Abstract
Background & objectives:
Obesity is a major risk factor for cardiovascular disease (CAD). This study was aimed to assess the risk for CAD determined by certain new and conventional body composition parameters such as visceral fat area (VFA), body mass index (BMI), waist to hip ratio (WHR), etc.
Methods:
We did an age and sex matched case-control study of acute myocardial infarction with 100 participants in a tertiary care hospital (50 cases and 50 controls) representing the serving army personnel. The relation between VFA, per cent body fat (PBF), BMI, waist and hip circumferences, and WHR to CAD was assessed.
Results:
The study showed that there was a significantly increased risk for CAD associated with VFA (OR: 5.67; 95% CI: 1.96, 16.95), WHR (7.07; 2.19, 24.27), waist circumference (WC) (2.63; 1.05, 6.66) and BMI (2.53; 1.03, 6.26).
Interpretation & conclusions:
In conclusion, increased VFA, BMI, WHR and WC showed an association with CAD. VFA is a good index for assessing not only visceral fat accumulation but also cardiovascular risk factors.
Keywords: Bioelectrical impedence analysis, body mass index, coronary artery disease, visceral fat area, waist-hip ratio
Coronary artery disease (CAD) is a global health problem. CAD burden is projected to increase from around 47 million DALYs (disability adjusted life years) globally in 1990 to 82 million DALYs in 20201. In India, CAD is gaining momentum and there were 46.97 million cases in 2010 (urban: 24.69 million and rural: 22.28 million)2.
Obesity has long been considered as an indicator of lifestyle diseases. Consequently, body mass index (BMI) was being considered as an indicator of CAD and metabolic syndrome3. However, physicians have been puzzled by the heterogeneity of variables as not every obese person develops CAD3,4. The body fat distribution, especially intra-abdominal adipose tissue accumulation, has been found to be a key correlate of a cluster of diabetogenic, atherogenic, prothrombotic and inflammatory metabolic abnormalities increasing the risk of type 2 diabetes and CAD4. Though, waist circumference can be used in clinical practice as a first approach and as a crude index to identify patients who have excess visceral abdominal tissue, newer methods are now available to assess accurate distribution of fat which include hydrodensitometry, computed tomography (CAT) scan, magnetic resonance imaging (MRI), near infrared interactance, dual-energy X-ray absorptiometry (DEXA), neutron activation and body image assessment (BIA). We undertook this study to determine various body composition parameters that could act as correlates of CAD among patients with CAD and healthy controls.
Material & Methods
The study was carried out amongst the armed forces service personnel aged more than 30 yr randomly selected from the Cardiology OPD of Armed Forces Medical College (AFMC), Pune, India, between April 2012 and June 2012. Considering α as 5 per cent, power 80 per cent, proportion among cases having increased adiposity as 50 per cent and those among controls as 20 per cent, the sample size was calculated to be 46 using STATA (Intercooled) ver 9.25. Criteria for selecting CAD cases were: ECG suggesting ischaemic changes; angiography confirmed cases; those already had an episode of myocardial infarction (MI). Frequency matched, hospital based controls were selected from serving army persons. The controls were asked for any history suggestive of CAD and an ECG was taken to ensure that they were not cases. Athletes, cases of carcinoma, chronic infections like TB, HIV, AIDS, cases of hypertension, diabetes mellitus were excluded from both the cases and controls. The study protocol was approved by the Institutional Ethical Committee.
After obtaining the written informed consent and filling a pre-tested questionnaire, patients from Cardiology OPD (reporting for first review after discharge) and controls from surgical OPD were requested to undergo anthropometric measurements and body composition analysis using in body 720 body composition analyser imported South Korea. The study participants were asked to stand bare footed. All metallic items were removed. Minimal clothing was kept on. The participant was asked to stand on the machine such that both heel and the ball of feet would touch the foot electrode. The participant was instructed to take the hand electrode in their hand and stand still for 2 to 3 min. Once the test was underway, the patient was asked to keep the same posture until the end of the test. The parameters recorded were visceral fat area (VFA), body mass index (BMI), waist hip ratio (WHR), waist circumference (WC), per cent body fat (PBF), physical activity, family history of CAD, food habits, smoking and alcohol status.
Statistical analysis was done by using Epi info 2002 and IBM SPSS Statistics 20 (Evaluation copy, AFMC, Pune). The Student t-test, Mann-Whitney U Test, Chi-square test and Binary logistic regression was used and P<0.05 was considered as significant.
Results & Discussion
The study population included 50 CAD patients and 50 age and sex matched controls. Significantly higher values (P<0.05) of BMI, WC, WHR, VFA and PBF were found in cases than in controls (Table I). The difference was not significant for weight and hip circumference between cases and controls.
Table I.
Body composition and characteristics of cases and controls
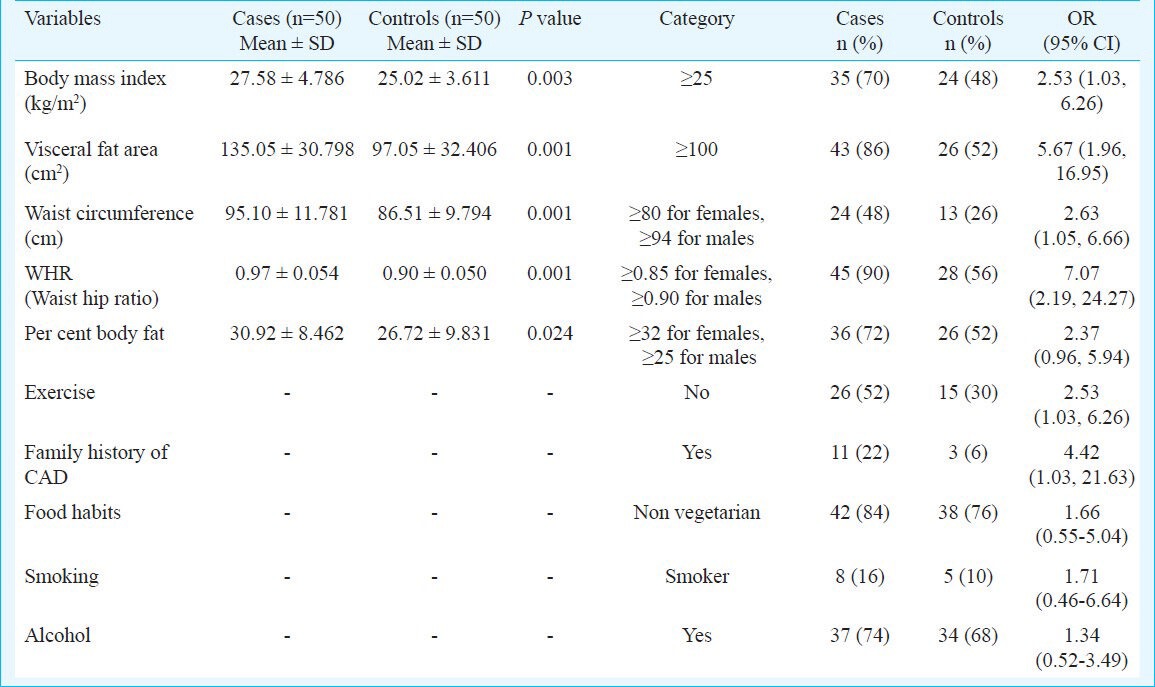
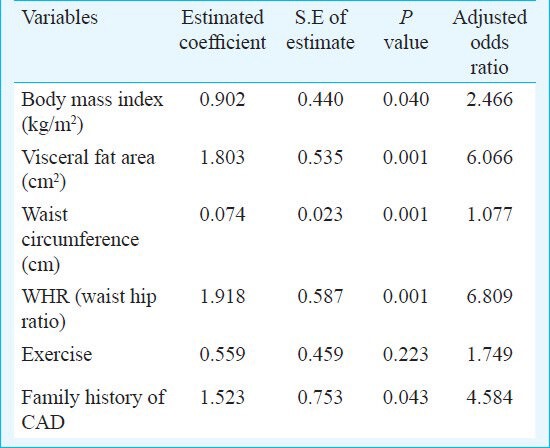
Univariate analysis showed significant risk for CAD with BMI, WC, WHR, VFA, physical inactivity and family history of CAD (Table I). Though Odds ratios (OR) were higher for PBF, smoking and alcohol, these were not significant. In multivariate analysis, the adjusted ORs were significantly higher for BMI (2.466), WC (1.077), WHR (6.809), VFA (6.066) and family history of CAD (4.584) (Table II).
Table II.
Step-wise binary logistic model for multivariate analysis of selected variables
The association between body fat distribution and cardiovascular events has been much discussed during the past decades. Wolk et al6 found that BMI had a significant association with CAD while a large case-control study found WHR having a significantly higher odds ratio7. Using ultrasonography for visceral fat assessment, Kim et al8 found higher OR for CAD in the middle and high visceral fat thickness (VFT) tertiles (4.48; 1.29, 5.51 and 2.04; 1.06, 3.94, respectively)8, while an Indian study concluded that VFA was significantly higher (122.58 ± 37.59 vs. 88.4 ± 36.95) in cases compared to controls9. The present study also has similar finding (Table I).
Adjusted ORs for CAD for light, moderate, and heavy drinking were reported to be 1.16 (0.68 to 1.94), 1.78 (1.35 to 2.27), and 2.18 (1.46 to 3.25), respectively among Chinese men10. However, an Indian study did not find significant association between habit of drinking and CAD11.
Another study among Indians mentioned that about 50 per cent of Asian Indians are vegetarians, but their rates of CAD are as high as of non-vegetarians12. Family history of CAD as an independent risk factor for CAD (9.41; 1.60-55.49) was found in a Korean study13 and we also observed the same.
The limitation of our study was the wide confidence interval for some of the ORs for which more data from a large sample may be required to generate robust evidence. Only subjects with BMI <25 kg/m2 should have been considered to highlight the importance of VFA.
In conclusion, increased VFA, BMI, WHR, WC and family history of CAD showed a significant association with CAD. To further validate these findings further studies with appropriate sample size would be required.
Acknowledgment
The first author (RS) acknowledges the Indian Council of Medical Research for short-term studentship (STS 2012-00896).
References
- 1.The Atlas of Heart Disease and Stroke. [accessed on January 11, 2012]. Available from: http://www.who.int/cardiovascular_diseases/resources/atlas/en .
- 2.National Health Profile. 2010. [accessed on January 13, 2012]. Available from: http://cbhidghs.nic.in/index2.asp?slid=1125&sublinkid=929 .
- 3.Mathieu P, Pibarot P, Larose E, Poirier P, Marette A, Després JP. Visceral obesity and the heart. Int J Biochem Cell Biol. 2008;40:821–36. doi: 10.1016/j.biocel.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Despres JP. Intra-abdominal obesity: an untreated risk factor for type 2 diabetes and cardiovascular disease. J Endocrinol Invest. 2006;29(Suppl 3):77–82. [PubMed] [Google Scholar]
- 5.STATA: Data Analysis and Statistical Software. Intercooled STATA ver 9.2. [accessed on January 13, 2012]. Available from: www.stata.com .
- 6.Wolk R, Berger P, Lennon RJ, Brilakis ES, Somers VK. Body mass index: a risk factor for unstable angina and myocardial infarction in patients with angiographically confirmed coronary artery disease. Circulation. 2003;108:2206–11. doi: 10.1161/01.CIR.0000095270.85646.E8. [DOI] [PubMed] [Google Scholar]
- 7.Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640–9. doi: 10.1016/S0140-6736(05)67663-5. [DOI] [PubMed] [Google Scholar]
- 8.Kim SK, Kim HJ, Hur KY, Choi SH, Ahn CS, Lim SK, et al. Visceral fat thickness measured by ultrasonography can estimate not only visceral obesity but also risks of cardiovascular and metabolic diseases. Am J Clin Nutr. 2004;79:593–9. doi: 10.1093/ajcn/79.4.593. [DOI] [PubMed] [Google Scholar]
- 9.Varghese B, Swamy S, Srilakshmi MA, Santhosh MJ, Shetty GG, Varghese K, et al. Visceral adiposity in young patients with coronary artery disease-a case control study. Indian Heart J. 2012;64:284–9. doi: 10.1016/S0019-4832(12)60088-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou X, Li C, Xu W, Hong X, Chen J. Relation of alcohol consumption to angiographically proved coronary artery disease in Chinese men. Am J Cardiol. 2010;106:1101–3. doi: 10.1016/j.amjcard.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 11.Bagchi S, Biswas R, Bhadra UK, Roy A, Mundle M, Dutta PK. Smoking, alcohol consumption & coronary heart disease - A risk factor study. Indian J Community Med. 2001;26:208. [Google Scholar]
- 12.Enas EA, Senthilkumar A. Coronary artery disease in Asian Indians: An update and review. Internet J Cardiol. 2001. [accessed on November 2, 2013]. p. 1. Available from: http://ispub.com/IJC/1/2/4493 .
- 13.Yoo WS, Kim HJ, Kim D, Lee MY, Chung HK. Early detection of asymptomatic coronary artery disease in patients with type 2 diabetes mellitus. Korean J Intern Med. 2009;24:183–9. doi: 10.3904/kjim.2009.24.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]


