
- 123. Duffy S, Noar JH, Evans RD, Sanders R (2000) Three-dimensional analysis of the child cleft face. Cleft Palate Craniofac J 37: 137–144. [DOI] [PubMed] [Google Scholar]
- 124. Honda Y, Suzuki A, Nakamura N, Ohishi M (2002) Relationship between primary palatal form and maxillofacial growth in Japanese children with unilateral cleft lip and palate: infancy to adolescence. Cleft Palate Craniofac J 39: 527–534. [DOI] [PubMed] [Google Scholar]
- 125. Mori A, Nakajima T, Kaneko T, Sakuma H, Aoki Y (2005) Analysis of 109 Japanese children's lip and nose shapes using 3-dimensional digitizer. Brit J Plast Surg 58: 318–329. [DOI] [PubMed] [Google Scholar]
- 126. Nakamura N, Suzuki A, Takahashi H, Honda Y, Sasaguri M, et al. (2005) A longitudinal study on influence of primary facial deformities on maxillofacial growth in patients with cleft lip and palate. Cleft Palate Craniofac J 42: 633–640. [DOI] [PubMed] [Google Scholar]
- 127. Schwenzer-Zimmerer K, Chaitidis D, Berg-Boerner I, Krol Z, Kovacs L, et al. (2008) Quantitative 3D soft tissue analysis of symmetry prior to and after unilateral cleft lip repair compared with non-cleft persons (performed in Cambodia). J Craniomaxillofac Surg 36: 431–438. [DOI] [PubMed] [Google Scholar]
- 128. Schwenzer-Zimmerer K, Chaitidis D, Boerner I, Kovacs L, Schwenzer NF, et al. (2008) Systematic contact-free 3D topometry of the soft tissue profile in cleft lips. Cleft Palate Craniofac J 45: 607–613. [DOI] [PubMed] [Google Scholar]
- 129. Meyer-Marcotty P, Stellzig-Eisenhauer A (2009) Dentofacial self-perception and social perception of adults with unilateral cleft lip and palate. J Orofac Orthop 70: 224–236. [DOI] [PubMed] [Google Scholar]
- 130. Smahel Z, Veleminska J, Trefny P, Mullerova Z (2009) Three-dimensional morphology of the palate in patients with bilateral complete cleft lip and palate at the stage of permanent dentition. Cleft Palate Craniofac J 46: 399–408. [DOI] [PubMed] [Google Scholar]
- 131.Meyer-Marcotty P, Alpers GW, Gerdes AB, Stellzig-Eisenhauer A (2010) Impact of facial asymmetry in visual perception: a 3-dimensional data analysis. Am J Orthod Dentofacial Orthop 137: 168 e161–168. [DOI] [PubMed]
- 132. Nakamura N, Okawachi T, Nishihara K, Hirahara N, Nozoe E (2010) Surgical technique for secondary correction of unilateral cleft lip-nose deformity: clinical and 3-dimensional observations of preoperative and postoperative nasal forms. J Oral Maxillofac Surg 68: 2248–2257. [DOI] [PubMed] [Google Scholar]
- 133.Vasiliauskas A, Sidlauskas A, Saferis V, Adaskevicius R, Linkeviciene L (2010) Applications of 3D Maxillary Dental Arch Scanning for Mathematical Prediction of Orthodontic Treatment need for Complete Unilateral Cleft Lip and Palate Patients. Elektronika Ir Elektrotechnika: 107–112.
- 134. Wojtaszek-Slominska A, Renkielska A, Dobke M, Gosman A, Slominski W (2010) Orthodontic characteristics of maxillary arch deficiency in 5-year-old patients undergoing unilateral cleft lip and palate repair with and without early gingivoplasty. J Craniomaxillofac Surg 38: 155–159. [DOI] [PubMed] [Google Scholar]
- 135. Meyer-Marcotty P, Kochel J, Boehm H, Linz C, Klammert U, et al. (2011) Face perception in patients with unilateral cleft lip and palate and patients with severe Class III malocclusion compared to controls. J Craniomaxillofacial Surg 39: 158–163. [DOI] [PubMed] [Google Scholar]
- 136. Nakamura N, Okawachi T, Nozoe E, Nishihara K, Matsunaga K (2011) Three-dimensional analyses of nasal forms after secondary treatment of bilateral cleft lipnose deformity in comparison to those of healthy young adults. J Oral Maxillofacial S 69: e469–e481. [DOI] [PubMed] [Google Scholar]
- 137. Nakamura N, Sasaguri M, Okawachi T, Nishihara K, Nozoe E (2011) Secondary correction of bilateral cleft lip nose deformity - Clinical and three-dimensional observations on pre- and postoperative outcome. J Craniomaxillofac Surg 39: 305–312. [DOI] [PubMed] [Google Scholar]
- 138. Okawachi T, Nozoe E, Nishihara K, Nakamura N (2011) 3-dimensional analyses of outcomes following secondary treatment of unilateral cleft lip nose deformity. J Oral Maxillofac Surg 69: 322–332. [DOI] [PubMed] [Google Scholar]
- 139. Bejdová S, Krajíček V, Peterka M, Trefný P, Velemínská J (2012) Variability in palatal shape and size in patients with bilateral complete cleft lip and palate assessed using dense surface model construction and 3D geometric morphometrics. J Craniomaxillofac Surg 40: 201–8. [DOI] [PubMed] [Google Scholar]
- 140. Dogan S, Olmez S, Semb G (2012) Comparative assessment of dental arch relationships using goslon yardstick in patients with unilateral complete cleft lip and palate using dental casts, two-dimensional photos, and three-dimensional images. Cleft Palate Craniofac J. 49: 347–51. [DOI] [PubMed] [Google Scholar]
- 141. Chawla O, Atack NE, Deacon S, Leary SD, Ireland AJ, et al. (2013) Three-dimensional digital models for rating dental arch relationships in unilateral cleft lip and palate. Cleft Palate Craniofac J 50: 182–6. [DOI] [PubMed] [Google Scholar]
- 142. Kilpelainen PV, Laine-Alava MT (1996) Palatal asymmetry in cleft palate subjects. Cleft Palate Craniofac J 33: 483–488. [DOI] [PubMed] [Google Scholar]
- 143. Kilpelainen PV, Laine-Alava MT, Lammi S (1996) Palatal morphology and type of clefting. Cleft Palate Craniofac J 33: 477–482. [DOI] [PubMed] [Google Scholar]
- 144. Maull DJ, Grayson BH, Cutting CB, Brecht LL, Bookstein FL, et al. (1999) Long-term effects of nasoalveolar molding on three-dimensional nasal shape in unilateral clefts. Cleft Palate Craniofac J 36: 391–397. [DOI] [PubMed] [Google Scholar]
- 145. Kratzsch H, Opitz C (2000) Investigations on the palatal rugae pattern in cleft patients. Part II: Changes in the distances from the palatal rugae to maxillary points. J Orofac Orthop 61: 421–431. [DOI] [PubMed] [Google Scholar]
- 146. Kratzsch H, Opitz C (2000) Investigations on the palatal rugae pattern in cleft patients. Part I: A morphological analysis. J Orofac Orthop 61: 305–317. [DOI] [PubMed] [Google Scholar]
- 147. Trotman CA, Faraway JJ, Essick GK (2000) Three-dimensional nasolabial displacement during movement in repaired cleft lip and palate patients. Plast Reconstr Surg 105: 1273–1283. [DOI] [PubMed] [Google Scholar]
- 148. Russell KA, Waldman SD, Tompson B, Lee JM (2001) Nasal morphology and shape parameters as predictors of nasal esthetics in individuals with complete unilateral cleft lip and palate. Cleft Palate Craniofac J 38: 476–485. [DOI] [PubMed] [Google Scholar]
- 149. Ferrario VF, Sforza C, Dellavia C, Tartaglia GM, Colombo A, et al. (2003) A quantitative three-dimensional assessment of soft tissue facial asymmetry of cleft lip and palate adult patients. J Craniofac Surgery 14: 739–746. [DOI] [PubMed] [Google Scholar]
- 150. Ferrario VF, Sforza C, Dellavia C, Tartaglia GM, Sozzi D, et al. (2003) A quantitative three-dimensional assessment of abnormal variations in facial soft tissues of adult patients with cleft lip and palate. Cleft Palate Craniofac J 40: 544–549. [DOI] [PubMed] [Google Scholar]
- 151. Ferrario VF, Sforza C, Dellavia C, Vizzotto L, Caru A (2003) Three-dimensional nasal morphology in cleft lip and palate operated adult patients. Ann Plast Surg 51: 390–397. [DOI] [PubMed] [Google Scholar]
- 152. Ferrario VF, Sforza C, Tartaglia GM, Sozzi D, Caru A (2003) Three-dimensional lip morphometry in adults operated on for cleft lip and palate. Plast Reconstr Surg 111: 2149–2156. [DOI] [PubMed] [Google Scholar]
- 153. Smahel Z, Trefny P, Formanek P, Mullerova Z, Peterka M (2003) Three-Dimensional Morphology of the Palate in Subjects with Isolated Cleft Palate at the Stage of Permanent Dentition. Cleft Palate Craniofac J 40: 577–584. [DOI] [PubMed] [Google Scholar]
- 154. Smahel Z, Trefny P, Formanek P, Mullerova Z, Peterka M (2004) Three-dimensional morphology of the palate in subjects with unilateral complete cleft lip and palate at the stage of permanent dentition. Cleft Palate Craniofac J 41: 416–423. [DOI] [PubMed] [Google Scholar]
- 155. Bilwatsch S, Kramer M, Haeusler G, Schuster M, Wurm J, et al. (2006) Nasolabial symmetry following Tennison-Randall lip repair: A three-dimensional approach in 10-year-old patients with unilateral clefts of lip, alveolus and palate. J Craniomaxillofac Surg 34: 253–262. [DOI] [PubMed] [Google Scholar]
- 156. Stauber I, Vairaktaris E, Holst A, Schuster M, Hirschfelder U, et al. (2008) Three-dimensional analysis of facial symmetry in cleft lip and palate patients using optical surface data. J Orofac Orthop 69: 268–282. [DOI] [PubMed] [Google Scholar]
- 157. Krey KF, Borngen J, Dannhauer KH (2009) Three-dimensional analysis of the deciduous dentition of patients with bilateral cleft lip and palate and delayed cleft closure. Journal of Orofacial Orthopedics 70: 237–246. [DOI] [PubMed] [Google Scholar]
- 158. Trotman CA, Faraway JJ, Phillips C, Van Aalst J (2010) Effects of lip revision surgery in cleft lip/palate patients. J Dent Res 89: 728–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Russell KA, Milne AD, Varma D, Josephson K, Lee JM (2011) Three-dimensional morphologic nasal surface characteristics that predict the extremes of esthetics in patients with repaired cleft lip and palate. Cleft Palate Craniofac J 48: 28–37. [DOI] [PubMed] [Google Scholar]
- 160.European Commission (2012) Radiation protection no 172. Cone beam CT for dental and maxillofacial radiology (evidence based guidelines). Available: http://www.sedentexct.eu/files/radiation_protection_172.pdf. Accessed 2014 Mar 16.
- 161. Lagravere MO, Major PW, Flores-Mir C (2005) Long-term skeletal changes with rapid maxillary expansion: a systematic review. Angle Orthod 75: 1046–1052. [DOI] [PubMed] [Google Scholar]
- 162. Sanderson S, Tatt ID, Higgins JP (2007) Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol 36: 666–676. [DOI] [PubMed] [Google Scholar]
- 163. Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses Eur J Epidemiol. 2010 25: 603–605. [DOI] [PubMed] [Google Scholar]
- 164. Clark HD, Wells GA, Huet C, McAlister FA, Salmi LR, et al. (1999) Assessing the quality of randomized trials: reliability of the Jadad scale. Control Clin Trials. 20: 448–452. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Methodological quality scores of CT studies.
(DOCX)
Methodological quality scores of CBCT studies.
(DOCX)
Methodological quality scores of MRI studies.
(DOCX)
Methodological quality scores of stereophotogrammetry studies.
(DOCX)
Methodological quality scores of laser surface scanning studies.
(DOCX)
Methodological quality scores of other studies.
(DOCX)
PRISMA checklist.
(DOCX)
Protocol for the systematic review as registered in PROSPERO (registration number: CRD42012002041).
(PDF)