Abstract
Introduction
Systemic inhibition of the inflammatory enzyme cyclooxygenase (COX) 2 decreases the risk of breast cancer and its recurrence. However, the biology of COX-2 in the multicellular tumor microenvironment is poorly defined.
Methods
Mammary tumor onset and multiplicity were examined in ErbB2 transgenic mice that were deficient in mammary epithelial cell COX-2 (COX-2MECKO) compared to wild type (WT) mice.
Tumors were analyzed, by real time PCR, immune-staining and flow cytometry, for proliferation, apoptosis, angiogenesis and immune microenvironment. Lentiviral shRNA delivery was used to knock down (KD) COX-2 in ErbB2-transformed mouse breast cancer cells (COX-2KD), and growth as orthotopic tumors was examined in syngenic recipient mice, with or without depletion of CD8+ immune cells.
Results
Mammary tumor onset was delayed, and multiplicity halved, in COX-2MECKO mice compared to WT. COX-2MECKO tumors showed decreased expression of Ki67, a proliferation marker, as well as reduced VEGFA, its receptor VEGFR2, endothelial NOS and the vascular endothelial marker CD31, indicating reduced tumor vascularization. COX-2MECKO tumors contained more CD4+ T helper (Th) cells and CD8+ cytotoxic immune cells (CTL) consistent with increased immune surveillance. The ratio of Th markers Tbet (Th1) to GATA3 (Th2) was higher, and levels of Retnla, a M2 macrophage marker, lower, in COX-2MECKO tumor infiltrating leukocytes compared to WT, suggesting a prevalence of pro-immune Th1 over immune suppressive Th2 lymphocytes, and reduced macrophage polarization to the immune suppressive M2 phenotype. Enhanced immune surveillance in COX-2MECKO tumors was coincident with increased intratumoral CXCL9, a T cell chemoattractant, and decreased expression of T lymphocyte co-inhibitory receptors CTLA4 and PD-1, as well as PD-L1, the ligand for PD-1. PD-L1 was also decreased in IFNγ-treated COX-2KD mouse mammary cancer cells in vitro and, compared to control cells, growth of COX-2KD cells as orthotopic tumors in immune competent mice was markedly suppressed. However, robust growth of COX-2KD tumor cells was evident when recipients were depleted of CD8+ cells.
Conclusions
The data strongly support that, in addition to its angiogenic function, tumor cell COX-2 suppresses intratumoral cytotoxic CD8+ immune cell function, possibly through upregulation of immune checkpoints, thereby contributing to tumor immune escape. COX-2 inhibition may be clinically useful to augment breast cancer immunotherapy.
Keywords: breast cancer, immune modulation, tumor microenvironment, cytotoxic immune cells, PD-L1
Introduction
The inducible form of cyclooxygenase (COX), COX-2, and one of its pro-inflammatory products, prostaglandin (PG) E2, are strongly implicated in a range of human cancers including breast cancer [1,2]. Global deletion or pharmacological inhibition of COX-2 suppressed tumorigenesis in mice [3,4] and humans [5]. PGE2 signals through multiple pro-tumor pathways, including PI3K/AKT, RAS-MAPK/ERK and Gs-axin-ß-catenin signaling, to increase tumor cell survival, inhibit apoptosis, increase cancer cell motility, stimulate angiogenesis and inhibit immune surveillance [6].
In the last decade it has become clear that the tumor microenvironment is critical for tumors to survive and progress. In addition to vascular supply, the interplay of tumor cells with non-malignant cells in the stroma provides growth, survival and motility advantages. A central part of the tumor microenvironment is infiltration of immune cells, which can positively or negatively influence tumor progression depending on their differentiation [7,8]. Tumor rejection is favored through T helper 1 (Th1)-derived cytokines that drive antigen-presenting and pro-immune M1 macrophage functions, and by the direct tumoricidal actions of CD8+ cytotoxic T lymphocytes (CTLs) and natural killer (NK) cells [6]. However, as tumors progress, soluble mediators and cellular interactions are thought to reprogram immune cells to type 2 functions so that Th2 lymphocyte-derived cytokines polarize macrophages to the M2 phenotype to suppress CTLs, promote angiogenesis and support tumor growth [6,9]. In breast cancer, poor prognosis is associated with elevated Th2 lymphocytes and tumor-associated macrophages (TAM), while Th1 lymphocytes, CTLs and NKs correlate with enhanced survival [8,10], raising intense interest in therapeutic approaches to modify the tumor immune microenvironment. COX-2-derived PGE2 has emerged as a tumor-derived mediator that contributes to development of immune tolerance [11-13]. Several studies report the association of tumor COX-2 with infiltrating T cells, dendritic cells, myeloid derived suppressor cells and macrophages [14-17], while PGE2 has been linked to immune suppression in hepatocellular carcinoma [18], lung [19], ovarian [20] and breast [14,15] cancers. The mechanisms through which COX-2/PGE2 suppress immune function are poorly defined; however, PGE2 suppressed the ability of mature CTLs to kill murine plasmocytoma cells [21] and inhibited Th1 generation of interferon γ (IFNγ) [22,23], a cytokine that is critical to sustain anti-tumor immune function [6,24].
We reported that selective deletion of mammary epithelial cell (MEC) COX-2 (COX-2MECKO) delayed carcinogen-induced mammary tumor onset coincident with enhanced markers of anti-tumor type 1 immunity [17]. Chemical carcinogens are generally not, however, considered significant in human breast cancer etiology; therefore, in the current study, we investigated the role of tumor cell COX-2-derived mediators in ErbB2 (HER-2/neu)-induced mammary tumorigenesis. ERBB2 gene amplification or overexpression of the HER-2 protein has been identified in 25% to 34% of human breast cancers [25,26]. ErBb2 mouse models show remarkable morphological resemblance to some forms of human breast cancer and accurately recapitulate the hallmark changes associated with the early stages of human breast cancer [27]. In COX-2MECKO mice transgenic for an activated ErbB2 mutant, we determined delayed tumor onset and reduced tumor multiplicity, as well as reduced tumor vascularization, compared to wild type (WT). Deletion of COX-2 in tumor cells also significantly impaired maintenance of pro-tumorigenic lymphoid and myeloid cell functions thereby facilitating enhanced immune surveillance.
Methods
Mice and tumor tissue collection
All procedures were conducted in accordance with National Institutes of Health regulations and were approved by the Institutional Animal Care and Use Committee of the University of Pennsylvania.
Floxed COX-2 mice, generated by flanking the COX-2 gene between introns 5 and 8 with loxP sites (COX-2flox/flox), were backcrossed fully (>9 generations) onto an FVB background and are denoted as wild type (WT) mice. COX-2flox/flox mice were crossed with FVB mice expressing Cre-recombinase under control of the mouse mammary tumor virus (mmtv) promoter (Cremmtv), which is used widely to target transgene expression to MEC. The resulting mice were termed COX-2MECKO and their characterization is described in our previous work [17]. WT and COX-2MECKO were crossed with mice transgenic for the ErbB2 (HER2/c-neu) oncogene carrying Eactivating Val664 to Glu664 mutation (Jackson Laboratory, Bar Harbor, ME, USA), also expressed under the control of mmtv promoter. Genotype verification was performed by conventional PCR using primers listed in Table 1.
Table 1.
Genotyping primer sequences
| Gene | Forward (F) and Reverse (R) primer sequences |
|---|---|
| COX-2 | F:TGA GGC AGA AAG AGG TCC AGC CTT |
| R:ACC AAT ACT AGC TCA ATA AGT GAC | |
| Cremmtv | F:TCG ATG CAA CGA GTG ATG AGG |
| R:ACG AAC CTG GTC GAA ATC AGT | |
| Erbb2 | F:GGACATCCAGGAAGTTCAGGGTTAC |
| R:ACAGGAGCCAGTTGGTTATTCTTG |
Mice were palpated weekly and considered tumor bearing if a palpable mammary mass persisted for more than one week. On necropsy, tumors were counted and isolated from surrounding tissues, after which they were either frozen and stored at -80°C for RNA extraction or fixed in Prefer (Anatech, Battle Creek, MI, USA) overnight and paraffin embedded or digested to obtain single cell suspension for flow cytometry and microbead separation. For tissue digestion, tumors were washed with (D)MEM/F12 + 5% fetal bovine serum (FBS) + gentamycin 50 mg/ml, minced and placed in digestion buffer consisting of 9 parts of wash buffer +1 part collagenase/hyaluronidase (StemCell Technologies, Vancouver, BC Canada). After two hours shaking at 37°C, the suspensions were centrifuged at 1,000 rpm for five minutes. Pellets were washed and treated with red cell lysis buffer (1 part HBSS+2%FBS + 3 parts NH4Cl) and then with Trypsin-ethylenediaminetetraacetic acid (EDTA) 0.25% (Gibco, Grand Island, NY, USA), followed by Dispase and DNase (StemCell Technologies). Thereafter, cell pellets were passed through a 40 μm cell strainer, counted and re-suspended either in fluorescence-activated cell sorting (FACS) buffer for flow cytometry (description below) or in degassed MACS buffer (PBS + 0.5% BSA + 2 mM EDTA) for positive selection of CD45+ cells using CD45-microbeads (Miltenyi Biotec, Auburn, CA, USA) according to the manufacturer's instructions.
NAF mammary tumor cell line culture, transduction, and treatments
The NAF tumor cell line, which was generated from mammary tumors of ErbB2-transgenic mice, was kindly provided by Dr. Lewis Chodosh (University of Pennsylvania). NAF were cultured in (D)MEM medium containing 10% FBS, 1% L-glutamine and 1% penicillin/streptomycin. For viral transduction, 15,000 cells/well were plated on 96-well plates. Mission plKO.1-puro Transduction Lentiviral Particles (20 μl), carrying either non-target control small hairpin RNA (shRNA) or COX-2 shRNA (Sigma, St. Louis, MO, USA), at 1 × 107 TU/ml were added to the wells with 8 μg/ml protamine sulfate. After 18 hours, lentiviral particles were removed and cells kept in medium containing 2 μg/ml puromycin (Sigma) to select for transduced cells. COX-2 knock down in COX-2 shRNA transduced NAF cells (NAF COX-2KD) compared to non-target shRNA transduced cells (NAF nt) was verified by Q-PCR. Cells were serum starved for 24 hours and then treated with 10 ng/ml IFNγ(PeproTech, Rocky Hill, NJ, USA ), with or without 250 nM PGE2 (Cayman Chemicals, Ann Arbor, MI, USA). Fresh IFNγ and PGE2 were added 24 hours later, and cells were harvested (0.25% Trypsin-EDTA) after 48 hour treatment, washed and re-suspended in FACS buffer for flow cytometry analysis.
Bone marrow-derived macrophage isolation and culture
Bone marrow-derived macrophages (BMDM) were isolated as described [28]. Femurs from female mice were flushed with (DMEM and cells pelleted (1,000 rpm) and incubated at 37°C for 24 hours in (DMEM containing 10% FBS, 1% L-glutamine, and 1% penicillin/streptomycin. Non-adherent cells were collected and plated in L929 cell-conditioned medium (LCCM). To make LCCM, medium collected from L929 cells (American Type Culture Collection, Manassas, VA, USA), that were split 1:5 and grown to confluency, was mixed 1:5 with (DMEM with 10% FBS, 1% L-glutamine, and 1% penicillin/streptomycin. Purity (approximately 99%) was verified by flow cytometry for F4/80 and CD11b (not shown). BMDM were plated (0.5 × 106 cells/well) in LCCM. At 100% confluency, media was replaced with (DMEM. After 24 hours, cells received vehicle, or M1 polarizing mix (100 ng/ml lipopolysaccharide (LPS; Sigma) and 20 ng/ml IFNγ (Peprotech)), or M2 polarizing mix (20 ng/mL IL-4 and 10 ng/mL IL-13; Peprotech), with or without 250 nM PGE2 (Cayman Chemicals). Supernatants were removed 18 hours later and cells lysed for RNA isolation.
Real Time RT-PCR
Total RNA from tumors and cells was isolated (RNeasy, Qiagen, Germantown, MD, USA), and reverse transcribed (TaqMan Reverse Transcriptase, Applied Biosystems, Carlsbad, CA, USA), according to the manufacturer's instructions. Real time quantitative (Q)-PCR of all genes, including 18S ribosomal RNA, was performed using inventoried gene expression assays and TaqMan Universal PCR Master Mix from Applied Biosystems. PCR products were detected in ABI-PRISM 7900 sequence detection systems (Applied Biosystems). Results were analyzed using the comparative Ct method, and normalized to 18S RNA.
Immunohistochemistry
Paraffin embedded tumor tissues were sectioned (4 μm). After de-paraffinization and rehydration, endogenous peroxidase was blocked with 3% hydrogen peroxide. Heat induced epitope retrieval was performed with 1 mM EDTA (Invitrogen, Grand Island, NY, USA). After overnight blocking at 4°C with 5% donkey serum (Sigma) + 0.1% Triton 100× (Sigma), sections were incubated with primary antibodies overnight at 4°C as follows: anti-Ki67 (Abcam, Cambridge, MA, USA,1:50 dilution), anti-CD31 (Abcam, 1:200 dilution) or anti-CXCL9 (Aviva Systems Biology, San Diego, CA, USA 1:125 dilution). Thereafter, the Polink-2 HRP Plus AEC System for Immunohistochemistry (Golden Bridge International, Inc, Mukillteo, WA, USA) was used, according to the manufacturer's instructions. Slides were then counterstained with hematoxylin (Vector Laboratories, Burlingame, CA, USA), and mounted (Aqua-Mount; Lerner Laboratories, Pittsburgh, PA, USA). Images were taken with a Nikon Eclipse E600 microscope using ACT-1 imaging program (Nikon Instruments Inc., Hicksville, NY, USA).
Flow cytometry
Single cell suspensions from tumor digestions (above) were centrifuged, washed and re-suspended in FACS buffer (PBS + 2% FBS +1 mM EDTA + 0.01% sodium azide), 1 × 106 cell/100 μl/tube. After a five minute incubation with rat anti-mouse CD16/CD32 (Mouse BD Fc Block, BD Pharmingen, Franklin Lakes, NJ, USA), 1 μg/ml of fluorescein isothiocyanate (FITC) conjugated anti-CD3, PE conjugated anti-CD4, and AF647 conjugated anti-CD8a, or PE conjugated anti-F4/80 and AF647 conjugated anti-CD86 antibodies (Invitrogen) were added. OneComp eBeads (eBioscience, San Diego, CA, USA) were incubated with anti-CD3 or anti-CD4 or anti-CD8a antibodies to perform compensation for spectral overlap. NAF COX-2KD and NAF nt (1 × 106 cell/100 μl), were incubated with PE conjugated anti-PD-L1 antibody (Biolegend, San Diego, CA USA). After a 30-minute incubation, cells were washed and re-suspended in 500 μl FACS buffer. Unstained tumor cells and cells incubated with isotype control rat anti-mouse antibody were used as negative controls. FACS analysis was performed on a BD FACSCalibur machine (BD Biosciences, San Jose, CA, USA). Data was analyzed using FlowJo Research Flow Cytometry Analysis Software (TreeStar, Ashland, OR USA).
Orthotopic tumor growth and CD8+ depletion
NAF COX-2KD and NAF nt tumor cells were injected into the #4 and #9 mammary glands (1 × 106 cells/gland in 100 μl Hanks Balanced Salt Solution) of normal WT female mice between 8 to 14 weeks of age. Orthotopic tumor volume was determined weekly using standard caliper measurement. For CD8+ depletion experiments, mice were injected intraperitoneally with 200 μg of an anti-CD8 or isotype control antibody (BioXCell, West Lebanon, NH, USA), four days and again two days prior to injection of tumor cells, and then twice weekly for a further four weeks. Depletion of CD8+ cells was confirmed by flow cytometry of erythrocyte lysed whole blood (ACK Lysing Buffer, Invitrogen), four days and again four weeks after tumor cell injections.
Statistical analysis
Statistical analyses were performed using Prism (GraphPad Software, Inc., La Jolla, CA, USA). As appropriate, comparisons were made using logrank analysis, unpaired t-test (with Welch's correction when variances were significantly different by F-test), Mann Whitney test (when the data distribution was not normal), or, for multiple group comparisons, analysis of variance (ANOVA) followed by Bonferroni's multiple comparison test.
Results
Tumor onset, development, and vascularization in WT and COX-2 MECKO mice
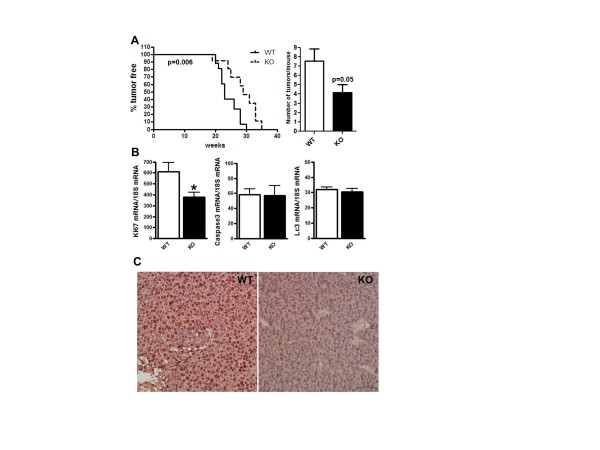
The current investigation was designed to study the role of MEC COX-2 in mammary tumor development, with the goal of elucidating whether and how targeted inhibition of COX-2 in epithelial cells affects the disease. In our previous study we confirmed COX-2 deletion in MEC isolated from COX-2MECKO mice by Q-PCR and Western blotting, and loss of PGE2 generation by COX-2MECKO cells was established by mass spectrometry [17]. COX-2 expression and PGE2 production were unchanged in peripheral macrophages isolated from COX-2MECKO compared to WT confirming the selectivity of the deletion [17]. In the current study, tumor onset was significantly delayed in COX-2MECKO mice compared to their WT littermates (Figure 1A). On necropsy, COX-2MECKO mice had significantly fewer tumors compared to WT (Figure 1A). Consistent with these observations, cell proliferation appeared higher in WT tumors, as indicated by higher levels of mRNA for the proliferation marker Ki67 in WT compared to COX-2MECKO tumors (Figure 1B). Markers for apoptosis (caspase3) and autophagy (Lc3) were not different between the two genotypes (Figure 1B). Abundant expression of Ki67 protein in WT, but not COX-2MECKO, tumors was confirmed by immunohistochemistry (Figure 1C).
Figure 1.
Tumor onset, multiplicity and cell proliferation were suppressed in COX-2MECKO tumors. COX-2MECKO tumors are denoted as KO. (A) Percent of tumor free mice against weeks of age. Mean tumor free time for COX-2MECKO mice was 29 weeks versus 23 weeks for WT (left graph, n = 13 to 19). The right graph shows tumor multiplicity as number of tumors per mice at necroscopy (n = 14 to 18). (B) Gene expression levels of Ki67 (proliferation), Caspase3 (apoptosis) and Lc3 (autophagy) in whole tumors by Q-PCR (n = 8 to 18). (C) Immunohistochemistry staining for Ki67 (dark red-brown) in sections of paraffin embedded WT and COX-2MECKO tumors (image shown is representative of n = 4). Cell nuclei are counterstained with hematoxylin. The bar on the KO panel indicates 20× magnification. Data in column graphs are mean ± sem. P values are compared to WT; *P < 0.05. COX, cyclooxygenase; KO, knock out; WT, wild type.
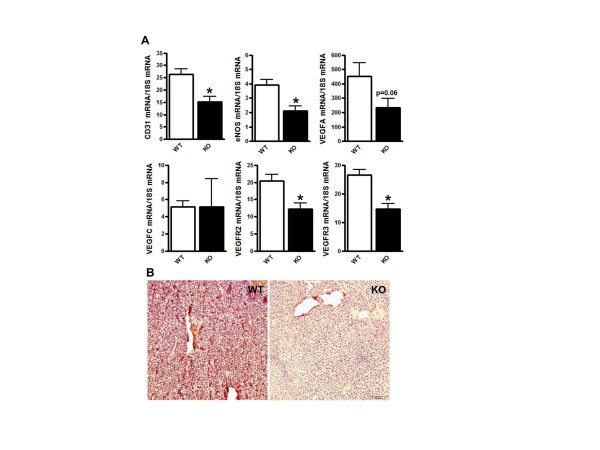
Q-PCR analysis of tumors revealed lower expression levels of CD31, an endothelial marker, endothelial (e) NOS, the angiogenic factor VEGFA and its receptor VEGFR2 (Figure 2A), in COX-2MECKO compared to WT. Although no difference was observed in mRNA levels of the lymphangiogenic factor VEGFC, its receptor VEGFR3 was significantly lower in COX-2MECKO tumors (Figure 2A). Immunostaining for CD31 revealed a denser blood vessel network in WT tumors, confirming suppressed angiogenesis in COX-2MECKO tumors (Figure 2B).
Figure 2.
Angiogenesis was suppressed in COX-2MECKO tumors. COX-2MECKO tumors are denoted as KO. (A) Gene expression levels for CD31, eNOS, VEGFA, VEGFC, VEGFR2 and VEGFR3 in whole tumors by Q-PCR. Data are mean ± sem of n = 8 to 18. P values are compared to WT. *P < 0.05. (B) Immunohistochemistry staining for CD31 (dark red-brown) in sections of paraffin embedded WT and COX-2MECKO tumors (image is representative of n = 6). Cell nuclei are counterstained with hematoxylin. The bar on the KO panel indicates 20× magnification. COX, cyclooxygenase; KO, knock out; WT, wild type.
Subpopulations and phenotypes of tumor infiltrating immune cells in WT and COX-2MECKO tumors
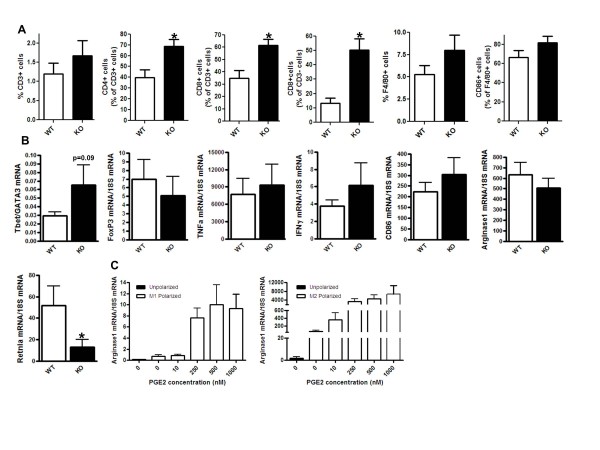
WT and COX-2MECKO tumors were analyzed by flow cytometry and Q-PCR to compare the populations of infiltrating immune cells and their phenotypes. By flow cytometry, there was no difference in the total number of F4/80+ TAMs between WT and COX-2MECKO tumors (Figure 3A). COX-2MECKO tumors did, however, have significantly higher numbers of CD3+CD4+ cells, a population that includes Th1, Th2, and regulatory T (Treg) cells, as well as CD3+CD8+ CTLs and CD3-CD8+ cells, encompassing NK and dendritic cells (Figure 3A). To further define their functional identify, tumor-infiltrating leukocytes (TILs) were isolated using magnetic microbeads coated with a pan-leukocyte marker CD45 and cells analyzed by Q-PCR for phenotypic markers and cytokines (Figure 3B). The ratio of Tbet (Th1 marker)/GATA3 (Th2 marker) tended to be higher in COX-2MECKO tumors compared to WT (Figure 3B), suggesting a prevalence of CD3+CD4+ Th1 over Th2 lymphocytes, when MEC COX-2-derived mediators are absent. Further, mRNA levels for either Tbet alone or the Tbet/GATA3 ratio were significantly correlated with CD4 mRNA in COX-2MECKO, but not WT, tumors (data not shown). Gene expression of FoxP3, a marker for Treg, was not altered and there was no difference in mRNA for macrophage type 1 cytokines TNFα and IFNγ or an M1 macrophage marker CD86, in CD45+ TILs, suggesting no major change in M1 polarization in this disease model. COX-2-derived PGE2 has been implicated in driving the immune suppressive phenotype typically associated with TAM [6]. Indeed, exogenous PGE2 treatment significantly increased the expression of M2 marker Arginase 1, a key enzyme in suppression of T cell function, in both M1 and M2 polarized bone-marrow derived macrophages (Figure 3C). In tumors, although arginase 1 mRNA levels were similar in TILs from COX-2MECKO and WT tumors, another M2 marker, Retnla, was significantly decreased in COX-2MECKO (Figure 3B). Taken as a whole, our flow cytometry, immune staining and CD45+ cell expression analysis indicates that absence of epithelial COX-2-derived mediators augments Th1 and cytotoxic immune function and reduces immune suppressive macrophage function in the mammary tumor microenvironment.
Figure 3.
Deletion of mammary epithelial COX-2 modified tumor infiltrating cell phenotype. COX-2MECKO tumors are denoted as KO. (A) Flow cytometry analysis of tumor associated lymphocytes and macrophages (n = 7 to 10). (B) Gene expression levels measured by Q-PCR in CD45+ tumor infiltrating leukocytes (TILs) isolated from whole tumors by microbead separation (n = 6 to 7). (C) Gene expression levels measured by Q-PCR in unpolarized, M1 polarized or M2 polarized bone marrow derived macrophages, treated without or with PGE2 (n = 8). Data are mean ± sem. P values are compared to WT; *p < 0.05. COX, cyclooxygenase; KO, knock out; PGE2, prostaglandin E2; WT, wild type.
COX-2 may enhance immune tolerance through suppression of T cell recruitment and activation
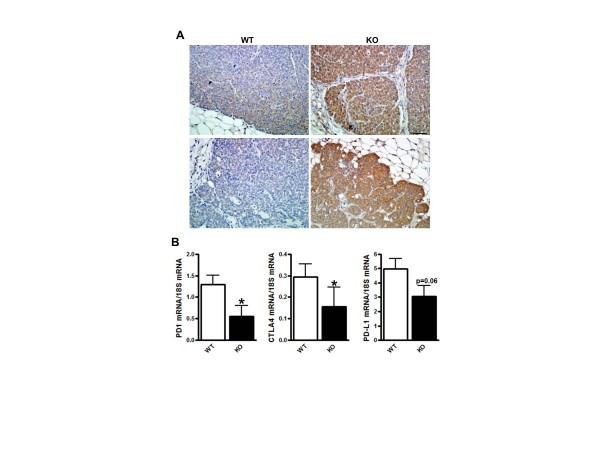
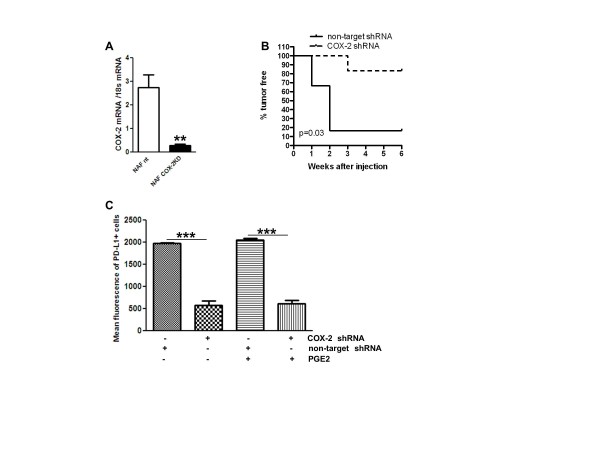
Our data thus far indicates a significant contribution of mammary epithelial COX-2-derived mediators to pro-tumor immune function, particularly T lymphocyte and cytotoxic immune cell function, in the tumor microenvironment. We next examined pathways that control T cell recruitment, activation and function. In breast cancer, tumor cell expression of the chemokines CXCL9 and 10 recruits lymphocytes, improves survival in mouse models and human studies [29,30], and PGE2 inhibits expression of both chemokines in breast cancer cells in vitro [12]. Paraffin embedded sections of WT and COX-2MECKO tumors showed substantially higher levels of CXCL9 expression, by immunohistochemistry, in COX-2MECKO tumors, and this staining was evident throughout the tumor cells (Figure 4A). WT tumors, in contrast, showed weak CXCL9 staining (Figure 4A). T cell activation requires binding of T cell receptors to antigen and is regulated by a balance of co-stimulatory and co-inhibitory receptor-ligand interactions. T cell CD28 receptor engagement by CD80 or CD86, expressed on antigen presenting cells, provides the additional signal necessary for T cell activation. The same ligands can, alternatively, drive T cells to a state of anergy through binding to cytotoxic T lymphocyte antigen 4 (CTLA-4) [31]. Inhibition of T cell function is also directed through binding of programmed death ligand 1 (PD-L1) to its receptor, PD-1, expressed on the T cell surface [32]. In our study, gene expression levels for both inhibitory receptors CTLA4 and PD-1, as well as PD-L1, were decreased in COX-2MECKO tumors compared to WT, suggesting suppressed signaling through co-inhibitory pathways (Figure 4B). Both cancer cells and tumor infiltrating myeloid cells are considered as sources of PD-L1 expression in the tumor microenvironment [33,34]. We did not observe any change in PD-L1 mRNA levels in CD45+ TILs from COX-2MECKO and WT tumors (data not shown), suggesting that tumor cell PD-L1 was suppressed by COX-2 deficiency. Indeed, NAF COX-2KD, which, compared to NAF nt, grew poorly as orthotopic tumors in immune competent syngenic mice (Figure 5B) also produced substantially less PD-L1 protein in response to IFNγ (Figure 5C). Interestingly, addition of exogenous PGE2 neither modified PD-L1 expression in NAF nt nor rescued IFNγ-induced PD-L1 expression in NAF COX-2KD cells.
Figure 4.
COX-2 suppresses immune surveillance by altering T cell recruitment and activation. COX-2MECKO tumors are denoted as KO. (A) Immunohistochemistry staining for CXCL9 (brown) of sections from paraffin embedded WT and COX-2MECKO tumors (two images from each genotype shown are representative of n = 4). Nuclei are counterstained with hematoxylin. The bar on the KO panel corresponds to 40× magnification. (B) Gene expression levels measured by Q-PCR in whole tumors (n = 8 to 18). Data are mean ± sem. P values are compared to WT; *P < 0.05. COX, cyclooxygenase; KO, knock out; WT, wild type.
Figure 5.
COX-2 knock down reduced tumor cell PD-L1 expression and orthotopic tumor growth. ErbB2-transformed mammary epithelial cells (NAF) were transduced with non-targeted shRNA (NAF nt) or COX-2 targeted shRNA (NAF COX-2KD). (A) COX-2 mRNA levels measured by Q-PCR, after 24 hours of treatment with 5 μg/ml LPS (n = 4). (B) Percent of tumor free mice after mammary fat pad injection of NAF nt and NAF COX-2KD (n = 6). (C) Mean fluorescence of PD-L1 in NAF, measured by flow cytometry, after 48 hours of treatment with 10 ng/ml IFNγ, with or without 250 nM PGE2 (n = 3 to 6). Data in column graphs are mean ± sem. P values are compared to NAF nt control, unless otherwise indicated. *P < 0.05, **P < 0.005, ***P < 0.0005. COX, cyclooxygenase; KO, knock out; shRNA, short hairpin RNA.
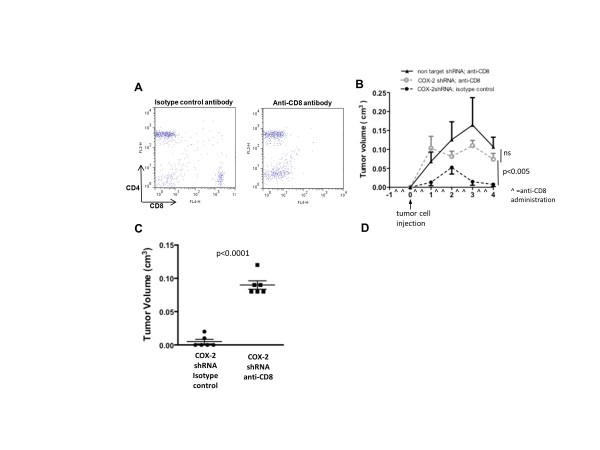
To assess how critical the loss of COX-2's immune suppressive actions was for reduced tumor growth and burden, we examined growth of NAF COX-2KD orthotopic tumors in recipient mice treated with an anti-CD8 antibody, to deplete CD8+ immune cells, or an isotype control antibody. Complete depletion of CD8+ cells in blood was confirmed by flow cytometry (Figure 6A). In isotype control antibody treated mice NAF COX-2KD grew poorly in only two of six injections. In contrast, six of six NAF COX-2KD tumors grew in CD8+ depleted mice, similar to NAF nt control cells (Figure 6B), and were markedly larger at necroscopy (four weeks after tumor injection; Figure 6C).
Figure 6.
CD8+ cell depletion restores growth of injected NAF COX-2KD tumor cells as orthotopic tumors. (A) Flow cytometry of peripheral blood from anti-CD8 or isotype control antibody treated mice four days after mammary fat pad injection (representative of n = 6). (B) Tumor growth of NAF nt and NAF COX-2KD cells injected into mammary fat pads of mice that received either anti-CD8 or isotype control antibody injection (antibody treatment denoted with ^ along X axis; n = 6). (C) NAF COX-2KD tumor volume measured on necropsy of animals that were treated with either isotype control or anti-CD8 antibody. In B and C data are mean ± sem of n = 6. **P < 0.005, ***P < 0.0005. COX, cyclooxygenase.
Discussion
Significant attention is now focused on understanding how resident and infiltrating cells in the tumor microenvironment support disease progression and in developing therapeutic strategies directed at microenvironmental targets [7]. Central to the pro-tumor microenvironment is suppression of immune cell function allowing tumor cells to avoid destruction. In the current study, we demonstrated enhanced immune cell recruitment and reduced T cell co-inhibitory pathways in tumors that lack mammary epithelial expression of the pro-inflammatory enzyme COX-2, coincident with delayed ErbB2 oncogene-driven mammary tumor development.
Consistent with established paradigms of COX-2 in cancer [6,35,36], deletion of MEC COX-2 delayed mammary tumor onset, lowered tumor multiplicity, reduced tumor cell proliferation and decreased tumor vascularization. Reduced vascularization in COX-2MECKO tumors was associated with lower expression of VEGFA and its receptor VEGFR2, a dominant pro-angiogenic pathway in tumors [37], consistent with the role of COX-2 in promoting the angiogenic switch that allows tumors to progress [38]. It may be that reduced tumor cell proliferation and suppressed angiogenesis associated with deletion of MEC COX-2 was sufficient to suppress tumors. However, the elevation of CD4+ and CD8+ immune cell populations we observed in COX-2MECKO mice, prompted us to consider how tumor cell COX-2 contributes to tumor immune function.
COX-2-mediated promotion of pro-tumorigenic Th2 lymphocyte and M2 macrophage functional phenotypes, as well as suppression of cytotoxic immune cell activity, has been reported [6]. However, it remains unclear how COX-2 contributes to the orchestration of immune cell function as tumors develop. In part, the paucity of information reflects the difficulties of working with global COX-2 knock out mice, which have breeding problems, severe renal pathology and a shortened life span [39], none of which are encountered in our targeted COX-2MECKO mice, as well as the extensive use of immune deficient host mice for tumor transplant studies. Compared to WT, three populations of immune cells - CD3+CD4+, which are Th lymphocytes, CD3+CD8+ cells, which are CTLs and CD3-CD8+, which encompass NKs and dendritic cells - were elevated in COX-2MECKO tumors. Within the CD3+CD4+ population, an increase in anti-tumorigenic Th1 cells may suppress tumors in COX-2MECKO mice; however, greater activity of Th2 lymphocytes and/or Treg would be expected to promote tumor growth [24]. The strong trend towards an increased T-bet/GATA3 mRNA ratio, a measure of the Th1 to Th2 balance [40], and the unchanged expression of FoxP3, a marker for Treg [6,24], indicates the likely prevalence of the pro-immune helper function of Th1 lymphocytes over pro-tumorigenic Th2 lymphocytes or immune suppressive Tregs, in COX-2MECKO tumors. These data are consistent with the shift toward type 1 immunity we reported previously in carcinogen-induced mammary tumors in COX-2MECKO mice, which were also delayed compared to WT [17].
Within the CD8+ populations, the suppressed tumor phenotype in COX-2MECKO mice may result from increased cytolytic actions of CTLs and NKs [24], as well as enhanced immunogenic actions of mature dentritic cells [41]. We did not directly discriminate between the relative contributions of these CD8+ subtypes; however, a key role for CD8+ immune cells in COX-2-mediated control of tumor immune function is strongly supported by the restoration of NAF COX-2KD tumor cell growth in CD8+-depleted mice.
TAM are abundant in mammary tumors and their density is generally directly correlated with disease severity and prognosis [42,43]. Similar to the Th1 and Th2 lymphocyte characterization, M1 and M2 macrophages are considered anti- and pro- tumor, respectively [44]. We reported previously that COX-2-derived PGE2 restrains M1 macrophage polarization in vitro and in carcinogen-induced mammary tumors [17]. In the current model, however, CD86, a M1 macrophage marker, was not different in COX-2MECKO tumor associated F4/80+ cells (macrophages) or in isolated CD45+ TILs, compared to WT. It is likely that the relevance of COX-2-mediated paracrine control of M1 macrophage function to tumor progression varies between models. Retnla (Resistin-like molecule alpha/FIZZ1), a cytokine derived from alternatively activated M2 type macrophages [45], was significantly lower in CD45+ TILs from COX-2MECKO tumors suggesting reduced M2 polarization, a possible reflection of reduced Th2-derived cytokines in the COX-2MECKO microenvironment and/or loss of paracrine COX-2-derived PGE2 activity, which augments M2 polarization of BMDM in vitro.
As a whole, our analysis of the tumor microenvironment strongly supported a shift towards enhanced helper and effector T lymphocyte recruitment and function in COX-2MECKO tumors. It may be that there is simply an increased immune cell recruitment to breast tumors lacking epithelial COX-2. Indeed, we saw a dramatic increase in tumor cell expression of the T cell chemokine CXCL9 in COX-2MECKO tumors, consistent with a recent report in patients with invasive breast cancer that tumor cells are the major source of CXCL9 [12]. In the same study, PGE2 suppressed IFNγ-induced CXCL9 levels in MCF-7 and MDA-MB 231 breast cancer cells, and COX inhibitors increased CXCL9 secretion. Despite the higher CXCL9 levels in COX-2MECKO tumors, however, the absolute number of CD3+ cells by flow cytometry was not higher than in WT tumors suggesting a local influence of tumor cell COX-2 derived mediators in limiting immune cell function rather than a simple recruitment effect.
Intense interest in cancer immunotherapy has focused recently on immune checkpoints, whose function to dampen immune responses is important for self tolerance and control of physiological immune responses. Two central and well-studied immune checkpoints are the co-inhibitory receptors CTLA4 and PD-1; antagonists to both are currently in clinical trials for melanoma and other cancers [32]. Engagement of CLTA4 or PD-1 on immune cells by their ligands CD80/CD86 or PD-L1, respectively, can suppress or shut down immune surveillance [46]. Conversely, blockade of co-inhibitory receptor-ligand interaction can enhance anti-tumor immunity [32]. In our study, levels of CTLA4 and PD-1, as well as PD-L1, were decreased in COX-2MECKO tumors. The PD-1-PD-L1 interaction is of particular interest in this regard since PD-1 expression in tissues is induced by inflammatory signals where it acts to suppress T cell activity and limit collateral tissue damage [32]. We reasoned, therefore, that COX-2, an established inflammatory gene, may act in tumors to upregulate expression of PD-1/PD-L1, thereby suppressing immune function and facilitating immune escape. In support of this hypothesis, NAF COX-2KD, which grew very poorly as orthotopic tumors, generated substantially less PD-L1 in response to IFNγ compared to NAF nt control cells. The failure of exogenous PGE2 to restore PD-L1 expression levels in NAF COX-2KD may suggest distinct actions of autocrine and paracrine PGE2, or indicate a role for other COX-2-derived products, in tumor cell COX-2 mediated control of PD-1 expression. The pathways through which COX-2-derived PGE2/other prostanoids control tumor cell expression of PD-L1 and other immune modulators are currently under investigation.
Our study provides significant insight into the complex autocrine and paracrine functions of mammary epithelial COX-2 in ErbB2-induced breast cancer and suggests that tumor cell COX-2 is an important component in establishing a permissive immune microenvironment. Recent studies indicated that CD8+ tumor infiltration bolstered chemotherapeutic responses in human breast cancer and mouse models [8]. Our demonstration that deletion of tumor cell COX-2 can enhance tumor-associated CD8+ cytotoxic immune cell infiltration and function may open new avenues to develop targeted strategies for COX-2 inhibition in combination with cytotoxic drugs. Further, there have been significant advances in cancer immunotherapy using antibodies to block CTLA4 or PD-1 co-inhibitory function, thereby augmenting anti-tumor immunity [32,47-49]. To our knowledge, our study is the first to link COX-2 to T cell co-inhibitory receptor/ligand function, a potentially new avenue to investigate COX-2 inhibitors as adjuvants to immunotherapy. Finally, we demonstrated that interruption of COX-2 function selectively in epithelial cells was sufficient to reduce ErbB2- (this study) and carcinogen [17] induced mammary tumorigenesis and growth. The clinical use of systemic COX-2 inhibitors in cancer, although supported across multiple studies [1], is limited by the associated gastrointestinal and cardiovascular hazards [50]. We speculate that, as improved targeted drug delivery modalities continue to emerge, delivery of COX-2 selective inhibitors directly to the tumor cells may allow for safe and effective use of these drugs in cancer without the deleterious side effects associated with systemic COX inhibition.
Conclusions
The data strongly support that, in addition to its angiogenic function, tumor cell COX-2-derived mediators suppress anti-tumor immune cell function, possibly through upregulation of inhibitory immune checkpoints, contributing to tumor immune escape. COX-2 inhibition may be clinically useful to augment breast cancer immunotherapy.
Abbreviations
BMDM: bone marrow derived macrophages; BSA: bovine serum albumin; COX: cycloogygenase; CTL: cytotoxic T lymphocyte; CTLA-4: cytotoxic T lymphocyte antigen 4; (D)MEM: (Dulbecco's) modified Eagle's medium; EDTA: ethylenediaminetetraacetic acid; FACS: fluorescence-activated cell sorting; FBS: fetal bovine serum; IFN: interferon; KO: knock out; KD: knock down; MEC: mammary epithelial cell; mmtv: mouse mammary tumor virus; NK: natural killer cells; nt: non-target; PCR: polymerase chain reaction; PD-1: programed death 1; PD-L1: programmed death ligand 1; PG: prostaglandin; shRNA: small hairpin RNA; TAM: tumor associated macrophage; TIL: tumor infiltrating leukocyte; TNF-α: tumor necrosis factor-α; WT: wild type.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
NM made substantial contributions to the study design, data acquisition, analysis and interpretation, as well as the writing and editing, of the manuscript. EPC contributed to data acquisition and analysis in the macrophage and flow cytometry experiments. RAE contributed to the design of the immune depletion experiments. VN contributed to the data acquisition. RHV contributed to the analysis and interpretation of the immune function data. EMS directed the conception and design of the study and the experimental work, contributed to the analysis and interpretation of data and critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Contributor Information
Nune Markosyan, Email: nune@mail.med.upenn.edu.
Edward P Chen, Email: edwardch@mail.med.upenn.edu.
Rebecca A Evans, Email: rebevans@vet.upenn.edu.
Victoire Ndong, Email: vndong@mail.med.upenn.edu.
Robert H Vonderheide, Email: rhv@exchange.upenn.edu.
Emer M Smyth, Email: emsmyth@mail.med.upenn.edu.
Acknowledgements
We thank Dr Lewis Chodosh for supplying the NAF mammary tumor cells. This work was supported by American Cancer Society grants RSG0802401 (to EMS), PF-11-226-01-CSM (to NM), by the National Institutes of Health training grant T32-GM08076 (EPC) and by a grant from the Breast Cancer Research Foundation (RHV)
References
- Harris RE. Cyclooxygenase-2 (cox-2) blockade in the chemoprevention of cancers of the colon, breast, prostate, and lung. Inflammopharmacology. 2009;15:55–67. doi: 10.1007/s10787-009-8049-8. [DOI] [PubMed] [Google Scholar]
- Howe LR. Inflammation and breast cancer. Cyclooxygenase/prostaglandin signaling and breast cancer. Breast Cancer Res. 2007;15:210. doi: 10.1186/bcr1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe LR, Chang SH, Tolle KC, Dillon R, Young LJ, Cardiff RD, Newman RA, Yang P, Thaler HT, Muller WJ, Hudis C, Brown AM, Hla T, Subbaramaiah K, Dannenberg AJ. HER2/neu-induced mammary tumorigenesis and angiogenesis are reduced in cyclooxygenase-2 knockout mice. Cancer Res. 2005;15:10113–10119. doi: 10.1158/0008-5472.CAN-05-1524. [DOI] [PubMed] [Google Scholar]
- Lanza-Jacoby S, Miller S, Flynn J, Gallatig K, Daskalakis C, Masferrer JL, Zweifel BS, Sembhi H, Russo IH. The cyclooxygenase-2 inhibitor, celecoxib, prevents the development of mammary tumors in Her-2/neu mice. Cancer Epidemiol Biomarkers Prev. 2003;15:1486–1491. [PubMed] [Google Scholar]
- Harris RE, Beebe-Donk J, Alshafie GA. Reduction in the risk of human breast cancer by selective cyclooxygenase-2 (COX-2) inhibitors. BMC Cancer. 2006;15:27. doi: 10.1186/1471-2407-6-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D, Dubois RN. Eicosanoids and cancer. Nat Rev Cancer. 2010;15:181–193. doi: 10.1038/nrc2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;15:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- DeNardo DG, Brennan DJ, Rexhepaj E, Ruffell B, Shiao SL, Madden SF, Gallagher WM, Wadhwani N, Keil SD, Junaid SA, rugo HS, Hwang ES, Jirström K, West BL, Coussens LM. Leukocyte complexity predicts breast cancer survival and functionally regulates response to chemotherapy. Cancer Discov. 2011;15:54–67. doi: 10.1158/2159-8274.CD-10-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeNardo DG, Andreu P, Coussens LM. Interactions between lymphocytes and myeloid cells regulate pro- versus anti-tumor immunity. Cancer Metastasis Rev. 2010;15:309–316. doi: 10.1007/s10555-010-9223-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finak G, Bertos N, Pepin F, Sadekova S, Souleimanova M, Zhao H, Chen H, Omeroglu G, Meterissian S, Omeroglu A, Hallett M, Park M. Stromal gene expression predicts clinical outcome in breast cancer. Nat Med. 2008;15:518–527. doi: 10.1038/nm1764. [DOI] [PubMed] [Google Scholar]
- Obermajer N, Muthuswamy R, Odunsi K, Edwards RP, Kalinski P. PGE(2)-induced CXCL12 production and CXCR4 expression controls the accumulation of human MDSCs in ovarian cancer environment. Cancer Res. 2011;15:7463–7470. doi: 10.1158/0008-5472.CAN-11-2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronger H, Kraeft S, Schwarz-Boeger U, Cerny C, Stockel A, Avril S, Kiechle M, Schmitt M. Modulation of CXCR3 ligand secretion by prostaglandin E2 and cyclooxygenase inhibitors in human breast cancer. Breast Cancer Res. 2012;15:R30. doi: 10.1186/bcr3115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chattopadhyay S, Bhattacharyya S, Saha B, Chakraborty J, Mohanty S, Sakib Hossain DM, Banerjee S, Das K, Sa G, Das T. Tumor-shed PGE(2) impairs IL2Rgammac-signaling to inhibit CD4 T cell survival: regulation by theaflavins. PLoS One. 2009;15:e7382. doi: 10.1371/journal.pone.0007382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pockaj BA, Basu GD, Pathangey LB, Gray RJ, Hernandez JL, Gendler SJ, Mukherjee P. Reduced T-cell and dendritic cell function is related to cyclooxygenase-2 overexpression and prostaglandin E2 secretion in patients with breast cancer. Ann Surg Oncol. 2004;15:328–339. doi: 10.1245/ASO.2004.05.027. [DOI] [PubMed] [Google Scholar]
- Sinha P, Clements VK, Fulton AM, Ostrand-Rosenberg S. Prostaglandin E2 promotes tumor progression by inducing myeloid-derived suppressor cells. Cancer Res. 2007;15:4507–4513. doi: 10.1158/0008-5472.CAN-06-4174. [DOI] [PubMed] [Google Scholar]
- Kojima M, Morisaki T, Uchiyama A, Doi F, Mibu R, Katano M, Tanaka M. Association of enhanced cyclooxygenase-2 expression with possible local immunosuppression in human colorectal carcinomas. Ann Surg Oncol. 2001;15:458–465. doi: 10.1007/s10434-001-0458-x. [DOI] [PubMed] [Google Scholar]
- Markosyan N, Chen EP, Ndong VN, Yao Y, Sterner CJ, Chodosh LA, Lawson JA, Fitzgerald GA, Smyth EM. Deletion of cyclooxygenase 2 in mouse mammary epithelial cells delays breast cancer onset through augmentation of type 1 immune responses in tumors. Carcinogenesis. 2011;15:1441–1449. doi: 10.1093/carcin/bgr134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwamoto A, Ikeguchi M, Matsumoto S, Hukumoto Y, Inoue M, Ozaki T, Ataka M, Tanida T, Endo K, Katano K, Hirooka Y. Tumor cyclooxygenase-2 gene suppresses local immune responses in patients with hepatocellular carcinoma. Tumori. 2006;15:130–133. doi: 10.1177/030089160609200208. [DOI] [PubMed] [Google Scholar]
- Stolina M, Sharma S, Lin Y, Dohadwala M, Gardner B, Luo J, Zhu L, Kronenberg M, Miller PW, Portanova J, Lee JC, Dubinett SM. Specific inhibition of cyclooxygenase 2 restores antitumor reactivity by altering the balance of IL-10 and IL-12 synthesis. J Immunol. 2000;15:361–370. doi: 10.4049/jimmunol.164.1.361. [DOI] [PubMed] [Google Scholar]
- Hamanishi J, Mandai M, Abiko K, Matsumura N, Baba T, Yoshioka Y, Kosaka K, Konishi I. The comprehensive assessment of local immune status of ovarian cancer by the clustering of multiple immune factors. Clin Immunol. 2011;15:338–347. doi: 10.1016/j.clim.2011.08.013. [DOI] [PubMed] [Google Scholar]
- Specht C, Bexten S, Kolsch E, Pauels HG. Prostaglandins, but not tumor-derived IL-10, shut down concomitant tumor-specific CTL responses during murine plasmacytoma progression. Int J Cancer. 2001;15:705–712. doi: 10.1002/1097-0215(200002)9999:9999<::AID-IJC1066>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- Betz M, Fox BS. Prostaglandin E2 inhibits production of Th1 lymphokines but not of Th2 lymphokines. J Immunol. 1991;15:108–113. [PubMed] [Google Scholar]
- Kalinski P. Regulation of immune responses by prostaglandin E2. J Immunol. 2012;15:21–28. doi: 10.4049/jimmunol.1101029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruffell B, DeNardo DG, Affara NI, Coussens LM. Lymphocytes in cancer development: polarization towards pro-tumor immunity. Cytokine Growth Factor Rev. 2010;15:3–10. doi: 10.1016/j.cytogfr.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borowsky AD. Choosing a mouse model: experimental biology in context--the utility and limitations of mouse models of breast cancer. Cold Spring Harb Perspect Biol. 2011;15:a009670. doi: 10.1101/cshperspect.a009670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross JS, Fletcher JA. The HER-2/neu oncogene in breast cancer: prognostic factor, predictive factor, and target for therapy. Stem Cells. 1998;15:413–428. doi: 10.1002/stem.160413. [DOI] [PubMed] [Google Scholar]
- Ursini-Siegel J, Schade B, Cardiff RD, Muller WJ. Insights from transgenic mouse models of ERBB2-induced breast cancer. Nat Rev Cancer. 2007;15:389–397. doi: 10.1038/nrc2127. [DOI] [PubMed] [Google Scholar]
- Sinha P, Clements VK, Ostrand-Rosenberg S. Reduction of myeloid-derived suppressor cells and induction of M1 macrophages facilitate the rejection of established metastatic disease. J Immunol. 2005;15:636–645. doi: 10.4049/jimmunol.174.2.636. [DOI] [PubMed] [Google Scholar]
- Specht K, Harbeck N, Smida J, Annecke K, Reich U, Naehrig J, Langer R, Mages J, Busch R, Kruse E, Klein-Hitpass L, Schmitt M, Kiechle M, Hoefler H. Expression profiling identifies genes that predict recurrence of breast cancer after adjuvant CMF-based chemotherapy. Breast Cancer Res Treat. 2009;15:45–56. doi: 10.1007/s10549-008-0207-y. [DOI] [PubMed] [Google Scholar]
- Walser TC, Ma X, Kundu N, Dorsey R, Goloubeva O, Fulton AM. Immune-mediated modulation of breast cancer growth and metastasis by the chemokine Mig (CXCL9) in a murine model. J Immunother. 2007;15:490–498. doi: 10.1097/CJI.0b013e318031b551. [DOI] [PubMed] [Google Scholar]
- Chen L. Co-inhibitory molecules of the B7-CD28 family in the control of T-cell immunity. Nat Rev Immunol. 2004;15:336–347. doi: 10.1038/nri1349. [DOI] [PubMed] [Google Scholar]
- Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;15:252–264. doi: 10.1038/nrc3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong H, Strome SE, Salomao DR, Tamura H, Hirano F, Flies DB, Roche PC, Lu J, Zhu G, Tamada K, Lennon VA, Celis E, Chen L. Tumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nat Med. 2002;15:793–800. doi: 10.1038/nm730. [DOI] [PubMed] [Google Scholar]
- Kuang DM, Zhao Q, Peng C, Xu J, Zhang JP, Wu C, Zheng L. Activated monocytes in peritumoral stroma of hepatocellular carcinoma foster immune privilege and disease progression through PD-L1. J Exp Med. 2009;15:1327–1337. doi: 10.1084/jem.20082173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gately S, Li WW. Multiple roles of COX-2 in tumor angiogenesis: a target for antiangiogenic therapy. Semin Oncol. 2004;15:2–11. doi: 10.1053/j.seminoncol.2004.03.040. [DOI] [PubMed] [Google Scholar]
- Karnezis T, Shayan R, Caesar C, Roufail S, Harris NC, Ardipradja K, Zhang YF, Williams SP, Farnsworth RH, Chai MG, Rupasinghe TW, Tull DL, Baldwin ME, Sloan EK, Fox SB, Achen MG, Stacker SA. VEGF-D promotes tumor metastasis by regulating prostaglandins produced by the collecting lymphatic endothelium. Cancer Cell. 2012;15:181–195. doi: 10.1016/j.ccr.2011.12.026. [DOI] [PubMed] [Google Scholar]
- Hicklin DJ, Ellis LM. Role of the vascular endothelial growth factor pathway in tumor growth and angiogenesis. J Clin Oncol. 2005;15:1011–1027. doi: 10.1200/JCO.2005.06.081. [DOI] [PubMed] [Google Scholar]
- Chang SH, Liu CH, Conway R, Han DK, Nithipatikom K, Trifan OC, Lane TF, Hla T. Role of prostaglandin E2-dependent angiogenic switch in cyclooxygenase 2-induced breast cancer progression. Proc Natl Acad Sci USA. 2004;15:591–596. doi: 10.1073/pnas.2535911100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang T, Huang YG, Ye W, Hansen P, Schnermann JB, Briggs JP. Influence of genetic background and gender on hypertension and renal failure in COX-2-deficient mice. Am J Physiol Renal Physiol. 2005;15:F1125–1132. doi: 10.1152/ajprenal.00219.2004. [DOI] [PubMed] [Google Scholar]
- Jenner RG, Townsend MJ, Jackson I, Sun K, Bouwman RD, Young RA, Glimcher LH, Lord GM. The transcription factors T-bet and GATA-3 control alternative pathways of T-cell differentiation through a shared set of target genes. Proc Natl Acad Sci USA. 2009;15:17876–17881. doi: 10.1073/pnas.0909357106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palucka K, Banchereau J. Cancer immunotherapy via dendritic cells. Nat Rev Cancer. 2012;15:265–277. doi: 10.1038/nrc3258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y, Zhou H, Krueger J, Kaplan C, Lee SH, Dolman C, Markowitz D, Wu W, Liu C, Reisfeld RA, Xiang R. Targeting tumor-associated macrophages as a novel strategy against breast cancer. J Clin Invest. 2006;15:2132–2141. doi: 10.1172/JCI27648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruffell B, Affara NI, Coussens LM. Differential macrophage programming in the tumor microenvironment. Trends Immunol. 2012;15:119–126. doi: 10.1016/j.it.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. J Clin Invest. 2012;15:787–795. doi: 10.1172/JCI59643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair MG, Du Y, Perrigoue JG, Zaph C, Taylor JJ, Goldschmidt M, Swain GP, Yancopoulos GD, Valenzuela DM, Murphy A, Karow M, Stevens S, Pearce EJ, Artis D. Alternatively activated macrophage-derived RELM-{alpha} is a negative regulator of type 2 inflammation in the lung. J Exp Med. 2009;15:937–952. doi: 10.1084/jem.20082048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou W. Immunosuppressive networks in the tumour environment and their therapeutic relevance. Nat Rev Cancer. 2005;15:263–274. doi: 10.1038/nrc1586. [DOI] [PubMed] [Google Scholar]
- Curran MA, Montalvo W, Yagita H, Allison JP. PD-1 and CTLA-4 combination blockade expands infiltrating T cells and reduces regulatory T and myeloid cells within B16 melanoma tumors. Proc Natl Acad Sci USA. 2010;15:4275–4280. doi: 10.1073/pnas.0915174107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD, Sosman JA, Atkins MB, Leming PD, Spigel DR, Antonia SJ, Horn L, Drake CG, Pardoll DM, Chen L, Sharfman WH, Anders RA, Taube JM, McMiller TL, Xu H, Korman AJ, Jure-Kunkel M, Agrawal S, McDonald D, Kollia GD, Gupta A, Wigginton JM, Sznol M. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;15:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K, Pitot HC, Hamid O, Bhatia S, Martins, R, Eaton K, Chen S, Salay TM, Alaparthy S, Grosso JF, Korman AJ, Parker SM, Agrawal S, Goldberg SM, Pardoll DM, Gupta A, Wigginton JM. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;15:2455–2465. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosser T, Yu Y, Fitzgerald GA. Emotion recollected in tranquility: lessons learned from the COX-2 saga. Annu Rev Med. 2010;15:17–33. doi: 10.1146/annurev-med-011209-153129. [DOI] [PubMed] [Google Scholar]