Abstract
Haemorrhagic cholecystitis is a known rare life-threatening complication of acute cholecystitis. In this case report, we describe clinical presentation and radiological findings of acute cholecystitis presenting with massive intra-abdominal haemorrhage. We present a case of a 57-year-old male presenting to the emergency department with clinical symptoms of acute cholecystitis. Initially, the patient was haemodynamically stable. Gallbladder could not be visualized by ultrasound. Computed tomography with IV contrast showed a large haematoma in the gallbladder fossa, with active extravasation of IV contrast. On angiography the bleeding was localized to a branch of the cystic artery, which was embolized using gelfoam material. The patient was taken to the operating room for an urgent laparotomy and cholecystectomy.
INTRODUCTION
Haemorrhagic cholecystitis with haemoperitoneum is a rare life-threatening complication of acute cholecystitis, several cases have been reported. The clinical presentation of haemorrhagic cholecystitis can vary widely. Symptoms could resemble acute cholecystitis or biliary colic. Other presentations may include upper gastrointestinal haemorrhage, haematemesis, melena, hemobilia or symptoms of biliary obstruction and jaundice. In addition, it may present with haemoperitoneum and haemorrhagic shock.
The diagnosis is made based on computed tomography (CT) scan. The role of sonography is limited, but can be helpful. The importance of early diagnosis comes from the fatality of any delay in the diagnosis. To our knowledge there is a few reported cases in the literature of a free intraperitoneal bleeding caused by gallbladder haemorrhage and perforation. We present this case report to emphasize the importance of early diagnosis and management.
CASE HISTORY
A 57-year-old male presented to the emergency department with 24 h history of right upper quadrant and epigastric pain. Which started the night before, following an ingestion of a fatty meal situated in the right upper quadrant and epigastric region. There was no associated fever, nausea or vomiting. The pain became constant with no relieving factors.
His past medical history includes ulcerative colitis for 20 years and primary sclerosing cholangitis (PSC) for 12 years with associated liver cirrhosis (Child A). On examination he was haemodynamically stable with a blood pressure of 145/75, a heart rate of 86 with normal temperature (36.8°C). He had tenderness over the right upper quadrant region with a positive Murphy's sign. He had no evidence of generalized peritonitis. The routine blood tests showed haemoglobin of 13.6 with an elevated white blood cell count of 18, a normal platelet count and a normal INR. The total bilirubin was elevated at 82 mmol/l along with an alkaline phosphatase (ALP) of 463, an alanine transaminase (ALT) of 153 and an aspartate transaminase (AST) of 101. This elevation in his liver function test was attributed to his PSC.
An ultrasound was done showing a mass in the right upper quadrant with no visualization of the gallbladder and no evidence of biliary tree dilatation. Therefore, a CT scan was performed which showed a large haematoma in the gallbladder fossa, which distends the gallbladder wall causing mass effect (Fig. 1a and b). Furthermore, active extravasation of IV contrast was seen. Initially, this was not clear if the haematoma is arising from the liver or within the gallbladder. Given his haemodynamic stability he was taken to the interventional angiography suite for an arteriogram of his abdominal aorta and splanchnic vessels. The bleeding was localized to a branch of the cystic artery and no pseudoaneurysm was identified (Fig. 2). Then, embolization of cystic artery with gelfoam material was performed. Since, embolization of the cystic artery proper was done, the decision was made to explore the patient and perform a cholecystectomy. Prior to the operation the patient became tachycardic at 100 with a systolic blood pressure of 90 and a diastolic of 60. His repeat haemoglobin was 10.1. Appropriate resuscitation with blood transfusion was performed.
Figure 1:
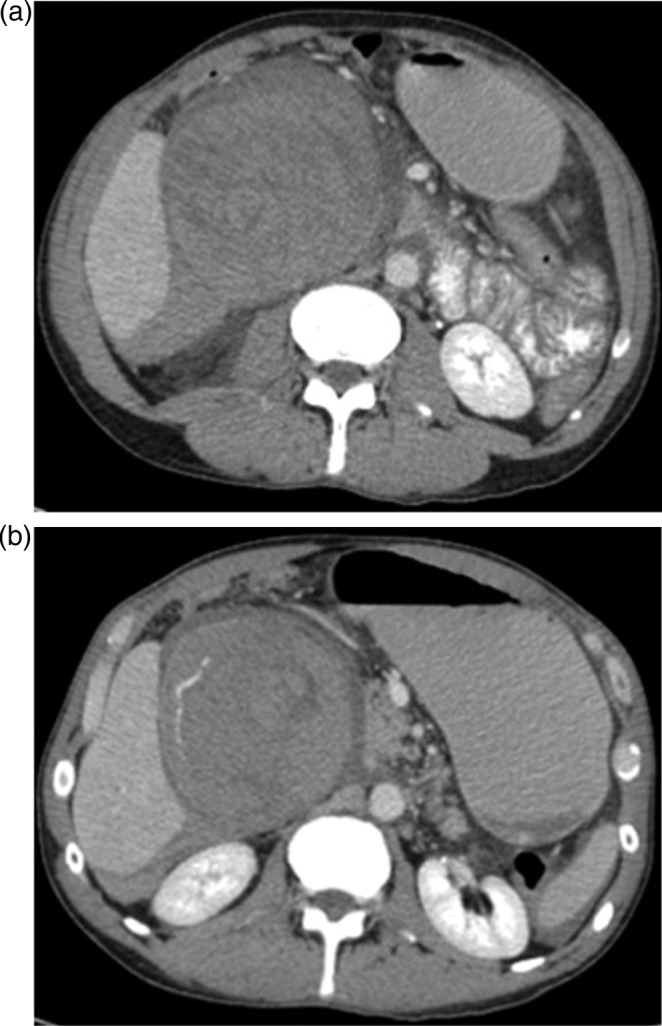
(a and b) CT scan upper abdomen showing a large haematoma in the gallbladder fossa, which distends the gallbladder wall causing mass effect.
Figure 2:
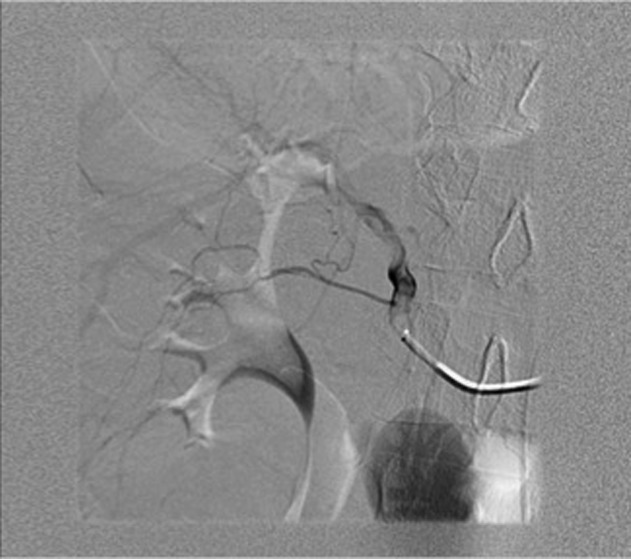
Arteriogram of abdominal aorta and splanchnic vessels showing localized bleeding in a branch of the cystic artery and no pseudoaneurysm.
In the operating room a right Kocher incision was performed. Upon entering the peritoneal cavity a large haematoma was encountered with some old blood. Following the evacuation of the haematoma, the gallbladder was identified; it was massively distended with a haemorrhagic-appearing wall and had a tear in the fundus. Inside the gallbladder lumen clots and fresh blood was seen (Figs 3 and 4). It was clear that the bleeding cystic artery branch distended the gallbladder with blood leading to gallbladder rupture and free haemorrhage into the peritoneal cavity, with a total amount of evacuated haematoma of 2.5 L. A cholecystectomy was performed in a retrograde fashion, and a drain inserted before the closure of the abdomen. The patient was extubated and transferred to the recovery room in a stable condition. He did well post-operatively and was discharged home on the 6th post-operative day.
Figure 3:
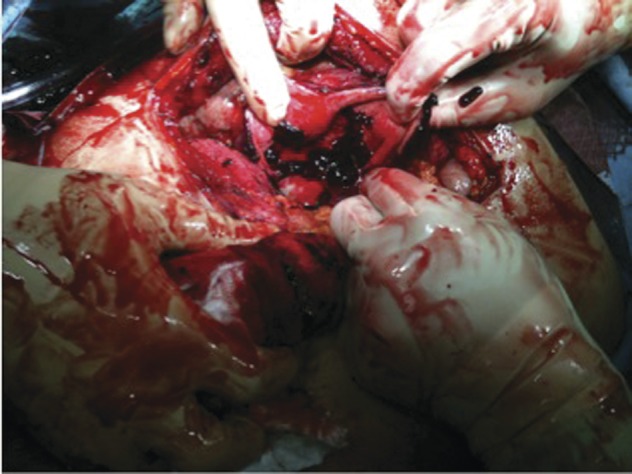
Intraoperative picture of gall bladder.
Figure 4:
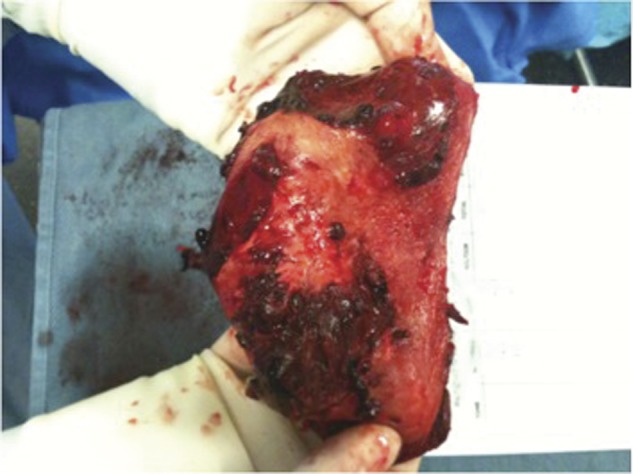
Intraoperative picture of gall bladder.
Pathology revealed an acute on chronic cholecystitis with a haematoma in the gallbladder wall (Fig. 5). The embolization material was identified in the small vessels leading to the gallbladder wall haematoma.
Figure 5:

Intraoperative picture of gall bladder.
DISCUSSION
The incidence of gallbladder perforation is estimated to be 3.5% of all cholecystitis, 9.5% of the perforated cases are free perforations into the peritoneal cavity [1], with high mortality and morbidity rates [1–4]. Bleeding caused by cholecystitis is extremely rare, since the inflammation is thought to cause vascular thrombosis mainly; however, the inflammation may also cause damage to the adventitia with thrombosis of the vasa vasorum leading to weakening of the vessel wall. Another proposed mechanism that could lead to gallbladder bleeding is wall inflammation leading to mucosal ulceration and necrosis [5]. Hemorrhage could also be from the liver bed when transhepatic perforation takes place [6, 7].
A possible explanation for the intraperitoneal rupture in this case would be the possibility of fibrosis at the ampulla due to the patient history of PSC requiring frequent endoscopic retrograde cholangiographies. This could have caused the retrograde accumulation of blood in the gallbladder and biliary system rather than bleeding into the intestine. In this case angiography was helpful in localizing the bleeding, and since an embolization of the cystic artery proper was done, an urgent cholecystectomy was indicated even though a perforation was not seen on preoperative investigation.
Diagnosis may be difficult due to the wide clinical presentation [8]. Imaging studies plays a significant role. Abdominal ultrasound has a limited role, though can aid in the diagnosis showing a non-shadowing, increased thickness of focal wall, intraluminal membranes, intraluminal echogenic material that is non-mobile and some echogenic layering material [8]. CT plays a crucial role in the diagnosis which may show hyperdense fluid surrounding the gallbladder or the perforation site of gallbladder as a wall defect, with or without spillage of stone within the peritoneum [3, 5]. An arterial phase-contrast enhanced CT may demonstrate active extravasation of contrast material into the gallbladder lumen which confirms the diagnosis [9]. Cholecystectomy was performed in this case.
REFERENCES
- 1.Smith EB. Perforation of the gallbladder: a clinical study. J Natl Med Assoc. 1981;73:333–5. [PMC free article] [PubMed] [Google Scholar]
- 2.Jenkins M, Golding RH, Cooperberg PL. Sonography and computed tomography of hemorrhagic cholecystitis. AJR Am J Roentgenol. 1983;140:1197–8. doi: 10.2214/ajr.140.6.1197. [DOI] [PubMed] [Google Scholar]
- 3.Kim YC, Park MS, Chung YE, Lim JS, Kim MJ, Kim KW. Gallstone spillage caused by spontaneously perforated hemorrhagic cholecystitis. World J Gastroenterol. 2007;13:5525–6. doi: 10.3748/wjg.v13.i41.5525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Syme RG, Thomas EJ. Massive hemoperitoneum from transhepatic perforation of the gallbladder: a rare complication of cholelithiasis. Surgery. 1989;105:556–9. [PubMed] [Google Scholar]
- 5.Bennett GL, Balthazar EJ. Ultrasound and CT evaluation of emergent gallbladder pathology. Radiol Clin North Am. 2003;41:1203–16. doi: 10.1016/s0033-8389(03)00097-6. [DOI] [PubMed] [Google Scholar]
- 6.Nural MS, Bakan S, Bayrak IK, Baydin A, Danaci M. A rare complication of acute cholecystitis: transhepatic perforation associated with massive intraperitoneal hemorrhage. Emerg Radiol. 2007;14:439–41. doi: 10.1007/s10140-007-0621-1. [DOI] [PubMed] [Google Scholar]
- 7.Kolder D, Geiger T, Tharakan AK, Kessel JW, Awad ZT. Massive hemoperitoneum from transhepatic perforation of the gallbladder. Mt Sinai J Med. 2006;73:1135–6. [PubMed] [Google Scholar]
- 8.Chinn DH, Miller EI, Piper N. Hemorrhagic cholecystitis. Sonographic appearance and clinical presentation. J Ultrasound Med. 1987;6:313–7. doi: 10.7863/jum.1987.6.6.313. [DOI] [PubMed] [Google Scholar]
- 9.Pandya R, O'Malley C. Hemorrhagic cholecystitis as a complication of anticoagulant therapy: role of CT in its diagnosis. Abdom Imaging. 2008;33:652–3. doi: 10.1007/s00261-007-9358-2. [DOI] [PubMed] [Google Scholar]


