Abstract
Climate change has the potential to influence the earth's biological systems, however, its effects on human health are not well defined. Developing nations with limited resources are expected to face a host of health effects due to climate change, including vector-borne and water-borne diseases such as malaria, cholera, and dengue. This article reviews common and prevalent infectious diseases in India, their links to climate change, and how health care providers might discuss preventive health care strategies with their patients.
Keywords: Climate change, human health, India, vector-borne disease, water-borne disease
Introduction
Infectious disease distribution involves complex social and demographic factors. These include human population density and behaviour, housing type and location, water supply, sewage and waste management systems, land use and irrigation systems, availability and use of vector control programmes, access to health care, and general environmental hygiene. Meteorological factors that influence transmission intensity of infectious diseases include temperature, humidity, and rainfall patterns. Social and demographic factors such as population growth, urbanization, immigration, changes in land use and agricultural practices, deforestation, international travel, and breakdown in public health services have been mainly responsible for the recent resurgence of infectious diseases1. The Intergovernmental Panel on Climate Change noted in its 2007 report that climate change may contribute to expanding risk areas for infectious diseases such as dengue and may increase the burden of diarrhoeal diseases, putting more people at risk2.
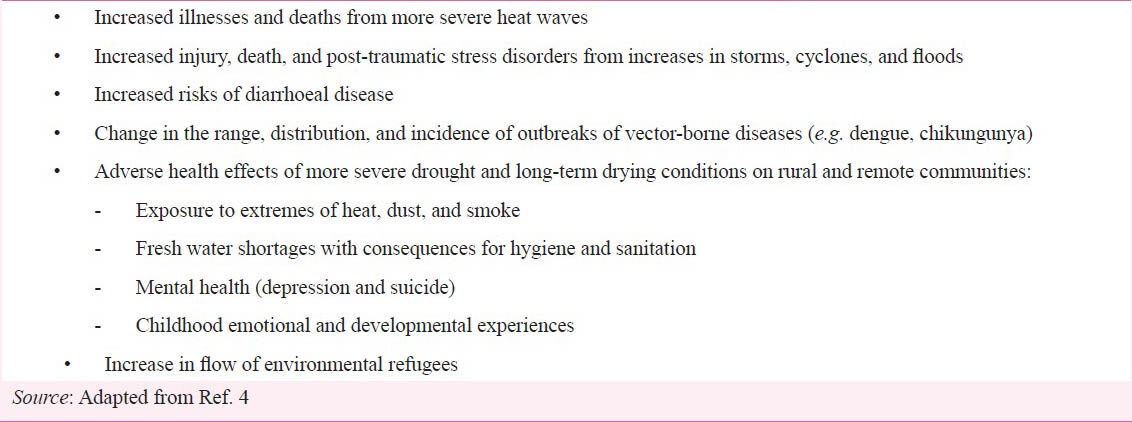
Global climate change is a phenomenon that is now considered strongly associated with human activities. Atmospheric carbon dioxide levels, which have remained steady at 180-220 ppm for the past 420,000 years, are now close to 370 ppm and rising3. Due to improvements in meteorology, we are now able to better understand long-term changes in climate. Such understanding might enable the prediction of where and when infectious disease outbreaks may occur. Box 1 outlines some of the consequences of climate change that clinicians in India could expect to see over the coming years. We describe in this paper these links between climate and health, future implications, and recommendations for clinician-patient interaction.
Box 1.
What clinicians might expect due to climate change
Climate change and health in India
The effects of climate change on human health in India is a broad topic, covering areas from extreme weather events to shifts in vector-borne diseases. In South Asia, scientists predict an increased frequency of floods due to greater intensity of rainfall events and to glacier lake outburst floods (GLOFs) in mountainous regions5. These trends are already being seen. In 2007, floods resulting from monsoon rains killed more than 2,000 persons and displaced more than 20 million persons in Bangladesh, India, and in Nepal6. In the Himalaya region of South Asia, the frequency of GLOFs rose during the second half of the 20th century, and GLOFs have occurred recently in Nepal, India, Pakistan, and Bhutan7,8.
Floods create conducive environments for numerous health consequences resulting from disease transmission. For example, if floodwaters become contaminated with human or animal waste, the rate of faecal-oral disease transmission might increase, allowing diarrhoeal disease and other bacterial and viral illnesses to flourish. Faecal-oral transmission of diseases is of particular concern in regions such as South Asia because of limited access to clean water and sanitation.
In developed countries, flood control efforts, sanitation infrastructure, and surveillance activities to detect and control outbreaks minimize disease risks caused from flooding9. In developing countries, increase in diarrhoeal disease, cholera, dysentery, and typhoid is of specific concern10. For example, after flooding in West Bengal in 1988, cholera was thought to be the cause of an outbreak of diarrhoea that resulted in 276 deaths11. Numerous studies have linked previous floods in Bangladesh and parts of India with outbreaks of diarrhoea as well as respiratory infections12,13,14,15. Flooding can also contribute to increased vector-and rodent-borne and other infectious diseases. For example, collections of stagnant water provide breeding grounds for mosquitoes, potentially aiding in the spread of malaria16. Other studies have linked flooding in Bangladesh and parts of India with outbreaks of rotavirus and leptospirosis17,18,19,20,21.
Rising sea-surface temperatures are expected to increase tropical cyclone intensity and the height of storm surges22. Although cyclones originating in the Bay of Bengal and the Arabian Sea have decreased in frequency since 1970, these have increased in intensity, causing significant damage in India and Bangladesh22,23,24. Public health effects of cyclones include diseases and illnesses associated with the loss of clean water, hygiene, and sanitation, loss of shelter and belongings, population displacement, toxic exposures, and hunger and malnutrition risk due to food scarcity25.
Water-borne diseases
A warmer climate could cause water-borne diseases to become more frequent, including cholera and diarrhoeal diseases such as giardiasis, salmonellosis, and cryptosporidiosis9. Diarrhoeal diseases are already a major cause of morbidity and mortality in South Asia, particularly among children. It is estimated that one-quarter of childhood deaths in South Asia are due to diarrhoeal diseases26. As rising ambient temperatures increase, bacterial survival time and proliferation and thus the incidence of diarrhoeal diseases might further increase27.
Diarrhoeal diseases are largely attributable to unsafe drinking water and lack of basic sanitation; thus, reductions in the availability of freshwater are likely to increase the incidence of such diseases28. Rapid urbanization and industrialization, population growth, and inefficient water use are already causing water shortages in India, Pakistan, Nepal, and Bangladesh6. Climate change will exacerbate the lack of available fresh water as annual mean rainfall decreases in many areas.
Cholera is a well-known water-borne diarrhoeal disease that has afflicted humankind since ancient times. Outbreaks of cholera have occurred in India, Bangladesh, and more recently, Latin America and Africa29. Molecular techniques have shown that bacteria are now recognized as naturally occurring in aquatic environments, with bacterial population peaks in spring and fall in association with plankton blooms29. The discovery of Vibrio cholerae in the natural environment, with a dormant state between epidemics, changed the understanding that this disease had only a human reservoir. A relationship has been observed between increase in sea-surface temperature and the onset of cholera epidemics, with the cholera outbreaks following the seasonal rise and fall in sea-surface height and temperature29. Increases in cholera bacterial populations associated with plankton blooms in spring and summer have been noted off the coasts of several Latin American countries and in Bangladesh29.
Malaria
Malaria is one of the most serious and complex public health problems. About 400-500 million cases of malaria and more than 1 million malaria-related deaths occur globally each year3. Several factors have caused the global resurgence of malaria, including the emergence of insecticide and drug resistance, human population growth and movement, land-use change, and deteriorating public health infrastructure. Changes in temperature, rainfall, humidity, and immunity levels also affect malaria transmission. All these factors can interact to affect adult mosquito densities and the development of the Plasmodium parasite within the mosquito.
Both the parasite and the mosquito that houses the parasite are susceptible to temperature changes. At temperatures close to the physiological tolerance limit of the parasite, a small increase in temperature can kill the parasite, thereby decreasing malaria transmission. At lower temperatures, however, a small increase in temperature can greatly increase the risk of malaria transmission due to increased numbers of mosquitoes3. Other environmental changes can also affect malaria transmission. For example, deforestation might elevate local temperatures and changes in housing types might change indoor temperatures where vectors spend most of the time resting. Deforestation, vegetation clearance, and irrigation can form open pools preferred by malaria vectors and thus increase transmission.
In South Asia, malaria is one of the most pertinent examples of increased occurrence of a vector-borne disease. Malaria is already one of the most important vector-borne diseases in India, Bangladesh, and Sri Lanka; changes in temperature and precipitation patterns have the potential to expand the geographical range of malaria into temperate and arid parts of South Asia9. For example, in India malaria distribution is expected to expand to higher latitudes and altitudes. Because the relationship between climate and disease distribution is complex, in some areas increasing temperatures may restrict malaria transmission. Reductions in transmission intensity in endemic areas might lead to greater proportions of the population losing immunity, resulting in epidemics in later years30.
Currently, all of India's population is at risk for contracting malaria except for those in the areas above 1700 m above sea surface. More than 973 million persons are exposed to vector-borne malarial parasites in India, and in 1998 an estimated 577,000 disability adjusted life years (DALYs) were lost due to malaria31.
The multifactorial nature of malaria causation does not lend itself easily to a simple model of disease prediction. To determine the role of climate change in malaria transmission, research efforts will be required that incorporate a disease surveillance system combining trend analyses from multiple sites to account for local factors. The first operationally useful early warning system for epidemic malaria was implemented in India32. The system combined human and meteorologic factors to provide about a month's lead-time of epidemic risk. Rainfall alone accounted for about 45 per cent of the variation in malaria transmission32. By the 2050s, the geographic range of malaria vectors is projected to shift away from central regions toward southwestern and northern States32. The duration of the transmission window is likely to widen in northern and western States and shorten in southern States. Malaria is likely to persist in Orissa, West Bengal, and southern parts of Assam. It might shift from central India to the southwestern coastal States (Maharashtra, Kerala, and Karnataka). The northern States might also become prone. The duration of exposure is likely to widen in north and west India, and shorten in south India33.
Other vector-borne and zoonotic diseases
Climate change might affect other diseases endemic to South Asia. These include mosquito-borne diseases such as chikungunya fever and dengue, parasitic diseases such as leishmaniasis, lymphatic filariasis and onchocerciasis, and tick-borne diseases, which may exhibit changes in transmission intensity or shifts in their geographical ranges due to the impact of climate on the relevant vector populations. Climatic factors might also influence human plague, a bacterial disease carried by rodents and transmitted by fleas. Temperature and rainfall are important determinants of rodent population abundance and distribution. Combined with the influence of temperature and humidity on flea survival and development, changes in any of these climatic components may result in changes in plague incidence30. Murine typhus, a rickettsial disease, is also transmitted by fleas and thus may exhibit similar climate sensitivity30.
The arboviral diseases chikungunya and dengue may also be influenced by climate, as both are transmitted by the common vector Aedes aegypti. The first reported outbreak of chikungunya in India was in 1963 in Calcutta (now Kolkata), with transmission continuing until 197334. The virus reemerged in 2005, and has since spread rapidly, with more than one million cases reported - despite no standardized surveillance system for the disease34,35. Dengue has also been a significant problem, with more than 50 dengue outbreaks reported in India since 196036. The activity, abundance, distribution, and ability to transmit viruses is influenced by temperature and precipitation30.
Summary and implications for health care systems and providers
As a developing country with high population density, India might experience myriad human health effects because of climate change. These effects could include infectious diseases such as malaria, chikungunya, and water-borne illnesses. Monitoring the spread of infectious diseases will require early warning systems, which have both health and economic benefits. Increases in extreme weather events will also have health consequences. Displacements due to the loss of housing, hunger, and injuries are some of the adverse outcomes to the population.
Health care providers will need to address at the primary level the negative health outcomes associated with climate change in India. Physicians should expect increasing cases of the infectious diseases. There will likely be a rise in demand for emergency medicine services such as urgent and ambulatory care37. Emerging vector-borne diseases may first appear at these emergency care facilities. Expanded surveillance activities could detect shifting patterns of disease distribution so that emergency department personnel would be aware of emerging threats. Many other fields of health care in India could be impacted by climate change, including family practice, internal medicine, paediatrics, geriatrics, and psychiatry37.
The Climate and Health Council of the General Medical Council of the United Kingdom38 has outlined several actions that health care providers can take, many of which are relevant to providers in India39. These include informing professional colleagues and the wider community about the health consequences of climate change, and advocating for carbon reductions to promote human health. Several recommendations have been made for health system preparedness, some of which are relevant for Indian hospitals39. These include undertaking energy audits, pursuing energy and water conservation and energy efficient construction. A review of overall emissions from petroleum-based energy sources such as diesel generators and hospital transportation systems is a key first step. Contingency plans for alternative methods of energy generation during electricity blackouts, particularly during the summer months, will facilitate preparedness for these events. To reduce waste, Health Care Without Harm has recommended several options: recycle and buy recycled products, collect and recycle nitrous oxide and anaesthetic gases, prevent waste, and dispose of waste locally40. Using native vegetation and planting trees on site can mitigate the heat-island effect. Vegetation lowers ground level temperatures near buildings, reducing the buildings’ cooling load, energy requirements, and greenhouse gas emissions. Such measures improve health by reducing ground-level smog formation. Smog leads to respiratory symptoms and illness. Native vegetation requires less water and attracts beneficial insects, thus eliminating pesticide use.
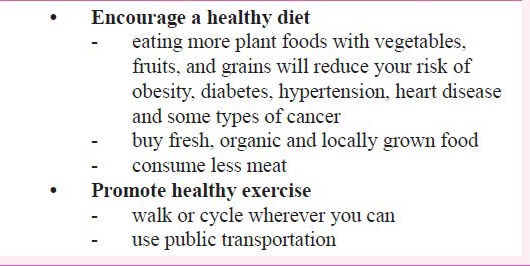
Climate impacts in India will not be uniform. Those of low socio-economic status will likely to be the most affected by the health impacts of climate change, as they have the least adaptive capacity4. As India's economy continues to expand, the growing middle class presents a unique situation. While rising out of poverty will improve sanitation levels and living conditions, thus increasing resilience to infectious diseases, it will also lead to higher consumption patterns that can initiate new health problems while leading to more carbon pollution. Box 2 outlines some of the topics health care providers can discuss with their patients to help maximize the benefits. General practitioners as well as specialists both can play a role in anticipating the health effects of climate change and improving the health through discussing effective preventive health care with their patients.
Box 2.
Discussing climate change effects with patients
References
- 1.Washington, DC: The National Academics Press; 2003. National Research Council. Microbial threats of health: Emergence, detection and response. [PubMed] [Google Scholar]
- 2.Confalonieri U, Menne B, Akhtar R, Ebi KL, Hauengue M, Kovats RS, et al., editors. Cambridge, UK: Cambridge University Press; 2007. Human health. Climate change 2007: Impacts, adaptation and vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. [Google Scholar]
- 3.Houghton JT, Ding Y, Griggs DJ, Noguer M, van der Linden PJ, Dai X, Maskell K, Johnson CA, editors. Cambridge, United Kingdom: Cambridge University Press; 2001. Intergovernmental Panel on Climate Change (IPCC). Climate change 2001: The scientific basis. Contribution of Working Group I to the Third Assessment Report of the Intergovernmental Panel on Climate Change; p. 881. [Google Scholar]
- 4.Blashki G. Climate change and primary health care. Aust Fam Physician. 2007;36:986–9. [PubMed] [Google Scholar]
- 5.Cruz RV, Harasawa H, Lal M, Wu S, Anokhin Y, Punsalmaa B, et al. Climate change 2007: Impacts, adaptation and vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. In: Parry ML, Canziani OF, Palutikof FP, van der Linden PJ, Hanson CE, editors. Cambridge, UK: Cambridge University Press; 2007. pp. 469–506. [Google Scholar]
- 6. [accessed on October 18, 2013]. Available from: http://www.unicef.org/media/media40495.html .
- 7.Bajracharya SR, Mool PK, Shrestha BR. Nepal: Nepal Engineering College, Ehime College and National Society for Earthquake Technology; 2006. The impact of global warming on the glaciers of the Himalaya. International symposium on Geo-disasters, infrastructure management and protection of world heritage sites, November 25-26; pp. 231–42. [Google Scholar]
- 8.New Delhi: WHO/SEARO; 2009. WHO/SEARO. Protecting human health from climate change, Report of the Technical Discussions. [Google Scholar]
- 9.Hales S, Edwards SJ, Kovats RS. Impacts on health of climate extremes. In: McMichael AJ, Campbell-Lendrum DH, Corvalan CF, Ebi KL, Githeko A, Scheraga JD, Woodward A, editors. Climate change and human health: Risks and responses. Geneva, Switzerland: World Health Organization; 2003. pp. 79–102. [Google Scholar]
- 10.Morgan O, Ahern M, Cairncross S. Revisiting the Tsunami: Health consequences of flooding. PLoS Med. 2005;2:491–3. doi: 10.1371/journal.pmed.0020184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sur D, Dutta P, Nair G, Bhattacharya S. Severe cholera outbreak following floods in a northern district of West Bengal. Indian J Med Res. 2000;112:178–82. [PubMed] [Google Scholar]
- 12.Siddique AK, Baqui AH, Eusof A, Zaman K. 1988 floods in Bangladesh: pattern of illness and causes of death. J Diarrhoeal Dis Res. 1991;9:310–4. [PubMed] [Google Scholar]
- 13.Kunii O, Nakamura S, Abdur R, Wakai S. The impact on health and risk factors of the diarrhoea epidemics in the 1998 Bangladesh floods. Public Health. 2002;116:68–74. doi: 10.1038/sj.ph.1900828. [DOI] [PubMed] [Google Scholar]
- 14.Biswas R, Pal D, Mukhopadhyay SP. A community based study on health impact of flood in a vulnerable district of West Bengal. Indian J Public Health. 1999;43:89–90. [PubMed] [Google Scholar]
- 15.Mondal NC, Biswas R, Manna A. Risk factors of diarrhea among flood victims: a controlled epidemiological study. Indian J Public Health. 2001;45:122–7. [PubMed] [Google Scholar]
- 16.Ahern MJ, Kovats RS, Wilkinson P, Few R, Matthies F. Global health impact of floods: epidemiological evidence. Epidemiol Rev. 2005;27:36–45. doi: 10.1093/epirev/mxi004. [DOI] [PubMed] [Google Scholar]
- 17.Fun BN, Unicomb L, Rahim Z, Banu NN, Podder G, Clemens J. Rotavirus-associated diarrhea in rural Bangladesh: two-year study of incidence and serotype distribution. J Clin Microbiol. 1991;29:1359–63. doi: 10.1128/jcm.29.7.1359-1363.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leptospirosis, India. Report of the investigation of a postcyclone outbreak in Orissa, November 1999. Wkly Epidemiol Rec. 2000;75:217–23. [PubMed] [Google Scholar]
- 19.Sehgal SC, Sugunan AP, Vijayachari P. Outbreak of leptospirosis after the cyclone in Orissa. Natl Med J India. 2002;15:22–3. [PubMed] [Google Scholar]
- 20.Karande S, Bhatt M, Kelkar A, Kulkakrni M, De A, Varaiya A, et al. An observational study to detect leptospirosis in Mumbai, India, 2000. Arch Dis Child. 2003;88:1070–5. doi: 10.1136/adc.88.12.1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karande S, Kulkarni H, Kulkarni M, De A, Varaiya A. Leptospirosis in children in Mumbai slums. Indian J Pediatr. 2002;69:855–8. doi: 10.1007/BF02723705. [DOI] [PubMed] [Google Scholar]
- 22.Ali A. Climate change impacts and adaptation assessment in Bangladesh. Climate Res. 1999;12:109–16. [Google Scholar]
- 23.Lal M. Tropical cyclones in a warmer world. Curr Sci. 2001;80:1103–4. [Google Scholar]
- 24.Lal M. Global climate change: India's monsoon and its variability. J Environ Stud Policy. 2003;6:1–34. [Google Scholar]
- 25.Keim ME. Cyclones, Tsunamis, and human health: The key role of preparedness. Oceanography. 2006;19:40–9. [Google Scholar]
- 26.Zaidi AKM, Awasthi S, deSilva HJ. Burden of infectious diseases in South Asia. BMJ. 2004;328:811–5. doi: 10.1136/bmj.328.7443.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Checkley W, Epstein LD, Gilman RH, Figueroa D, Cama RI, Patz JA, et al. Effects of El Nino and ambient temperature on hospital admissions for diarrheal diseases in Peruvian children. Lancet. 2000;355:442–50. doi: 10.1016/s0140-6736(00)82010-3. [DOI] [PubMed] [Google Scholar]
- 28.Ezzati M, Lopez A, Rodgers A, Murray C, editors. 1 and 2. Geneva: World Health Organization; 2004. Comparative quantification of health risks: Global and regional burden of disease due to selected major risk factors. [Google Scholar]
- 29.Lipp E, Huq A, Colwell R. Effects of global climate on infectious disease: the cholera model. Clin Microbiol Rev. 2002;15:757–70. doi: 10.1128/CMR.15.4.757-770.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gage KL, Burkot T, Eisen RJ, Hayes N. Climate and vector-borne diseases. Am J Prev Med. 2008;35:436–50. doi: 10.1016/j.amepre.2008.08.030. [DOI] [PubMed] [Google Scholar]
- 31.Garg A, Dhiman RC, Bhattacharya S, Shukla PR. Development, malaria and adaptation to climate change: A case study from India. Environ Manage. 2009;43:779–89. doi: 10.1007/s00267-008-9242-z. [DOI] [PubMed] [Google Scholar]
- 32.Kiszewski A, Mellinger A, Spielman A, Malaney P, Sachs E, Sachs J. A global index representing the stability of malaria transmission. Am J Trop Med Hyg. 2004;70:486–98. [PubMed] [Google Scholar]
- 33.Bhattacharya S, Sharma C, Dhiman RC, Mitra AP. Climate change and malaria in India. Curr Sci. 2006;90:369–75. [Google Scholar]
- 34.Mavalankar D, Shastri P, Raman P. Chikungunya epidemic in India: a major public-health disaster. Lancet Infect Dis. 2007;7:306–7. doi: 10.1016/S1473-3099(07)70091-9. [DOI] [PubMed] [Google Scholar]
- 35.Epstein Paul R. Chikungunya fever resurgence and global warming. Am J Trop Med Hyg. 2007;76:403–4. [PubMed] [Google Scholar]
- 36.Majra JP, Gur A. Climate change and health: Why should India be concerned? Indian J Occup Environ Med. 2009;13:11–6. doi: 10.4103/0019-5278.50717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hess JJ, Heilpern KL, Davis TE, Frumkin H. Climate change and emergency medicine: Impacts and opportunities. Acad Emerg Med. 2009;16:782–94. doi: 10.1111/j.1553-2712.2009.00469.x. [DOI] [PubMed] [Google Scholar]
- 38.Gill M, Godlee F, Horton R, Stott R. Doctors and climate change. BMJ. 2009;335:1104. doi: 10.1136/bmj.39412.488021.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jackson R, Shields KN. Preparing the U.S. health community for climate change. Annu Rev Public Health. 2008;29:57–73. doi: 10.1146/annurev.publhealth.29.020907.090755. [DOI] [PubMed] [Google Scholar]
- 40.Health Care Without Harm. Addressing Climate Change in the Health Care Setting: Opportunities for Action. [accessed on January 9, 2012]. Available from: http://www.noharm.org/lib/downloads/climate/Addressing_Climate_Change.pdf .


