Sir,
Staphylococcus aureus causes a wide array of infections, both community acquired and nosocomial. It is the commonest cause of surgical site infections and a prominent hospital acquired pathogen from blood stream infections and pneumonia1,2. Coagulase-negative staphylococci (CoNS) are an important cause of the device associated blood stream infections3. CoNS are more resistant to antibiotics than S. aureus3. The growing global prevalence of methicillin resistance among Staphylococcus is limiting the therapeutic options available to treat invasive staphylococcal infections. Till now both S. aureus and CoNS have remained by and large sensitive to glycopeptides except for a few case reports of vancomycin resistant and intermediate S. aureus (VRSA, VISA) and vancomycin resistant CoNS4,5,6,7. However, there are reports of therapeutic failure to vancomycin treatment for serious infections when the organisms, although in susceptible range, have increased minimum inhibitory concentrations (MICs) (2 μg/ml)4. There have been reports from a few hospitals of increasing MICs of vancomycin (MIC creep) in S. aureus5,6. Emergence of vancomycin resistance foretells a grave future for management of serious staphylococcal infections in view of the fact that no new antimicrobials are being developed and the recently introduced ones like tigecycline and daptomycin are very expensive.
The 165 bedded level-1 Trauma Centre of the All India Institute of Medical Sciences (AIIMS) hospital, New Delhi, India, became functional in November, 2006. The Microbiology Laboratory of the Trauma Centre receives around 12,000 samples annually from admitted trauma patients. Microrganisms are recovered from approximately 2500 of these samples. Staphylococcus spp. constitutes approximately 20 per cent of these isolates. In this study, we report the changing pattern of vancomycin MIC for S. aureus since the centre began functioning and overall resistance for vancomycin among CoNS isolates during the four years (2007-2010).
All consecutive, non duplicate Staphylococcus isolates were identified to species level by the Vitek II (Biomeriux, France) (as per manufacturer's instructions) and conventional methods8. These clinical isolates were tested for vancomycin susceptibility by Vitek 2 and E-test9. The MICs were evaluated both by Vitek 2 version 4.01 system and E- test following Clinical and Laboratory Standards Institute (CLSI) recommendations9. Vancomycin MIC ≤ 2 μg/ml was considered susceptible, MIC in range 4-8 μg/ml as intermediate and ≥8 μg/ml as resistant for S. aureus. Vancomycin MIC < 4 μg/ml was considered susceptible, MIC in range 8-16 μg/ml as intermediate and > 32 μg/ml as resistant for CoNS. Methicillin susceptibility was determined using both oxacillin and cefoxitin disk under CLSI recommended conditions9. Methicillin susceptibility was also confirmed by cefoxitin screen in Vitek 2. All results were interpreted according to the CLSI document M-100 - S1810. The following strains were taken as controls: S. aureus ATCC 25923 (vancomycin susceptible, methicillin sensitive), S. aureus ATCC 43300 (vancomycin susceptible, methicillin resistant) and S. aureus ATCC 700699 (vancomycin intermediate S aureus), Enterococcus faecalis ATCC 51299 (vancomycin susceptible Enterococcus) and S. epidermidis ATCC 12228 procured from ATCC (LGC Promochem, India).
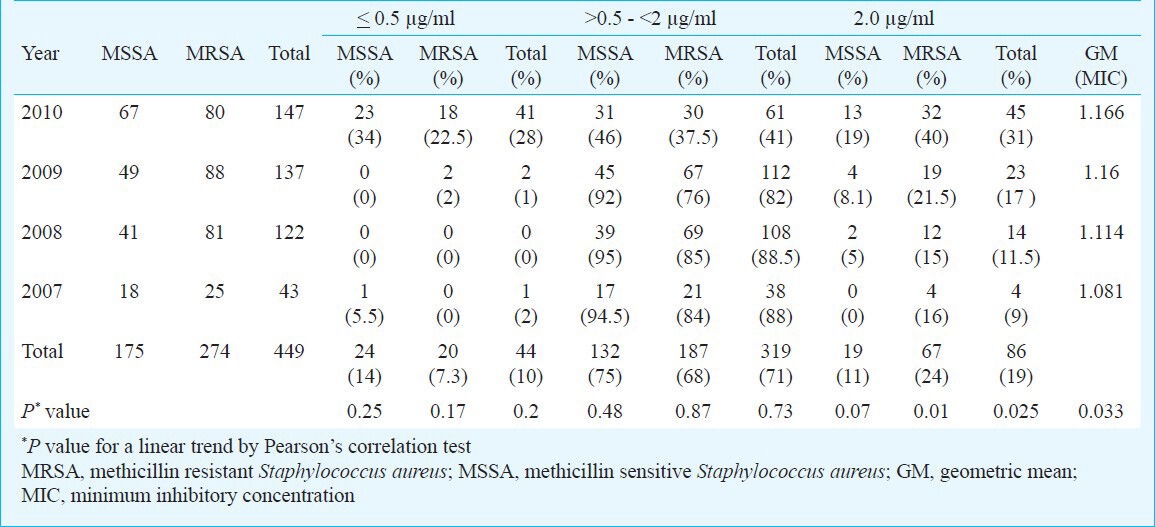
A total of 449 isolates of S. aureus were recovered during the study period. These included 315 (70%) from pus/wound swabs of post-operative infections, 40 (9%) from blood, 29 (6%) from respiratory samples, 34 (7.5%) from central vascular lines tips, 15 (3%) from tissues and 8 (2%) each from urine and 8 (1.78%) from body fluids. There were no discordant results regarding the interpretation of susceptibility testing as isolate being sensitive, intermediate or resistant between Vitek 2 and E-test. All isolates had vancomycin MIC in the susceptible range. However, a significant and progressive increase was observed in the percentage of isolates showing vancomycin MIC 2 μg/ml. In 2007 only 9 per cent isolates of S. aureus had an elevated vancomycin MIC, in contrast to 31 per cent in 2010 (Table).
Table.
Vancomycin MICs of S. aureus isolates by E-test from 2007 to 2010 (N=449)
Vancomycin MICs were determined for 127 CoNS using both Vitek 2 and E test. Of these, 116 (91%) were methicillin resistant and 19 (15%) had vancomycin MIC 4 μg/ml.
Thus, a trend of increasing vancomycin MICs among S. aureus isolates was observed. A lacuna of this study was that it could not be ascertained if the staphylococci with elevated MIC were associated with therapeutic failures since other antibiotics like linezolid or netilmicin were also administered for MRSA. In an earlier study from our Centre 58 per cent isolates were MRSA, and daptomycin was found to be an effective drug against MRSA11. The rate of methicillin resistance was 100 per cent amongst 40 isolates of CoNS in another study from our centre12. However, in the present study, the rates of methicillin resistance were 61 and 91 per cent, respectively in S. aureus and CoNS. Several studies from India have reported methicillin resistance varying from 50-80 per cent and 30-60 per cent among S. aureus and coagulase negative staphylococci, respectively13,14,15.
As per the reports available from the world 3-11 per cent CoNS isolates have decreased susceptibility to vancomycin16,17. In our study, 15 per cent CoNS isolates were observed with decreased susceptibility which is higher as compared to other studies. However, these CoNS isolates did not show any significant rising trend of vancomycin MICs.
In conclusion, the changing pattern of vancomycin MIC indicates the necessity of active surveillance for therapeutic failures and timely identification of VRSA and VISA isolates to prevent their transmission. Increasing vancomycin MICs at a centre which caters to trauma patients, who are otherwise usually immunocompetent indicate that strict infection control measures need to be instituted.
References
- 1.Bamberger DM, Boyd SE. Management of Staphylococcus aureus infections. Am Fam Physician. 2005;72:2474–81. [PubMed] [Google Scholar]
- 2.Dryden MS. Complicated skin and soft tissue infection. J Antimicrob Chemother. 2010;65:S35–44. doi: 10.1093/jac/dkq302. [DOI] [PubMed] [Google Scholar]
- 3.Natoli S, Fontana C, Favaro M, Bergamini A, Testore GP, Minelli S, et al. Characterization of coagulase-negative staphylococcal isolates from blood with reduced susceptibility to glycopeptides and therapeutic options. BMC Infect Dis. 2009;9:83. doi: 10.1186/1471-2334-9-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tenover FC. Vancomycin-resistant Staphylococcus aureus: a perfect but geographically limited storm? Clin Infect Dis. 2008;46:675–7. doi: 10.1086/527393. [DOI] [PubMed] [Google Scholar]
- 5.Robert J, Bismuth R, Jarlier V. Decreased susceptibility to glycopeptides in methicillin-resistant Staphylococcus aureus: a 20 year study in a large French teaching hospital, 1983-2002. J Antimicrob Chemother. 2006;57:506–10. doi: 10.1093/jac/dki486. [DOI] [PubMed] [Google Scholar]
- 6.Fridkin SK, Hageman J, McDougal LK, Mohammed J, Jarvis WR, Perl TM, et al. Epidemiological and microbiological characterization of infections caused by Staphylococcus aureus with reduced susceptibility to vancomycin, United States, 1997-2001. Clin Infect Dis. 2003;36:429–39. doi: 10.1086/346207. [DOI] [PubMed] [Google Scholar]
- 7.Srinivasan A, Dick JD, Perl TM. Vancomycin resistance in staphylococci. Clin Microbiol Rev. 2002;15:430–8. doi: 10.1128/CMR.15.3.430-438.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baird D. Staphylococcus: cluster-forming gram-positive cocci. In: Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Mackie & McCartney practical medical microbiology. 14th ed. New York: Churchill Livingstone; 1996. pp. 245–61. [Google Scholar]
- 9.Wayne, PA: CLSI; 2006. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing, 16th informational supplement, M100-S16. [Google Scholar]
- 10.Wayne, PA: CLSI; 2008. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing, 18th informational supplement, M100-S18. [Google Scholar]
- 11.Behera B, Jain N, Sharma S, Mathur P, Misra MC. Antimicrobial activity of daptomycin against Staphylococcus aureus isolates from skin and skin structure infections of trauma patients. J Infect. 2010;61:195–6. doi: 10.1016/j.jinf.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 12.Behera B, Mathur P. Erroneous reporting of vancomycin susceptibility for Staphylococcus spp. by vitek software version 2.01. Jpn J Infect Dis. 2009;62:298–9. [PubMed] [Google Scholar]
- 13.Mallick SK, Basak S. MRSA - too many hurdles to overcome: a study from Central India. Trop Doct. 2010;40:108–10. doi: 10.1258/td.2010.090440. [DOI] [PubMed] [Google Scholar]
- 14.Verma S, Joshi S, Chitnis V, Hemwani N, Chitnis D. Growing problem of methicillin resistant staphylococci - Indian scenario. Indian J Med Sci. 2000;54:535–40. [PubMed] [Google Scholar]
- 15.Sharma V, Jindal N. In vitro activity of vancomycin and teicoplanin against coagulase negative staphylococci. Oman Med J. 2011;26:186–8. doi: 10.5001/omj.2011.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singhal R, Dhawan S, Mohanty S, Sood S, Dhawan B, Das B, et al. Species distribution & antimicrobial susceptibility of coagulase negative staphylococci in a tertiary care hospital. Indian J Med Res. 2006;123:569–70. [PubMed] [Google Scholar]
- 17.Center KJ, Reboli AC, Hubler R, Rodgers GL, Long SS. Decreased vancomycin susceptibility of coagulase-negative staphylococci in a neonatal intensive care unit: Evidence of spread of Staphylococcus warneri. J Clin Microbiol. 2003;41:4660–5. doi: 10.1128/JCM.41.10.4660-4665.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]


