Abstract
Background & objectives:
Community outbreaks of disease amongst nomadic populations generally remain undocumented. Following a reported increase in acute respiratory tract infections (ARI) in May 2011 in a nomadic population of Sangerwini in Jammu & Kashmir, India, we examined the patients with ARI symptoms and their nasal swabs were tested for influenza virus.
Methods:
Patients with ARI (n=526) were screened from May 14 to 23, 2011 and nasopharyngeal swabs collected from 84 with Influenza like illness (ILI) for bacterial cultures and influenza virus testing. Samples were tested for influenza A and influenza B by real time (RT)-PCR.
Results:
Twelve (14.3%) of the 84 patients tested positive for influenza B, compared to only one (0.9%) of 108 patients with ILI in a parallel survey performed in Srinagar during the same period, suggesting a localized outbreak in the isolated nomadic community. All presented with respiratory symptoms of less than seven days. Familial clustering was seen in 40 per cent (25% of influenza B positives). Average daytime temperatures ranged from 15-16°C compared to 22°C in Srinagar. Four patients developed pneumonia whereas others ran a mild course with a total recovery with oseltamivir and symptomatic therapy.
Interpretation & conclusion:
Our report of confirmed influenza B in this underprivileged nomadic population argues for routine surveillance with efforts to improve vaccination and infection control practices.
Keywords: Epidemiology, influenza B, nomads, outbreak
Influenza outbreaks have frequently been described at mass gatherings (cruise ships, sporting events and pilgrimages) and in populations such as residents of nursing care facilities, residential schools or colleges, and other enclosed communities1,2. Although outbreaks of communicable diseases in isolated populations have been described; insufficient epidemiologic and pathogen-related data have been reported to characterize the outbreaks1,2. Nomads (estimated population 50-100 million)3 are mostly pastoralists (living by raising livestock) and migrate periodically with their herds. Community outbreaks of disease among nomadic populations, with minimal access to healthcare, generally remain undocumented. The nomads in Kashmir live in temperate conditions with cold temperature, generally in one room hutments shared by 4-12 family members. Crudely constructed of mud, stones and wooden logs, these hutments have no formal ventilation and are on occasion shared with cattle. Biomass fuels (soft pine wood and cow dung) burnt for cooking and warming render the dwellings smoky. Access to healthcare is poor and virtually no infection control measures are practised. Generally the families live below poverty line, engaged in farming of poor yield crops and cattle raising. Multiple pregnancies and malnutrition are common and vaccinations are nearly non-existent.
In May 2011, a spurt of acute respiratory tract infections (ARI) including four deaths was reported in the isolated nomadic population of Sangerwani in the Shopian district of Jammu and Kashmir (north India) by the local authorities of the region4. This outbreak presented a unique opportunity to study the effects of influenza in a nomadic population by combining epidemiologic data, laboratory data obtained after respiratory tract sampling, and influenza like illness (ILI) surveillance data obtained from the capital district of Srinagar.
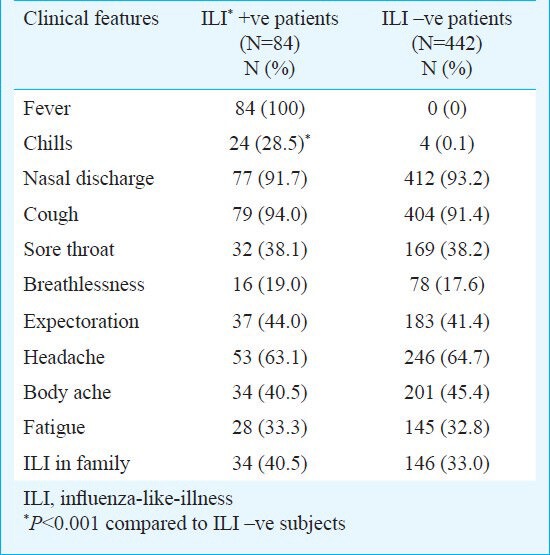
Material & Methods
Sangerwini (altitude 7500 ft) in the Himalayan Mountains consists of 13 villages with a total population of 17,573 nomads (31% aged 5-14 yr). The average daytime temperature is 7-10 degrees lower than neighbouring Srinagar. Four deaths were reported in April-May 2011 in young children of <4 yr of age due to severe pneumonia and acute respiratory distress and seven patients were admitted in the GB Pant hospital for children in Srinagar, Kashmir, for bronchopneumonia. Sher-i-Kashmir Institute of Medical Sciences (SKIMS), a tertiary care facility in Srinagar, was invited by the health directorate to investigate the cause of these respiratory illness related deaths. A medical team (consisting of 4 physicians and 5 laboratory personnel of influenza Laboratory of the SKIMS) visited the area during May 14-23, 2011. The clinical features of those fulfilling the criteria of ILI (defined by fever >38°C and a cough or sore throat) were recorded on a predefined questionnaire5. A total of 526 persons (age 1-75 yr, median 20 yr) with ARI were screened and throat/nasal swabs were obtained from 84 consecutive consenting patients (age 1-70 yr, median 7 yr) with ILI for influenza testing and transported to the Microbiology Laboratory at the All India Institute for Medical Sciences (AIIMS), New Delhi. The patients with ILI had significantly higher frequency of fever and chills (P<0.0001, Table I) as compared to those without features of ILI. Other symptoms were comparable in frequency (Table I). All the samples were tested by real-time (RT)-PCR for the detection of influenza viruses including 2009A ⁄H1N1 virus using the Centers for Disease Control and Prevention protocol6. Throat swabs were also sent for bacterial cultures and blood cultures were obtained in a subset (n=17). The distribution of influenza virus types was compared with that among 108 patients with ILI in Srinagar (SKIMS, 70 km away) at the same time (also in AIIMS, New Delhi as part of the Multisite Surveillance of Influenza Survey, samples collected both from hospitals and from the community). Informed consent was obtained from all participants and the study protocol was approved by the Institute Ethics Committee of the Sher-i-Kashmir Institute of Medical Sciences, Srinagar.
Table I.
Clinical features of the patients screened with ARI (ILI positive versus ILI negative patients)
Statistical analyses were performed using SPSS version 11.5 software (Chicago, Illinois, USA). Continuous data were compared using Student's t-test and the categorical data using Chi-square or Fisher's exact test, as appropriate.
Results & Discussion
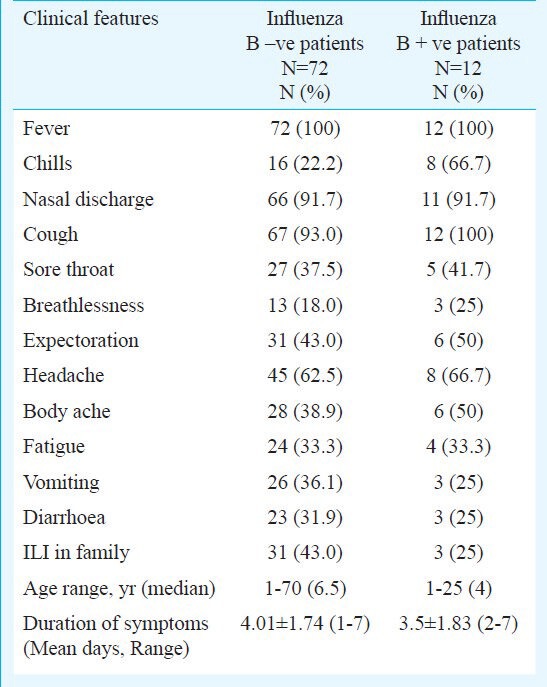
Of the 84 patients with ILI, (aged 1-70 yr, median 7 yr, 75% <10yr; 49 males, 35 females), 12 (14.3%; age 1-25 yr, median age 4 yr) tested positive for influenza B but none for influenza A or any bacterial organisms. In contrast, only one of 108 (1%; 39 female, age range 1-90 yr, median 28 yr) ILI cases from SKIMS was positive for influenza B, suggesting a localized outbreak in this isolated community of nomads. All 12 patients positive for influenza B presented with fever, respiratory and constitutional symptoms in variable frequency and all presented within seven days of their illness (Table II). Chills were more frequent among influenza B positive patients but other clinical features were similarly dispersed. Nearly 40 per cent of patients with ILI and 25 per cent of influenza B positives had evidence of familial clustering. There were no underlying co-morbid conditions in influenza B positive patients. Four patients developed features of pneumonia whereas all others had a rather mild course of illness and recovered fully over a period of two weeks with decongestants, antipyretics, azithromycin and oseltamivir therapy.
Table II.
Clinical features amongst the influenza B positive and negative ILI patients (n=84)
Though detailed data about the general health status of nomads are scant, they appear to be generally healthier than their settled neighbours4. Viral infections are reported to be less common among the nomads7,8,9. In light of these observations, transmission of infectious diseases among nomads is believed to be very low. However, the living conditions of the Himalayan nomads involved in the present study are quite distinct from those living in warmer climates in whom viral infections have been reported to be uncommon8,9.
Because influenza viruses are usually spread by droplets and aerosols produced by an infected person during coughing or sneezing, overcrowding in semi-enclosed environments can lead to the spread of the disease. Congregated settings have earlier been reported to contribute to influenza B outbreaks1,2,10, and current living conditions may have been conducive for the outbreak among the nomads.
The average temperatures in the terrain were about 8-10 degrees lower than the nearby city. The role of exposure to cold weather with regard to the emergence of respiratory diseases is unclear. The cold weather related increase in the incidence of and morbidity associated with respiratory diseases is generally attributed to cross-infection resulting from indoor crowding, effects of low temperature on the immune system, and, possibly, better survival of influenza in droplets during cold weather11.
Influenza outbreaks have been reported in times of no-influenza activity12. Influenza activity during the study period in general remained at low levels in both northern and southern hemisphere countries except South Africa, where widespread A(H1N1)2009 activity was reported13. A parallel survey conducted in the neighbouring capital district of Srinagar revealed no influenza activity at this time (unpublished observation). Likewise, no Influenza activity was observed in other parts of India during the same period13.
Influenza B viruses have been responsible for sporadic seasonal influenza and can be associated with severe illness and death. None of our patients with influenza B positivity had severe complications even though four patients developed features of pneumonia, but all scored <2 on CURB (confusion, urea, respiratory rate, blood pressure) scoring14 and did not develop respiratory failure necessitating hospitalized treatment. Severe complications like encephalitis/encephalopathy, influenza-associated myositis and acute respiratory distress syndrome (ARDS) have been reported from fatal cases with influenza B in Taiwan15. All patients with ILI were treated with oseltamivir including those who developed pneumonia. Limited data are available on the use of oseltamivir in influenza B outbreaks16,17.
The limitations of the study include a sample of convenience and the limitation of not having tested for other respiratory viruses. Additionally, patients not fulfilling the criteria for ILI could have carried the virus as well.
In conclusion, a confirmed outbreak of influenza B in this nomadic tribal community calls for intensive efforts for providing health care, surveillance and infection control practices including vaccination to this underprivileged community. However, despite documentation of a decline in influenza related outcomes associated with increased vaccination rates18, the challenges of adequate delivery of such measures especially vaccination in individuals dwelling in difficult terrains need a special address.
Acknowledgment
The study was funded by the Centre for Disease Control and Prevention, Influenza Division, Atlanta, GA, USA.
References
- 1.Blyth CC, Foo H, van Hall SJ, Hurt AC, Barr IG, McPhie K, et al. Influenza outbreaks during World Youth Day 2008 mass gathering. Emerg Infect Dis. 2010;16:809–15. doi: 10.3201/eid1605.091136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mook P, Ellis J, Watson JM, Thompson C, Zambon M, McMenamin J, et al. Public health implications of influenza B outbreaks in closed settings in the United Kingdom in the 2007/08 influenza season. Euro Surveill. 2008;13 pii=18986. [PubMed] [Google Scholar]
- 3.Berland JC, Rao A. Westport, CT (USA): Praeger Pub; 2004. Customary strangers: New perspective on peripatetic people in the Middle East, Africa and Asia. [Google Scholar]
- 4.Mysterious Disease hits Pulwama village. [accessed on May 10, 2010]. Available from: http://www.greaterkashmir.com/news/2011/May/10/mysterious-disease-hits-pulwama-village-36.asp .
- 5.Koul PA, Muneer MA, Bali NK, Chawla-Sarkar M, Sarkar M, Kaushik S, et al. Pandemic and seasonal influenza viruses among patients with Acute Respiratory Illness in Kashmir (India) Influenza Other Resp Viruses. 2011;5:e521–7. doi: 10.1111/j.1750-2659.2011.00261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Geneva: 2009. [accessed on September 28, 2010]. World Health Organization. CDC protocol of real-time RT PCR for influenza A (H1N1) Available from: http://www.who.int/csr/resources/publications/swineflu/CDCrealtimeRTPCRprotocol_20090428.pdfr . [Google Scholar]
- 7.Sheik-Mohamed A, Velema JP. Where healthcare has no access: the nomadic populations of sub-Saharan Africa. Trop Med Int Health. 1999;4:695–707. doi: 10.1046/j.1365-3156.1999.00473.x. [DOI] [PubMed] [Google Scholar]
- 8.Chabasse D, Roure C, Rhaly A, Maiga D, Traore M, Tounkara A, et al. The health of nomads and semi-nomads of the Malian Gourma:an epidemiological approach. In: Hill AG, editor. Population, health and nutrition in the Sahil. London: Routledge and Kegan Paul; 1985. pp. 319–39. [Google Scholar]
- 9.Loutan L, Paillard S. Measles in a West African nomadic community. Bull World Health Organ. 1992;70:741–4. [PMC free article] [PubMed] [Google Scholar]
- 10.Balkhy HH, Memish ZA, Bafaqeer S, Almuneef MA. Influenza a common viral infection among Hajj pilgrims: time for routine surveillance and vaccination. J Travel Med. 2004;11:82–6. doi: 10.2310/7060.2004.17027. [DOI] [PubMed] [Google Scholar]
- 11.Tamerius JD, Shaman J, Alonso WJ, Bloom-Feshbach K, Uejio CK, Comrie A, et al. Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog. 2013;9:e1003194. doi: 10.1371/journal.ppat.1003194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Broor S, Krishnan A, Roy DS, Dhakad S, Kaushik S, Mir MA, et al. Dynamic patterns of circulating seasonal and pandemic 2009A (H1N1) influenza viruses from 2007-2010 in and around Delhi, India. PLoS One. 2012;7:e29129. doi: 10.1371/journal.pone.0029129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Influenza Update 134. [accessed on December 19, 2013]. Available from: http://www.who.int/influenza/surveillance_monitoring/updates/2011_05_20_GIP_surveillance/en .
- 14.Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–82. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li WC, Shih SR, Huang YC, Chen GW, Chang SC, Hsiao MJ, et al. Clinical and genetic characterization of severe influenza B-associated diseases during an outbreak in Taiwan. J Clin Virol. 2008;42:45–51. doi: 10.1016/j.jcv.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 16.Kawai N, Ikematsu H, Iwaki N, Maeda T, Satoh I, Hirotsu N, et al. A comparison of the effectiveness of oseltamivir for the treatment of influenza A and influenza B: a Japanese multicenter study of the 2003e2004 and 2004e2005 influenza seasons. Clin Infect Dis. 2006;43:439–44. doi: 10.1086/505868. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control. Antivirals for the treatment and chemoprophylaxis of Influenza. Recommendations of the Advisory Committee on Immunization Practices. Recommendations and Reports. [accessed on June 22, 2012];MMWR Morb Mortal Wkly Rep. 2011 Jan;60(RR01):1–24. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6001a1.htm . [Google Scholar]
- 18.Viboud C, Miller M. Health benefits of universal influenza vaccination strategy. PLoS Med. 2008;5:e216. doi: 10.1371/journal.pmed.0050216. [DOI] [PMC free article] [PubMed] [Google Scholar]


