Abstract
BACKGROUND
There is a paucity of data describing the sustained benefits of lifestyle interventions on health behaviors and blood pressure (BP).
METHODS
We examined the persistence of changes in health habits and BP in the ENCORE study, a trial in which 144 overweight individuals with above-normal BP were randomized to one of the following 16-week interventions: Dietary Approaches to Stop Hypertension (DASH) diet alone (DASH-A), DASH diet plus a behavioral weight management intervention (DASH-WM), or Usual Care. Follow-up assessments were conducted 8 months after the end of treatment.
RESULTS
At 16 weeks, systolic BP was reduced by 16.1 (95% confidence interval (CI) = 13.0–19.2) mm Hg in the DASH-WM group, 11.2 (95% CI = 8.1–14.3) mm Hg in the DASH-A group, and 3.4 (95% CI = 0.4–6.4) mm Hg in the Usual Care group. A decrease in BP persisted for 8 months, with systolic BP lower than baseline by 11.7 (95% CI = 8.1–15.3) mm Hg in the DASH-WM group, 9.5 (95% CI = 6.7–12.1) mm Hg in the DASH-A group, and 3.9 (95% CI = 0.5–7.3) mm Hg in the Usual Care group (P < 0.001 for active treatments vs. Usual Care). DASH-WM subjects lost 8.7kg during the intervention and remained 6.3kg lighter on follow-up examination. Changes in diet content were sustained in both DASH intervention groups. Among those who participated in DASH-WM, however, caloric intake was no longer lower, and only 21% reported still exercising regularly 8 months after completing the intervention.
CONCLUSIONS
Changes in dietary habits, weight, and BP persisted for 8 months after completion of the 16-week ENCORE program, with some attenuation of the benefits. Additional research is needed to identify effective methods to promote long-term maintenance of the benefits of lifestyle modification programs.
CLINICAL TRIAL REGISTRATION
Clinicaltrials.gov identifier: NCT00571844.
Keywords: blood pressure, DASH diet, exercise, hypertension
Lifestyle modifications are recommended as the initial treatment for high blood pressure (BP).1–3 Randomized, controlled trials have demonstrated that the Dietary Approaches to Stop Hypertension (DASH) diet, weight loss, and exercise are effective in lowering BP in the short term.4–8 However, there is a paucity of data describing the persistence of the effects of short-term interventions on health behaviors and BP. We recently reported results of a trial demonstrating that a 16-week lifestyle modification program emphasizing the DASH diet alone or in combination with a weight management intervention resulted in significant BP lowering and improved cardiovascular biomarkers.4 In this paper, we examine the persistence of changes in dietary habits, exercise behaviors, body weight, and BP 1 year after study enrollment.
METHODS
Subjects
Participants were 144 healthy but overweight men and women with above-normal BP who were not treated with antihypertensive medications. Persons were eligible if they were aged >35 years, had a body mass index of 25–39.9kg/m2, were sedentary, and had a BP of 130–160/80–99mm Hg. Exclusion criteria included clinical or laboratory evidence of cardiac disease, chronic kidney disease, or diabetes.
Design
Details of the ENCORE (Exercise and Nutrition Interventions for Cardiovascular Health) study protocol have been described previously.4 The study was approved by the institutional review board at Duke University Medical Center, and written informed consent was obtained from each subject before participation.
Participants were recruited from physician referrals, community-based screenings, and advertisements. Eligibility was established during a series of screening visits that included a history and physical examination, measurement of height and weight, assessment of dietary content, and determination of baseline BP. Participants were then randomized with equal probability to 1 of the following 16-week treatment conditions: (i) DASH diet alone (DASH-A); (ii) DASH diet plus behavioral weight management (DASH-WM); or (iii) Usual Care. Measurements of weight, dietary content, and BP were repeated at the conclusion of the intervention. None of the treatment conditions included a maintenance phase, although DASH-A and Usual Care subjects were provided information about behavioral strategies to lose weight. Participants returned for a follow-up visit 1 year after enrollment (8 months after completion of the intervention), at which time BP, weight, dietary content, exercise habits, antihypertensive medications, and cardiovascular events were assessed.
Measurements
BP was measured by a trained examiner blinded to the study group assignment using a mercury sphygmomanometer and adhering to the guidelines for proper BP measurement technique described in the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.1 After the participant rested for 5 minutes in the seated position, 4 readings were acquired, each 2 minutes apart, and the results were averaged. Measurements were acquired on 4 screening sessions over a 3–4-week period for baseline values, on 4 visits to the research clinic during the final week of the intervention phase, and on a single follow-up visit 8 months after completion of the intervention.
Body weight was measured in kilograms using a calibrated digital scale. Dietary intake patterns were assessed using a 4-day food diary,9 and data were analyzed using Food Processor SQL Edition software, version 10.3 (ESHA Research, Salem, OR). Physical activity was determined on the follow-up visit by self-report; adherence to a program of regular exercise was defined as exercise ≥3 times a week at an intensity of ≥4 on a scale of 1–5. Medication use and interval history of cardiovascular events were assessed by questionnaire.
Interventions
After randomization, participants entered a 2-week controlled feeding period during which they were provided meals according to their assigned dietary patterns (DASH diet, reduced calorie DASH diet, or control diet). Additional details of the study diets are described in a previous publication.4 After the initial 2 weeks of controlled feeding, participants were instructed to maintain the DASH diet either with (DASH-WM) or without (DASH-A) weight loss.
DASH diet alone.
Participants in the DASH-A condition met weekly with the study nutritionist in small group sessions to discuss the DASH diet and receive feedback on their adherence to the diet. The goal of the weekly sessions was to assist participants in learning how to buy and prepare the appropriate foods, to enhance their motivation to choose to eat those foods, and to overcome obstacles to following the diet.
DASH plus weight management.
Participants in the DASH-WM condition received the same instruction in the DASH diet as the DASH-A group, but their small group sessions also included a weekly cognitive behavioral weight loss intervention and supervised exercise sessions 3 times per week. The cognitive behavioral weight loss intervention was based on cognitive behavioral strategies10 and included appetite awareness training, a self-monitoring strategy in which individuals learn to identify internal cues of moderate hunger and fullness and to use these cues to guide their eating behavior.11 The supervised exercise routine consisted of 10 minutes of warm-up exercises, 30 minutes of biking and/or walking or jogging at 70%–85% of the initial heart rate reserve, and 5 minutes of cool-down exercises.
Usual Care control subjects.
Participants in the Usual Care condition were asked to maintain their usual dietary and exercise habits for the 4 months of the intervention.
Statistical analysis
We examined treatment group differences on systolic BP, diastolic BP, and weight 1 year after study entry (8 months after the intervention ended) using an intent-to-treat analysis with mixed repeated measures models with SAS PROC MIXED (SAS version 9.2; SAS, Cary, NC). The BP outcomes measured at 16 weeks and 1 year were modeled as discrete repeated measures (with the post-treatment measurement occasions specified as a class variable and used in the REPEATED statement in PROC MIXED); predictors included the corresponding baseline BP, age, sex, ethnicity, time, treatment group, body weight at baseline, and a time by treatment group interaction term. The weight outcome was modeled in similar fashion, using 16-week and 1-year weight as repeated measures, with age, sex, ethnicity, time, treatment group, weight at baseline, and a time by treatment group interaction term as predictors. Continuous variables were centered at their medians, with time coded in reverse such that 1 year = 0. The contrasts of primary interest were (i) active treatments (DASH-A and DASH-WL) vs. Usual Care and (ii) DASH-WL vs. DASH-A, each evaluated at the 1-year measurement occasion. Because subjects in the Usual Care and DASH-A groups were asked to maintain their weight during the 16-week intervention, for the weight outcome, we used contrasts that compared DASH-WM to DASH-A and Usual Care and also DASH-A and Usual Care to each other. An important advantage of mixed models is that all randomized participants can be included in the analysis irrespective of missing data on post-treatment assessments. Mixed models have been shown to produce treatment effect estimates that are less biased and have narrower confidence intervals compared with conventional case-wise deletion or last-observation-carried-forward analyses.12 Thus, the analyses described above included the entire initial cohort of 144 participants. BP and body weight data were available for 140 participants at the 16-week measurement occasion (46 in DASH-WM, 46 in DASH-A, and 48 in Usual Care) and 124 participants at the 1-year assessment (42 in DASH-WM, 41 in DASH-A, and 41 in Usual Care). Models were estimated using restricted maximum likelihood. The variance components structure was found to be a reasonable assumption for the covariance matrix. Assumptions were evaluated for all models and found to be reasonably met.
Group differences in dietary component intake at 1 year were evaluated using the general linear model, again with models adjusted for age, sex, ethnicity, and the baseline measure for the relevant outcome variable. Binary exercise and medication variables at 1 year were analyzed using logistic regression. As with the primary analyses, contrasts were constructed based on the a priori expectation for a given outcome variable. In these latter analyses, only participants with complete data were included.
RESULTS
Participants
After screening, 144 participants were randomized: 46 to the DASH-A group, 49 to the DASH-WM condition, and 49 to Usual Care. Only 4 subjects (3 from DASH-WM and 1 from Usual Care) withdrew during the intervention phase. Sixteen additional subjects (5 from DASH-A, 4 from DASH-WM, and 7 from Usual Care) did not return for the follow-up evaluation at 1 year (Figure 1). Compared with those who had complete weight and BP data, subjects who dropped out at either 16 weeks or 1 year tended to be younger (mean age = 48 vs. 53 years; P= 0.02), but did not differ statistically on BP, baseline weight, weight lost during the intervention, sex, or ethnicity.
Figure 1.
Patient flow from initial screening to 1-year follow-up. Abbreviations: DASH-A, Dietary Approaches to Stop Hypertension (DASH) diet alone; DASH-WM, DASH diet plus behavioral weight management.
Characteristics of the 144 participants enrolled in the trial are shown in Table 1. They were primarily middle aged (mean age = 52 (SD = 10) years), white (60%), and female (67%) and had an average body mass index of 33.1 (SD = 3.9) kg/m2. The mean clinic BP was 138 (SD = 9)/86 (SD = 6) mm Hg. The groups were comparable across the background demographic and clinical variables (Table 1).
Table 1.
Baseline characteristics of sample
| Characteristic | No. | DASH-WM (n = 49) | DASH-A (n = 46) | Usual Care (n = 49) | All (n = 144) |
|---|---|---|---|---|---|
| Age, y | 144 | 52.3 (10) | 51.8 (10) | 51.8 (9) | 52.0 (10) |
| Sex: female | 144 | 69% (34) | 63% (29) | 69% (34) | 67% (97) |
| Ethnicity | 144 | ||||
| White | 69% (34) | 50% (23) | 59% (29) | 60% (56) | |
| Black | 31% (15) | 48% (22) | 39% (19) | 39% (86) | |
| Asian | 0% (0) | 2% (1) | 2% (1) | 1% (2) | |
| Hispanic | 144 | 4% (2) | 0% (0) | 6% (3) | 3% (5) |
| Level of education | 143 | ||||
| High school | 31% (15) | 30% (14) | 42% (20) | 34% (49) | |
| Some college | 8% (4) | 9% (4) | 14% (7) | 11% (15) | |
| Completed college | 29% (14) | 30% (14) | 18% (9) | 22% (32) | |
| Graduate school | 20% (10) | 28% (13) | 20% (10) | 24% (34) | |
| Other | 12% (6) | 13% (6) | 2% (1) | 9% (13) | |
| Household income per year | 123 | ||||
| < $20,000 | 10% (5) | 13% (6) | 20% (10) | 15% (21) | |
| $20,000–$49,999 | 14% (7) | 4% (2) | 8% (4) | 11% (13) | |
| $50,000–$99,999 | 6% (3) | 13% (6) | 18% (9) | 15% (18) | |
| >$100,000 | 55% (27) | 50% (23) | 43% (21) | 49% (71) | |
| Weight, kg | 144 | 93.9(14) | 93.0 (14) | 92.6 (15) | 93.1 (14.1) |
| BMI, kg/m2 | 144 | 33.5 (4.4) | 32.8 (3.4) | 33.0 (3.9) | 33.1 (3.9) |
| Peak VO2 | 142 | 23.4 (6.2) | 23.8 (6.5) | 23.2 (5.8) | 23.4 (6.2) |
| Systolic BP, mm Hg | 144 | 139 (8) | 138 (9) | 138 (9) | 138 (9) |
| Diastolic BP, mm Hg | 144 | 85 (7) | 86 (6) | 86 (6) | 86 (6) |
| Current smoker | 144 | 4% (2) | 7% (3) | 10% (5) | 7% (10) |
| Diabetes | 144 | 2% (1) | 0% (0) | 0% (0) | <1% (1) |
| Hyperlipidemia | 144 | 33% (16) | 22% (10) | 33% (16) | 29% (42) |
Values are mean (SD) for continuous variables and % (No.) for categorical variables.
Abbreviations: BMI, body mass index; BP, blood pressure; DASH-A, Dietary Approaches to Stop Hypertension (DASH) diet alone; DASH-WM, DASH diet plus behavioral weight management; VO2, exercise oxygen consumption.
Weight, DASH dietary components, aerobic fitness, and blood pressure at 16 weeks
As previously reported,4 participants in DASH-WM lost 8.7kg during the treatment period compared with a loss of 0.3kg in DASH-A (P < 0.001) and a gain of 0.9kg in Usual Care (P < 0.001). Daily dietary sodium intake was lower, and consumption of potassium, magnesium, and calcium was greater in DASH-A and DASH-WM than in Usual Care at 16 weeks (Ps < 0.001). BP was reduced in the DASH-WM group by 16.1 (95% confidence interval (CI) = 13.0–19.2)/9.9 (95% CI = 8.1–11.6) mm Hg, compared with 11.2 (95% CI = 8.1–14.3)/7.5 (95% CI = 5.8–9.3) mm Hg in DASH-A and 3.4 (95% CI = 0.4–6.4)/3.8 (95% CI = 2.2–5.5) mm Hg in Usual Care. Contrasts between all active treatments and Usual Care were statistically significant for both systolic BP and diastolic BP (Ps < 0.001); similarly, the contrast between DASH-WM and DASH-A was statistically significant for both systolic BP (P = 0.01) and diastolic BP (P = 0.03).
Weight, DASH dietary components, exercise behaviors, and medication use at 1 year
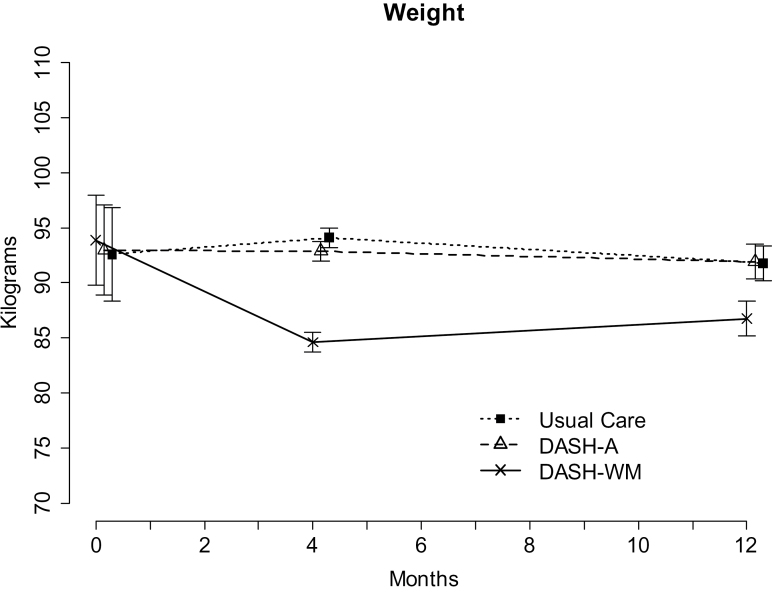
Figure 2 displays the adjusted mean weight and 95% CI for each group at the 3 time points. Participants’ average body weight at 1 year was 86.7kg in DASH-WM, 91.9kg in DASH-A, and 91.8kg in Usual Care (Ps = 0.001 for DASH-WM compared with either DASH-A or Usual Care after adjusting for baseline weight and demographic characteristics). Those in the DASH-WM group were 6.3kg lighter than at baseline (2.4kg heavier than at 16 weeks), whereas sustained weight loss averaged 1.5kg in DASH-A and 1.6kg in Usual Care.
Figure 2.
Mean weight in kilograms for each treatment group before and after 16 weeks of treatment and 1 year after study entry. Baseline values are adjusted for age, race, and sex. Values for 4 and 12 months are derived from the mixed model and are adjusted for age, race, sex, and baseline body weight. Error bars represent 95% confidence intervals. The narrow confidence intervals for the 4 and 12 month values reflect the adjustment of these values for baseline body weight. Abbreviations: DASH-A, Dietary Approaches to Stop Hypertension (DASH) diet alone; DASH-WM, DASH diet plus behavioral weight management.
Levels of nutrient and caloric intake, self-reported exercise frequency, and medication use at 1 year are shown in Table 2. Consumption of sodium was lower, and dietary intake of potassium, calcium, and magnesium was greater in the 2 DASH groups compared with the Usual Care group. There were no significant differences in daily caloric intake between participants in DASH-WM and the other 2 groups. Self-reported intake in the DASH-WM group increased by about 150 calories between completion of the intervention and the follow-up visit.
Table 2.
Self-reported dietary intake, exercise habits, and medication after 1 year
| Variable | DASH-WM (n = 40) | DASH-A (n = 36) | Usual Care (n = 37) | All (n= 113) | Contrast | |
|---|---|---|---|---|---|---|
| Treatment vs. Usual Care | DASH-WM vs. DASH-A | |||||
| Sodium, mg/d | 2,324 (712) | 2,031 (1,126) | 2,803 (849) | 2,436 (1,132) | 0.002 | 0.107 |
| Potassium, mg/d | 3,069 (1,211) | 3,217 (1,834) | 2,702 (1,144) | 2,953 (1,307) | <0.001 | 0.481 |
| Calcium, mg/d | 906 (450) | 937 (380) | 828 (431) | 902 (442) | 0.041 | 0.438 |
| Magnesium, mg/d | 362 (155) | 337 (210) | 299 (130) | 317 (151) | <0.001 | 0.598 |
| BP medication | 12% (5) | 12% (5) | 15% (6) | 13% (16) | 0.968 | 0.687 |
| DASH-WM vs DASH-A | DASH-WM vs Usual Care | |||||
| Total calories, kcal/d | 1,806 (550) | 1,772 (653) | 1,873 (669) | 1,810 (652) | 0.498 | 0.569 |
| Exercising ≥ 3×/week | 21% (9) | 22% (9) | 7% (3) | 17% (21) | 0.954 | 0.242 |
Values are mean (SD) for continuous variables and (%) No. for categorical variables.
Abbreviations: BP, blood pressure; DASH-A, Dietary Approaches to Stop Hypertension (DASH) diet alone; DASH-WM, DASH diet plus behavioral weight management.
At follow-up only about 1 in 5 subjects who had completed the DASH-WM intervention, which emphasized physical activity and weight loss, reported still exercising ≥3 times weekly. Only 16 patients (13%)—5 (12%) in DASH-WM, 5 (13%) in DASH-A, and 6 (16%) in Usual Care—were prescribed antihypertensive medications 1 year after study enrollment. No subjects experienced adverse cardiovascular events over the year of observation.
Blood pressure at 1 year
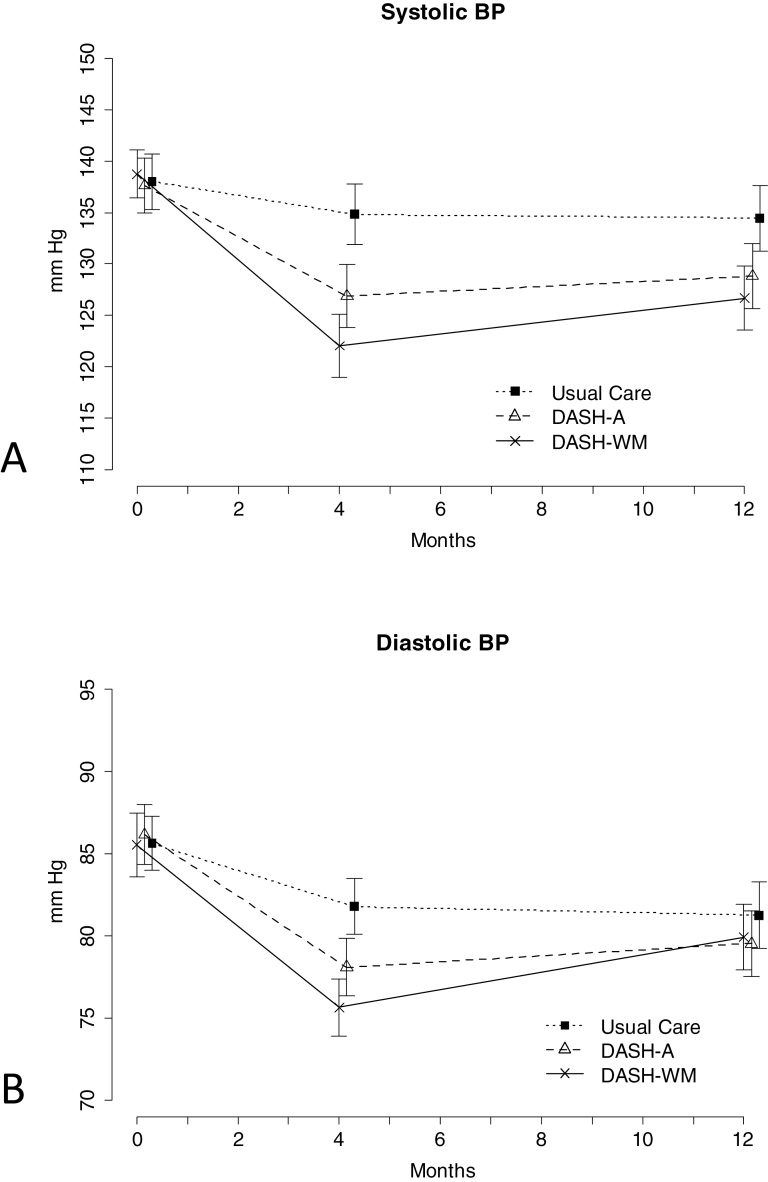
Systolic BP at 1 year was significantly lower in participants in the active treatment groups compared with those randomized to Usual Care (difference = −6.7mm Hg; 95% CI = −10.6 to −2.9; P < 0.001) (Figure 3a), with no significant difference between DASH-WM and DASH-A participants (difference = −2.2mm Hg; 95% CI = −.6.7 to 2.3; P = 0.33). The adjusted 1-year means derived from the mixed model were 126.6 (95% CI = 123.5–129.8) mm Hg in DASH-WM, 128.9 (95% CI = 125.7–132.0) mm Hg in DASH-A, and 134.5 (95% CI = 131.3–137.6) mm Hg in Usual Care. Examining change at 1 year compared with baseline, systolic BP was reduced 11.7 (95% CI = 8.1–15.3) mm Hg in the DASH-WM, 9.5 (95% CI = 6.7–12.1) mm Hg in DASH-A, and 3.9 (95% CI = 0.5–7.3) mm Hg in Usual Care. In the mixed model for diastolic BP the groups did not differ at 1 year (Figure 3b). Reanalyzing the data excluding the 16 patients who were prescribed antihypertensive medication after randomization did not alter the conclusions regarding the treatment effect at 1 year for either systolic BP or diastolic BP.
Figure 3.
Mean (a) systolic and (b) diastolic BP for each treatment group before and after 16 weeks of treatment and 1 year after study entry. Baseline values are adjusted for age, race, and sex. Values for 4 and 12 months are derived from the mixed model and are adjusted for age, race, sex, baseline body weight, and baseline BP. Error bars represent 95% confidence intervals. Abbreviations: BP, blood pressure; DASH-A, Dietary Approaches to Stop Hypertension (DASH) diet alone; DASH-WM, DASH diet plus behavioral weight management.
DISCUSSION
In our study of overweight, sedentary men and women with high BP, a structured, 16-week lifestyle intervention, consisting of the DASH diet with or without a weight loss and exercise component, resulted in significant decreases in BP compared with a Usual Care control group. In both DASH diet conditions, a lower systolic BP persisted for 8 months. There was, however, some attenuation of the weight loss and BP benefits of the DASH-WM intervention during the follow-up period. The attenuation of weight loss was likely due to both small increases in caloric intake and decreased energy expenditure. Changes in dietary content were sustained in both DASH groups. However, among those who participated in the weight management condition, caloric intake was no longer lower and only about 20% reported still exercising regularly 8 months after completing the intervention.
Although there is substantial evidence documenting the efficacy of the DASH diet, weight loss, and exercise in lowering BP, there is little information on the persistence of benefits of life-style interventions on BP. Several studies have examined the sustained effects of weight loss and diet interventions that have included a prolonged maintenance phase. The Trials of Hypertension Prevention (TOHP) II tested interventions to promote weight loss, dietary sodium reduction, and their combination in untreated, overweight adults with high-normal BP over a 3- to 4-year period.13,14 Over the 6 months of the initial intensive intervention, the weight loss and combined groups experienced losses of more than 4kg, and the estimated main effect of the sodium intervention was a reduction of 48 mmol/day. These changes were associated with BP reductions of 2.4/2.0mm Hg attributable to weight loss and 1.6/0.8mm Hg for sodium reduction. Between 6 and 36 months, the net changes in sodium excretion, weight, and BP diminished by about one-fourth for sodium excretion, one-half for weight, and two-thirds for BP. Trial of Nonpharmacologic Interventions in the Elderly (TONE) was a 4-center randomized trial to test whether weight loss, reduced sodium intake, or both could maintain BP control after withdrawal of antihypertensive drug therapy.15,16 At a median of 8 months after discontinuation of the intervention, weight loss from baseline remained somewhat greater (−3.9kg) in the weight intervention group than in the group not assigned to weight loss (−2.2kg), but this difference was no longer statistically significant. In contrast, significant differences in 24-hour urine sodium excretion persisted throughout the extended follow-up. There was a long-term effect of the intervention on blood pressure; 48 months after discontinuation of contact between participants and the clinical center, 23% of the combined intervention group vs. 7% in the Usual Care group remained off medication. The weight loss results from the TOHP and TONE trials reflect outcomes from other high-intensity counseling studies—a reduction in body weight may persist for up to 72 months but is significantly attenuated.17–21 As in our study, desirable changes in dietary content in TOHP and in TONE were more persistent than weight loss.
Exercise was an important component of our DASH diet and weight management intervention. Although adherence with the 16-week exercise program was high, 8 months later only 21% of subjects were engaging in high-intensity aerobic physical activity ≥3 times per week. In general, short-term trials examining the effects of exercise on BP have demonstrated more marked reductions than longer-term studies, perhaps reflecting better adherence to the exercise intervention in the short-term studies, many of which included supervised exercise programs.22 Decreased adherence to an exercise intervention over time has also been demonstrated in individual trials.23 Adherence to a program of regular physical activity may be key to the long-term persistence of weight loss and the associated lower blood pressure after completion of a lifestyle invention program.24–27
The main limitation of this follow-up study is the lack of 1-year data for 20 of the 144 subjects who enrolled in the trial. The duration of follow-up was relatively short, and longer-term data would be valuable in assessing the persistence of benefits from our lifestyle intervention. Patterns of dietary intake were assessed by a 4-day food diary, a method that is well-validated but nonetheless prone to some bias.28 Similarly, physical activity can be difficult to measure by self-report because of the episodic nature of recreational exercise and the subjectivity of assessments of exercise intensity. Our research was conducted in well-educated and highly motivated individuals who volunteered for a clinical study, and the results may not be generalizable to all obese, sedentary individuals with high BP.
Our analysis demonstrated that a clinically meaningful reduction in BP persisted for 8 months after completion of structured lifestyle intervention programs emphasizing the DASH diet, with some attenuation of the BP and weight loss benefits in the group with an exercise and weight management component. The greater difficulty experienced by our subjects in maintaining lower caloric intake than in maintaining changes in food type suggests that weight loss interventions need to focus even more on ways to prevent the gradual upward drift to pretreatment levels of energy consumption. Changes in the types of food regularly consumed may be more obvious to patients than relatively small increments in quantity and may reflect the development of preferences for healthier foods. Future studies may need to place greater emphasis on specific strategies to enhance feelings of satiety so that patients are better able to maintain the reductions in calorie intake that they achieve during a weight loss intervention. Furthermore, development of strategies to promptly identify patients who are not maintaining lifestyle changes, including regular physical activity, may be useful; these individuals may need tailored help in getting back on track. The use of personal digital devices can be effective in promoting lifestyle change, and mobile technology may prove particularly useful in promoting the maintenance of healthy exercise and dietary habits over time when the accountability and support provided by an active intervention is no longer available.29
DISCLOSURES
The authors declared no conflict of interest.
ACKNOWLEDGMENTS
This work was supported by grants from the National Heart, Lung, and Blood Institute (HL074103); the General Clinical Research Center, National Institutes of Health (M01-RR-30); and the National Center of Research Resources (5UL1RR024128-03).
REFERENCES
- 1. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ, National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, National High Blood Pressure Education Program Coordinating Committee The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572 [DOI] [PubMed] [Google Scholar]
- 2. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O’Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B, Management of Arterial Hypertension of the European Society of Hypertension, European Society of Cardiology 2007 guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25:1105–1187 [DOI] [PubMed] [Google Scholar]
- 3. National Institute for Health and Care Excellence Hypertension: management of primary hypertension in adults. www.nice.org.uk/guideline/CG127
- 4. Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin PH, Caccia C, Johnson J, Waugh R, Sherwood A. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Arch Intern Med 2010; 170:126–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 1997; 336:1117–1124 [DOI] [PubMed] [Google Scholar]
- 6. Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin PH, Svetkey LP, Stedman SW, Young DR, Writing Group of the PREMIER Collaborative Research Group Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 2003; 289:2083–2093 [DOI] [PubMed] [Google Scholar]
- 7. Blumenthal JA, Sherwood A, Gullette EC, Babyak M, Waugh R, Georgiades A, Craighead LW, Tweedy D, Feinglos M, Appelbaum M, Hayano J, Hinderliter A. Exercise and weight loss reduce blood pressure in men and women with mild hypertension: effects on cardiovascular, metabolic, and hemodynamic functioning. Arch Intern Med 2000; 160:1947–1958 [DOI] [PubMed] [Google Scholar]
- 8. Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, Williams B, Ford GA. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens 2006; 24:215–233 [DOI] [PubMed] [Google Scholar]
- 9. Krall EA, Dwyer JT. Validity of a food frequency questionnaire and a food diary in a short-term recall situation. J Am Diet Assoc 1987; 87:1374–1377 [PubMed] [Google Scholar]
- 10. Fairburn C. Cognitive-Behavioral Treatment of Obesity: a Clinician’s Guide. Guilford Press: New York, 2003 [Google Scholar]
- 11. Craighead L. The Appetite Awareness Workbook: how to Listen to Your Body and Overcome Binge Eating, Overeating, and Obsession with Food. New Harbinger: Oakland, 2006 [Google Scholar]
- 12. Chakraborty H, Gu H. A mixed model approach of intent-to-treat analyses in longitudinal clinical trials with missing values. http://www.rti.org/rtipress [PubMed]
- 13. Cutler JA. Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. Arch Intern Med 1997; 157:657–667 [PubMed] [Google Scholar]
- 14. Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D, Milas NC, Mattfeldt-Beman M, Belden L, Bragg C, Millstone M, Raczynski J, Brewer A, Singh B, Cohen J, Trials for the Hypertension Prevention Research Group Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med 2001; 134:1–11 [DOI] [PubMed] [Google Scholar]
- 15. Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH, Jr, Kostis JB, Kumanyika S, Lacy CR, Johnson KC, Folmar S, Cutler JA. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA 1998; 279:839–846 [DOI] [PubMed] [Google Scholar]
- 16. Kostis JB, Wilson AC, Shindler DM, Cosgrove NM, Lacy CR. Non-drug therapy for hypertension: do effects on weight and sodium intake persist after discontinuation of intervention? Am J Med 2000; 109:734–736 [DOI] [PubMed] [Google Scholar]
- 17. Tinker LF, Bonds DE, Margolis KL, Manson JE, Howard BV, Larson J, Perri MG, Beresford SA, Robinson JG, Rodriguez B, Safford MM, Wenger NK, Stevens VJ, Parker LM, Women’s Health Initiative Low-fat dietary pattern and risk of treated diabetes mellitus in postmenopausal women: the Women’s Health Initiative randomized controlled dietary modification trial. Arch Intern Med 2008; 168:1500–1511 [DOI] [PubMed] [Google Scholar]
- 18. Hivert MF, Langlois MF, Berard P, Cuerrier JP, Carpentier AC. Prevention of weight gain in young adults through a seminar-based intervention program. Int J Obes (Lond) 2007; 31:1262–1269 [DOI] [PubMed] [Google Scholar]
- 19. Oldroyd JC, Unwin NC, White M, Imrie K, Mathers JC, Alberti KG. Randomised controlled trial evaluating the effectiveness of behavioural interventions to modify cardiovascular risk factors in men and women with impaired glucose tolerance: outcomes at 6 months. Diabetes Res Clin Pract 2001; 52:29–43 [DOI] [PubMed] [Google Scholar]
- 20. Simkin-Silverman LR, Wing RR, Boraz MA, Meilahn EN, Kuller LH. Maintenance of cardiovascular risk factor changes among middle-aged women in a lifestyle intervention trial. Womens Health 1998; 4:255–271 [PubMed] [Google Scholar]
- 21. Thompson JL, Allen P, Helitzer DL, Qualls C, Whyte AN, Wolfe VK, Herman CJ. Reducing diabetes risk in American Indian women. Am J Prev Med 2008; 34:192–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med 2002; 136:493–503 [DOI] [PubMed] [Google Scholar]
- 23. Wing RR, Venditti E, Jakicic JM, Polley BA, Lang W. Lifestyle intervention in overweight individuals with a family history of diabetes. Diabetes Care 1998; 21:350–359 [DOI] [PubMed] [Google Scholar]
- 24. Jakicic JM, Marcus BH, Lang W, Janney C. Effect of exercise on 24-month weight loss maintenance in overweight women. Arch Intern Med 2008; 168:1550–1559; discussion 1559–1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jeffery RW, Wing RR, Sherwood NE, Tate DF. Physical activity and weight loss: does prescribing higher physical activity goals improve outcome? Am J Clin Nutr 2003; 78:684–689 [DOI] [PubMed] [Google Scholar]
- 26. Hunter GR, Brock DW, Byrne NM, Chandler-Laney PC, Del Corral P, Gower BA. Exercise training prevents regain of visceral fat for 1 year following weight loss. Obesity (Silver Spring) 2010; 18:690–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bartfield JK, Stevens VJ, Jerome GJ, Batch BC, Kennedy BM, Vollmer WM, Harsha D, Appel LJ, Desmond R, Ard JD. Behavioral transitions and weight change patterns within the PREMIER trial. Obesity (Silver Spring) 2011; 19:1609–1615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fowles ER, Sterling BS, Walker LO. Measuring dietary intake in nursing research. Can J Nurs Res 2007; 39:146–165 [PubMed] [Google Scholar]
- 29. Spring B, Duncan JM, Janke EA, Kozak AT, McFadden HG, Demott A, Pictor A, Epstein LH, Siddique J, Pellegrini CA, Buscemi J, Hedeker D. Integrating technology into standard weight loss treatment: a randomized controlled trial. Arch Intern Med 2012; 173:105–111 [DOI] [PMC free article] [PubMed] [Google Scholar]