Abstract
Purpose
To describe outcomes of the Acupuncture to Decrease Disparities in Outcomes of Pain Treatment (ADDOPT) trial, testing acupuncture as an adjunct to usual treatment for chronic pain in urban health centers.
Method
We conducted quasi-experimental trial. Primary care patients (>21 yrs) with chronic pain due to osteoarthritis, neck or back pain at four hospital owned safety net health centers in the Bronx, NY received weekly acupuncture treatments provided by supervised acupuncture students for up to 14 weeks. Pain and functional status were assessed during a 6-week run-in period before acupuncture, during treatment and post treatment.
Results
Of 495 referred patients, 226 (47%) initiated acupuncture. Back pain was the most common referring diagnosis (59.5%) followed by OA (16.3%). Patients were older (mean age 54.3), mostly Medicaid insured (60.4%), often on disability (38.3%), often (46.7%) in poor or fair overall health, and had high baseline levels of pain (mean BPI pain severity 6.8; mean days with pain, 12.3 of 14 days). The mean number of treatments was 9.7 (SD = 7.3). Pain severity improved from baseline (6.8 vs 5.6 at 12 wks and 5.5 at 24 wks) as did physical well-being (31.8 vs 35.7 at 12 wks and 35.3 at 24 wks). Using HLM methods, reduction in pain severity between baseline and treatment phase was significant (p <.001). Improvements in physical well-being were significant at 12 and 24 weeks post-baseline (p <.001).
Conclusions
Referred primary care patients experienced high levels of pain and pain-related disability. Weekly acupuncture was associated with short-term improvements in pain and quality of life.
INTRODUCTION
This article reports on the outcomes of the Acupuncture to Decrease Disparities in Pain Treatment (ADDOPT) trial, a recent NIH-funded clinical trial of acupuncture for chronic back pain, neck pain and osteoarthritis, offered in the community health center setting to an ethnically diverse and medically underserved patient population in the Bronx, NY.
Chronic pain is a major problem in primary care practice, affecting an estimated 10–40% of the population. (1–6) Minority populations experience disparities in both the prevalence and outcomes of chronic pain. (7–10) There are strong positive associations between pain and impairment of physical and psychological functioning, (11, 12) lost productivity, (13) and lower socioeconomic status. (6) Particularly in light of recent concerns regarding abuse of prescription analgesics and the consequent growing pressure to limit prescription of narcotic medications, primary care physicians are in desperate need of more effective strategies for managing patients with chronic pain conditions.
A great deal of evidence now supports the use of acupuncture therapy in the treatment of chronic pain conditions, particularly in three common causes of chronic pain: osteoarthritis, (14–16) neck pain, (17, 18) and low back pain. (19–23) Although the mechanism of action remains unclear, and although many studies find both “sham” (needles in non-acupuncture points) and real acupuncture to be effective, it is clear that 40–50% of patients experience a reduction in pain with acupuncture treatment.
For the most part, patients from lower socioeconomic groups have not had access to acupuncture treatment in the U.S., services not generally reimbursed by insurers. To examine the effectiveness of acupuncture for chronic pain, we developed a new delivery model offering care inside the community health center primary care setting, utilizing student acupuncturists so that services could be provided at no cost to patients.
The ADDOPT trial sought to demonstrate both the feasibility and acceptability of offering acupuncture in the primary care setting, and the impact of this treatment on pain and functional outcomes. The feasibility findings have been reported elsewhere (24); here we report the impact of acupuncture on pain and functional status.
METHODS
The overall goal of the ADDOPT study was to introduce and evaluate the addition of acupuncture to the management of chronic pain for ethnically diverse, low-income primary care patients. The Albert Einstein College of Medicine Institutional Review Board approved the study.
Setting and Participants
The study was conducted in four Bronx hospital-owned primary care health centers serving low-income families. Practices serve a mostly minority population (29–69% Black, 23–58% Hispanic) who are mostly Medicaid insured (43–59%) or uninsured (5–15%). All practices were part of the New York City Research and Improvement Networking Group (NYC RING), a practice-based research network dedicated to decreasing health disparities through primary care research and quality improvement in the urban safety net setting.
Recruitment
Medical staff at each participating practice received a brief (60 minutes) orientation to the study including an overview of acupuncture procedures and a summary of the evidence of effectiveness in chronic pain conditions. Enrollment occurred between March of 2009 and July 2011. Primary care physicians (PCP) referred interested and eligible patients (age >21, suffering from chronic pain [3 months or more] due to osteoarthritis, neck or back pain, fluent in English or Spanish, able to provide home phone numbers to facilitate scheduling, and available for up to 14 weekly treatments). Patients on anticoagulants were not eligible. Once referred, the study coordinator contacted patients by telephone to confirm eligibility and describe study procedures.
Design
The study employed a repeated measures quasi-experimental design, (25) with each participant having multiple pre and post measures, allowing assessment of what may be variable patterns of pain pre-intervention. (26) Although a randomized design with usual care control would have been ideal, because this was primarily a feasibility and acceptability trial with limited funding resources, we chose this pragmatic non-randomized design to maximize our recruiting ability and the acceptability of the trial to staff and to patients. This pragmatic design allowed us to offer the intervention without randomization to all patients with target diagnoses who met eligibility criteria, maximizing limited resources and also maximizing feasibility and acceptability to patients and staff. Pre-acupuncture assessments of pain were collected biweekly during a 6 week run-in period prior to the initial acupuncture session. A priori power analyses indicated that adequate power (90%) to detect small effects (.25) could be achieved by recruiting n = 43 participants per site assuming correlations between measures of r = .10, and alpha = .05.
Intervention
Treatment (up to 14 sessions) was provided in weekly sessions at each practice by faculty student acupuncture teams (third year interns from the Pacific College of Oriental Medicine and Swedish Institute and their licensed acupuncturist supervisors), at no cost to patients. Trainees saw the same patient for repeated visits though in some cases the student changed at the end of an academic term; faculty supervisors tended to be consistent for each patient. Acupuncturists evaluated patient s based on the medical history, examination of the tongue (Tongue Diagnosis) and pulse (Pulse Diagnosis) and palpating the meridians, then make an assessment and formulate a treatment plan. This approach to acupuncture is an extremely broad-based and flexible approach, incorporating both the recently-popularized principles of Traditional Chinese Medicine (TCM) as well as techniques of Classical Chinese Medicine, which includes sinew, primary and divergent meridian treatments as well. (27) The acupuncture team was free to adapt and change the treatment approach from week to week based on the condition of the patient and response to treatment. Usual care from the PCP continued while receiving acupuncture.
Data Collection
During the pre-acupuncture run-in period, participants completed biweekly pain assessments during brief phone calls. A baseline interview was conducted in person before the first acupuncture treatment; this interview included detailed demographics, functional status, and multiple pain measures. Pain was reassessed approximately every two weeks (to capture variation in pain) in person at visits or by phone; functional status was collected at 12 weeks and 24 weeks from start of treatment. Pain was assessed using 1) the Brief Pain Inventory (BPI) (28), which includes subscales measuring pain severity and the extent to which pain interferes with function; 2) The Chronic Pain Grading Scale (CPGS) which assesses pain intensity and pain-related disability at present and over the preceding 4 weeks (29); and reported pain free days in the previous 2 weeks. (30) A change of 30% on the BPI is generally accepted as clinically significant change (31, 32). Post intervention, patients completed a single question validated measure of global impression of change. Health related quality of life was assessed using the SF-12 -- a 12-item generic health related quality of life inventory that assesses 8 dimensions of physical and mental health-related quality of life, and provides two composite scores, the Physical Component Scale and the Mental Health Scale. (33) No minimum clinically meaningful difference as been established in our population for the SF-12. A change of 4–5 on the SF-36 is considered meaningful and is thought to apply to the SF-12 as well. (34)
Analysis
Prior to analysis, all data were reviewed for accuracy, and descriptive summaries (means, standard deviations, frequencies and proportions) were generated for sample socio -demographic, baseline pain, disability and health measures. Spearman’s rho was used to evaluate the relationship between patient and clinician assessments of change and observed improvements in self-rated pain severity and physical health. Hierarchical linear modeling (HLM) (35) was used to evaluate change in outcomes over time while accounting for the correlations among the repeated measures and the variability attributable to individual and site characteristics. Unlike repeated measures ANOVA or traditional OLS regression which drop cases when all data points are not assessed or do not occur at fixed intervals, HLM models do not require fixed data collection points nor require that all patients have measures at all time points-allowing HLM to make use of all available data.
Prior to modeling, covariance estimates and intraclass correlations were calculated to determine the variability in outcomes attributable to site and individual characteristics. Significant variability in outcomes was found between individuals (SF12 ICC = .47, BPI ICC = .58), and a smaller, non-significant amount of variability in outcomes was attributable to site characteristics (SF12 ICC = .013, BPI ICC = .019). Based on these findings, random effects terms representing individuals were used in the model and site was treated as a fixed effect. Preliminary HLM models were run to determine which random effects components (slopes, intercepts) were necessary to model individual variability in outcomes. All potential predictors were examined to assess their relationship to pain severity and physical health. During the model building stage, predictors were considered significant at the p=0.10 level; in the final model, predictors that were significant at the .05 level were retained. Fixed effects representing site, time and treatment period were retained in the model regardless of significance level to ensure proper specification. Two self-reported outcomes were analyzed. Functional status, measured with the SF12 Physical Health composite score, was recorded at 3 points during the study (baseline, 12 weeks after baseline [treatment period], and 24 weeks [post-treatment]). The pain severity scale of the BPI was measured at 10 points during the study (4 during the run-in period including baseline, 4 treatment period assessments and 2 post-treatment assessments). All analyses were conducted using PASW Statistics 18, Release Version 18.0.0 (SPSS, Inc., 2009, Chicago, IL, www.spss.com).
RESULTS
Figure 1 provides details of study recruitment. PCPs referred 495 patients, of whom 291 were reached and confirmed eligible, and of these, 226 (78%) initiated acupuncture. The most common reason for not initiating was inability to attend the scheduled acupuncture session due to schedule conflict. As expected, back pain was the most common enrolled diagnosis (n=133; 58.8%), followed by osteoarthritis (n=39; 17.3%) and multiple conditions (n=36, 15.9%). Patients who did not initiate treatment did not differ significantly from those who initiated in pain condition, demographics (age, race/ethnicity, US born, education, insurance, Medicaid) pain severity, physical health or disability.
Figure 1.
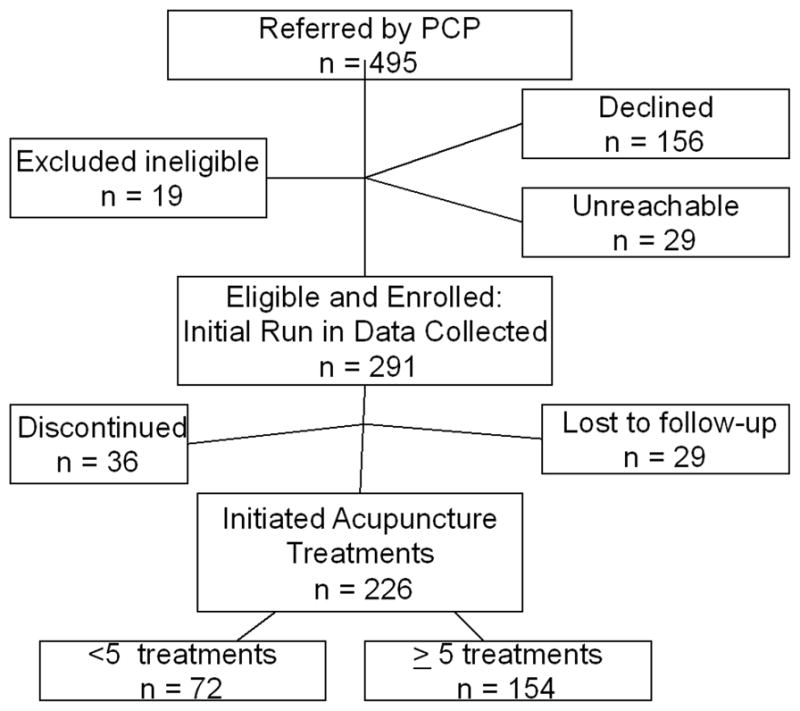
Recruitment and Study Participation
The average age was 54.3 (SD 14, median = 53.9); 70.8% of participants described themselves as English-speaking and 27% as primarily Spanish speaking and over half (53.5%) were Hispanic (Table 1). Many participants (38.5%) described themselves as disabled, an additional 10.2% were unemployed, and the remaining participants were employed either full or part time. Almost half (42%) of participants were from households earning less than $20,000 per year; 3.1% reported household incomes of $50,000 or greater. Over half (57.1%) were on Medicaid; 23% had private insurance, and 5.8% were uninsured.
Table 1.
Demographics for participants who initiated treatment (n=226).
| M | SD | |
|---|---|---|
| Age (years) | 54.3 | 14 |
| n | % | |
|
|
||
| Born in US | 107 | 47.3 |
| Language spoken most frequently | n | % |
|
| ||
| English | 160 | 70.8 |
| Spanish | 60 | 26.5 |
| Other | 6 | 2.7 |
| Marital Status | n | % |
|
| ||
| Married | 48 | 21.2 |
| Living with a partner | 12 | 5.3 |
| Divorced | 30 | 13.3 |
| Widowed | 30 | 13.3 |
| Separated | 27 | 11.9 |
| Never Married | 1 | .4 |
| Single | 75 | 33.2 |
| Other | 1 | .4 |
| Race/Ethnicity | n | % |
|
| ||
| Hispanic | 121 | 53.5 |
| Non-Hispanic Black | 61 | 27 |
| Non-Hispanic White | 9 | 4 |
| Non-Hispanic Other | 34 | 15 |
| Working status | n | % |
|
| ||
| Unemployed | 23 | 10.2 |
| F/T | 52 | 23 |
| P/T | 13 | 58 |
| Disabled | 87 | 38.5 |
| Insurance | n | % |
|
| ||
| Fee for service Medicaid | 7 | 3.1 |
| Mgd Care Medicaid | 129 | 57.1 |
| Private Ins | 52 | 23 |
| No Insurance | 13 | 5.8 |
| Household Income | n | % |
|
| ||
| Less than $20 000 | 95 | 42 |
| $20–$29 000 | 27 | 11.9 |
| $30–$39 000 | 18 | 8 |
| $40–49 000 | 6 | 2.7 |
| Greater than $50 000 | 7 | 3.1 |
| Don’t Know/Refused | 67 | 29.6 |
| Education | n | % |
|
| ||
| Some HS or less | 79 | 34.9 |
| HS Grad | 55 | 24.3 |
| Some college | 57 | 25.2 |
| College grad + | 31 | 13.7 |
Baseline pain and disability scores are included in Table 2. Patients reported an average baseline disability score of 66.7 (SD 30.9, possible range 0–100) and an average baseline pain severity on the BPI of 6.7 (SD 2.1, possible range 0–10) and pain interference mean of 6.4 (SD 2.9). Baseline scores on the SF-12 also reflected significant morbidity with 46.3% of the sample scoring in the “poor” or “fair” range for overall health.
Table 2.
Pain, disability and functional status
| BPI Pain Severity (0–10) | BPI Pain Interference (0–10) | SF12 Physical Health (0–100) | SF12 Mental Health (0–100) | SF12-Fair/Poor General Health | CPGS Disability Score (0–100%) | CPGS - Characteristic Pain Intensity (0–100%) | PFD-Days with pain last 2 weeks (0–14) | PIQ-6 (40–78) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | n | % | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |
| 6 weeks prior to baseline | 6.9 | (6.6, 7.1) | 6.9 | (6.6, 7.3) | - | - | - | - | - | - | 72.6 | (69.1, 76.1) | 78.6 | (76.8, 80.3) | 13.0 | (12.6, 13.3) | 68.4 | (67.5, 69.2) |
| 4 weeks prior to baseline | 6.9 | (6.6, 7.2) | 6.6 | (6.2, 7) | - | - | - | - | - | - | - | - | - | - | 12.5 | (12, 12.9) | - | - |
| 2 weeks prior to baseline | 7.0 | (6.6, 7.4) | 6.5 | (6, 7) | - | - | - | - | - | - | - | - | - | - | 12.5 | (11.9, 13) | - | - |
| Baseline | 6.7 | (6.5, 7) | 6.4 | (6, 6.8) | 31.7 | (30.4, 33.1) | 38.2 | (36.2, 40.1) | 107 | 46.7 | 66.8 | (62.8, 70.8) | 77.3 | (75.2, 79.3) | 12.3 | (11.9, 12.8) | 67.4 | (66.4, 68.3) |
| 2 week follow-up | 6.2 | (5.8, 6.5) | 5.5 | (5, 5.9) | - | - | - | - | - | - | - | - | - | - | 11.1 | (10.5, 11.8) | 63.9 | (62.7, 65.2) |
| 4 week follow-up | 5.7 | (5.3, 6.1) | 5.0 | (4.5, 5.6) | - | - | - | - | - | - | - | - | - | - | 10.7 | (10, 11.4) | 62.3 | (60.9, 63.7) |
| 8 week follow-up | 5.6 | (5.2, 6) | 5.0 | (4.4, 5.6) | - | - | - | - | - | - | - | - | - | - | 10.7 | (9.9, 11.4) | 61.5 | (59.9, 63.1) |
| 12 week follow-up | 5.6 | (5.2, 6.1) | 4.9 | (4.3, 5.5) | 35.7 | (33.8, 37.6) | 43.7 | (41, 46.4) | 52 | 40.63 | 43.7 | (37.7, 49.8) | 65.1 | (61.2, 69.1) | 10.1 | (9.3, 10.9) | 61.8 | (60.1, 63.4) |
| 16 week follow-up | 5.7 | (5.2, 6.3) | 5.0 | (4.4, 5.7) | - | - | - | - | - | - | - | - | - | - | 10.6 | (9.7, 11.5) | 61.7 | (59.9, 63.5) |
| 24 week follow-up | 5.5 | (4.9, 6.1) | 5.0 | (4.4, 5.7) | 35.3 | (33, 37.5) | 45.2 | (42.5, 47.8) | 36 | 33.64 | 45.2 | (38.2, 52.2) | 64.7 | (59.9, 69.5) | 10.9 | (10, 11.7) | 62.2 | (60.2, 64.1) |
- Not measured;
higher BPI score = more severe pain; higher SF-12 score = better function
Of patients initiating treatment (N = 226), the mean number of treatments per patient was 9.7 (SD 7.3) and 154 (68.1%) had five or more treatments (chosen to indicate a meaningful engagement with treatment, based on expert opinion). There were no statistically significant differences in the proportion of patients engaging in 5 or more treatments in regard to referring diagnosis, baseline level of pain and disability, baseline functional status as measured by SF-12, and specific demographic factors (data not shown). A few participants (n=9) reported an adverse event, all related to transient increase in pain or numbness. The most common reasons for discontinuing treatment were “no longer interested” (27%), poor health (23%) and lack of improvement (18%).
Multivariate results
Table 2 and Figure 2 show the trend in pre and post baseline mean scores for our primary outcomes, functional status and pain severity. In assessing change over time using HLM, the covariates retained in the multivariate model for functional health status included treatment site, number of acupuncture treatments received, baseline disability and age. In the adjusted model, functional status was significantly improved for in-treatment and post-treatment periods. Functional status did not differ by site, though site was retained in the model for complete specification. Number of treatments was significantly related to functional status; degree of disability and age were negatively related to functional health. The multivariate model for pain severity revealed a significant reduction in severity during the treatment period, and a non-significant reduction (from baseline) during the post-treatment period. Interaction terms representing time by treatment periods were non-significant indicating the slope of pain severity did not change across treatment periods. Baseline degree of disability and receiving Medicaid were both positively related with reported pain severity. Adjusted regression coefficients for pain severity and functional status are reported in Table 3.
Figure 2.
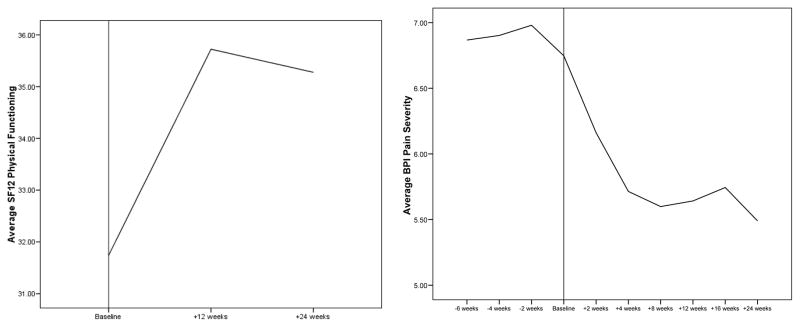
Average Physical Function and Pain Severity Over Time
Table 3.
Adjusted Regression (HLM) Coefficients for Pain Severity and Physical Function
| SF12 Physical functioning | BPI Pain Severity | |||||||
|---|---|---|---|---|---|---|---|---|
| Estimate | 95% Confidence Interval | Sig. | Estimate | 95% Confidence Interval | Sig. | |||
| Treatment period | 3.03 | 4.81 | 1.24 | <.001 | −0.71 | −0.40 | −1.03 | <.001 |
| Post-treatment period | 2.61 | 4.47 | 0.77 | 0.006 | −0.41 | 0.77 | −1.59 | 0.496 |
| Time (weeks centered around baseline) | - | - | - | - | −0.04 | −0.13 | 0.04 | 0.117 |
| Time x Treatment Period | - | - | - | - | −0.02 | 0.04 | −0.08 | 0.554 |
| Time x Post-Treatment Period | - | - | - | - | −0.01 | 0.07 | −0.08 | 0.854 |
| Site | 0.44 | 0.744 | ||||||
| Site A | −0.55 | −3.68 | 2.58 | 0.12 | −0.36 | 0.60 | ||
| Site B | 2.00 | −1.50 | 5.50 | −0.20 | −0.74 | 0.35 | ||
| Site C | −0.66 | −3.45 | 2.13 | 0.00 | −0.43 | 0.43 | ||
| Site D | ref | ref | ref | ref | ref | ref | ||
| CPGS Disability score | −0.14 | −0.18 | −0.10 | <.001 | 0.04 | 0.03 | 0.04 | <.001 |
| Treatments received | 0.23 | 0.08 | 0.38 | 0.003 | - | - | - | - |
| Age | −0.18 | −0.26 | −0.10 | <.001 | - | - | - | - |
| Medicaid | - | - | - | - | 0.50 | 0.85 | 0.15 | 0.005 |
Almost one-third of participants (30.3%) experienced a 30% or greater improvement in pain and 39.9% experienced 20% or greater between baseline run-in period and last measurement; the overall sample experienced 11.5% improvement. Patient assessment of change was significantly related to change in pain severity and physical health following treatment (Table 4). Clinical global ratings (reported by acupuncturists) were not related to change in either outcome or patient impression of change.
Table 4.
Correlation between global assessment of change and observed change in outcomes.
| CGIC | ΔBPI | ΔSF12 | |
|---|---|---|---|
| Patient Global Impression of Change† | 0.132 | .293** | −.249* |
| Clinical Global Impression of change (CGIC)† | 0.166 | 0.001 | |
| Change in BPI (4-months post baseline) | −.277* |
<.05;
<.01;
lower scores
indicate greater improvement
DISCUSSION
The goals of this study were twofold. First, we sought to evaluate the feasibility and acceptability to patients and clinicians of offering acupuncture for chronic pain in the urban community health center setting, where it has rarely been available in the past. As we report elsewhere, we identified many patients with substantial chronic pain and related disability, and great enthusiasm among clinicians and patients for acupuncture. (24) We have also demonstrated a high level of engagement with treatment among this patient population, with over two thirds of our participants attending five or more acupuncture treatment sessions. This suggests that despite a lack of familiarity with the discipline and despite the many barriers to regular attendance in care experienced by patients in this setting, patients are motivated to incorporate acupuncture into their care in a serious and committed fashion.
Our second goal, and the focus of this report, was to evaluate the effectiveness of acupuncture in treating chronic pain in this setting. Here we were able to reach two important conclusions new to the literature on this subject. First, acupuncture offered in the primary care community health center setting to an ethnically and racially diverse and socioeconomically underprivileged population with moderate to severe chronic pain is associated with clinically and statistically significant reduction of pain in over 30% of subjects. Most clinical trials of acupuncture to date have not delivered the service in the primary care setting, and none to our knowledge have focused exclusively on a medically underserved, community health center-based population. Given the challenges primary care doctors face in the treatment of chronic pain, particularly with new concerns being raised regarding the use of narcotic medications, and the overall safety of acupuncture as a treatment, this finding has potentially great importance in the management of pain in this setting. Acupuncture also is significantly associated with improved functional status among patients with a high degree of baseline disability.
Second, we were able to demonstrate this level of effectiveness in a difficult-to-treat pain population using student acupuncturists who were available at no cost to the clinical sites or to the patients. Because the one-on-one delivery model most common in the U.S. is extremely expensive to deliver, cost has been a major barrier to providing acupuncture to uninsured or underinsured patients without private financial resources. The model developed and tested in ADDOPT—using student acupuncture teams under the supervision of acupuncture faculty as part of their clinical training—has potential as a means to provide this clinical service to underserved patients. Almost every major urban area in the U.S. has at least one acupuncture training program, and many of these schools seek clinical training sites within conventional health care settings where their students can gain experience. Critics may argue that the acupuncture care provided by students is of slightly lower quality than that provided by more experienced practitioners. This could explain why only 32% of our participants experienced 30% or greater reduction in pain score (compared to the 40–50% response rate seen in many studies). Yet the fact that this delivery model makes acupuncture available where it would otherwise not be feasible makes it an important approach to consider for community health centers interested in adding acupuncture to their options for chronic pain treatment.
Limitations
Several limitations should be acknowledged related to intervention delivery and study design. Our delivery model involved supervised students with related consequences. Constraints of the academic calendar resulted in more turnover of clinicians, and breaks in treatment course not typical of care in other settings. Though preceptors were highly experienced, the variable skill levels of student acupuncturists could have influenced outcomes. However, our design did allow for an individualized approach to treatment that more accurately reflects real-world acupuncture treatment than the fixed point protocols often used in clinical trials.
With regard to study design, in the absence of a randomized trial, we cannot say that the improvements we saw were due specifically to acupuncture. For example, it is possible that omitted variables, such as other concurrent treatment for pain, differential use of medications –prescribed and over-the-counter-could have contributed to the differences seen. There was also substantial variation in “dosage” -- the number of acupuncture treatments varied widely between patients. The exclusion of variables such as these, and that not all patients received the planned dosage, may result in misestimating the magnitude of the effect.
CONCLUSION
Referred primary care patients experienced high levels of pain and pain-related disability. In this setting, weekly acupuncture was associated with statistically significant improvements in pain and quality of life. The model developed here of bringing acupuncturists-in-training directly into the primary care setting for an underserved population is effective and viable as a way to deliver a non-pharmacological approach to the management of chronic pain in this setting.
Acknowledgments
Funding: Supported by the National Center for Complementary and Alternative Medicine
Footnotes
Conflicts or competing interests: None
Contributor Information
M. Diane McKee, Albert Einstein College of Medicine.
Benjamin Kligler, Beth Israel Medical Center.
Jason Fletcher, Albert Einstein College of Medicine.
Francesca Biryukov, Swedish Institute.
William Casalaina, Swedish Institute.
Belinda Anderson, Pacific College of Oriental Medicine.
Arthur Blank, Albert Einstein College of Medicine.
References
- 1.Elliott AM, Smith BH, Penny KI, Smith WC, Chambers WA. The epidemiology of chronic pain in the community. Lancet. 1999;354(9186):1248–52. doi: 10.1016/s0140-6736(99)03057-3. [DOI] [PubMed] [Google Scholar]
- 2.Gureje O, Von Korff M, Simon GE, Gater R. Persistent pain and well-being: a World Health Organization Study in Primary Care. JAMA. 1998;280(2):147–51. doi: 10.1001/jama.280.2.147. [DOI] [PubMed] [Google Scholar]
- 3.Reyes-Gibby CC, Aday L, Cleeland C. Impact of pain on self-rated health in the community-dwelling older adults. Pain. 2002;95(1–2):75–82. doi: 10.1016/s0304-3959(01)00375-x. [DOI] [PubMed] [Google Scholar]
- 4.Von Korff M, Dworkin SF, Le Resche L. Graded chronic pain status: an epidemiologic evaluation. Pain. 1990;40(3):279–91. doi: 10.1016/0304-3959(90)91125-3. [DOI] [PubMed] [Google Scholar]
- 5.Verhaak PF, Kerssens JJ, Dekker J, Sorbi MJ, Bensing JM. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain. 1998;77(3):231–9. doi: 10.1016/S0304-3959(98)00117-1. [DOI] [PubMed] [Google Scholar]
- 6.Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010;11(11):1230–9. doi: 10.1016/j.jpain.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 7.Pargeon KL, Hailey BJ. Barriers to effective cancer pain management: a review of the literature. J Pain Symptom Manage. 1999;18(5):358–68. doi: 10.1016/s0885-3924(99)00097-4. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen M, Ugarte C, Fuller I, Haas G, Portenoy RK. Access to care for chronic pain: racial and ethnic differences. J Pain. 2005;6(5):301–14. doi: 10.1016/j.jpain.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;269(12):1537–9. [PubMed] [Google Scholar]
- 10.Todd KH, Deaton C, D’Adamo AP, Goe L. Ethnicity and analgesic practice. Ann Emerg Med. 2000;35(1):11–6. doi: 10.1016/s0196-0644(00)70099-0. [DOI] [PubMed] [Google Scholar]
- 11.Watkins E, Wollan PC, Melton LJ, 3rd, Yawn BP. Silent pain sufferers. Mayo Clin Proc. 2006;81(2):167–71. doi: 10.4065/81.2.167. [DOI] [PubMed] [Google Scholar]
- 12.Elliott AM, Smith BH, Hannaford PC, Smith WC, Chambers WA. The course of chronic pain in the community: results of a 4-year follow-up study. Pain. 2002;99(1–2):299–307. doi: 10.1016/s0304-3959(02)00138-0. [DOI] [PubMed] [Google Scholar]
- 13.Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S. The health and productivity cost burden of the “top 10” physical and mental health conditions affecting six large U.S. employers in 1999. J Occup Environ Med. 2003;45(1):5–14. doi: 10.1097/00043764-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Berman BM, Lao L, Langenberg P, Lee WL, Gilpin AM, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004;141(12):901–10. doi: 10.7326/0003-4819-141-12-200412210-00006. [DOI] [PubMed] [Google Scholar]
- 15.Scharf HP, Mansmann U, Streitberger K, Witte S, Kramer J, Maier C, et al. Acupuncture and knee osteoarthritis: a three-armed randomized trial. Ann Intern Med. 2006;145(1):12–20. doi: 10.7326/0003-4819-145-1-200607040-00005. [DOI] [PubMed] [Google Scholar]
- 16.Manheimer E, Linde K, Lao L, Bouter LM, Berman BM. Meta-analysis: acupuncture for osteoarthritis of the knee. Ann Intern Med. 2007;146(12):868–77. doi: 10.7326/0003-4819-146-12-200706190-00008. [DOI] [PubMed] [Google Scholar]
- 17.Willich SN, Reinhold T, Selim D, Jena S, Brinkhaus B, Witt CM. Cost-effectiveness of acupuncture treatment in patients with chronic neck pain. Pain. 2006;125(1–2):107–13. doi: 10.1016/j.pain.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 18.Witt CM, Jena S, Brinkhaus B, Liecker B, Wegscheider K, Willich SN. Acupuncture for patients with chronic neck pain. Pain. 2006;125(1–2):98–106. doi: 10.1016/j.pain.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 19.Manheimer E, White A, Berman B, Forys K, Ernst E. Meta-analysis: acupuncture for low back pain. Ann Intern Med. 2005;142(8):651–63. doi: 10.7326/0003-4819-142-8-200504190-00014. [DOI] [PubMed] [Google Scholar]
- 20.Brinkhaus B, Witt CM, Jena S, Linde K, Streng A, Wagenpfeil S, et al. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med. 2006;166(4):450–7. doi: 10.1001/archinte.166.4.450. [DOI] [PubMed] [Google Scholar]
- 21.Haake M, Muller HH, Schade-Brittinger C, Basler HD, Schafer H, Maier C, et al. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167(17):1892–8. doi: 10.1001/archinte.167.17.1892. [DOI] [PubMed] [Google Scholar]
- 22.Cherkin DC, Sherman KJ, Avins AL, Erro JH, Ichikawa L, Barlow WE, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009;169(9):858–66. doi: 10.1001/archinternmed.2009.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yuan J, Purepong N, Kerr DP, Park J, Bradbury I, McDonough S. Effectiveness of acupuncture for low back pain: a systematic review. Spine (Phila Pa 1976) 2008;33(23):E887–900. doi: 10.1097/BRS.0b013e318186b276. [DOI] [PubMed] [Google Scholar]
- 24.McKee MD, Kligler B, Blank AE, Fletcher J, Jeffres A, Casalaina W, et al. The ADDOPT study (Acupuncture to Decrease Disparities in Outcomes of Pain Treatment): feasibility of offering acupuncture in the community health center setting. J Altern Complement Med. 2012;18(9):839–43. doi: 10.1089/acm.2011.0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Glasgow RE, Magid DJ, Beck A, Ritzwoller D, Estabrooks PA. Practical clinical trials for translating research to practice: design and measurement recommendations. Med Care. 2005;43(6):551–7. doi: 10.1097/01.mlr.0000163645.41407.09. [DOI] [PubMed] [Google Scholar]
- 26.Gracely E. The Role of Quasi-Experimental Designs in Pain Research. Pain Medicine. 2004;5(2):146–7. doi: 10.1111/j.1526-4637.2004.04023.x. [DOI] [PubMed] [Google Scholar]
- 27.Nielsen A, Hammerschlag R. In: Acupuncture in East Asian Medicine. Integrative medicine: principles for practice. 1. Kligler Benjamin Lee, Roberta A., editors. New York: McGraw-Hill, Medical Pub. Div; 2004. p. xxiii.p. 936. [Google Scholar]
- 28.Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain. 2004;5(2):133–7. doi: 10.1016/j.jpain.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 29.Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50(2):133–49. doi: 10.1016/0304-3959(92)90154-4. [DOI] [PubMed] [Google Scholar]
- 30.Weidenhammer W, Linde K, Streng A, Hoppe A, Melchart D. Acupuncture for chronic low back pain in routine care: a multicenter observational study. Clin J Pain. 2007;23(2):128–35. doi: 10.1097/01.ajp.0000210952.09127.df. [DOI] [PubMed] [Google Scholar]
- 31.Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9(2):105–21. doi: 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 32.Mease PJ, Spaeth M, Clauw DJ, Arnold LM, Bradley LA, Russell IJ, et al. Estimation of minimum clinically important difference for pain in fibromyalgia. Arthritis Care Res (Hoboken) 2011;63(6):821–6. doi: 10.1002/acr.20449. [DOI] [PubMed] [Google Scholar]
- 33.Kosinski M, Ware JE, Turner-Bowker D, Gandek B, et al. Improvements in the SF-12 Health Survey: The SF-12v2. Journal of Clinical Epidemiology. 2008 [Google Scholar]
- 34.Samsa G, Edelman D, Rothman ML, Williams GR, Lipscomb J, Matchar D. Determining clinically important differences in health status measures: a general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics. 1999;15(2):141–55. doi: 10.2165/00019053-199915020-00003. [DOI] [PubMed] [Google Scholar]
- 35.Raudenbach SW, Bryk AS. Hierarchical Linear Models: Applications and data analysis methods. 2. Thousand Oaks (CA): Sage; 2002. [Google Scholar]


