The endocytosis regulator dynamin 2 is required for the regulation of S1PR1 internalization and continued S1PR1 signaling in low S1P environments.
Abstract
Sphingosine-1-phosphate (S1P) receptor 1 (S1PR1) is critical for lymphocyte egress from lymphoid organs. Lymphocytes encounter low S1P concentrations near exit sites before transmigration, yet S1PR1 signaling is rapidly terminated after exposure to S1P. How lymphocytes maintain S1PR1 signaling in a low S1P environment near egress sites is unknown. Here we identify dynamin 2, an essential component of endocytosis, as a novel regulator of T cell egress. Mice with T cell–specific dynamin 2 deficiency had profound lymphopenia and impaired egress from lymphoid organs. Dynamin 2 deficiency caused impaired egress through regulation of S1PR1 signaling, and transgenic S1PR1 overexpression rescued egress in dynamin 2 knockout mice. In low S1P concentrations, dynamin 2 was essential for S1PR1 internalization, which enabled continuous S1PR1 signaling and promoted egress from both thymus and lymph nodes. In contrast, dynamin 2–deficient cells were only capable of a pulse of S1PR1 signaling, which was insufficient for egress. Our results suggest a possible mechanism by which T lymphocytes positioned at exit portals sense low S1P concentrations, promoting their egress into circulatory fluids.
The egress of T lymphocytes from lymphoid organs is essential for adaptive immune responses. The exit of mature single-positive (SP) thymocytes from the thymus into blood establishes a pool of naive T cells with a diverse repertoire in peripheral organs. Egress from lymph nodes into lymph is required for the recirculation of T cells through secondary lymphoid organs and for immune surveillance. Egress from lymphoid organs is critically dependent on the binding of sphingosine-1-phosphate (S1P) to S1P receptor 1 (S1PR1) that is expressed on T cells (Matloubian et al., 2004; Pappu et al., 2007; Zachariah and Cyster, 2010; Cyster and Schwab, 2012). Sensing of S1P gradients that exist between lymphoid tissues (interstitial S1P concentration in low nanomolar range) and blood or lymph (plasma S1P concentration ∼100–1,000 nM) is required for egress (Schwab et al., 2005; Pappu et al., 2007; Cyster and Schwab, 2012). Beyond a requirement for S1PR1, the lymphocyte-intrinsic molecular mechanisms that regulate egress remain incompletely defined.
S1PR1 is a G protein–coupled receptor (GPCR) with unique properties (Lee et al., 1996, 1998; Windh et al., 1999; Rivera et al., 2008; Rosen et al., 2009; Spiegel and Milstien, 2011; Cyster and Schwab, 2012). It is highly sensitive to desensitization and internalization in the continued presence of its ligand S1P (Liu et al., 1999; Schwab et al., 2005; Oo et al., 2007, 2011; Pappu et al., 2007; Arnon et al., 2011), particularly when compared with chemokine receptors and even when compared with members of the same receptor family, such as S1PR5 (Jenne et al., 2009). Receptor desensitization is mediated by GPCR kinase 2 (GRK2), which phosphorylates serine residues in the cytoplasmic tail of S1PR1 (Watterson et al., 2002; Arnon et al., 2011). Receptor phosphorylation recruits β-arrestins that sterically uncouple the receptor from heterotrimeric G proteins, thereby leading to the rapid loss of receptor responsiveness (“desensitization”). Arrestin binding also leads to GPCR internalization via clathrin-mediated endocytosis and either receptor degradation or recycling back to the cell surface (Ferguson, 2001; Pierce et al., 2002; Sorkin and von Zastrow, 2009). Receptor internalization can restore GPCR responsiveness (“resensitization”) as has been shown for the β2-adrenergic receptor (Zhang et al., 1997).
Although large S1P gradients exist between blood/lymph and lymphoid tissue, several data indicate that lymphocytes encounter small S1P gradients that likely instruct migration toward exit portals within lymphoid tissues. For example, thymocytes are attracted to egress sites at corticomedullary junctions in response to S1P produced locally by pericytes that ensheath thymic blood vessels (Zachariah and Cyster, 2010). Furthermore, S1PR1 signaling enforces internalization of the surface molecule CD69 (Shiow et al., 2006; Bankovich et al., 2010; Cyster and Schwab, 2012), a molecular timer which delays egress (Zachariah and Cyster, 2010). A prediction from these observations is the presence of an intrathymic gradient of low S1P concentration that guides thymocytes to exit sites, although technical limitations have not yet allowed direct visualization of S1P gradients within tissue (Cyster and Schwab, 2012). Given the rapid and sensitive down-regulation of S1PR1 signaling upon S1P engagement, this prediction also implies that S1PR1, after exposure to intrathymic S1P, maintains S1P responsiveness to promote thymocyte egress. However, the molecular requirements for, and the functional significance of, S1PR1 resensitization for T cell egress have not been defined.
Intravital microscopy of S1PR1-deficient lymphocytes revealed that T cells approach lymph node egress sites (cortical lymphatic sinuses) efficiently, but S1PR1 is critical for the transendothelial migration step (Grigorova et al., 2009). The data on lymph node egress are consistent with a model in which a pulse of S1PR1 signaling, as opposed to sustained signaling, is sufficient for lymphocyte egress. Alternatively, egress requires sustained S1PR1 signaling, and therefore, lymphocytes need to maintain S1PR1 responsiveness even in the presence of low S1P concentrations. The latter mode of egress would predict that rapid S1PR1 resensitization mechanisms are essential for egress to occur.
Binding of S1P to S1PR1 triggers both signaling through the receptor and its endocytosis (Liu et al., 1999; Oo et al., 2007, 2011), yet whether and how endocytosis regulates S1PR1 signaling are unclear. Given the critical role for dynamins in promoting the membrane scission step during endocytosis (Praefcke and McMahon, 2004; McMahon and Boucrot, 2011; Schmid and Frolov, 2011; Ferguson and De Camilli, 2012), we used mice genetically deficient in dynamin 2 (Dnm2; Ferguson et al., 2009), the dynamin isoform expressed in immune cells, to investigate the physiological function of endocytosis in T lymphocytes. We report here that dynamin 2 is critical for T cell egress from thymus and lymph nodes by directly regulating S1PR1 signaling. Surprisingly, dynamin 2–dependent endocytosis was not required for termination of S1PR1 signaling. Instead, dynamin 2 was required for S1PR1 resensitization in T lymphocytes, thereby promoting sustained S1PR1 signaling in vivo. We propose that dynamin 2–dependent endocytosis enables continuous S1PR1 signaling in T lymphocytes that are positioned near exit sites in a low S1P environment and promotes their egress into blood and lymph. Overall, our findings identify a previously unknown mechanistic link between endocytosis and T lymphocyte egress.
RESULTS
T cell–specific dynamin 2 deficiency causes lymphopenia
To determine the physiological function of dynamin 2 in T cells, we generated Cd4-creDnm2flox/flox (referred to as “Dnm2 KO”) mice by crossing mice with conditional expression of dynamin 2 (Dnm2flox/flox) to Cd4-cre transgenic mice. Littermate Cd4-creDnm2flox/+ (referred to as “Dnm2 HET”) mice were used as controls. The floxed Dnm2 allele was deleted in T cells from the thymus and periphery of Dnm2 KO mice, and Dnm2 KO T cells lacked dynamin 2 protein (not depicted). In addition, we confirmed the absence of dynamin 1 and 3 in Dnm2 KO T cells by using a pan-dynamin antibody (Ab) that recognizes the three dynamin isoforms (not depicted; Ferguson et al., 2007).
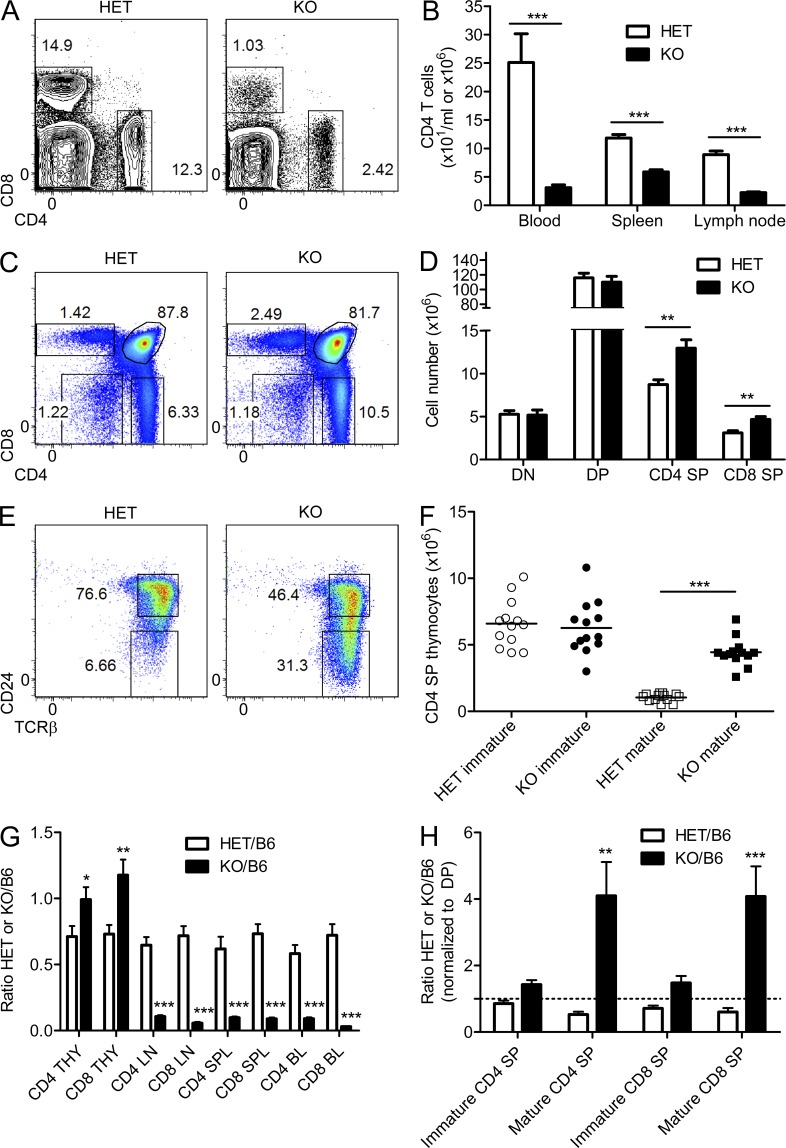
We found that Dnm2 KO mice had profound lymphopenia with a reduction of both CD4 and CD8 T cells in blood by a factor of ∼10 (Fig. 1, A and B). This was not caused by a defect in T cell development because developing thymocytes were present in Dnm2 HET and KO mice (Fig. 1, C and D). However, Dnm2 KO mice showed a significant increase in the number of CD4 and CD8 SP thymocytes (Fig. 1 D). Specifically, the frequency and number of CD4 SP and CD8 SP thymocytes with a mature phenotype (TCRβhiCD24lo) were increased by a factor of approximately four to five in Dnm2 KO mice (Fig. 1, E and F; and not depicted). We performed mixed bone marrow chimera experiments to address whether the observed defects were cell intrinsic or caused by an altered environment in Dnm2 KO mice. We reconstituted sublethally irradiated Rag1-deficient mice with a 1:1 mixture of Dnm2 HET or KO bone marrow cells (CD45.2+) and WT C57BL/6 (B6) cells (CD45.1+). Mixed Dnm2 KO/WT chimeras contained fewer peripheral T cells derived from Dnm2 KO cells than from WT bone marrow cells when compared with Dnm2 HET/WT chimeras (Fig. 1 G). In contrast, there were more mature SP thymocytes derived from Dnm2 KO bone marrow than from WT bone marrow in Dnm2 KO/WT chimeras (Fig. 1 H), indicating that the lymphopenia and the increase in mature SP thymocytes were cell-intrinsic defects. These data demonstrate that dynamin 2 is necessary for establishing a full T cell compartment in the periphery.
Figure 1.
T cell–specific dynamin 2 deficiency leads to lymphopenia and accumulation of mature thymocytes. (A and B) Flow cytometric analysis of blood CD4 and CD8 T cells (A) and numbers of CD4 T cells (B) in blood, spleen, and lymph node from Dnm2 HET and KO mice (n = 10). (C and D) Flow cytometric analysis (C) and numbers (D) of double-negative (DN), DP, and CD4 and CD8 SP thymocytes from Dnm2 HET and KO mice (n = 13). (E and F) Flow cytometric analysis (E) and numbers (F) of immature (TCRβhiCD24hi) and mature (TCRβhiCD24lo) CD4 SP thymocytes from Dnm2 HET and KO mice (n = 13). Horizontal bars indicate the mean. (G) Bone marrow cells from Dnm2 HET or KO mice (CD45.2+) were mixed 1:1 with WT B6 cells (CD45.1+) and injected into irradiated Rag1 KO recipients (CD45.1+) to generate bone marrow chimeras. Ratio of CD4 and CD8 T cells in thymus (THY), lymph nodes (LN), spleen (SPL), and blood (BL) from Dnm2 HET/B6 and Dnm2 KO/B6 mixed chimeras (n = 16–17) is shown. (H) Mixed bone marrow chimeras were generated as in G. Ratio of immature and mature CD4 and CD8 SP thymocytes from Dnm2 HET/B6 and Dnm2 KO/B6 mixed chimeras (n = 11–16) is shown. Ratios were normalized to the ratio of DP thymocytes to account for variable chimerism among mice. The dashed line indicates a control cell/KO cell ratio of 1. All error bars represent SEM. *, P < 0.05; **, P < 0.01; ***, P < 0.001 by unpaired Student’s t test (B, D, F, and G) or one-way ANOVA, Tukey’s post-test (H). Results are representative of or combined from three (D and F), four (G and H), or more than five (A–C and E) experiments.
Thymic egress is dependent on dynamin 2
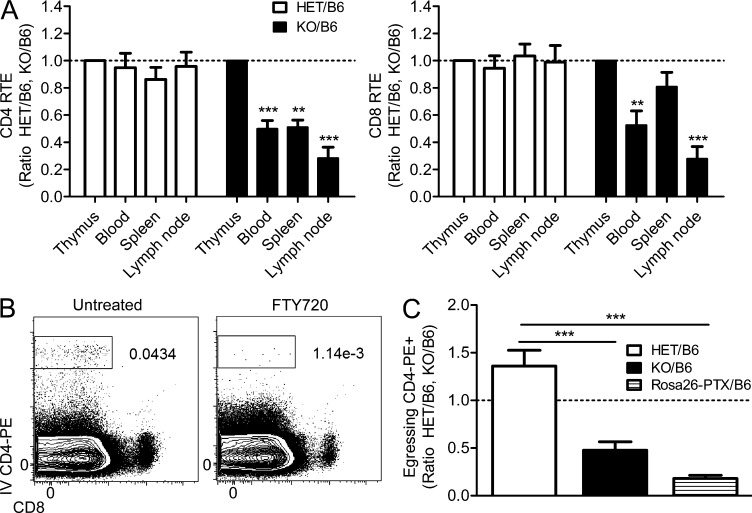
The observed accumulation of mature T cells in the thymus and corresponding reduction of T cells in the blood led us to ask whether T cell emigration from the thymus into blood requires dynamin 2. To test this possibility, we quantified recent thymic emigrants (RTEs) by intrathymic FITC dye injection (Carlson et al., 2006). Peripheral T cells that carry the label (FITC+) correspond to RTEs that can be identified by flow cytometry. These experiments were performed in mixed bone marrow chimeras to exclude any potential lymphopenia-related effects on thymic egress. Using this technique, we found that both CD4+ and CD8+ RTEs were reduced by ∼50% in the blood of Dnm2 KO mice (Fig. 2 A). The increase in mature T cells together with decreased RTEs suggests that thymocyte egress requires dynamin 2. To further test this hypothesis, we directly visualized egressing thymocytes by injecting mice with PE-conjugated α-CD4 Ab i.v. for 4 min, a procedure which selectively labels blood-exposed thymocytes (Pereira et al., 2009; Zachariah and Cyster, 2010). The specific labeling of egressing thymocytes (i.v. CD4-PE+) was confirmed by the reduction of i.v. CD4-PE+ cells in mice treated with the high-affinity S1P agonist FTY720 (Fig. 2 B), which blocks thymic egress by disrupting S1P gradients and by inducing S1PR1 degradation (Cyster and Schwab, 2012). Analysis of mixed bone marrow chimeras revealed a significant reduction of egressing thymocytes in the absence of dynamin 2 (Fig. 2 C), similar to that in mice with impaired Gαi signaling (Cd4-creRosa26PTX/+ mice, see below for description of mice). Together, our results establish that dynamin 2 is essential for T cell egress from the thymus.
Figure 2.
Dynamin 2 is required for T cell egress from thymus. (A) Mixed Dnm2 HET/B6 and Dnm2 KO/B6 bone marrow chimeras generated as in Fig. 1 G were injected intrathymically with 20 µg FITC to label CD4+ and CD8+ RTEs. RTEs were gated as CD4+ or CD8+FITC+ cells in blood, spleen, and lymph node 24 h after injection. Ratio of HET/B6 and KO/B6 FITC+ T cells in various tissues is shown (n = 11–12). Ratios in blood, spleen, and lymph nodes were normalized to the ratio in thymus (ratio = 1) to account for differences in labeling. (B and C) Mixed bone marrow chimeras generated as in Fig. 1 G were injected i.v. with 1 µg α–CD4-PE Ab. (B) Egressing WT CD4 SP thymocytes in circulation were gated as CD4-PE+ cells in untreated chimeras or chimeras injected with FTY720 (to inhibit egress) 16 h before analysis. (C) Ratio of egressing CD4 SP thymocytes (CD4-PE+) from Dnm2 HET/B6, Dnm2 KO/B6, and Cd4-creRosa26PTX/+ (Rosa26-PTX)/B6 mixed bone marrow chimeras (n = 9–16). (A and C) The dashed line indicates a control cell/KO cell ratio of 1. All error bars represent SEM. **, P < 0.01; ***, P < 0.001 by one-way ANOVA, Tukey’s post-test (C) or two-way ANOVA, Bonferroni post-test (A). Results are combined from two (A) or six (B and C) experiments.
Dynamin 2 regulates S1PR1 signaling in vivo
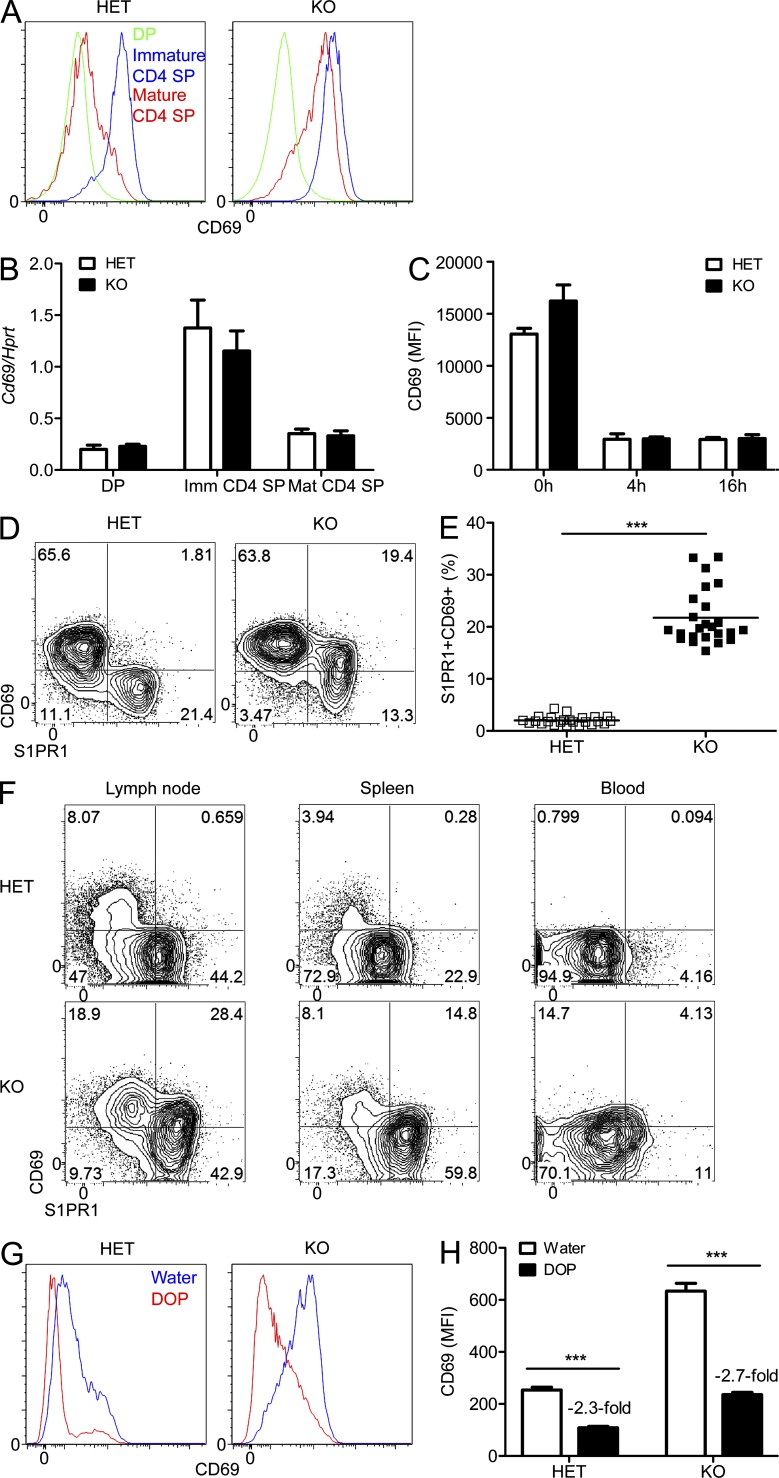
Lymphocyte egress from lymphoid organs is critically dependent on intrinsic S1PR1 signaling in response to S1P gradients (Cyster and Schwab, 2012). Thus, we asked whether dynamin 2 regulates T cell egress by modulating S1PR1 signaling in vivo. During their maturation, thymocytes become egress competent by expressing S1PR1 and down-modulating CD69 from the cell surface, the latter being dependent on S1PR1 signaling (Matloubian et al., 2004; Zachariah and Cyster, 2010; Bréart et al., 2011; Cyster and Schwab, 2012). We examined CD69 expression to determine whether S1PR1 signaling was functional in dynamin 2–deficient T cells. We found that CD69 surface expression was increased on mature CD4 SP thymocytes that lacked dynamin 2 (Fig. 3 A, compare red histograms). This increase also occurred in naive T cells in the periphery (not depicted). CD69 mRNA expression is augmented by TCR signaling and other activating stimuli (Shiow et al., 2006), but control and Dnm2 KO thymocytes expressed similar amounts of CD69 mRNA (Fig. 3 B), indicating that the increased CD69 surface expression in Dnm2 KO T cells is a posttranscriptional event and not secondary to increased TCR and/or inflammatory cytokine signaling. Finally, increased CD69 surface expression was also not caused by impaired endocytosis of CD69 because Ab-mediated CD69 internalization in vitro was normal in the absence of dynamin 2 (Fig. 3 C).
Figure 3.
Dynamin 2 regulates S1PR1 signaling in vivo. (A) CD69 surface expression on thymocytes from Dnm2 HET and KO mice (n > 10) was measured by flow cytometry. (B) Quantitative RT-PCR analysis of CD69 mRNA expression in thymocyte populations from Dnm2 HET and KO mice (n = 4). mRNA expression was normalized to Hprt. (C) Flow cytometric analysis of CD69 surface expression on immature CD4 SP thymocytes treated with α-CD69 Ab in vitro (n = 6). MFI, mean fluorescence intensity. (D and E) Flow cytometric analysis (D) and frequencies (E) of S1PR1-CD69 coexpressing CD4 SP thymocytes from Dnm2 HET and KO mice (n = 24). Horizontal bars indicate the mean. (F) Flow cytometric analysis of S1PR1 and CD69 surface expression on naive (CD44lo) CD4 T cells from Dnm2 HET and KO mice (n = 9). (G and H) Dnm2 HET and KO mice received 30 mg/liter DOP in the drinking water or water alone. 3 d later, CD69 surface expression on mature CD4 SP thymocytes (n = 7) was measured by flow cytometry. All error bars represent SEM. ***, P < 0.001 by unpaired Student’s t test. Results are representative of or combined from two (C, G, and H), three (F), four (B), or more than five (A, D, and E) experiments.
S1PR1 and CD69 can form a protein complex and antagonize each other by inducing down-regulation of the respective protein from the cell surface depending on their individual abundance (Shiow et al., 2006; Bankovich et al., 2010; Cyster and Schwab, 2012). Therefore, when S1P-S1PR1 signaling is intact, S1PR1 and CD69 show mutually exclusive expression on the cell surface of T cells (Fig. 3 D). In dynamin 2–deficient mice, however, we observed S1PR1-CD69 surface coexpression in a substantial fraction of SP thymocytes (Fig. 3, D and E). This phenomenon was cell autonomous (not depicted). It also occurred in peripheral T cells (Fig. 3 F), albeit to a lesser degree, inversely correlating with the reported S1P concentrations (lowest in thymus, low in lymph node, intermediate in spleen, and high in blood; Schwab et al., 2005; Pappu et al., 2007). Because we observed that S1PR1/CD69 coexpression in dynamin 2–deficient cells was most pronounced in thymus and lymph node (Fig. 3, D and F), where S1P concentrations are lower than in spleen and blood, we hypothesized that dynamin 2 promotes S1PR1 signaling when S1P is present at low concentrations. To test this hypothesis, we asked whether raising the S1P concentration in a low S1P environment (i.e., thymus) to the high S1P concentration found in blood would induce a similar amount of S1PR1 signaling in WT and Dnm2 KO cells. This was achieved by pharmacologically inhibiting S1P degradation with deoxypyridoxine (DOP; Schwab et al., 2005) and using CD69 surface down-modulation as a surrogate of S1PR1 signaling in vivo. We found that surface CD69 levels in WT and Dnm2 KO thymocytes decreased to a similar extent after DOP treatment (Fig. 3, G and H), suggesting that the S1PR1 response in a high S1P environment is the same in WT and KO cells. We conclude that dynamin 2 is particularly required for S1PR1-mediated CD69 down-modulation in microenvironments containing low S1P concentrations, such as thymus and lymph nodes.
Dynamin 2 is required for S1PR1 internalization at low S1P concentrations
We next wanted to define how dynamin 2 regulates S1PR1 signaling. Considering the physiological role played by dynamin proteins in endocytosis, we explored the possibility that S1PR1 signaling is regulated by dynamin 2–dependent S1PR1 internalization. S1PR1 internalization is induced by S1P binding, coupling of S1PR1 to G proteins, and phosphorylation of the intracellular C-terminal tail of S1PR1 by GRK2. In normal T cells, S1PR1 surface expression inversely correlates with the S1P concentration found in the different lymphoid tissues (Schwab et al., 2005; Pappu et al., 2007), i.e., surface S1PR1 is highest in thymus (where S1P is lowest), high in lymph nodes, intermediate in spleen, and undetectable in blood (Fig. 4 A). We observed that dynamin 2–deficient T cells in lymph nodes and spleen expressed more S1PR1 on the cell surface than control cells (Fig. 4 A). Mixed bone marrow chimera experiments revealed that this higher S1PR1 surface was cell intrinsic (Fig. 4 B), i.e., it was not caused by altered S1P concentration or gradients in the lymphoid organ interstitium of Dnm2 KO mice. Furthermore, it was also not caused by higher S1PR1 mRNA expression (not depicted). Expression of S1PR1 on Dnm2 KO thymocytes was only slightly increased (Fig. 4 A), likely because the amount of surface S1PR1 in thymocytes is already near its maximum as a consequence of the low S1P concentration in the thymus. This notion is supported by the finding that thymocytes isolated from mice lacking S1P show only a minor increase in surface S1PR1 (Pappu et al., 2007). To test whether dynamin 2 is also required for S1PR1 down-modulation in thymocytes, we treated mice with the S1P receptor agonist FTY720. Dynamin 2–deficient thymocytes exhibited reduced FTY720-induced S1PR1 down-modulation (Fig. 4 C). Interestingly, S1PR1 internalization was largely complete on Dnm2 KO T cells in blood (Fig. 4 A). This finding suggested that, depending on the local S1P concentration, distinct pathways regulate S1PR1 internalization: Dynamin 2–mediated S1PR1 internalization occurs in response to low S1P concentrations (e.g., thymus and lymph nodes), whereas dynamin 2–independent mechanisms operate in higher S1P environments such as blood. Consistent with this possibility, the defect in FTY720-induced S1PR1 internalization was most prominent at low (1–2 mg/kg) and overcome at high (4 mg/kg) FTY720 concentrations in dynamin 2–deficient cells (Fig. 4, D and E). To further confirm this concept, we raised the normally low S1P concentration in the thymus to that in blood by inhibiting S1P degradation with DOP (Schwab et al., 2005). In agreement with our hypothesis, DOP treatment led to complete S1PR1 down-modulation in Dnm2 KO thymocytes (Fig. 4, F and G). Exposure of mature thymocytes to increasing concentrations of S1P in vitro confirmed that dynamin 2 is dispensable for S1PR1 internalization at high S1P concentrations (100–1,000 nM; Fig. 4 H and see Fig. 8 D) that are similar to those found in circulatory fluids (Schwab et al., 2005; Pappu et al., 2007; Cyster and Schwab, 2012). S1PR1 down-modulation seemed to be more marked in response to high ligand concentration in vivo (Fig. 4, C–G) than in vitro (Fig. 4 H).
Figure 4.
Dynamin 2 is necessary for ligand-induced S1PR1 internalization at low S1P concentrations. (A) S1PR1 surface expression on mature CD4 SP thymocytes and naive (CD44lo) CD4 T cells from Dnm2 HET and KO cells (n > 10) was measured by flow cytometry. To define background S1PR1 staining, control mice were injected i.p. with FTY720 16 h before flow cytometry. (B) S1PR1 surface expression on splenic naive CD4 T cells from Dnm2 HET/B6 and Dnm2 KO/B6 mixed bone marrow chimeras (n = 6) generated as in Fig. 1 G. Green histograms represent background S1PR1 staining (thymocytes from control chimeras injected with FTY720). (C) Dnm2 HET and KO mice were injected i.p. with PBS or FTY720 (2 mg/kg body weight). S1PR1 surface expression on mature CD4 SP thymocytes (n = 6) was measured by flow cytometry 16 h later. Green histograms represent S1PR1 staining on DP thymocytes as negative control. (D and E) S1PR1 surface expression on mature CD4 SP thymocytes from Dnm2 HET and KO mice treated with PBS or the indicated concentrations (per body weight) of FTY720 16 h before analysis (n = 3). (F and G) Dnm2 HET and KO mice received 30 mg/liter DOP in the drinking water or water alone. 3 d later, S1PR1 surface expression on mature CD4 SP thymocytes (n = 7) was measured by flow cytometry. Green histograms represent background S1PR1 staining (thymocytes from mice injected with FTY720). (H) S1PR1 surface expression on mature CD4 SP thymocytes from Dnm2 HET and KO mice treated in vitro with the indicated concentrations of S1P (n = 3–7). All error bars represent SEM. *, P < 0.05; **, P < 0.01 by unpaired Student’s t test. Results are representative of or combined from two (B, F, and G), three (C–E and H), or four (A) experiments.
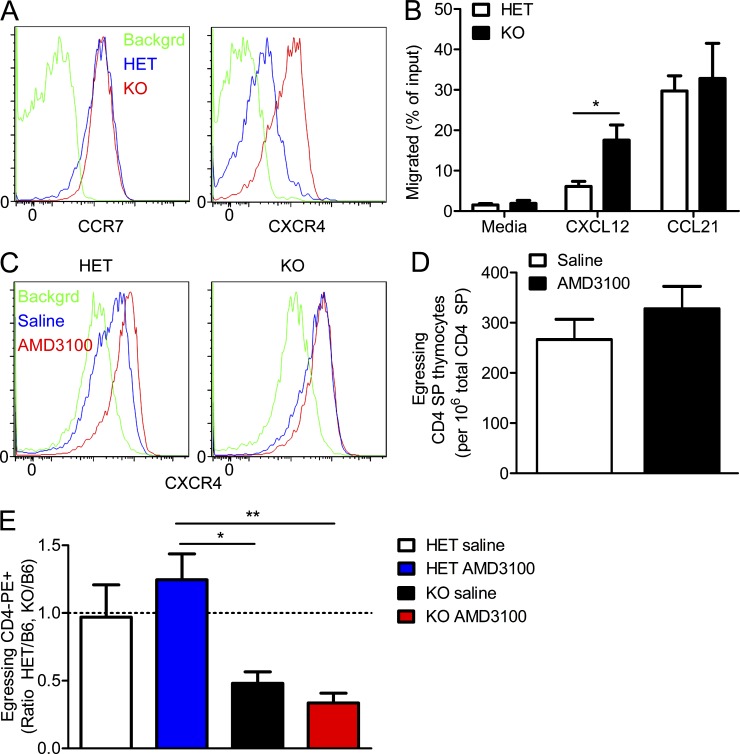
Finally, we examined whether dynamin 2 regulated the internalization of other GPCRs besides S1PR1 that are involved in thymocyte migration. Surface expression of the chemokine receptor CCR7 was not altered in dynamin 2–deficient thymocytes, whereas Dnm2 KO T cells expressed more CXCR4 on the cell surface than Dnm2 HET cells (Fig. 5 A). Consistent with higher CXCR4 expression, mature CD4 SP thymocytes from Dnm2 KO mice showed enhanced chemotaxis toward the CXCR4 ligand CXCL12 in vitro, whereas chemotaxis to the CCR7 ligand CCL21 was not different between Dnm2 HET and KO cells (Fig. 5 B). Thus, dynamin 2 is required for the internalization of S1PR1 and CXCR4 but dispensable for the internalization of CCR7. We hypothesized that this requirement of dynamin 2 for the internalization of specific GPCRs is caused by intrinsic differences in their interactions with ligands. To test this hypothesis, we determined ligand-induced internalization of S1PR1, CXCR4, and CCR7 in WT thymocytes. In support of our hypothesis, we found that S1P induced S1PR1 down-modulation from the cell surface at concentrations as low as 0.1 nM, whereas CCR7 down-modulation occurred only at a 100-times-higher ligand concentration (10 nM CCL21; Fig. 6). CXCR4 showed intermediate sensitivity to ligand-induced internalization (1 nM CXCL12; Fig. 6). The increased response of Dnm2 KO thymocytes to CXCL12 (Fig. 5 B) led us to ask whether CXCR4-mediated retention could contribute to the impaired egress of thymocytes lacking dynamin 2. To address this possibility, we treated Dnm2 KO mice with the specific CXCR4 antagonist AMD3100, which prevents binding of the ligand CXCL12 to the receptor (Donzella et al., 1998). As expected, AMD3100 treatment caused increased CXCR4 surface expression on Dnm2 HET thymocytes as the result of reduced ligand-induced receptor internalization (Fig. 5 C). In contrast, surface CXCR4 did not further increase in dynamin 2–deficient cells after treatment (Fig. 5 C), consistent with impaired receptor internalization caused by dynamin 2 deficiency. AMD3100 treatment only slightly increased the number of egressing B6 CD4 SP thymocytes (Fig. 5 D), suggesting that CXCR4 does not play a major role in the egress of WT thymocytes. This is consistent with our observation that inhibiting signaling through all Gαi-dependent receptors leads to defective, not enhanced, egress (Fig. 2 C), supporting the notion that egress-promoting signals (through S1PR1) dominate over any retention signals (through chemokine receptors) in the thymus. Blocking CXCR4 did not rescue the defective egress of Dnm2 KO thymocytes (Fig. 5 E), demonstrating that dynamin 2 deficiency does not cause impaired thymic egress through CXCR4-mediated retention. We conclude that dynamin 2 specifically regulates GPCRs that are internalized at low ligand concentrations, which explains the strong effect of dynamin 2 deficiency on S1PR1 internalization and signaling.
Figure 5.
Effect of dynamin 2 deficiency on thymocyte chemokine receptors. (A) CCR7 and CXCR4 surface expression on mature CD4 SP thymocytes from Dnm2 HET and KO mice (n = 6). (B) Chemotaxis of mature CD4 SP thymocytes from Dnm2 HET and KO mice. Migration through 5-µM Transwells in response to 0.3 µg/ml CXCL12 or 1 µg/ml CCL21 was assessed by flow cytometry after 3 h (n = 5–9). (C) Mixed Dnm2 HET/B6 and Dnm2 KO/B6 bone marrow chimeras generated as in Fig. 1 G were treated with saline or 1 mg AMD3100. After 24 h of continuous treatment, CXCR4 surface expression on mature CD4 SP thymocytes was measured by flow cytometry. (A and C) Green histograms show isotype staining (backgrd). (D) Number of egressing WT (B6) CD4 SP thymocytes from mixed bone marrow chimeras treated with saline (n = 9) or AMD3100 (n = 10) as in C. (E) Ratio of egressing CD4 SP thymocytes from Dnm2 HET/B6 and Dnm2 KO/B6 mixed bone marrow chimeras treated with saline or AMD3100 (n = 5) as in C. The dashed line indicates a control cell/KO cell ratio of 1. All error bars represent SEM. *, P < 0.05; **, P < 0.01 by unpaired Student’s t test (B) or one-way ANOVA, Tukey’s post-test (E). Results are representative of or combined from two (A and C–E) or five (B) experiments.
Figure 6.
Differential sensitivity of thymocyte-expressed GPCRs to ligand-induced internalization. (A and B) Thymocytes from WT mice were incubated with the indicated concentrations of S1P, CXCL12, or CCL21 in vitro. Flow cytometry was used to measure S1PR1, CXCR4, and CCR7 surface expression in response to their ligands S1P, CXCL12, and CCL21, respectively. (A) Representative histograms showing S1PR1 and CCR7 surface expression on mature CD4 SP thymocytes and CXCR4 expression on DP thymocytes. (B) Ligand-induced down-modulation of S1PR1, CXCR4, and CCR7 in response to their respective ligands (n = 6). Receptor down-modulation is shown as percent surface down-modulation (calculated as described in Materials and methods) to account for differences in staining intensity between receptors and to compare them in the same graph. Error bars represent SEM. Results are representative of or combined from two experiments.
S1PR1 internalization and CD69 down-modulation are independent of Gαi signaling in vivo
We next wished to establish whether the defect in S1PR1 internalization caused impaired S1PR1 signaling or, alternatively, if impaired S1PR1 internalization was caused by a primary defect in S1PR1 signaling. The latter predicts that S1PR1 internalization is dependent on intact S1PR1 signaling. To test this prediction, we took advantage of Rosa26PTX mice in which pertussis toxin (PTX) is expressed in a Cre-dependent manner (Regard et al., 2007). PTX blocks GPCR signaling by catalyzing ADP ribosylation of Gαi proteins in an irreversible manner. We crossed Rosa26PTX mice with Cd4-Cre transgenic mice to achieve PTX expression and inhibition of Gαi signaling specifically in T cells. Cd4-creRosa26PTX/+ mice had more mature thymocytes and developed lymphopenia (not depicted), as expected (Chaffin and Perlmutter, 1991). Interestingly, surface S1PR1 expression on peripheral T cells from Cd4-creRosa26PTX/+ mice was unaffected (Fig. 7 A), and S1PR1 down-modulation in thymocytes occurred normally after FTY720 administration (Fig. 7 B). Similar to CD4 SP thymocytes, chemotaxis to CCL21 was largely abolished in splenic CD4 T cells from Cd4-creRosa26PTX/+ mice (preliminary data not depicted), suggesting that most peripheral Cd4-creRosa26PTX/+ T cells have not escaped Cre-mediated excision of the transcriptional silencer cassette upstream of PTX (Regard et al., 2007) and do express PTX protein. These results demonstrate that Gαi signaling was not required for S1PR1 internalization in vivo. To our surprise, Cd4-creRosa26PTX/+ thymocytes did not coexpress S1PR1 and CD69 on the cell surface (Fig. 7 C), establishing that S1PR1-mediated CD69 down-modulation in vivo is also independent of Gαi signaling. These data contrast with a PTX-sensitive CD69-S1PR1 interaction in a B cell line in vitro (Shiow et al., 2006; Bankovich et al., 2010).
Figure 7.
S1PR1 internalization and CD69 down-modulation are not dependent on Gαi signaling. (A) S1PR1 surface expression on mature CD4 SP thymocytes and naive CD4 T cells (n = 5). Green histograms represent background S1PR1 staining (FTY720-treated mice). (B) WT and Cd4-creRosa26PTX/+ mice were injected i.p. with PBS or FTY720 (2 mg/kg body weight). S1PR1 surface expression on mature CD4 SP thymocytes (n = 3) was measured by flow cytometry 16 h later. Green histograms represent S1PR1 staining on DP thymocytes as negative control. (C) S1PR1 and CD69 surface expression on CD4 SP thymocytes from WT and Cd4-creRosa26PTX/+ mice (n = 4). Results are representative of two (B and C) or three (A) experiments.
Dynamin 2 is critical for continuous S1PR1 signaling and lymph node egress
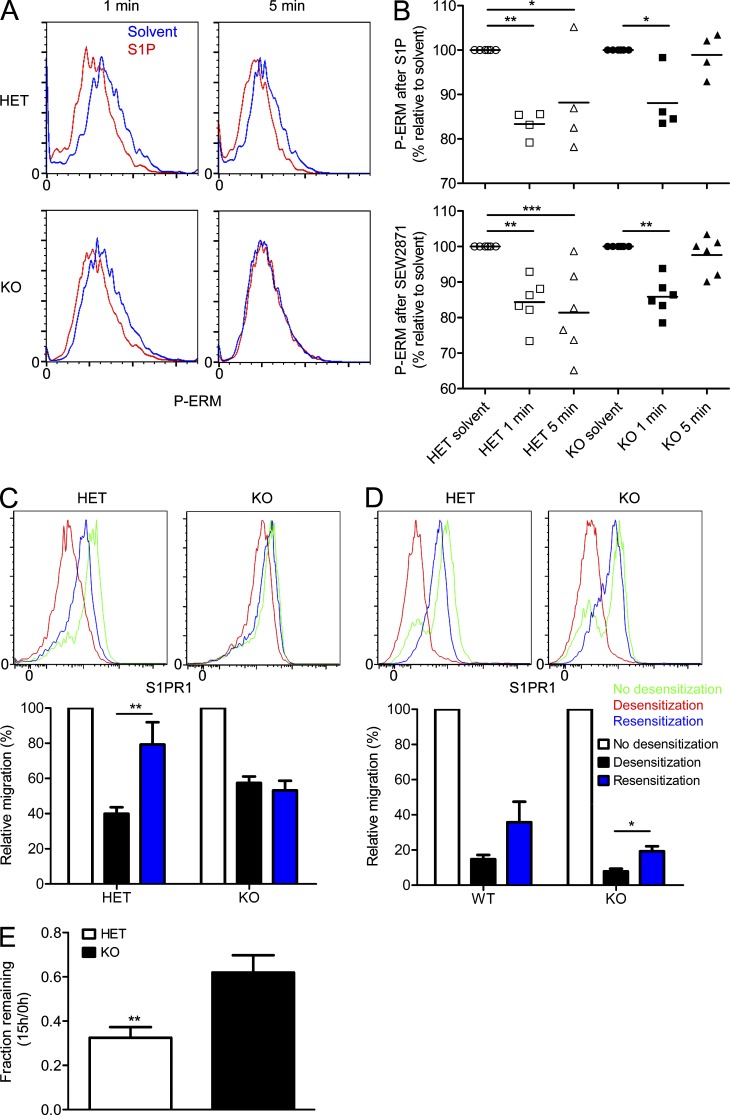
GPCR internalization can support signaling either by continued signaling from internalized receptors or by receptor resensitization during recycling of the receptor back to the cell surface (Sorkin and von Zastrow, 2009). Thus, we asked whether dynamin 2–dependent internalization sustains S1PR1 signaling. To address this question, we stimulated Dnm2 KO thymocytes with S1P in vitro. To measure S1PR1 signaling, we examined the phosphorylation status of ezrin/radixin/moesin (ERM) proteins because Gαi signaling is sufficient to dephosphorylate ERM proteins (Arnon et al., 2011). In contrast to control cells, dynamin 2–deficient mature SP thymocytes displayed impaired ERM dephosphorylation in response to S1P (Fig. 8 A). Closer examination revealed that although the initial S1PR1 signaling at 1 min reduced phospho-ERM (pERM) by ∼20%, the levels were restored to nearly 100% at 5 min in Dnm2 KO cells, whereas pERM levels continued to decrease in dynamin 2–sufficient T cells (Fig. 8 B). We obtained similar results with the S1PR1 agonist SEW2871 (Fig. 8 B), confirming that the observed signaling induced by S1P occurred through S1PR1. Thus, dynamin 2–sufficient T cells were capable of sustained S1PR1 signaling, whereas in dynamin 2–deficient cells, S1PR1 signals in a pulse and is not maintained.
Figure 8.
Dynamin 2 is essential for sustained S1PR1 signaling and lymph node egress. (A and B) Thymocytes from Dnm2 HET and KO mice were treated with solvent, 100 nM S1P, or 1 µM SEW2871 (S1PR1 agonist) in vitro. After 1 and 5 min, intracellular pERM expression was measured in mature CD4 SP thymocytes by flow cytometry. (A) Representative histograms showing intracellular pERM expression in mature CD4 SP thymocytes. (B) pERM expression after stimulation with S1P or SEW2871 was normalized to solvent control. Symbols represent measurements from individual mice (n = 4–6). Horizontal bars indicate the mean. (C and D, top) Thymocytes from Dnm2 HET and KO mice were not exposed to S1P (no desensitization), exposed to low (10 nM; C) or high (1,000 nM; D) S1P concentration (desensitization), or exposed to S1P and washed/rested for 30 min after exposure to S1P (resensitization). S1PR1 surface expression on mature CD4 SP thymocytes was measured by flow cytometry. (bottom) Transwell migration of mature CD4 SP thymocytes from Dnm2 HET and KO mice to 50 nM S1P (n = 5). No desensitization, cells not preexposed to S1P; desensitization, cells preexposed to low (1–10 nM; C) or high (1,000 nM; D) S1P concentration; resensitization, cells preexposed to S1P, washed, and incubated in medium without S1P for 30 min before the Transwell assay. Migration was normalized to that of non-desensitized cells to allow comparison between different experiments. (E) Fluorescently labeled Dnm2 HET and KO splenocytes (CD45.2+) were cotransferred into B6 recipient mice (CD45.1+) to measure T cell egress from lymph nodes as described in Materials and methods. The fraction of transferred CD4 T cells remaining in lymph nodes 15 h after injection of Abs against integrin αL and α4 was measured by flow cytometry (n = 6). All error bars represent SEM. *, P < 0.05; **, P < 0.01; ***, P < 0.001 by unpaired Student’s t test (E) or one-way ANOVA, Tukey’s post-test (B–D). Results are representative of or combined from two (A, B, and E) or three (C and D) experiments.
Defective S1PR1 resensitization would allow each receptor molecule to pulse signal, but not to signal continuously. If this is the case, the magnitude of pulse signaling in response to S1P should be normal. This is a testable hypothesis using in vitro transwell chemotaxis assays. In brief, chemotaxis assays measuring migration toward S1P gradients are notoriously difficult and inefficient at measuring S1PR1 responses, and this is argued to be the result of rapid S1PR1 internalization and desensitization caused by constant exposure to S1P. Thus, in these assays S1PR1 signaling is brief and can only support chemotaxis for a short period of time. We took advantage of these limitations and compared the chemotaxis of dynamin 2–deficient and –sufficient cells toward S1P. We observed that Dnm2 HET and KO thymocytes had a similar chemotactic response to S1P in vitro (Fig. 9, A and B), strongly suggesting that the magnitude of pulse S1PR1 signaling is similar. In support of this possibility, we found that inhibition of forskolin-induced intracellular cAMP generation (Thangada et al., 2010) by S1P was similar in Dnm2 WT and KO cells after brief stimulation in vitro (Fig. 9, C and D).
Figure 9.
Normal primary chemotaxis of dynamin 2–deficient thymocytes to S1P in vitro. (A and B) Transwell migration of mature CD4 SP thymocytes from Dnm2 HET and KO mice (A) or from Dnm2 HET/B6 and Dnm2 KO/B6 mixed bone marrow chimeras (B) to S1P (n = 5). (C and D) cAMP amounts in thymocytes from Dnm2 WT and KO mice after incubation for 1 (C) and 5 min (D) in medium containing IBMX (phosphodiesterase inhibitor) and FSK (forskolin; adenylate cyclase activator) in the absence or presence of 10 nM S1P. All error bars represent SEM. Results are representative of or combined from two (B–D) or five (A) experiments.
These observations also raise the hypothesis that dynamin 2 is required for S1PR1 resensitization. To directly test this possibility, we performed transwell migration assays to S1P in vitro after S1PR1 desensitization and resensitization. Thymocytes were preexposed to S1P to desensitize S1PR1, washed extensively to remove S1P, and incubated in medium without S1P to allow S1PR1 resensitization, or only washed once immediately before the chemotaxis assay (no resensitization). For desensitization, we used low S1P concentrations (1–10 nM) that are likely to occur within thymus and lymph nodes, but are lower than in blood (100–1,000 nM). We detected down-modulation of S1PR1 from the cell surface in control cells after exposure to S1P (desensitization), followed by reexpression of S1PR1 after removal of S1P (resensitization; Fig. 8 C). S1P-induced S1PR1 down-modulation was reduced in Dnm2 KO cells (Fig. 8 C), but the amount of surface S1PR1 after resensitization was not lower than in control cells. Chemotaxis assays showed that S1PR1 resensitized in control thymocytes (Fig. 8 C), allowing them to respond to a second exposure of S1P (∼80% of non-desensitized response). In contrast, S1PR1 was not resensitized in Dnm2 KO cells (Fig. 8 C) despite similar surface expression, suggesting that surface S1PR1 in dynamin 2–deficient cells remains desensitized after exposure to S1P.
We also tested S1PR1 resensitization after desensitization of the receptor with a high S1P concentration (1,000 nM) that induces full S1PR1 down-modulation in both Dnm2 HET and KO cells (Fig. 8 D). S1PR1 surface expression did not recover in thymocytes that were preexposed to 1,000 nM S1P, washed, and resensitized in S1P-free medium (not depicted), likely because of inefficient removal of surface-bound S1P. To overcome this problem, we incubated the thymocytes with splenocytes using a protocol by Kabashima et al. (2006) because splenic B cells have the ability to degrade extracellular S1P. After a 30-min coincubation, the splenocytes (CD45.1+) were immunomagnetically removed before the resensitized thymocytes (CD45.2+) were subjected to chemotaxis assays. This approach resulted in almost complete restoration of S1PR1 surface expression in resensitized thymocytes (Fig. 8 D). However, both Dnm2 HET and KO cells showed poor S1PR1 resensitization as measured by chemotaxis to S1P (Fig. 8 D). Overall, we conclude that dynamin 2–dependent internalization is critical for S1PR1 resensitization after exposure to low S1P concentrations, thereby allowing continuous signaling.
T cell egress from lymph nodes is dependent on S1PR1-mediated reverse transmigration into the cortical lymphatic sinus (Grigorova et al., 2009; Cyster and Schwab, 2012), whereas S1PR1 is not required to approach the sinus (egress site). This raises the possibility that a pulse of S1PR1 signaling is sufficient for the reverse transmigration step and for lymph node egress. The fact that dynamin 2–sufficient T cells are capable of continuous S1PR1 signaling, whereas dynamin 2–deficient cells can only pulse signal, enabled us to test this possibility. To measure lymph node egress, we cotransferred dye-labeled Dnm2 HET and KO cells (CD45.2+) into WT B6 recipients (CD45.1+) and allowed the cells to equilibrate for 24 h before blocking further lymph node entry by the injection of blocking Abs against α4 and αL integrins (Pham et al., 2008). Lymph nodes were harvested before (t1 = 0 h) and 15 h after integrin blockade (t2 = 15 h), and the fraction of transferred Dnm2 HET and KO cells (t2/t1) remaining in lymph nodes was determined by flow cytometry. We found that significantly fewer Dnm2 KO cells had left the lymph nodes as compared with Dnm2 HET cells (Fig. 8 E). The greater reduction in circulating over lymphoid-resident T cells (Fig. 1 B) is also consistent with impaired lymph node exit in Dnm2 KO mice. We conclude that dynamin 2–dependent continuous S1PR1 signaling is essential for T cell egress from lymph nodes in addition to thymus.
S1PR1 overexpression rescues T cell egress in dynamin 2–deficient mice
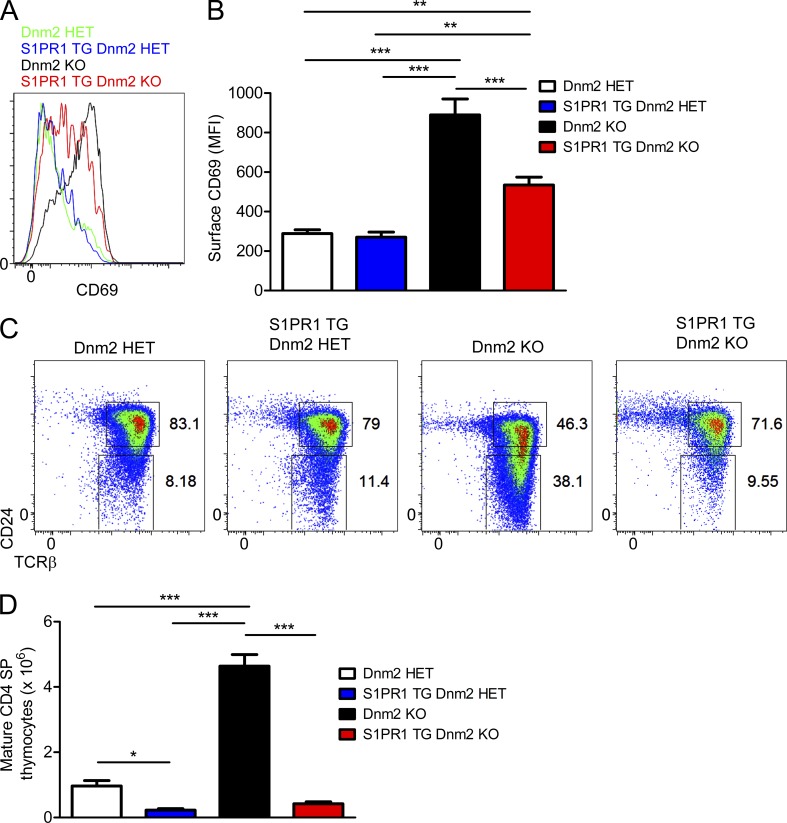
The fact that S1PR1 is both necessary (Matloubian et al., 2004) and sufficient (Zachariah and Cyster, 2010) for egress, coupled to our observation that S1PR1 function is impaired in cells lacking dynamin 2 (Figs. 3 and 8), strongly suggests that dynamin 2 specifically promotes egress by regulating S1PR1. The latter predicts that overexpression of S1PR1 should improve T cell egress in Dnm2 KO mice. To test this prediction and exclude any non-S1PR1–dependent effects, we crossed Dnm2 KO mice to S1PR1 transgenic mice (Zachariah and Cyster, 2010). S1PR1 overexpression improved S1PR1 signaling in dynamin 2–deficient mature CD4 SP thymocytes because it significantly reduced the elevated CD69 surface expression (Fig. 10, A and B). Improved S1PR1 signaling in S1PR1 transgenic Dnm2 KO mice prevented the accumulation of mature CD4 SP thymocytes that occurs in Dnm2 KO mice (Fig. 10, C and D), consistent with improved thymic egress. S1PR1 overexpression also rescued the egress of dynamin 2–deficient T cells from lymph nodes (preliminary data not depicted). These results collectively suggest that dynamin 2 acts specifically through S1PR1 to promote T cell egress from lymphoid organs.
Figure 10.
S1PR1 overexpression rescues T cell egress in dynamin 2–deficient mice. (A and B) CD69 surface expression on mature CD4 SP thymocytes from Dnm2 HET, S1PR1 TG Dnm2 HET, Dnm2 KO, and S1PR1 TG Dnm2 KO mice (n = 6–9). (C and D) Flow cytometric analysis of CD4 SP thymocytes (C) and numbers of mature CD4 SP thymocytes (D) from Dnm2 HET, S1PR1 TG Dnm2 HET, Dnm2 KO, and S1PR1 TG Dnm2 KO mice (n = 9–12). All error bars represent SEM. *, P < 0.05; **, P < 0.01; ***, P < 0.001 by one-way ANOVA, Tukey’s post-test. Results are representative of or combined from two (A and B) or three (C and D) experiments.
DISCUSSION
Endocytosis is a fundamental process that regulates the abundance of proteins and the signaling output of receptors in the plasma membrane (Sorkin and von Zastrow, 2009). Dynamins are GTPases that are required for endocytosis by promoting the final membrane fission step (Praefcke and McMahon, 2004; Schmid and Frolov, 2011; Ferguson and De Camilli, 2012). In this study, we identify dynamin 2 as a novel and essential regulator of S1PR1 signaling and of T cell egress from lymphoid organs.
S1PR1 promotes lymphocyte egress by sensing sharp S1P concentration gradients, with S1P being abundant in circulatory fluids (blood and lymph) and undetectable in lymphoid organ interstitium (Cyster and Schwab, 2012). Minutes after sensing S1P, S1PR1 signaling is rapidly terminated by GRK2-dependent phosphorylation and by receptor internalization (Watterson et al., 2002; Arnon et al., 2011). We establish a crucial role for dynamin 2 in S1PR1 internalization and for sustaining signaling through the receptor. The thymus is a low S1P environment, and it has been shown that the rate of thymic egress, surface S1PR1 levels, and surface CD69 expression on mature thymocytes are all dependent on S1PR1 signaling. All three of these parameters are altered in dynamin 2–deficient thymocytes, strongly suggesting that dynamin 2 is required for S1PR1 signaling in a low S1P environment. Our results demonstrate that S1PR1 internalization is critical for receptor resensitization, which enables continuous S1PR1 signaling in the presence of low S1P concentrations and promotes lymphocyte egress. We propose that, in the absence of dynamin 2, S1PR1 remains phosphorylated, associated with β-arrestins, and unavailable for G protein association, i.e., desensitized after exposure to S1P.
A previous study demonstrated that thymocytes are attracted to low S1P concentrations generated by specialized pericytes that ensheath blood vessels (Zachariah and Cyster, 2010). In lymph nodes, however, although T lymphocytes reach lymphatic vessel exit sites in an S1PR1-independent manner, they require S1PR1 for entering lymphatic sinuses. We now establish that in both situations the rapid dynamin 2–dependent S1PR1 internalization is critical for T lymphocyte egress. We propose that when cells encounter low S1P environments, cycles of S1PR1 signaling, GRK2-dependent desensitization, and dynamin 2–dependent resensitization allow cell access to exit sites and/or the rapid transition from sinus probing to transendothelial migration (Grigorova et al., 2009). The time course of S1PR1 resensitization in vivo relative to the exit time is unknown. It is also unknown how many rounds of S1PR1 signaling are required for egress and what fraction of S1PR1 receptors needs to be engaged. Our findings in dynamin 2–deficient mice provide a starting point for studying these interesting questions in the future.
Our finding that Dnm2 KO cells showed normal chemotaxis to S1P suggested that the brief S1PR1 pulse signaling that occurs during in chemotaxis assays was sufficient for migration toward S1P in vitro, whereas migration to S1P in vivo required continuous S1PR1 signaling. It is known that S1PR1-mediated responses of lymphocytes to S1P are not very robust in vitro, although the receptor functions efficiently in vivo (Cyster and Schwab, 2012). Therefore, any differences in S1PR1 activity between WT and dynamin 2–deficient T cells might be more pronounced in vivo than in vitro, where maximal responses are small. Importantly, S1PR1 resensitization cannot occur during chemotaxis assays because of the continued presence of S1P, and therefore, the extent of S1PR1 desensitization alone may determine the magnitude of the response to S1P in vitro. In contrast to this situation, T cells likely encounter low gradient concentrations of S1P during their interstitial migration in the thymus over an extended period of time, and in these circumstances S1PR1 resensitization occurs. Alternatively, dynamin 2–dependent S1PR1 internalization could promote egress by modulating the S1PR1 signal that is required for the transmigration step while T lymphocytes are egressing.
Dynamin 2 deficiency is likely to affect the internalization of multiple surface receptors. However, our data strongly suggest that dynamin 2 promotes T lymphocyte egress specifically through regulation of S1PR1. First, S1PR1 has a nonredundant role in T cell egress because its expression in T cells is both necessary (Matloubian et al., 2004) and sufficient (Zachariah and Cyster, 2010) for egress as shown in S1PR1 KO and S1PR1 transgenic mice, respectively. Second, chemokine-mediated retention is unlikely to explain defective thymic egress because egress-promoting signals through S1PR1 predominate over any retention signals as shown in mice with blocked Gαi signaling. In support of this, inhibition of CXCR4 function did not improve the egress of dynamin 2–deficient cells. Third, impaired egress in Dnm2 KO mice is not caused by a general defect in cell motility because T cells lacking dynamin 2 were able to migrate toward various chemotactic stimuli in vitro. Importantly, we found that S1PR1 overexpression rescued the egress defect of dynamin 2–deficient T cells, consistent with a specific function of dynamin 2 in S1PR1-mediated egress. We propose that this is explained by the unique biology of S1PR1 because it is likely to be the T cell–expressed GPCR that is most sensitive to ligand-induced internalization and should therefore be highly dependent on mechanisms that maintain or restore receptor responsiveness.
We observed that impaired S1PR1 internalization caused by the absence of dynamin 2 resulted in increased S1PR1 surface expression. Based on prior knowledge, this was predicted to lead to enhanced responsiveness of dynamin 2–deficient cells to S1P because of reduced signal termination as in cells lacking GRK2 (Arnon et al., 2011). Unexpectedly, loss of dynamin 2 caused impaired rather than enhanced S1PR1 function. Egress is sensitive to the amount of surface S1PR1 because S1PR1 heterozygous T cells (which have less surface S1PR1) show reduced egress compared with WT cells (Lo et al., 2005). Thus, it was especially surprising that dynamin 2 deficiency in lymph node T cells caused impaired egress despite having approximately two- to threefold more S1PR1 on their cell surface. Overall, our results demonstrate a novel and unexpected role of receptor internalization for S1PR1 function, underscoring the unique properties of this lipid-recognizing receptor.
Our findings therefore conclusively define the role played by S1PR1 internalization in regulating S1PR1 function during T lymphocyte trafficking. A previous study has shown that GRK2-mediated S1PR1 internalization terminates S1PR1 signaling and allows the homing of lymphocytes from blood to lymphoid tissues, i.e., from a high to a low S1P environment (Arnon et al., 2011). Similarly, another study, using knock-in mice expressing S1PR1 with a mutated proximal C-terminal desensitization motif, demonstrated a role of S1PR1 internalization in limiting responses to high S1PR1 ligand concentrations (FTY720 administration; Thangada et al., 2010). Remarkably, our findings reveal that S1PR1 internalization is especially important for enabling sustained S1PR1 signaling in the presence of low S1P concentrations, a feature which is perhaps shared among GPCRs characterized by high sensitivity for ligand-mediated internalization and desensitization (Arnon et al., 2011; Cyster and Schwab, 2012). Thus, in an S1P-high environment (blood), receptor internalization functions to terminate S1PR1 signaling and promotes tissue homing, whereas in an S1P-low environment (found near exit sites in thymus and lymph nodes), S1PR1 internalization permits continuous signaling and egress.
An interesting area for future studies will be the elucidation of the molecular basis for the preferential role for dynamin 2 in S1PR1 internalization after exposure to low versus high concentrations of S1P. Although less well-characterized, the existence of dynamin- and clathrin-independent endocytic mechanisms is well established (Howes et al., 2010). For example, bulk endocytosis/pinocytosis is intact in cells lacking functional dynamin (Damke et al., 1994; Ferguson et al., 2009), and, very similar to what we observed for S1PR1, the EGF receptor is preferentially internalized by clathrin- and dynamin-dependent mechanisms in response to stimulation with low concentrations of ligand but can be internalized in a clathrin- and dynamin-independent manner when cells are exposed to high EGF (Sigismund et al., 2005). Interestingly, in the case of EGFR and also TGFβR, clathrin-dependent endocytosis in response to low ligand concentration promotes receptor recycling and persistent signaling, whereas high concentrations of ligand triggers an alternative internalization and trafficking mechanism that promotes their degradation (Le Roy and Wrana, 2005). Therefore, saturation of receptor occupancy and maximal activation of downstream signaling pathways by high ligand concentration might trigger the recruitment of alternative components of the endocytic machinery to ensure efficient receptor internalization and signal termination. A better molecular understanding of dynamin-independent forms of endocytosis will be necessary to address this interesting area of S1P-S1PR1 biology.
A previous study reported S1PR1-CD69 surface coexpression (impaired CD69 down-modulation) in an immature B cell line after treatment with PTX (Shiow et al., 2006). Surprisingly, we find that S1PR1 internalization and S1PR1-mediated CD69 down-modulation are both independent of Gαi signaling, whereas Gαi signaling is required for thymic egress, as expected (Chaffin and Perlmutter, 1991). We suspect that these conflicting findings are caused by the differences in the cell types analyzed and in the methods used for PTX delivery. Specifically, PTX treatment in vitro can induce TLR4 signaling (Nishida et al., 2010). Furthermore, TLR4 is already expressed during the early stages of B cell development and induces CD69 expression in B cells (Pereira et al., 2003). In contrast, in the Cd4-creRosa26PTX/+ mice used in our study, PTX is expressed intracellularly in T cells and naive T cells do not express TLR4 (Caramalho et al., 2003).
Therefore, our results suggest a differential requirement of Gαi signaling for S1P-mediated responses that occur in thymocytes during their maturation. Both S1PR1 internalization and S1PR1-mediated CD69 down-modulation are dependent on dynamin 2 (and GRK2) but independent of Gαi signaling. In contrast, thymic egress requires dynamin 2 (but not GRK2) and is dependent on Gαi signaling. These findings raise the interesting possibility that some S1PR1 signaling events are mediated by coupling to Gα proteins other than Gαi. Switching of G proteins (resulting in different signaling outputs) has been described for the β2-adrenergic receptor (Sorkin and von Zastrow, 2009). Possible candidates that mediate S1PR1 internalization are Gαq proteins. Indeed, CXCR4 can be internalized upon Gαq signaling (Rochdi and Parent, 2003). Alternatively, the Gαi-independent S1PR1 responses could be driven by β-arrestin–mediated signaling (Pierce et al., 2002; Sorkin and von Zastrow, 2009), which would also be dependent on dynamin 2. A precise understanding of the regulation of intracellular S1PR1 trafficking and its effect on S1PR1 signaling is of considerable importance because drugs targeting S1PR1 are now in clinical use for the treatment of autoimmune diseases such as multiple sclerosis (Cyster and Schwab, 2012) and hold promise for the treatment of cytokine storm induced by highly pathogenic viruses (Teijaro et al., 2011).
MATERIALS AND METHODS
Mice.
Dynamin 2 conditional KO mice (Ferguson et al., 2009) were backcrossed to B6 mice for 11 generations and bred to Cd4-Cre transgenic mice (Lee et al., 2001). S1PR1 transgenic mice (provided by J.G. Cyster, University of California, San Francisco [UCSF], San Francisco, CA; Zachariah and Cyster, 2010) were bred to Cd4-creDnm2flox/flox mice to generate S1PR1 TG Cd4-creDnm2flox/+ (“S1PR1 TG Dnm2 HET”) and S1PR1 TG Cd4-creDnm2flox/flox (“S1PR1 TG Dnm2 KO”) mice. Mice expressing PTX under control of the Rosa26 locus in a Cre-dependent manner (provided by S.R. Coughlin, UCSF; Regard et al., 2007) were bred to Cd4-Cre transgenic mice to generate Cd4-creRosa26PTX/+ mice. All mouse experiments were performed in accordance with protocols approved by the Institutional Animal Care and Use Committee of Yale University.
Mixed bone marrow chimeras.
Bone marrow cells from Dnm2 HET or KO mice (CD45.2+) were mixed at a ratio of 1:1 with WT B6 cells (CD45.1+). 2 × 106 cell mixture was injected i.v. into sublethally irradiated (6 Gy) Rag1 KO recipient mice (CD45.1+). Mice were analyzed 7–12 wk after reconstitution.
In vivo treatments.
Mice were injected i.p. with the indicated concentrations of FTY720 (Cayman Chemical) and analyzed 16 h after injection. Mice received 30 mg/liter DOP (Sigma-Aldrich) in the drinking water for 3 d. Because of its short half-life, 1 mg AMD3100 (Cayman Chemical) was administered continuously for 24 h by surgically implanted osmotic mini-pump.
Flow cytometry.
Single-cell suspensions were prepared from organs of mice at 6–12 wk of age. Enriched CD4 SP thymocytes were obtained by negative immunomagnetic selection with CD8 beads (Miltenyi Biotec). For gene expression experiments, double-positive (DP; CD4+CD8+), immature (TCRβhiCD24hi), and mature (TCRβhiCD24lo) CD4 (CD4+CD8−) SP thymocytes were sorted. A “dump” stain for CD25, NK1.1, and TCRγδ was used to exclude regulatory T cells, NKT cells, and γδ T cells. T cells were purified from spleen and lymph nodes by positive immunomagnetic selection using CD4 beads and sorted as naive (CD44loCD62Lhi) CD4+ cells. Cells were stained with fluorochrome-labeled Abs (BioLegend): CD4 (RM4-5), CD8α (53-6.7), TCRβ (H57-597), CD24 (M1/69), CD25 (3C7), CD44 (IM7), CD45.1 (A20), CD45.2 (104), CD62L (MEL-14), CD69 (H1.2F3), NK1.1 (PK136), Qa2 (695H1-9-9), TCRγδ (UC7-13D5), and CCR7 (4B12). Ab against CXCR4 (2B11) was purchased from BD. Surface S1PR1 was detected as described previously (Arnon et al., 2011).
Thymic egress.
Mixed bone marrow chimeras received 20 µl of 1 mg/ml FITC (Sigma-Aldrich) by intrathymic injection, and RTEs were gated as CD4+ or CD8+FITC+ cells in blood, spleen, and lymph nodes 24 h after injection. The ratio of Dnm2 HET or KO RTEs (CD45.2+)/B6 RTEs (CD45.1+) was normalized to thymic FITC+ ratios to account for differences in labeling. Egressing CD4 SP thymocytes were identified by an intravascular labeling technique (Pereira et al., 2009; Zachariah and Cyster, 2010). Mixed bone marrow chimeras were injected i.v. with 1 µg PE-conjugated α-CD4 Ab (clone GK1.5; BioLegend), and thymi were harvested after 4 min. Egressing CD4 SP thymocytes were gated as i.v. CD4-PE+CD8− cells, and the ratio of Dnm2 HET or KO (CD45.2+) egressing cells/B6 (CD45.1+) egressing cells was calculated.
Lymph node egress.
Dnm2 HET and KO splenocytes (CD45.2+) were labeled with 2.5 µM CFSE or 10 µM CMTMR, mixed, and cotransferred into B6 recipient mice (CD45.1+). Transferred cells were allowed to equilibrate for 24 h before blocking further lymph node entry by the i.v. injection of integrin α4 (clone PS/II) and αL (clone M17/4; both from Bio X Cell) Abs at 100 µg each per mouse (Pham et al., 2008). Lymph nodes were harvested before (t1 = 0 h) and 15 h after integrin blockade (t2 = 15 h), and the fraction of transferred Dnm2 HET and KO CD4 T cells (t2/t1) remaining in lymph nodes was determined.
PCR.
Genomic DNA was isolated from tail biopsies and purified cells. WT, floxed, and deleted Dnm2 alleles were distinguished with 5′-CCTGCTAGTGACCTTTCTTGAG-3′ (primer 1), 5′-GCAGGAAGACACACAACTGAAC-3′ (primer 2), and 5′-CAGCAATTCTGGTTGCCAGGCAAGAC-3′ (primer 3). Total RNA was extracted from purified cells with TRIzol reagent (Invitrogen) and used for cDNA synthesis with the SuperScript First-Strand Synthesis system (Invitrogen). Quantitative RT-PCR was performed on a 7500 Fast Real-Time PCR system with primer-probe sets purchased from Applied Biosystems.
Chemotaxis assays.
Enriched CD4 SP thymocytes were rested in migration medium (RPMI 1640/0.5% fatty acid–free BSA [Sigma-Aldrich]/10 mM Hepes) for 30 min at 37°C/5% CO2. Migration through 5-µM Transwells (Corning) in response to 1 µg/ml CCL21 (R&D Systems), 0.3 µg/ml CXCL12 (PeproTech), or S1P (Cayman Chemical) was assessed after 3 h. For S1PR1 resensitization assays, thymocytes were first desensitized by incubation with a low (1–10 nM) or high (1,000 nM) concentration of S1P for 30 min. An aliquot of cells was incubated in medium alone (“no desensitization”). Cells were then either washed three times with warm RPMI 1640 and incubated in medium without S1P for 30 min (“resensitization”) or were not resensitized, i.e., washed once with RPMI 1640 just before the transwell assay (“desensitization”). To recover S1PR1 surface expression after desensitization with 1,000 nM S1P, thymocytes were incubated with CD45.1+ splenocytes as described previously (Kabashima et al., 2006). Chemotaxis to 50 nM S1P was then tested as above.
S1PR1 signaling in vitro.
Total thymocytes were rested in RPMI 1640/10 mM Hepes for 30 min at 37°C/5% CO2 before stimulation with 100 nM SP or 1 µM SEW2871 (Cayman Chemical) or solvent (DMSO). Cells were fixed in 1.5% paraformaldehyde (Electron Microscopy Sciences) for 10 min, washed, and stained with CD4–Alexa Fluor 700, CD8α–Pacific blue, Qa2–Alexa Fluor 647, and CD24-FITC Abs. Cells were permeabilized in 100% ice-cold methanol for 15 min, and intracellular staining with a rabbit pERM polyclonal Ab (Cell Signaling Technology) was performed for 60 min, followed by incubation with a PE-conjugated anti–rabbit secondary Ab (Invitrogen). pERM expression in mature (Qa2hiCD24lo) SP thymocytes was determined. For cAMP measurements, thymocytes were stimulated with 50 µM of the adenylate cyclase activator forskolin (Cayman Chemical) in the absence or presence of 10 nM S1P in medium containing 500 µM of the phosphodiesterase inhibitor IBMX (Cayman Chemical). Intracellular cAMP was extracted with 0.1 M HCl, and cAMP concentrations were determined using the Cyclic AMP EIA kit (Cayman Chemical) according to the manufacturer’s instructions.
GPCR down-modulation in vitro.
Enriched CD4 SP thymocytes were rested in migration medium for 30 min before incubation with the indicated concentrations of S1P, CXCL12, or CCL12 for 1 h at 37°C/5% CO2. After washing, cells were stained for flow cytometric analysis with Abs against S1PR1, CXCR4, and CCR7, respectively. In the case of CXCR4, an acidic glycine wash (Samanta et al., 1990) was performed to remove ligand completely before surface staining. Percent receptor down-modulation was calculated as follows: 100 × [MFI (incubation with medium) − MFI (incubation with ligand)]/MFI (incubation with medium).
CD69 down-modulation in vitro.
Sorted immature (TCRβhiCD24hi) CD4 SP thymocytes were incubated with 10 µg/ml biotinylated hamster α-CD69 Ab (H1.2F3) for 30 min on ice in a 96-well plate (2.5 × 105 cells per well). After washing twice with cold PBS, CD69 was cross-linked with 50 µg/ml goat α-hamster IgG (Jackson ImmunoResearch Laboratories, Inc.) on ice, and cells were incubated for 0, 4, or 16 h at 37°C/5% CO2 to allow CD69 internalization. Cells were washed twice with cold PBS and stained with PE-conjugated streptavidin (BioLegend) for 30 min on ice for flow cytometric analysis.
Statistical analysis.
Student’s t test was used to determine statistical significance between two groups (α = 0.05). For multigroup comparisons, we applied one-way ANOVA with post hoc testing using Tukey’s Multiple Comparison Test (α = 0.05). Error bars represent SEM.
Acknowledgments
We thank J.G. Cyster and S.R. Coughlin for mice and reagents and J. Henao-Mejia and L. Zenewicz for comments on the manuscript.
T. Willinger was supported by an Irvington Institute Postdoctoral Fellowship from the Cancer Research Institute; R.A. Flavell and P. De Camilli are Investigators of the Howard Hughes Medical Institute. This work was supported by National Institutes of Health grant R37NS036251 to P. De Camilli.
The authors declare no competing financial interests.
Footnotes
Abbreviations used:
- Ab
- antibody
- DOP
- deoxypyridoxine
- DP
- double positive
- ERM
- ezrin/radixin/moesin
- GPCR
- G protein–coupled receptor
- PTX
- pertussis toxin
- RTE
- recent thymic emigrant
- S1P
- sphingosine-1-phosphate
- SP
- single positive
References
- Arnon T.I., Xu Y., Lo C., Pham T., An J., Coughlin S., Dorn G.W., Cyster J.G. 2011. GRK2-dependent S1PR1 desensitization is required for lymphocytes to overcome their attraction to blood. Science. 333:1898–1903 10.1126/science.1208248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bankovich A.J., Shiow L.R., Cyster J.G. 2010. CD69 suppresses sphingosine 1-phosophate receptor-1 (S1P1) function through interaction with membrane helix 4. J. Biol. Chem. 285:22328–22337 10.1074/jbc.M110.123299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bréart B., Ramos-Perez W.D., Mendoza A., Salous A.K., Gobert M., Huang Y., Adams R.H., Lafaille J.J., Escalante-Alcalde D., Morris A.J., Schwab S.R. 2011. Lipid phosphate phosphatase 3 enables efficient thymic egress. J. Exp. Med. 208:1267–1278 10.1084/jem.20102551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caramalho I., Lopes-Carvalho T., Ostler D., Zelenay S., Haury M., Demengeot J. 2003. Regulatory T cells selectively express toll-like receptors and are activated by lipopolysaccharide. J. Exp. Med. 197:403–411 10.1084/jem.20021633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson C.M., Endrizzi B.T., Wu J., Ding X., Weinreich M.A., Walsh E.R., Wani M.A., Lingrel J.B., Hogquist K.A., Jameson S.C. 2006. Kruppel-like factor 2 regulates thymocyte and T-cell migration. Nature. 442:299–302 10.1038/nature04882 [DOI] [PubMed] [Google Scholar]
- Chaffin K.E., Perlmutter R.M. 1991. A pertussis toxin-sensitive process controls thymocyte emigration. Eur. J. Immunol. 21:2565–2573 10.1002/eji.1830211038 [DOI] [PubMed] [Google Scholar]
- Cyster J.G., Schwab S.R. 2012. Sphingosine-1-phosphate and lymphocyte egress from lymphoid organs. Annu. Rev. Immunol. 30:69–94 10.1146/annurev-immunol-020711-075011 [DOI] [PubMed] [Google Scholar]
- Damke H., Baba T., Warnock D.E., Schmid S.L. 1994. Induction of mutant dynamin specifically blocks endocytic coated vesicle formation. J. Cell Biol. 127:915–934 10.1083/jcb.127.4.915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donzella G.A., Schols D., Lin S.W., Esté J.A., Nagashima K.A., Maddon P.J., Allaway G.P., Sakmar T.P., Henson G., De Clercq E., Moore J.P. 1998. AMD3100, a small molecule inhibitor of HIV-1 entry via the CXCR4 co-receptor. Nat. Med. 4:72–77 10.1038/nm0198-072 [DOI] [PubMed] [Google Scholar]
- Ferguson S.M., De Camilli P. 2012. Dynamin, a membrane-remodelling GTPase. Nat. Rev. Mol. Cell Biol. 13:75–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson S.M., Brasnjo G., Hayashi M., Wölfel M., Collesi C., Giovedi S., Raimondi A., Gong L.W., Ariel P., Paradise S., et al. 2007. A selective activity-dependent requirement for dynamin 1 in synaptic vesicle endocytosis. Science. 316:570–574 10.1126/science.1140621 [DOI] [PubMed] [Google Scholar]
- Ferguson S.M., Raimondi A., Paradise S., Shen H., Mesaki K., Ferguson A., Destaing O., Ko G., Takasaki J., Cremona O., et al. 2009. Coordinated actions of actin and BAR proteins upstream of dynamin at endocytic clathrin-coated pits. Dev. Cell. 17:811–822 (published erratum appears in Dev. Cell. 2010. 18:332) 10.1016/j.devcel.2009.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson S.S. 2001. Evolving concepts in G protein-coupled receptor endocytosis: the role in receptor desensitization and signaling. Pharmacol. Rev. 53:1–24 [PubMed] [Google Scholar]
- Grigorova I.L., Schwab S.R., Phan T.G., Pham T.H., Okada T., Cyster J.G. 2009. Cortical sinus probing, S1P1-dependent entry and flow-based capture of egressing T cells. Nat. Immunol. 10:58–65 10.1038/ni.1682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howes M.T., Mayor S., Parton R.G. 2010. Molecules, mechanisms, and cellular roles of clathrin-independent endocytosis. Curr. Opin. Cell Biol. 22:519–527 10.1016/j.ceb.2010.04.001 [DOI] [PubMed] [Google Scholar]
- Jenne C.N., Enders A., Rivera R., Watson S.R., Bankovich A.J., Pereira J.P., Xu Y., Roots C.M., Beilke J.N., Banerjee A., et al. 2009. T-bet–dependent S1P5 expression in NK cells promotes egress from lymph nodes and bone marrow. J. Exp. Med. 206:2469–2481 10.1084/jem.20090525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabashima K., Haynes N.M., Xu Y., Nutt S.L., Allende M.L., Proia R.L., Cyster J.G. 2006. Plasma cell S1P1 expression determines secondary lymphoid organ retention versus bone marrow tropism. J. Exp. Med. 203:2683–2690 10.1084/jem.20061289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Roy C., Wrana J.L. 2005. Clathrin- and non-clathrin-mediated endocytic regulation of cell signalling. Nat. Rev. Mol. Cell Biol. 6:112–126 10.1038/nrm1571 [DOI] [PubMed] [Google Scholar]
- Lee M.J., Evans M., Hla T. 1996. The inducible G protein-coupled receptor edg-1 signals via the Gi/mitogen-activated protein kinase pathway. J. Biol. Chem. 271:11272–11279 10.1074/jbc.271.19.11272 [DOI] [PubMed] [Google Scholar]
- Lee M.J., Van Brocklyn J.R., Thangada S., Liu C.H., Hand A.R., Menzeleev R., Spiegel S., Hla T. 1998. Sphingosine-1-phosphate as a ligand for the G protein-coupled receptor EDG-1. Science. 279:1552–1555 10.1126/science.279.5356.1552 [DOI] [PubMed] [Google Scholar]
- Lee P.P., Fitzpatrick D.R., Beard C., Jessup H.K., Lehar S., Makar K.W., Pérez-Melgosa M., Sweetser M.T., Schlissel M.S., Nguyen S., et al. 2001. A critical role for Dnmt1 and DNA methylation in T cell development, function, and survival. Immunity. 15:763–774 10.1016/S1074-7613(01)00227-8 [DOI] [PubMed] [Google Scholar]
- Liu C.H., Thangada S., Lee M.J., Van Brocklyn J.R., Spiegel S., Hla T. 1999. Ligand-induced trafficking of the sphingosine-1-phosphate receptor EDG-1. Mol. Biol. Cell. 10:1179–1190 10.1091/mbc.10.4.1179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo C.G., Xu Y., Proia R.L., Cyster J.G. 2005. Cyclical modulation of sphingosine-1-phosphate receptor 1 surface expression during lymphocyte recirculation and relationship to lymphoid organ transit. J. Exp. Med. 201:291–301 10.1084/jem.20041509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matloubian M., Lo C.G., Cinamon G., Lesneski M.J., Xu Y., Brinkmann V., Allende M.L., Proia R.L., Cyster J.G. 2004. Lymphocyte egress from thymus and peripheral lymphoid organs is dependent on S1P receptor 1. Nature. 427:355–360 10.1038/nature02284 [DOI] [PubMed] [Google Scholar]
- McMahon H.T., Boucrot E. 2011. Molecular mechanism and physiological functions of clathrin-mediated endocytosis. Nat. Rev. Mol. Cell Biol. 12:517–533 10.1038/nrm3151 [DOI] [PubMed] [Google Scholar]
- Nishida M., Suda R., Nagamatsu Y., Tanabe S., Onohara N., Nakaya M., Kanaho Y., Shibata T., Uchida K., Sumimoto H., et al. 2010. Pertussis toxin up-regulates angiotensin type 1 receptors through Toll-like receptor 4-mediated Rac activation. J. Biol. Chem. 285:15268–15277 10.1074/jbc.M109.076232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oo M.L., Thangada S., Wu M.T., Liu C.H., Macdonald T.L., Lynch K.R., Lin C.Y., Hla T. 2007. Immunosuppressive and anti-angiogenic sphingosine 1-phosphate receptor-1 agonists induce ubiquitinylation and proteasomal degradation of the receptor. J. Biol. Chem. 282:9082–9089 10.1074/jbc.M610318200 [DOI] [PubMed] [Google Scholar]
- Oo M.L., Chang S.H., Thangada S., Wu M.T., Rezaul K., Blaho V., Hwang S.I., Han D.K., Hla T. 2011. Engagement of S1P₁-degradative mechanisms leads to vascular leak in mice. J. Clin. Invest. 121:2290–2300 10.1172/JCI45403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappu R., Schwab S.R., Cornelissen I., Pereira J.P., Regard J.B., Xu Y., Camerer E., Zheng Y.W., Huang Y., Cyster J.G., Coughlin S.R. 2007. Promotion of lymphocyte egress into blood and lymph by distinct sources of sphingosine-1-phosphate. Science. 316:295–298 10.1126/science.1139221 [DOI] [PubMed] [Google Scholar]
- Pereira J.P., Girard R., Chaby R., Cumano A., Vieira P. 2003. Monoallelic expression of the murine gene encoding Toll-like receptor 4. Nat. Immunol. 4:464–470 10.1038/ni917 [DOI] [PubMed] [Google Scholar]
- Pereira J.P., An J., Xu Y., Huang Y., Cyster J.G. 2009. Cannabinoid receptor 2 mediates the retention of immature B cells in bone marrow sinusoids. Nat. Immunol. 10:403–411 10.1038/ni.1710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham T.H., Okada T., Matloubian M., Lo C.G., Cyster J.G. 2008. S1P1 receptor signaling overrides retention mediated by Gαi-coupled receptors to promote T cell egress. Immunity. 28:122–133 10.1016/j.immuni.2007.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce K.L., Premont R.T., Lefkowitz R.J. 2002. Seven-transmembrane receptors. Nat. Rev. Mol. Cell Biol. 3:639–650 10.1038/nrm908 [DOI] [PubMed] [Google Scholar]
- Praefcke G.J., McMahon H.T. 2004. The dynamin superfamily: Universal membrane tubulation and fission molecules? Nat. Rev. Mol. Cell Biol. 5:133–147 10.1038/nrm1313 [DOI] [PubMed] [Google Scholar]
- Regard J.B., Kataoka H., Cano D.A., Camerer E., Yin L., Zheng Y.W., Scanlan T.S., Hebrok M., Coughlin S.R. 2007. Probing cell type-specific functions of Gi in vivo identifies GPCR regulators of insulin secretion. J. Clin. Invest. 117:4034–4043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera J., Proia R.L., Olivera A. 2008. The alliance of sphingosine-1-phosphate and its receptors in immunity. Nat. Rev. Immunol. 8:753–763 10.1038/nri2400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochdi M.D., Parent J.L. 2003. Gαq-coupled receptor internalization specifically induced by Gαq signaling. Regulation by EBP50. J. Biol. Chem. 278:17827–17837 10.1074/jbc.M210319200 [DOI] [PubMed] [Google Scholar]
- Rosen H., Gonzalez-Cabrera P.J., Sanna M.G., Brown S. 2009. Sphingosine 1-phosphate receptor signaling. Annu. Rev. Biochem. 78:743–768 10.1146/annurev.biochem.78.072407.103733 [DOI] [PubMed] [Google Scholar]
- Samanta A.K., Oppenheim J.J., Matsushima K. 1990. Interleukin 8 (monocyte-derived neutrophil chemotactic factor) dynamically regulates its own receptor expression on human neutrophils. J. Biol. Chem. 265:183–189 [PubMed] [Google Scholar]
- Schmid S.L., Frolov V.A. 2011. Dynamin: Functional design of a membrane fission catalyst. Annu. Rev. Cell Dev. Biol. 27:79–105 10.1146/annurev-cellbio-100109-104016 [DOI] [PubMed] [Google Scholar]
- Schwab S.R., Pereira J.P., Matloubian M., Xu Y., Huang Y., Cyster J.G. 2005. Lymphocyte sequestration through S1P lyase inhibition and disruption of S1P gradients. Science. 309:1735–1739 10.1126/science.1113640 [DOI] [PubMed] [Google Scholar]
- Shiow L.R., Rosen D.B., Brdicková N., Xu Y., An J., Lanier L.L., Cyster J.G., Matloubian M. 2006. CD69 acts downstream of interferon-α/β to inhibit S1P1 and lymphocyte egress from lymphoid organs. Nature. 440:540–544 10.1038/nature04606 [DOI] [PubMed] [Google Scholar]
- Sigismund S., Woelk T., Puri C., Maspero E., Tacchetti C., Transidico P., Di Fiore P.P., Polo S. 2005. Clathrin-independent endocytosis of ubiquitinated cargos. Proc. Natl. Acad. Sci. USA. 102:2760–2765 10.1073/pnas.0409817102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorkin A., von Zastrow M. 2009. Endocytosis and signalling: Intertwining molecular networks. Nat. Rev. Mol. Cell Biol. 10:609–622 10.1038/nrm2748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel S., Milstien S. 2011. The outs and the ins of sphingosine-1-phosphate in immunity. Nat. Rev. Immunol. 11:403–415 10.1038/nri2974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teijaro J.R., Walsh K.B., Cahalan S., Fremgen D.M., Roberts E., Scott F., Martinborough E., Peach R., Oldstone M.B., Rosen H. 2011. Endothelial cells are central orchestrators of cytokine amplification during influenza virus infection. Cell. 146:980–991 10.1016/j.cell.2011.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thangada S., Khanna K.M., Blaho V.A., Oo M.L., Im D.S., Guo C., Lefrancois L., Hla T. 2010. Cell-surface residence of sphingosine 1-phosphate receptor 1 on lymphocytes determines lymphocyte egress kinetics. J. Exp. Med. 207:1475–1483 10.1084/jem.20091343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watterson K.R., Johnston E., Chalmers C., Pronin A., Cook S.J., Benovic J.L., Palmer T.M. 2002. Dual regulation of EDG1/S1P1 receptor phosphorylation and internalization by protein kinase C and G-protein-coupled receptor kinase 2. J. Biol. Chem. 277:5767–5777 10.1074/jbc.M110647200 [DOI] [PubMed] [Google Scholar]
- Windh R.T., Lee M.J., Hla T., An S., Barr A.J., Manning D.R. 1999. Differential coupling of the sphingosine 1-phosphate receptors Edg-1, Edg-3, and H218/Edg-5 to the Gi, Gq, and G12 families of heterotrimeric G proteins. J. Biol. Chem. 274:27351–27358 10.1074/jbc.274.39.27351 [DOI] [PubMed] [Google Scholar]
- Zachariah M.A., Cyster J.G. 2010. Neural crest-derived pericytes promote egress of mature thymocytes at the corticomedullary junction. Science. 328:1129–1135 10.1126/science.1188222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Barak L.S., Winkler K.E., Caron M.G., Ferguson S.S. 1997. A central role for β-arrestins and clathrin-coated vesicle-mediated endocytosis in β2-adrenergic receptor resensitization. Differential regulation of receptor resensitization in two distinct cell types. J. Biol. Chem. 272:27005–27014 10.1074/jbc.272.43.27005 [DOI] [PubMed] [Google Scholar]