Abstract
Background
Minority physicians are more likely than their counterparts to work in underserved communities and care for minority, poor, and uninsured patients, but much of this research has examined primary care physicians alone. Few have investigated whether non–primary care specialists of minority backgrounds are more likely to serve the underserved than nonminority specialists.
Objective
We examined whether underrepresented minority (URM) physicians from a wide variety of specialties are more likely than non-URM physicians to practice in underserved communities.
Methods
Using California Medical Board Physician Licensure Survey (2007) data for 48 388 physicians, we geocoded practice zip codes to medically underserved areas (MUAs) and primary care health professional shortage areas (HPSAs). Logistic regression models adjusting for age, gender, specialty, and other characteristics were used to explore associations with race, ethnicity, specialty, and designated underserved areas.
Results
We found that African American, Latino, and Pacific Islanders were more likely to work in MUAs and HPSAs than were white physicians (adjusted odds ratio, 1.22–2.25; p < .05). Similar patterns of practice in MUAs and HPSAs by physician race and ethnicity were found when performing the analyses separately among primary care physicians and physicians in non–primary care specialties.
Conclusion
In summary, our study underscores the importance of underrepresented minority physicians in all specialties for the physician workforce needs of disadvantaged communities. To improve health care for underserved communities, continued efforts to increase physician diversity are essential.
Keywords: workforce, physicians, access, underserved
INTRODUCTION
The limited racial and ethnic diversity of the health care workforce has been implicated as a contributor to disparities in health care access and health outcomes. The Institute of Medicine concluded that producing a diverse and adequate physician supply, particularly for geographic areas with many poor, racial/ethnic minority, and uninsured residents, is one of several solutions for eliminating health disparities.1,2 In medically underserved areas, both an adequate supply of primary care physicians and greater physician racial-ethnic diversity is associated with decreased disparities in access to care.3
Minority physicians are more likely than their counterparts to work in underserved communities and care for minority, poor, and uninsured patients.4–8 However, prior studies have almost exclusively focused on African American and Latino physicians, with limited examination of Asian, Pacific Islander and other racial/ethnic minority physicians, and have tended to only focus on primary care physicians. Historically, studies of minority physicians have included only African Africans, Mexican Americans, Native Americans, and mainland Puerto Ricans. Few have investigated whether non–primary care specialists of minority backgrounds are more likely than nonminority specialists to serve the underserved. We conducted a study to examine whether physician race/ethnicity was associated with the likelihood of physicians practicing in disadvantaged communities in California, using a large statewide sample that included physicians of diverse backgrounds and specialties.
METHODS
Sample
We used data from the 2007 California Medical Board Relicensure Survey.4 The California Medical Board licenses physicians with doctor of medicine (MD) degrees and requires physicians to renew their license every 2 years and complete a brief survey questionnaire with each license renewal application. Detailed survey methods have been reported elsewhere.5 Survey response rate was 83%. We included responses from the most recent survey data available if a physician responded to the survey in different years. Respondents were included in the data set if they reported that they were active in patient care, practicing in California, and not in residency/fellowship training (N = 61 138). For this analysis, we further restricted our sample to the 48 388 physicians who reported their race, ethnicity, and specialty. We obtained institutional review board approval through University of California, San Francisco and RAND Health institutional review boards.
Main Predictors
The questionnaire asked physicians to self-identify their race and/or ethnicity from a list of 27 categories. Physicians were allowed to report more than 1 racial or ethnic category. Less than 5% of our sample reported 2 or more races. Similar to previous studies, we assigned physicians who reported more than 1 ethnicity to a single ethnic group based on the following algorithm: a physician who reported African American and another ethnicity was assigned to the African American group; a physician who reported Latino but not African American was assigned to the Latino group; and similarly for Native Americans, Asians, Pacific Islanders, and whites in that rank order.6 The survey included several categories for these overall categories. For example, our Pacific Islander category included Fijian, Filipino, Guamanian, Hawaiian, Samoan, Tongan, and other Pacific Islanders. Similarly, Asian and Latinos would provide more detailed breakdowns of their ethnicity. Completion of the item on race or ethnicity was voluntary.
Based on previous workforce studies, we collapsed responses from 51 possible specialty choices into 7 categories: primary care (family medicine, general internal medicine, general pediatrics), facility-based (anesthesiology, emergency medicine, and radiology), surgical specialties, medical subspecialties, obstetrics/gynecology, psychiatry, and other specialties. We defined specialists as physicians who were not primary care physicians.
Covariate Measures
The survey also included items on weekly hours in patient care (categorized as 1–9, 10–19, 20–29, 30–39, and ≥40 hours) and board certification (yes/no). Data on physician gender (female/male), age (categorized as <35, 35–44, 45–54, and ≥65 years), and medical school of graduation (categorized as US graduate or international medical graduate) were obtained from the California Medical Board administrative license file.
Outcome Measures
Using physician-reported zip code for their primary practice location, respondents were geocoded to a state-defined medical service study area (MSSA). MSSAs are rational service areas defined by state agencies for health workforce planning and federal designations. Consistent with prior published studies,7,9 we used 2 measures to identify MSSAs that were disadvantaged communities: medically underserved area (MUA) and primary care health professional shortage area (HPSA). These 2 categories are not mutually exclusive, with 26 out of 490 California MSSAs qualifying as a HPSA. MUAs are designated by the federal government for having a combination of health disparities and relatively low local health care resources. HPSAs are designated by the federal government based on several criteria, including having less than 1 primary care physician for every 3500 residents. We included in the HPSA categories all MSSAs that were designated as falling in a whole county of population group primary care HPSA.8
Analysis
We calculated the proportion of physicians in each racial or ethnic group practicing in each type of federally designated shortage area (HPSA and MUA). We used χ2 tests to assess statistically significant differences between groups. We then stratified the sample of physicians by specialty group and calculated the proportion of clinicians by race and ethnicity in each specialty group practicing in a HPSA or MUA.
Using multiple logistic regression models, we determined the odds of working in a HPSA or MUA for physicians in different racial/ethnic groups relative to their white counterparts. Physician age, gender, patient care hours, place of medical school graduation (US or international medical graduate, physician specialty), and board certification were included in the models as covariates. We used studies in the literature to guide our inclusion of these covariates in regression models.6–11 In a second set of regressions models, we performed a regression on each outcome (practice in a HPSA or MUA) after stratifying the sample into 2 separate specialty groupings, a primary care group and a non–primary care group, to explore possible interaction among race, ethnicity, and specialty groups broadly defined. Finally, in a sensitivity analysis, we also used multiple regressions to examine the magnitude of adjusted associations between missingness for race, ethnicity, and practice in the designated outcome measures. The analyses were performed using STATA version 10.0 (Stata Corp, College Station, Texas).
RESULTS
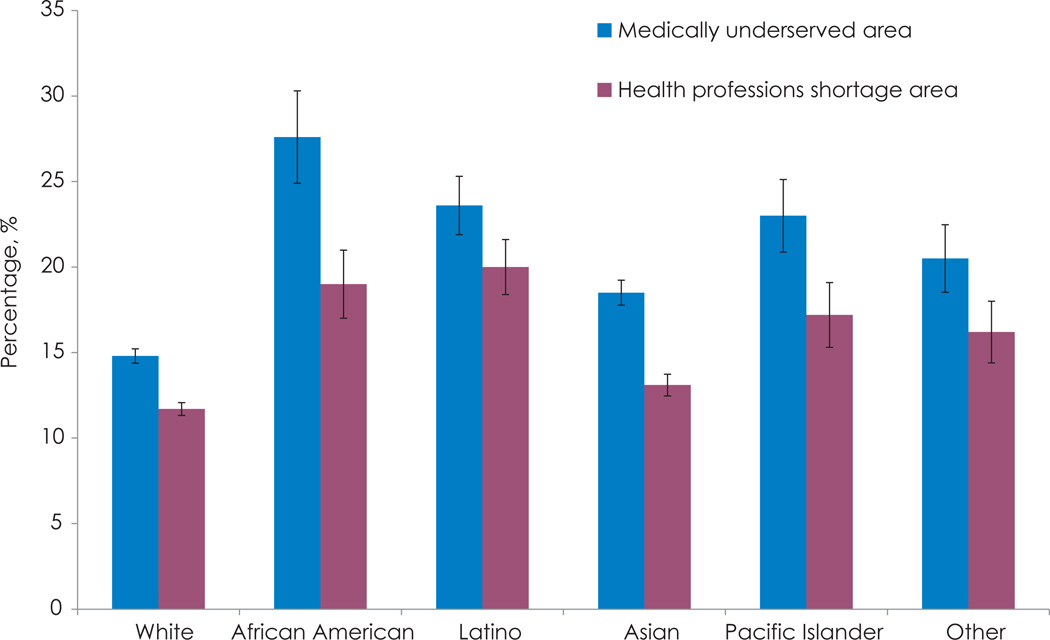
Eighty-four percent of the physicians were either white (61.6%) or Asian (23.4%), with smaller percentages of physicians from other racial/ethnic groups (Table 1). African American, Latino, Pacific Islander, and other racial/ethnic minority physicians were more likely to be in primary care specialties than were white physicians. Overall, on unadjusted analyses, a greater proportion of nonwhite physicians than white physicians worked in MUAs and HPSAs (Figure). For example, 15% of white physicians practiced in an MUA, compared with 28% of African American physicians, 24% of Latino physicians, 19% of Asian physicians, 23% of Pacific Islander physicians, and 21% of other physicians (p < .001)
Table 1.
Physician Characteristics and Practice Location Shortage Designation by Race and Ethnicity in Californiaa
| White | African American |
Latino | Asian | Pacific Islander |
Other | Total | |
|---|---|---|---|---|---|---|---|
| Total, n | 29 797 | 1555 | 2475 | 11 303 | 1585 | 1673 | 48 388 |
| Specialty, % | |||||||
| Primary careb | 29.0 | 38.1 | 46.7 | 40.9 | 54.6 | 42.6 | 34.3 |
| Medical subspecialties | 11.2 | 7.9 | 9.5 | 13.6 | 8.6 | 11.9 | 11.5 |
| Obstetrics/gynecology | 5.2 | 9.7 | 6.7 | 4.5 | 3.2 | 5.3 | 5.2 |
| Surgical specialties | 17.6 | 13.1 | 11.0 | 4.4 | 7.1 | 10.4 | 15.2 |
| Psychiatry | 8.2 | 6.4 | 6.6 | 12.1 | 9.5 | 6.0 | 7.2 |
| Facility-basedc | 10.9 | 7.8 | 6.6 | 11.2 | 7.9 | 10.4 | 10.5 |
| Other | 17.9 | 16.9 | 12.8 | 13.2 | 13.3 | 13.3 | 16.0 |
| Age, y, % | |||||||
| <35 | 2.5 | 3.3 | 4.6 | 6.7 | 3.3 | 6.0 | 3.7 |
| 35–44 | 19.6 | 25.5 | 28.9 | 35.2 | 24.5 | 29.5 | 24.4 |
| 45–54 | 28.9 | 32.9 | 35.7 | 25.6 | 30.3 | 29.3 | 28.7 |
| 55–64 | 31.0 | 24.6 | 21.4 | 22.0 | 25.0 | 24.9 | 27.8 |
| ≥65 | 18.1 | 13.6 | 9.4 | 10.4 | 16.9 | 10.3 | 15.4 |
| Gender, % | |||||||
| Male | 75.8 | 63.3 | 71.2 | 67.4 | 54.4 | 67.7 | 72.3 |
| Female | 24.2 | 36.7 | 28.8 | 32.6 | 45.6 | 32.3 | 27.8 |
| International graduate status, % | |||||||
| United States | 85.5 | 88.7 | 69.5 | 56.0 | 70.2 | 54.7 | 75.0 |
| International | 14.5 | 11.3 | 30.5 | 44.0 | 29.8 | 45.3 | 25.0 |
| Patient care hours per week, % | |||||||
| 1–9 | 7.8 | 5.4 | 3.9 | 3.8 | 3.7 | 4.3 | 6.4 |
| 10–19 | 8.6 | 7.3 | 6.2 | 5.1 | 4.6 | 5.8 | 7.4 |
| 20–29 | 13.4 | 11.1 | 11.7 | 9.6 | 8.0 | 10.1 | 12.1 |
| 30–39 | 20.2 | 19.9 | 21.6 | 20.5 | 18.6 | 19.4 | 20.2 |
| ≥40 | 50.1 | 56.3 | 56.6 | 60.9 | 65.1 | 60.4 | 54.0 |
All categories are significantly different at p < .001 using χ2 test.
Primary care = family medicine, internal medicine, and pediatrics.
Facility-based = anesthesiology, emergency medicine, and radiology.
Figure. Unadjusted Percentage of Physicians by Race in Designated California Shortage Areas.
Medically underserved area and health professional shortage area percentages represent proportion of physicians in each racial/ethnic group working in an medically underserved area or health professional shortage area.
Table 2 shows the same general trends in among each specialty group, with a lower proportion of white physicians than of physicians of other ethnicities tending to practice in a HPSA or MUA. African Americans who specialized in primary care, a medical subspecialty, obstetrics/gynecology, psychiatry, or surgery had the highest percentage of physicians practicing in MUA-designated areas compared to other racial orethnic groups in the respective specialties. African American physicians in most specialties were significantly more likely than white physicians to practice in a HPSA. Latino and Pacific Islander physicians were also more likely than white physicians in most specialty groups to practice in MUAs or HPSAs. For several of the specialty groupings, Asian physicians were also significantly more likely than white physicians to work in a MUA or HPSA.
Table 2.
Percent of Racial and Ethnic Groups by Specialty Practicing in Designated Service Areas in Californiaa
| Characteristic | Practice Location Shortage Designation | |
|---|---|---|
| Medically Underserved Area, % | Health Professional Shortage Area, % | |
| Primary careb | ||
| White | 16.5 (15.4–17.2) | 14.0 (13.2–14.7) |
| African American | 31.5 (27.8–35.3) | 21.8 (18.4–25.1) |
| Latino | 25.8 (23.3–28.3) | 24.4 (21.9–26.8) |
| Asian | 19.6 (18.5–20.8) | 14.6 (13.6–15.6) |
| Pacific Islander | 21.8 (19.1–24.6) | 16.4 (13.9–18.9) |
| Other | 22.1 (19.1–24.6) | 19.5 (16.6–22.4) |
| P value | <.001 | <.001 |
| Medical subspecialties | ||
| White | 12.7 (11.5–13.8) | 9.0 (8.1–10.0) |
| African American | 23.4 (15.9–30.9) | 17.7 (11.0–24.5) |
| Latino | 20.8 (15.6–25.9) | 13.1 (8.8–17.5) |
| Asian | 16.6 (14.7–18.4) | 11.3 (9.7–12.9) |
| Pacific Islander | 23.4 (16.2–30.5) | 15.3 (9.3–21.4) |
| Other | 16.1 (11.1–21.2) | 9.6 (5.4–13.6) |
| P value | <.001 | .001 |
| Obstetrics/gynecology | ||
| White | 13.8 (12.1–15.6) | 11.6 (10.0–13.2) |
| African American | 27.3 (20.2–34.5) | 17.3 (11.3–23.4) |
| Latino | 23.5 (17.0–30.0) | 18.1 (12.2–23.9) |
| Asian | 15.9 (12.7–19.0) | 9.4 (6.9–11.9) |
| Pacific Islander | 24.0 (12.0–36.0) | 14.0 (4.3–23.7) |
| Other | 24.7 (15.7–33.7) | 19.1 (10.9–27.3) |
| P value | <.001 | .004 |
| Psychiatry | ||
| White | 15.1 (13.7–16.6) | 10.5 (9.3–11.7) |
| African American | 32.3 (23.1–41.6) | 23.2 (14.9–31.6) |
| Latino | 28.4 (21.4–35.4) | 20.4 (14.1–26.6) |
| Asian | 24.6 (20.8–28.3) | 15.8 (12.6–19.0) |
| Pacific Islander | 26.5 (19.4–33.6) | 21.2 (14.6–27.7) |
| Other | 21.8 (13.7–29.9) | 16.8 (9.5–24.2) |
| P value | <.001 | <.001 |
| Surgery | ||
| White | 13.7 (12.7–14.6) | 10.7 (9.9–11.6) |
| African American | 26.5 (20.4–32.5) | 20.1 (14.6–25.6) |
| Latino | 18.4 (13.7–23.0) | 13.2 (9.2–17.3) |
| Asian | 16.2 (14.2–18.1) | 11.9 (10.2–13.6) |
| Pacific Islander | 23.2 (15.4–31.1) | 23.2 (15.4–31.1) |
| Other | 19.0 (13.1–24.8) | 13.2 (8.1–18.3) |
| P value | <.001 | <.001 |
| Facility-based specialtiesc | ||
| White | 15.1 (13.8–16.3) | 11.1 (10.0–12.2) |
| African American | 19.8 (12.7–27.0) | 16.5 (9.9–23.2) |
| Latino | 18.4 (12.4–24.4) | 16.0 (10.3–21.6) |
| Asian | 17.7 (15.6–19.8) | 11.9 (10.1–13.7) |
| Pacific Islander | 22.4 (15.1–29.7) | 17.6 (10.9–24.3) |
| Other | 14.4 (9.1–19.6) | 13.8 (8.7–18.9) |
| P value | .06 | .04 |
P values assessed by χ2 tests.
Primary care = family medicine, internal medicine, and pediatrics.
Facility-based = anesthesiology, emergency medicine, and radiology.
Table 3 shows the results of adjusted regression models. In model 1, after adjusting for age, gender, graduate status, board certification, specialty, and practice hours, Latinos, African Americans, Asians, Pacific Islanders, and “other” physicians were generally more likely than white physicians to work in MUAs and HPSAs (Table 3). Physicians in most of the non–primary care specialties were significantly less likely than primary care physicians to practice in an MUA or HPSA, adjusting for race, ethnicity, and the other covariates in the model. When stratified by primary care and non–primary care specialties, the same general patterns were found in the regression analyses (Table 3, models 2 and 3). Within both the primary care and non-primary care groups, a significantly greater proportion of African American, Latino, Pacific Islander, and Asian physicians than of white physicians worked in these areas. The exception to this pattern was for practice in HPSAs, where Asian and Pacific Islander primary care physicians were not significantly more likely than white primary care physicians to work in a HPSA.
Table 3.
Adjusted Odds Ratios of Physicians Practicing in California Designated Areas for all Physicians and by Medical Specialty Groups
| Practice Location | ||
|---|---|---|
| Shortage Designation | ||
| Medically Underserved Area | Health Professional Shortage Area | |
| Model 1: All Physicians | ||
| Race/ethnicity | ||
| White (Ref) | 1.0 | 1.0 |
| African American | 2.25c (2.00–2.52) | 1.78c (1.56–2.03) |
| Latino | 1.68c (1.52–1.86) | 1.75c (1.58–1.95) |
| Asian | 1.22c (1.14–1.30) | 1.06 (0.98–1.13) |
| Pacific Islander | 1.45c (1.28–1.65) | 1.33c (1.15–1.53) |
| Other | 1.36c (1.20–1.54) | 1.34c (1.16–1.53) |
| Specialty | ||
| Primary care (Ref) | 1.0 | 1.0 |
| Medical subspecialties | 0.77c (0.70–0.84) | 0.62c (0.57–0.69) |
| Obstetrics/gynecology | 0.87a (0.78–0.98) | 0.78c (0.69–0.89) |
| Surgical specialties | 0.82c (0.76–0.89) | 0.74c (0.68–0.81) |
| Psychiatry | 0.98 (0.90–1.08) | 0.80c (0.72–0.90) |
| Facility-based | 0.88c (0.80–0.95) | 0.76c (0.69–0.83) |
| Other | 0.92 (0.86–0.99) | 0.79c (0.73–0.86) |
| Model 2: Primary Care Physicians | ||
| Race/ethnicity | ||
| White (Ref) | 1.0 | 1.0 |
| African-American | 2.49c (2.07–2.99) | 1.75c (1.43–2.16) |
| Latino | 1.81c (1.56–2.09) | 1.97c (1.70–2.29) |
| Asian | 1.22c (1.10–1.35) | 1.00 (0.90–1.12) |
| Pacific Islander | 1.31b (1.09–1.56) | 1.09 (0.89–1.33) |
| Other | 1.39b (1.16–1.69) | 1.40b (1.14–1.71) |
| Model 3: Specialists Physicians | ||
| Race/ethnicity | ||
| White (Ref) | 1.0 | 1.0 |
| African-American | 2.10c (1.81–2.44) | 1.81c (1.52–2.16) |
| Latino | 1.57c (1.37–1.81) | 1.52c (1.30–1.78) |
| Asian | 1.20c (1.11–1.30) | 1.09 (0.99–1.19) |
| Pacific Islander | 1.68c (1.40–2.01) | 1.67c (1.37–2.05) |
| Other | 1.32c (1.12–1.57) | 1.27a (1.05–1.53) |
Excluding those with missing race or specialty did not change the main results; however, those in MUAs were less likely to report race (p < .05) than those in other areas as well as those who were older, male, noninternational medical graduates, board certified, and in non–primary care specialties. Those missing specialty designation were more likely to be in a HPSA and were also more likely to be older, male, white, board certified, a noninternational medical graduate, and work more hours (p < .05) than their counterparts.
DISCUSSION
Through comparing practice locations among physicians with a wide range of specialties and racial or ethnic groups, we found that physicians from groups historically underrepresented in medicine, including African Americans, Latinos, and Pacific Islanders, are significantly more likely than their white counterparts to practice in underserved communities in California. By demonstrating that physicians in almost all specialties who are African American or Latino are more likely than non-Latino whites to practice in disadvantaged communities, our study extends findings from previous research on physician race, ethnicity, and practice location that, with rare exceptions, only included primary care physicians.4–8 Our study indicates that physicians in all specialties from racial and ethnic groups underrepresented in medicine tend to be significantly more likely than white physicians in the respective specialties to practice in underserved communities.
Using a larger physician sample than prior studies, we also have been able to examine some racial and ethnic groups often not systematically assessed in prior research. In particular, Pacific Islanders and other less-populous racial and ethnic groups have been largely unexamined in prior studies due to small sample sizes and inadequate statistical power. In analyses stratified by specialty, Asian physicians were also more likely than white physicians to practice in underserved areas. The current definition of underrepresented in medicine from the Association of American Medical Colleges states “Underrepresented in medicine means those racial and ethnic populations that are underrepresented in the medical profession relative to their numbers in the general population.”10 Pacific Islanders are not historically underrepresented nor explicitly stated in the current definition, yet they are considered an underrepresented minority group in California and many other states. Our findings are particularly revealing for this group and emphasize the role of Pacific Islanders in serving disadvantaged areas.
We also were able to use 2 commonly used definitions of underserved areas. Using both HPSA and MUA in our analysis underscores that these 2 definitions capture different types of areas with differing physician supply characteristics. Although these definitions are based on primary care supply, specialty supply is intrinsically linked to populations needs and health care demands. These findings underscore the importance of the ongoing federal debate on how to define and categorize underserved and shortage areas.11
Our study has several strengths, including the large sample size, detailed information on physicians’ race and/or ethnicity, and more reliable data on patient care hours and practice zip code than that available from national physician databases, including the American Medical Association Masterfile. Our study also has several limitations. First, using cross-sectional survey data from California allows us to only analyze one state’s patterns. Although this state-level data set has strengths as noted above, our findings may not be generalizable to other states. Secondly, we do not have information available regarding number of practice locations, federal or state loan obligation requirements, or practice at federally qualified health centers, which may influence work in an underserved area. Furthermore, some specialists, such as those that are facility-based, are likely to practice at hospitals that are not often located in disadvantaged communities. Finally, although the response rate of the survey is much higher than that for most physician surveys, there may be potential nonresponse bias from the physicians who did not complete the survey.
From a policy perspective, many organizations argue that the United States needs more physicians from ethnic groups underrepresented in medicine.1,14 In California, Latinos are one-third of the state’s population but comprise only 5.2% of the state’s physicians.10 African Americans are 6.7% of the state’s population but comprise only 3.2% of California’s physicians. Our results suggest that increasing the diversity of the physician workforce would preferentially improve physician supply and patient access in disadvantaged communities. Minority health professionals have been shown to be an important part of health care delivery for the underserved, including those from low socioeconomic backgrounds or in the National Health Service Corps.12
Moreover, our study shows that this implication holds not just for primary care physicians, but for underrepresented minorities in most specialties. Promoting greater diversity in the physician workforce across specialties is an important strategy for improving access, enhancing culturally and linguistically competent care, and eliminating health disparities. Studies have shown that doctor-patient racial concordance may increase patient participatory decision making,13 communication,14 and patient satisfaction,15 although some controversy exists as to whether these benefits of racial concordance translate into better health outcomes for minorities.16,17 In addition, one study found that minority patients choose physicians due to preference and language, not simply due to geographic accessibility.18
The Sullivan Alliance and Institute of Medicine have released comprehensive recommendations to promote increased health professions diversity.2,19 These recommendations include increased investment in educational health career pipeline programs for minority and disadvantaged students, such as the federally funded Centers of Excellence and Health Careers Opportunity Programs, establishing enforceable accreditation standards that promote diversity, and strengthening institutional commitment to student and faculty diversity at medical schools. These reports have also called attention to the critical role of historically black colleges and universities and other minority serving institutions in recruiting and training underrepresented minority health professionals.
CONCLUSION
In summary, our study underscores the importance of underrepresented minority physicians in all specialties for the physician workforce needs of disadvantaged communities. Increasing the diversity of the physician workforce should be an essential component of a national physician workforce strategy to improve health care for underserved communities and eliminate health care disparities.
Acknowledgments
Funding/Support: Drs Walker and Moreno were funded by the Robert Wood Johnson Foundation Clinical Scholars Program at the University of California, Los Angeles.
Financial Disclosure: Dr Walker received support from the University of California, Los Angeles Resource Center for Minority Aging Research/Center for Health Improvement of Minority Elderly under National Institutes of Health/National Institute on Aging grant P30AG021684.
Footnotes
Previous Presentation: Preliminary results of this work were presented at the American Association of Medical Colleges Annual Workforce Meeting in May 2009.
REFERENCES
- 1.Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; Institute of Medicine; 2002. [Google Scholar]
- 2.In the Nation’s Compelling Interest: Ensuring Diversity in the Nation’s Healthcare Workforce. Washington, DC: National Academy Press; Institute of Medicine; 2004. [PubMed] [Google Scholar]
- 3.Laditka J. Physician Supply, physician diversity, and outcomes of primary healthcare for older persons in the United States. Health Place. 2004;10(3):231–244. doi: 10.1016/j.healthplace.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Grumbach K, Odom K, Moreno G, et al. California Physician Diversity: New Findings from the California Medical Board Survey. UCSF Center for California Health Workforce Studies. 2008 Apr [Google Scholar]
- 5.Grumbach K, Chattopadhyah A, Bindman AB. Fewer and More specialized; A New Assessment of Physician Supply in California. [Accessed February 1, 2010];2009 Jun; www.chcf.org/documents/policy/FewerAndMoreSpecializedMDSupplyInCA.pdf. [Google Scholar]
- 6.Mertz E, Jain R, Breckler J, et al. Foreign versus domestic education of physicians for the United States: a case study of physicians of South Asian ethnicity in California. J Health Care Poor Underserved. 2007;18(4):984–993. doi: 10.1353/hpu.2007.0100. [DOI] [PubMed] [Google Scholar]
- 7.Ko M, Heslin KC, Edelstein RA, et al. The role of medical education in reducing healthcare disparities: the first ten years of the UCLA/Drew Medical Education Program. J Gen Intern Med. 2007;22(5):625–631. doi: 10.1007/s11606-007-0154-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Health Resources and Services Administration (HRSA), US Department of Health and Human Services. [Accessed October 18, 2010]; http://bhpr.hrsa.gov/shortage/index.htm.
- 9.Singer JD, Davidson SM, Graham S, et al. Physician retention in community and migrant health centers: who stays and for how long? Med Care. 1998;36(8):1198–1213. doi: 10.1097/00005650-199808000-00008. [DOI] [PubMed] [Google Scholar]
- 10.AAMC. Underrepresented in Medicine Definition. [Accessed February 10, 2010]; www.aamc.org/meded/urm/start.htm. [Google Scholar]
- 11.US Department of Health and Human Services. Negotiated Rulemaking Committee on Designation of MUPs and HPSAs. [Accessed July 14, 2011]; www.hrsa.gov/advisory-committees/shortage/index.html.
- 12.Saha S, Shipman S. Race-Neutral Versus Race-Conscious Workforce Policy To Improve Access To Care. Health Affairs. 2008;27(1):234–245. doi: 10.1377/hlthaff.27.1.234. [DOI] [PubMed] [Google Scholar]
- 13.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender and partnership in the patient-physician relationship. JAMA. 1999;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 14.Cooper LA, Roter DL, Johnson RL, et al. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 15.LaViest TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43(3):296–306. [PubMed] [Google Scholar]
- 16.Meghani SH, Brooks JM, Gipson-Jones T, et al. Patient-provider race-concordance: does it matter in improving minority patients’ health outcomes? Ethn Health. 2009;14(1):107–130. doi: 10.1080/13557850802227031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Konrad TR, Howard DL, Edwards LJ, et al. Physician-patient racial concordance, continuity of care and patterns of care for hypertension. Am J Public Health. 2005;95(12):2186–2190. doi: 10.2105/AJPH.2004.046177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saha S, Taggart SH, Komaromy M, et al. Do patients choose physicians of their own race? Health Aff. 2000;19(4):76–83. doi: 10.1377/hlthaff.19.4.76. [DOI] [PubMed] [Google Scholar]
- 19.Sullivan LW, Suez Mittman I. The State of Diversity in the Health Professions a Century after Flexner. Acad Med. 2010;85(2):246–253. doi: 10.1097/ACM.0b013e3181c88145. [DOI] [PubMed] [Google Scholar]