Abstract
This meta-analysis is a systematic compilation of research focusing on various exercise interventions and their impact on the health and behavior outcomes of healthy African American, Hispanic, Native American, and Native Hawaiian adults. Comprehensive searching located published and unpublished studies. Random-effects analyses synthesized data to calculate effect sizes (ES) as a standardized mean difference (d) and variability measures. Data were synthesized across 21,151 subjects in 100 eligible samples. Supervised exercise significantly improved fitness (ES=.571–.584). Interventions designed to motivate minority adults to increase physical activity changed subsequent physical activity behavior (ES=.172–.312) and anthropometric outcomes (ES=.070–.124). Some ES should be interpreted in the context of limited statistical power and heterogeneity. Attempts to match intervention content and delivery with minority populations were inconsistently reported. Healthy minority adults experienced health improvements following supervised exercise. Interventions designed to motivate subjects to increase physical activity have limited magnitude heterogeneous effects.
Keywords: Exercise, meta-analysis, minority groups, intervention studies
Inadequate physical activity (PA) is a leading preventable cause of morbidity and mortality.1 Insufficient PA is common among minority adults in the United States.2–4 Health disparities in major illnesses, such as cardiovascular disease and diabetes, may be partially attributable to insufficient PA.5–7 The urgent need to increase minority adults’ PA to improve important health outcomes has prompted numerous primary studies testing not only interventions to increase PA but also how PA interventions affect health outcomes.
Numerous narrative reviews have examined PA intervention studies conducted with minority adults.4, 5, 7–15 None of these reviews has quantitatively synthesized PA behavior or health outcomes to estimate effect sizes (ESs) across extant research. The reviews include unstated or narrow searches and inclusion criteria, narrow foci (e.g., studies in health care settings) and small numbers of primary studies.2, 5, 7, 10–13 Further, most reviews have included some studies with chronically ill adults and thus provide limited information about healthy minority adults. Previous reviews have not adequately distinguished studies with supervised exercise interventions, and verified exercise dose, from studies with interventions designed to motivate subjects to exercise. The Physical Activity Guideline Advisory Committee called for meta-analyses of PA studies, and this project answers that call.3 This meta-analysis addressed the following research questions:
What are the overall effects of supervised PA interventions with verified PA performance on physical fitness, lipids, anthropometric measures, diabetes risk, and mood outcomes among healthy minority adult samples?
What are the overall effects of PA motivation interventions on PA behavior outcomes, lipids, anthropometric outcomes, diabetes risk, and quality of life?
Methods
Standard research synthesis and meta-analysis methods were used to identify and obtain potential primary studies, determine eligibility, reliably extract data, execute meta-analytic statistical procedures, and interpret results.16,17, 18 For the purpose of this research the word minority is defined as individuals living in the United States, but descended from one of the following racial/ethnic groups: African American, Hispanic American, Native American Indian, or Native Hawaiian. Physical activity is defined as any bodily movement which raises energy expenditure beyond resting levels. Exercise (a subset of physical activity) is planned, structured, and repetitive physical activity focused on improving or maintaining physical fitness.
Data sources
Multiple search strategies were used to ensure a comprehensive search and limit bias while moving beyond previous reviews.19 An expert health sciences librarian used comprehensive searching with broad search terms in MEDLINE, EMBASE, Healthstar, Cochrane Controlled Trials Register, PsychINFO, Dissertation Abstracts International, Sport Discus, Combined Health Information Database, Nursing and Allied Health Database, Database of Abstracts of Reviews of Effectiveness, and Educational Resources Information Center (sample MEDLINE intervention terms: adherence, behavior therapy, clinical trial, compliance, counseling, evaluation, evaluation study, evidence-based medicine, health care evaluation, health behavior, health education, health promotion, intervention, outcome & process assessment, patient education, program, program development, program evaluation, self care, treatment outcome, validation study; PA terms: exercise, exertion, exercise therapy, physical activity, physical fitness, physical education & training, walking). Terms for minority studies were not used to narrow the search because these terms are inconsistently applied to primary studies and thus would have failed to locate some eligible studies. Searches were completed for 1960 through 2009, depending on database availability. Ancestry searches were completed on all eligible studies and previous review papers. The mRCT database, which contains 14 active registers and 16 archived registers, and the National Institutes of Health Computer Retrieval of Information on Scientific Projects database of funded studies were searched back to 1973. Computerized database searches were conducted using names of principal investigators of funded studies and for the first three authors of eligible studies. Author searches were completed for dissertations to determine if published reports were available; dissertations were included when publications were not found. Hand searches in 114 journals that frequently published PA intervention reports were completed. Hand searches began with examination of article titles for either PA or exercise terms; articles with suggestive titles were examined to locate eligible studies.
Study selection
Research studies which tested PA interventions among predominantly minority adults were included. Studies of children and youth younger than 18 years of age were not included because different interventions may be required due to differences in children’s developmental state, Studies were thinking capacity/patterns, and ability to make decisions independent of parental authority. limited to those reported in English between 1960 and early 2010. The 50-year time span for eligible primary studies was selected to facilitate a comprehensive review. Although many changes have occurred between 1960 and 2010, there is little reason to believe these changes would affect health outcomes of supervised exercise or outcomes of interventions designed to motivate individuals to increase PA. Primary studies were included if the report described the sample as healthy. Studies of samples with acute or chronic mental (e.g., schizophrenia, clinical depression, drug abuse) or physical (e.g., hypertension, diabetes, cardiovascular diseases) illnesses were excluded because this project focused on healthy adults. Both published and unpublished studies were included because the single biggest difference between published and unpublished research is the statistical significance of findings.20 Publication status is an inadequate proxy for study quality.20 Meta-analyses using only published research may overestimate the magnitude of effects. Physical activity interventions included supervised PA intervention sessions in which researchers verified exercise dose and PA motivation interventions with content designed to increase PA behavior but without any supervised PA. For supervised PA studies, outcomes were included only when the variables were measured within seven days after completion of the supervised PA intervention. For PA motivation interventions, outcomes were coded from the most distal data reported for each study since enduring behavior change is more important than immediate changes that may not persist over time.
Small-sample studies, which often lack statistical power to detect treatment effects, were included if they reported data for at least five subjects. These studies may include difficult-to-recruit samples or may test novel interventions.19 Studies were weighted so that those with larger samples had proportionally more influence on aggregate findings. Given variations in primary study quality, several strategies were considered for addressing primary study quality (e.g., setting scientific rigor inclusion criteria, weighting effect sizes by individual quality attributes, weighting effect sizes by an overall study quality score). These approaches were not selected because study design quality and study report quality are often confounded, little agreement exists on the most important study quality attributes in specific areas of science, and study quality scales lack validity. Both experimental and pre-experimental studies were included. Pre-experimental studies with single-group designs were included because some investigators find it unethical to withhold interventions from comparison groups, and because some evaluations of existing programs can contribute to meta-analyses. Single-group studies were analyzed separately from two-group studies. Single-group findings are reported here as ancillary findings to the more valid two-group treatment vs. control results. Effect sizes were calculated for control group pre-post comparisons to determine if participation in studies affected outcome variables.
Data extraction and analyses
A codebook addressing source characteristics, participant attributes, experimental characteristics, and study findings was prepared. The codebook was composed of individual questions with structured possible answers for converting study information to numerical values for analyses. The codebook was developed from previous meta-analyses which examined PA interventions, PA experts, and a review of available data in primary reports.21–23 Pilot-testing of the codebook was conducted with 20 studies to revise and clarify coding. (The codebook is available from the corresponding author). Coded outcomes included PA behavior following interventions, physical fitness (maximal oxygen consumption), lipids (high-density lipoproteins, low-density lipoproteins, total cholesterol, total cholesterol:high density lipoprotein), anthropometric measures (body mass index, percent body fat, body weight), diabetes risk (fasting glucose, insulin resistance), mood (depression, anxiety, combined mood measures), and quality-of-life outcomes. Because primary study reports sometimes include multiple measures of some outcomes (e.g., report both percent body fat and body weight), a prioritized list of desirable outcome measures with strong validity was developed a priori to avoid potential bias toward statistically significant findings. Two extensively trained and closely supervised coders with graduate degrees independently coded every variable in every study. Outcome ES data were further verified by a third doctorally-prepared coder. All data were compared across coders to achieve 100% agreement on each variable. Coding differences were adjudicated by the principal investigator, other members of the research team, or by contacting corresponding authors for clarification. Multiple publications about the same study were used to extract data when different papers reported different outcomes.
Data analysis
All analyses were conducted separately for studies that tested supervised PA interventions and for studies which tested interventions designed to motivate subjects to increase their PA. Data calculations used standard meta-analytic approaches to develop standardized mean difference (d) ESs. Effect sizes were weighted by the inverse of varianceto give larger samples more influence.24, 25 Effect sizes were adjusted for bias.25 To acknowledge that individual ESs vary due both to subject-level sampling error and to other sources of variations among studies, analyses employed random-effects models.26 The random-effects weights are based on within study variance plus between studies variance. Intervention content and delivery, samples, instrumentation, and study execution and quality differ among PA studies. The random-effects model is appropriate given the expected heterogeneity among studies because it estimates the mean of a distribution of ESs across diverse studies.25, 26 The alternative model, the fixed-effect model, was not used to analyze the data because it assumes one true ES underlies all the primary studies which is not accurate for PA studies.25 Effect sizes were examined graphically and statistically (large externally standardized residuals) to identify outliers. Normal-theory standard errors were used to construct 95% confidence intervals for the common or mean ES and to test whether the ES was significantly different from 0.
Between-study homogeneity was assessed using a conventional heterogeneity statistic (Q). Heterogeneity was expected because statistical and clinical heterogeneity are common in behavior-change research.21 Heterogeneity was handled in three ways.27 First, random-effects analyses were used because they take into account unexplained heterogeneity. Second, heterogeneity was quantified in addition to the location parameter. Third, findings were interpreted in the context of discovered heterogeneity. A fourth possible strategy to handle heterogeneity, moderator analyses, was not used due to the limited amount of two-group comparison data available for each variable.
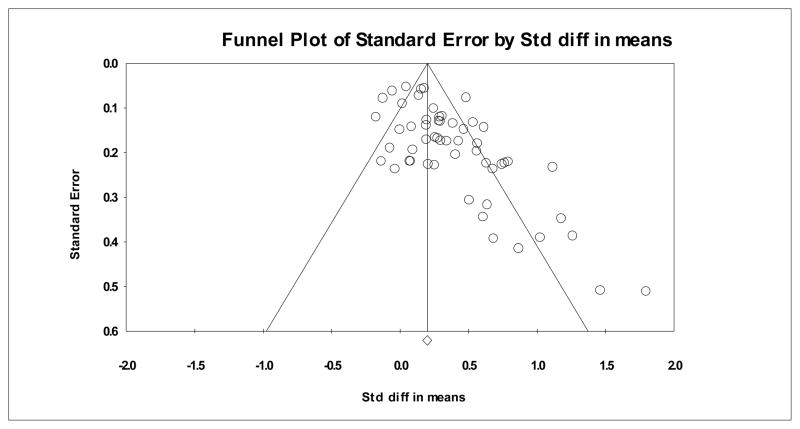
Both treatment and control group pre-post comparisons were analyzed when baseline data were available. Control group change information was explored to address partially common concerns about single-group designs. Studies with multiple treatment groups and no control groups were handled as single-group pre-post comparisons. The single-group treatment group findings were never combined with two-group findings. Funnel plots of ESs against sampling variance were developed to explore publication bias when at least 10 comparisons were available.28 Findings from funnel plots should be interpreted cautiously given the small number of cases for many variables. The funnel plot for the ES with the largest number of data points is presented in Figure 1. Funnel plots not included in the article are available from the corresponding author. Findings regarding publication bias should be viewed as exploratory, given the small number of ESs.
Figure 1.
Funnel plot for PA behavior outcomes of motivational and education interventions in single-group pre-post comparisons.
Results
Exhaustive searching located 54,893 possible studies. These numerous potential studies were considered because there are no reliable strategies to locate intervention studies or to specify studies focused on minority subjects. Although keywords (such as MESH headings) exist which one might think would identify relevant work, their application lacks sensitivity and specificity and thus they are not reliable to locate eligible studies. Careful examination of potential studies yielded 100 eligible samples from 77 research reports with a total of 21,151 subjects.29–105 The earliest study was published in 1990, only 18 papers were published prior to 2000. Most paper (s=59) were published from 2000 through 2010 (s indicates the number of reports, k indicates the number of comparisons). Thirty-two papers were published after 2004. More papers were published in 2005 (s=12) than any other year. Twelve studies were reported in multiple publications. Fifty-five reports were derived from funded studies.
Primary study characteristics
African American subjects were the predominant minority sample. See Tables 1, 2, and 3 for descriptive statistics for the entire sample, the supervised exercise intervention studies, and the motivational and education intervention primary studies, respectively. Fifty-three studies were composed entirely of African American participants, and another 15 comparisons included over 50% African American subjects. Nine studies targeted Hispanic American subjects exclusively, with 10 other studies reporting over 50% Hispanic American subjects. Few studies targeted exclusively Native American Indian (k=4) or Native Hawaiian (k=2) subjects. Most studies reported excluding European American subjects (k=73).
Table 1.
Characteristics of all primary studies included in meta-analyses
| Characteristic | k | Min | Q1 | Mdn | Q3 | Max |
|---|---|---|---|---|---|---|
| Treatment group sample size | 100 | 6 | 16 | 30 | 65 | 3226 |
| Control group sample size | 29 | 9 | 16 | 35 | 51 | 11153 |
| Percentage female | 89 | 0 | 84 | 100 | 100 | 100 |
| Percentage African-American | 97 | 0 | 30 | 100 | 100 | 100 |
| Percentage Hispanic | 94 | 0 | 0 | 0 | 23 | 100 |
| Percent European-American | 92 | 0 | 0 | 0 | 0 | 47 |
| Mean age (years) | 85 | 20 | 37.40 | 45.10 | 48.90 | 76.4 |
Note. Includes all studies that contributed to primary analyses at least one effect size for any type of comparison. Not all studies reported information in the table.
k = number of studies providing data on characteristic; Q1 = first quartile, Q3 = third quartile.
Table 2.
Characteristics of supervised exercise intervention primary studies included in meta-analyses
| Characteristic | k | Min | Q1 | Mdn | Q3 | Max |
|---|---|---|---|---|---|---|
| Treatment group sample size | 32 | 6 | 12.5 | 18.5 | 55 | 198 |
| Control group sample size | 13 | 9 | 12 | 18 | 39 | 135 |
| Percentage female | 32 | 0 | 84 | 100 | 100 | 100 |
| Percentage African-American | 32 | 0 | 64 | 100 | 100 | 100 |
| Percentage Hispanic | 29 | 0 | 0 | 0 | 21 | 100 |
| Percent European-American | 28 | 0 | 0 | 0 | 0 | 36 |
| Mean age (years) | 30 | 20 | 33 | 44 | 56.3 | 76.4 |
| Minutes of supervised exercise per session | 23 | 25 | 32.5 | 38.5 | 52.5 | 60 |
| Frequency per week of supervised PA | 27 | 1 | 2 | 3 | 3 | 4 |
| Total number of supervised exercise sessions | 27 | 8 | 20 | 33 | 48 | 84 |
Note. Includes all studies that contributed to primary analyses at least one effect size for any type of comparison. Not all studies reported information in the table.
k = number of studies providing data on characteristic; Q1 = first quartile, Q3 = third quartile.
Table 3.
Characteristics of motivational and educational intervention exercise primary studies included in meta-analyses
| Characteristic | k | Min | Q1 | Mdn | Q3 | Max |
|---|---|---|---|---|---|---|
| Treatment group sample size | 68 | 7 | 22 | 35 | 71 | 3226 |
| Control group sample size | 16 | 12 | 20.5 | 36.5 | 68 | 11153 |
| Percentage female | 57 | 0 | 0 | 100 | 100 | 100 |
| Percentage African-American | 65 | 0 | 21 | 100 | 100 | 100 |
| Percentage Hispanic | 65 | 0 | 0 | 0 | 30 | 100 |
| Percent European-American | 64 | 0 | 0 | 0 | 4 | 47 |
| Mean age (years) | 55 | 26.5 | 39.6 | 45.9 | 48.46 | 68.3 |
| Minutes of motivation content/session | 28 | 15 | 32.5 | 48.75 | 60.0 | 90 |
| Total number of motivation sessions | 29 | 1 | 5 | 10 | 22 | 54 |
Note. Includes all studies that contributed to primary analyses at least one effect size for any type of comparison. Not all studies reported information in the table.
k = number of studies providing data on characteristic; Q1 = first quartile, Q3 = third quartile.
Many studies did not report strategies to align the project (recruitment, intervention, or delivery) with the target population group. Information from the few studies which reported strategies to ensure minority recruitment, aligned interventions with minority participants or both are reported below. Fourteen reports indicated that at least one member of the research team was a member of the target minority group. Thirteen studies reported using literature about the target minority for planning interventions. Nineteen studies used data the researchers collected from members of the target minority to design interventions. Twenty-five intervention delivery sites were selected for appropriateness, based on the target minority group. Twenty-three studies recruited subjects in locations frequented by members of the target population. Three reports indicated the study employed members of the target group for recruitment. Seven studies both recruited subjects at target-minority locations and used recruiters of the minority group. Twelve reports indicated interventions were delivered in churches. Four of these studies used church staff to help in interventions.
Although a few very large studies were included in the meta-analysis, most studies reported modest sample sizes with a median of 30 subjects in the treatment group (Table 1). Studies predominantly included female subjects. Although a few studies focused on younger and older adults, middle-aged participants were most common (median age 45 years). Although few studies intentionally recruited overweight or obese samples, nearly half of the studies (k=44) reported that more than half of the sample was overweight (body mass index=25–29.9), and 22 noted that over half of the participants were obese (body mass index≥ 30). Information about socioeconomic status was not summarized because it was infrequently reported in the primary studies.
Tables 2 and 3 contain some information about the interventions. The typical supervised exercise intervention included nearly 40 minutes of verified exercise three times weekly over 11 weeks. Supervised PA studies most often used moderate-intensity exercise (k=19), followed by low-intensity (k=3) and high-intensity (k=1). Details of PA motivation intervention dose were inconsistently reported, so findings in Table 3 should be interpreted with caution. The typical PA motivation intervention was of 10 sessions lasting 49 minutes.
Effects of supervised exercise interventions
Random-effects outcome estimates and tests for supervised exercise interventions are reported in Table 4. Fitness results indicated moderate ESs for both 2-group (.571) and treatment pre-post (.584) comparisons. Fitness outcomes for both comparisons were significantly heterogeneous (Q in Table 4). Funnel plots revealed no evidence of publication bias for fitness outcomes in treatment group pre- vs. post- intervention comparisons. Lipids improvements were not statistically different from 0. The lipid 2-group analyses had little statistical power given the very low number of comparisons (k=2). The lipid single-group ES was significantly heterogeneous (Q=17.726).
Table 4.
Random-effects outcome estimates and tests for supervised physical activity interventions
| Comparison | k | ES | p (ES) | 95% CI | SE | Q | p (Q) |
|---|---|---|---|---|---|---|---|
| Fitness | |||||||
| Treatment vs. control groups at post-test | 7 | .571 | .012 | .127, 1.015 | .226 | 17.239 | .008 |
| Treatment group pre- vs. post-test | 16 | .584 | <.001 | .431, .737 | .078 | 23.622 | .072 |
| Control group pre- vs. post-test | 6 | .073 | .519 | −.149, .294 | .113 | 1.010 | .962 |
| Lipids | |||||||
| Treatment vs. control groups at post-test | 2 | .286 | .180 | −.132, .704 | .213 | 1.752 | .186 |
| Treatment group pre- vs. post-test | 7 | .227 | .062 | −.011, .465 | .121 | 17.726 | .007 |
| Control group pre- vs. post-test | 2 | .044 | .828 | −.350, .437 | .201 | 2.719 | .099 |
| Anthropometric outcomes | |||||||
| Treatment vs. control groups at post-test | 9 | .041 | .643 | −.132, .214 | .088 | 7.276 | .507 |
| Treatment group pre- vs. post-test | 20 | .104 | .010 | .025, .182 | .040 | 13.956 | .786 |
| Control group pre- vs. post-test | 9 | −.036 | .563 | −.156, .085 | .062 | 1.229 | .996 |
| Diabetes risk | |||||||
| Treatment vs. control groups at post-test | - | - | - | - | - | - | - |
| Treatment group pre- vs. post-test | 5 | −.064 | .793 | −.539, .412 | .243 | 19.407 | .001 |
| Control group pre- vs. post-test | - | - | - | - | - | - | - |
| Mood | |||||||
| Treatment vs. control groups at post-test | 2 | .198 | .365 | −.231, .627 | .219 | 2.194 | .139 |
| Treatment group pre- vs. post-test | 4 | .410 | .021 | .063, .757 | .177 | 17.212 | .001 |
| Control group pre- vs. post-test | 2 | .119 | .308 | −.110, .348 | .117 | .016 | .900 |
k: number of comparisons; ES: effect size; 95%CI: 95% confidence interval; SE: standard error; Q: heterogeneity statistic
Although the treatment group pre-post comparison for anthropometric outcomes achieved statistical significance, the magnitude of the effect was small (.104). Anthropometric outcomes of 2-groups comparisons did not find better outcomes among treatment as compared to control subjects. Anthropometric ESs were homogenous. Funnel plots revealed some evidence of publication bias for anthropometric outcomes in treatment group pre- vs. post- intervention comparisons. Diabetes risk was unchanged in treatment group pre-post comparisons. The significant improvement in mood among subjects in single-group comparisons (ES = .410) was not verified in the two studies reporting treatment vs. control group outcomes. The moderate mood ES for single-group comparisons was significantly heterogeneous. No studies reported quality-of-life outcomes of supervised PA interventions. Control group pre-post comparisons documented no significant positive benefits from study participation on fitness, lipids, anthropometric outcomes, or mood outcomes.
Effects of PA motivation interventions
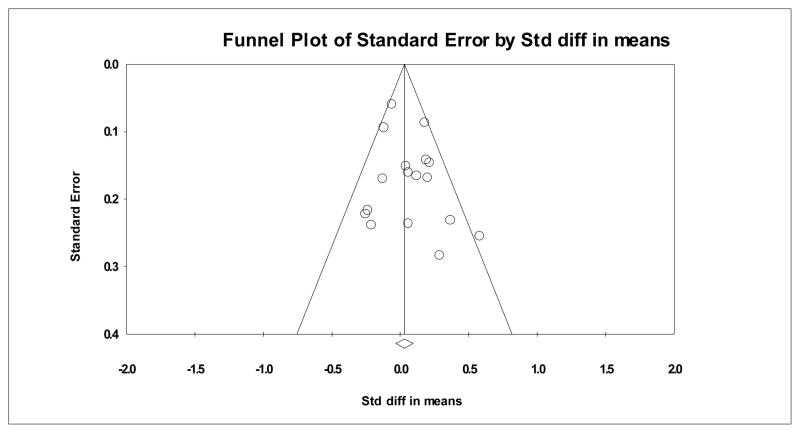
Random-effects outcome estimates and tests for PA motivation interventions that were designed to increase PA but that lacked verified PA performance are reported in Table 5. Interventions effectively increased PA behavior as documented for both 2-group (ES = .172) and treatment-group pre-post (ES=.312) comparisons. PA behavior ESs were very heterogeneous (Q in Table 5). Figure 1 presents the funnel plot for PA behavior outcomes among the treatment group pre-post comparisons. The asymmetry in Figure 1 provides evidence of possible publication bias. In contrast, the plot for the control group pre- vs. post-intervention comparison (Figure 2) does not suggest publication bias.
Table 5.
Random-effects outcome estimates and tests for motivational and education interventions designed to increase physical activity
| Comparison | k | ES | p (ES) | 95% CI | SE | Q | p (Q) |
|---|---|---|---|---|---|---|---|
| Physical activity behavior | |||||||
| Treatment vs. control groups at post-test | 21 | .172 | .024 | .023, .321 | .076 | 89.309 | <.001 |
| Treatment group pre- vs. post-test | 55 | .312 | <.001 | .237, .386 | .038 | 203.128 | <.001 |
| Control group pre- vs. post-test | 17 | .053 | .251 | −.037, .142 | .046 | 24.777 | .074 |
| Lipids | |||||||
| Treatment vs. control groups at post-test | 4 | .005 | .976 | −.305, .314 | .158 | .578 | .902 |
| Treatment group pre- vs. post-test | 20 | .109 | .087 | −.016, .234 | .064 | 59.362 | .000 |
| Control group pre- vs. post-test | 3 | −.217 | .074 | −.455, .021 | .121 | .736 | .692 |
| Anthropometric outcomes | |||||||
| Treatment vs. control groups at post-test | 9 | .124 | .077 | −.014, .262 | .070 | 4.530 | .806 |
| Treatment group pre- vs. post-test | 43 | .070 | .001 | .027, .112 | .022 | 23.031 | .992 |
| Control group pre- vs. post-test | 8 | −.069 | .195 | −.173, .035 | .053 | 5.580 | .590 |
| Diabetes risk | |||||||
| Treatment vs. control groups at post-test | 2 | −.024 | .899 | −.393, .345 | .188 | .324 | .569 |
| Treatment group pre- vs. post-test | 11 | .041 | .225 | −.025, .108 | .034 | 9.383 | .496 |
| Control group pre- vs. post-test | 2 | −.521 | .414 | −1.771, .729 | .638 | 17.475 | <.001 |
| Quality of life | |||||||
| Treatment vs. control groups at post-test | - | - | - | - | - | - | - |
| Treatment group pre- vs. post-test | 3 | .464 | .108 | −.102, 1.031 | .289 | 16.312 | <.001 |
| Control group pre- vs. post-test | - | - | - | - | - | - | - |
k: number of comparisons; ES: effect size; 95%CI: 95% confidence interval; SE: standard error; Q: heterogeneity statistic
Figure 2.
Funnel plot for PA behavior outcomes of motivational and education interventions in control group pre-post comparisons.
Anthropometric outcomes improved significantly in the treatment group pre-post comparison, but the magnitude of the effect (ES=.070) is small and probably not clinically meaningful. The funnel plot for this outcome did not suggest publication bias. Neither lipid nor diabetes risks significantly improved in any of the comparisons. The funnel plots for the treatment group pre- vs. post-intervention comparisons for both anthropometric and diabetes risk outcomes showed no evidence of publication bias. The quality of life outcome ES was moderate sized (ES = .464) but did not achieve statistical significance, probably due to the small sample size (k=3). The single group comparisons for quality of life and lipids were significantly heterogeneous. Inadequate primary study data existed to synthesize finding for fitness or mood outcomes of PA motivation interventions.
Control group subjects did not experience any benefit in PA behavior, lipids, anthropometric outcomes, or diabetes risk by participating in studies. The pattern across lipids, anthropometric outcomes, and diabetes risk suggested trends toward decline in health outcomes among control subjects.
Findings from both the PA supervision and PA motivation interventions should be interpreted cautiously for analyses with small number of primary studies (small k values in Tables 4 and 5). These findings should be considered exploratory and hypothesis-generating.
Discussion
This study answered the Physical Activity Guideline Advisory Committee call for meta-analyses of PA intervention studies among minority adults which was based on accumulating primary studies.3 Our comprehensive search strategies yielded far more studies than previous narrative reviews. These findings documented that healthy minority adults experienced significant improvements in fitness following verified exercise stimuli in supervised exercise sessions. These improvements are important because they followed short-term exercise sessions, typically three times weekly for 11 weeks. Further improvements could accrue with more sustained exercise over many months or years. Better outcomes might also follow exercise variations such as increased intensity or session frequency. Significant heterogeneity suggests some interventions were more effective than others. Insufficient primary studies were available to test supervised exercise dose, form, or intensity as potential moderators of ESs. Future work meta-analyses, when more studies accrue, should examine whether variations in geographic distribution, culture, and settings account for heterogeneity among studies.
Inadequate PA has been suggested as an important factor in overweight and obesity among minority adults.8 Some evidence suggests African Americans may have lower resting metabolic rates than European Americans that is not explained by differences in age or fat-free mass.106 Although adequate PA may prevent weight gain, the findings from these primary studies documented that supervised exercise sessions had little influence on anthropometric measures over the limited timeframe of these studies. Motivation interventions were followed by small improvements. For both PA supervision and PA motivation interventions, these small improvements in treatment subjects contrasted with a pattern of deterioration in anthropometric outcomes among control subjects. Exercise may be more effective in preventing weight gain than to promote weight reduction. Although exercise is often recommended to reduce weight, muted exercise effects on weight change are common. Exercise alone only modestly reduces weight.107, 108 It is unclear if exercise may be effective for improving anthropometric outcomes when performed over many months, instead of these short supervised PA trials, which averaged 11 weeks. Although guidelines differ with respect to the recommended amount and intensity of exercise necessary to provide health benefits, findings from recent an epidemiological study suggest that normal-weight women require 60 minutes of moderate-intensity activity every day to avoid long-term weight gain.109 Nevertheless, other health outcomes can follow increased PA regardless of changes in anthropometric outcomes.
Some health outcome ESs in this study may not have achieved statistical significance due to limited statistical power, those results (e.g., lipids) should be interpreted cautiously. After more studies accrue, these ESs will be more stable. PA motivation interventions had little effect on health outcomes, probably because of the modest ESs for PA behavior (.172–.312). The ESs for PA in this study are similar to a recent comprehensive meta-analysis across healthy adults (.19), but smaller than findings from chronically ill adults (.45) and an earlier meta-analysis with very limited search strategies (.72).18, 21, 23 Recent comprehensive meta-analyses of healthy adults and chronically ill adults reported that the proportion of minority subjects was not a significant moderator of PA behavior ESs.18, 21 The larger ES reported by Dishman and Buckworth than this study may reflect the present study’s much more comprehensive search strategies, which probably located more obscure studies with smaller ESs. The larger ESs among studies of chronically ill adults may reflect a window of opportunity when subjects are especially receptive to interventions for increasing PA. Healthy adults, such as those included in these primary studies, may not consider increasing PA a high priority in the midst of many other demands on their time and resources. Nevertheless, effective interventions are needed for increasing PA among healthy minority adults in order to reduce the burden of inactivity-related illnesses. The modest ES in this study should generate testing of more powerful interventions to change PA behavior.
Although the ES for PA is modest, it is important to note that the largest difference in mortality is between sedentary and mildly/moderately active people as compared to the smaller mortality reduction between moderately active and highly active adults.110 The heterogeneity of PA ESs document that interventions are variably effective. Variations in intervention content and delivery, samples included in studies, measures, study procedures, and study quality may have contributed to heterogeneity.111, 112 Once further primary studies are reported, moderator analyses may explore these sources of heterogeneity.
The primary studies targeted minority subjects, but rarely reported socioeconomic characteristics of samples. It is difficult to separate minority status or ethnicity from socioeconomic issues.113 Ethnicity and socioeconomic status are co-determinants of health outcomes. Even among studies controlling socioeconomic status, health disparities do not entirely disappear.113 Primary studies must consistently record socioeconomic attributes of samples to clearly describe participants, as well as provide data for future moderator analyses. Future meta-analyses examining the intersection between socioeconomic and minority characteristics should be very informative.
This meta-analysis was limited by the available primary studies. Despite comprehensive searching, some primary studies may not have been not located. Many of the eligible studies we retrieved were not labeled as minority studies in computerized database structured language (e.g., MESH headings). The scant research on Hispanic American and Native American populations is unfortunately common across topics.5 Hispanic American adults have low levels of PA.2 African American and other minority categories used in this report are not composed of entirely homogeneous groups. Many diverse samples may be grouped together in these broad categories. These differences may impact PA study findings. Unfortunately, too few studies were retrieved to conduct moderator analyses between groupings (e.g., between African American and Hispanic American) or between diverse samples within groupings. Although minority subjects have been poorly represented in trials of interventions to increase PA, 114, 109 this study located far more studies of healthy African American adults than other minority populations.114
The strong inclusion of women in the primary studies is important because adequate PA is especially important for minority women, who have increased rates of cardiovascular disease.8 The preponderance of female subjects in the primary studies is also a limitation. Findings may have limited generalizability to males. Recruitment of male minority samples may be especially difficult given common strategies for recruitment may be biased toward females (e.g., religious settings). Both genders must be represented in primary study samples for valid generalizable findings. The heterogeneous findings document the significant differences among studies, but inadequate studies prevented moderator analyses to explore sources of heterogeneity.
The meta-analysis was also limited to the information reported among the retrieved primary studies. We used multiple publications to code information about individual studies when those publications were cited in the index paper or we located the additional paper via author name searches. Some information may have appeared in additional publications we did not locate. Few studies reported attrition rates, and those who reported attrition rarely explained the point in the study where subjects were lost (e.g., after consent but before baseline data collection, during interventions, after interventions but before outcome data collection). Attrition may influence findings in unknown ways. Studies which did not report PA behavior outcomes provided little information about PA behavior among control subjects. A similar lack of information was reported about treatment integrity in terms of the extent to which treatment subjects completed supervised PA session.
Although all of the primary studies targeted minority adults, many studies did not report specific strategies to align the study with minority participants. Most strategies reported by the few studies which provided this information were surface matching, not deeper cultural matching.114–116 Descriptions of interventions rarely stated that they were designed to match cultural norms.115, 117 Programs with religious links were faith-placed instead of faith-based.118 Faith-placed interventions were developed by investigators without any emphasis on faith themes, then delivered by researchers in faith-related locations. Faith-based interventions incorporate faith themes in the intervention. Studies comparing culturally relevant interventions to standard interventions to determine if cultural relevance modifications are effective would move this area of science forward.12, 116
Despite the growing volume of primary studies testing PA interventions among minority adults, the quality of the primary studies is a problem.117 Primary studies reported varied measures of some outcomes and some measures were not ideal. For example, lipid measures sometimes examined only total cholesterol. Most retrieved studies used single treatment group pre-post designs. The field urgently needs randomized controlled trials with strong internal validity that can provide evidence about interventions tested among minority adults. In some reports, it is difficult to determine if the design and conduct of the study were methodologically flawed or if the study report inadequately described methodological features. As more studies become available, future meta-analysts will be able to conduct moderator analyses on study quality features to identify patterns in findings related to methodological attributes. As more rigorously designed studies are distributed, confidence in internal validity of findings will grow. Publication bias, selective reporting of studies with positive ESs over studies with smaller or negative ESs, was suggested by some of the funnel plots in this study. This is a widespread problem.111 Consumers of research should consider potential publication bias and study quality limitations when reviewing existing literature.
Primary studies often contained limited information about samples and study methods. Future publications of intervention studies conducted with minority samples should report:
Strategies to align the study with target participants (e.g., recruitment location, intervention delivery location, intervention content, interventionist),
Sample attributes (e.g., ethnicity, age, gender distribution, weight/BMI, socio-economic status),
Design characteristics (e.g., recruitment, retention/attrition, allocation procedure, control/comparison group management, management of missing data including from subjects lost to attrition),
Intervention details (e.g., theoretical underpinnings, behavior target [e.g., PA alone vs. PA plus diet], content, delivery [location, interventionist, possible mediated delivery], possible links with organizations [e.g., religious groups, social groups, worksites, health care systems], social context, dose [individual session dose, frequency, number of sessions]),
Baseline and outcome variables (e.g., measures used, means, standard deviations, sample size for each outcome variable at each measurement point).
These details will allow readers and future meta-analysts to completely understand methods, compute effect sizes for aggregation, and conduct moderator analyses to identify sample, design, and intervention characteristics linked with outcomes.
The primary studies designed to increase PA continue to focus on individual motivation. No research in this area uses ecological models, which understand behavior in the environment and context.11, 114, 119, 120 This may be particularly important for minority adults, who may disproportionately reside in areas with fewer, less varied, poorer quality, and less accessible PA locations.121
Physical activity levels are lower in minority populations, and health problems that might be prevented or delayed with adequate PA are more common among minority than majority populations.4, 6 This meta-analysis is the first synthesis of both PA supervision and PA motivation interventions that targeted minority samples. The quantified ESs are important to understand the effectiveness of previously tested interventions. The modest ES for PA should stimulate further work to identify the most effective interventions to achieve long-term increases in PA behavior. The limited effects of supervised exercise on some outcomes requires further testing of different exercise interventions (e.g., variations in intensity or frequency) over longer periods of time (e.g., 26 weeks instead of 12 weeks). Methodologically rigorous studies testing culturally consistent interventions in minority samples remain a vital area of science. Future meta-analysis moderator analyses that can identify characteristics of interventions associated with better health outcomes and PA behavior change can be conducted when more primary studies are completed.
Acknowledgments
Financial support provided by a grant from the National Institutes of Health (R01NR009656) to Vicki Conn, principal investigator.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Marcus BH, Williams DM, Dubbert PM, Sallis JF, King AC, Yancey AK, et al. Physical activity intervention studies: what we know and what we need to know: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation. 2006;114(24):2739–52. doi: 10.1161/CIRCULATIONAHA.106.179683. [DOI] [PubMed] [Google Scholar]
- 2.Perez A, Fleury J, Keller C. Review of Intervention Studies Promoting Physical Activity in Hispanic Women. West J Nurs Res. 2010;32(3):341–362. doi: 10.1177/0193945909351300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report. US Department of Health & Human Services; 2009. [Google Scholar]
- 4.Whitt-Glover MC, Kumanyika SK. Systematic review of interventions to increase physical activity and physical fitness in African-Americans. Am J Health Promot. 2009;23(6):S33–56. doi: 10.4278/ajhp.070924101. [DOI] [PubMed] [Google Scholar]
- 5.Davis AM, Vinci LM, Okwuosa TM, Chase AR, Huang ES. Cardiovascular health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007;64(5 Suppl):29S–100S. doi: 10.1177/1077558707305416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall WD, Clark LT, Wenger NK, Wright JT, Jr, Kumanyika SK, Watson K, et al. The Metabolic Syndrome in African Americans: a review. Ethn Dis. 2003;13(4):414–28. [PubMed] [Google Scholar]
- 7.Pekmezi D, Marquez B, Marcus-Black J. Health Promotion in Latinos. American Journal of Lifestyle Medicine. 2010;4(2):151–165. [Google Scholar]
- 8.Banks-Wallace J, Conn V. Interventions to promote physical activity among African American women. Public Health Nurs. 2002;19(5):321–35. doi: 10.1046/j.1525-1446.2002.19502.x. [DOI] [PubMed] [Google Scholar]
- 9.Blocker DE, Freudenberg N. Developing comprehensive approaches to prevention and control of obesity among low-income, urban, African-American women. J Am Med Wom Assoc. 2001;56(2):59–64. [PubMed] [Google Scholar]
- 10.Crook ED, Bryan NB, Hanks R, Slagle ML, Morris CG, Ross MC, et al. A review of interventions to reduce health disparities in cardiovascular disease in African Americans. Ethn Dis. 2009;19(2):204–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Fleury J, Lee SM. The social ecological model and physical activity in African American women. Am J Community Psychol. 2006;37(1–2):129–40. doi: 10.1007/s10464-005-9002-7. [DOI] [PubMed] [Google Scholar]
- 12.Pekmezi D, Jennings E. Physical Activity Interventions in Minority Populations. Current Cardiovascular Risk Reports. 2009;3:275–280. [Google Scholar]
- 13.Sharma M. Physical activity interventions in Hispanic American girls and women. Obesity Reviews. 2008;9(6):560–71. doi: 10.1111/j.1467-789X.2008.00501.x. [DOI] [PubMed] [Google Scholar]
- 14.Whitt-Glover MC, Brand DJ, Turner ME, Ward SA, Jackson EM. Increasing physical activity among African-American women and girls. Current Sports Medicine Reports. 2009;8(6):318–24. doi: 10.1249/JSR.0b013e3181c27ade. [DOI] [PubMed] [Google Scholar]
- 15.Yancey A, Kumanyika SK, Ponce N, McCarthy W, Fielding J, Leslie J, et al. Population-based interventions engaging communities of color in healthy eathing and active living: A review. Preventing Chronic Disease. 2004;1(1):1–18. [PMC free article] [PubMed] [Google Scholar]
- 16.Cooper H, Hedges L, Valentine J. The Handbook of Research Synthesis and Meta-Analysis. 2. New Yord City: Russell Sage; 2009. [Google Scholar]
- 17.Conn VS, Hafdahl AR, Cooper PS, Brown LM, Lusk SL. Meta-analysis of workplace physical activity interventions. Am J Prev Med. 2009;37(4):330–9. doi: 10.1016/j.amepre.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Conn VS, Hafdahl AR, Mehr DR. Interventions to Increase Physical Activity among Healthy Adults: Meta-Analysis of Outcomes. Am J Public Health. doi: 10.2105/AJPH.2010.194381. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Conn V, Isaramalai S, Rath S, Jantarakupt P, Wadhawan R, Dash Y. Beyond MEDLINE for literature searches. Journal of Nursing Scholarship. 2003;35(2):177–82. doi: 10.1111/j.1547-5069.2003.00177.x. [DOI] [PubMed] [Google Scholar]
- 20.Conn VS, Valentine JC, Cooper HM, Rantz MJ. Grey literature in meta-analyses. Nurs Res. 2003;52(4):256–61. doi: 10.1097/00006199-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Conn VS, Hafdahl AR, Brown SA, Brown LM. Meta-analysis of patient education interventions to increase physical activity among chronically ill adults. Patient Educ Couns. 2008;70(2):157–72. doi: 10.1016/j.pec.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Conn VS, Valentine JC, Cooper HM. Interventions to increase physical activity among aging adults: a meta-analysis. Ann Behav Med. 2002;24(3):190–200. doi: 10.1207/S15324796ABM2403_04. [DOI] [PubMed] [Google Scholar]
- 23.Dishman RK, Buckworth J. Increasing physical activity: a quantitative synthesis. Med Sci Sports Exerc. 1996;28(6):706–19. doi: 10.1097/00005768-199606000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Shaddish W, Haddock C. Combining estimates of effect size. In: Cooper H, Hedges L, Valentine J, editors. The handbook of research synthesis and meta-analysis. New York: Russell Sage Foundation; 2009. pp. 257–277. [Google Scholar]
- 25.Borenstein M, Hedges L, JH, Rothstein H. Introduction to Meta-Analyais. West Sussex, United Kingdom: John Wiley & Sons, Ltd; 2009. [Google Scholar]
- 26.Raudenbush S. Random effects models. In: Cooper H, Hedges L, Valentine J, editors. The handbook of research synthesis and meta-analysis. 2. New York, NY: Russell Sage Foundation; 2009. pp. 295–315. [Google Scholar]
- 27.Conn VS, Hafdahl AR, Mehr DR, LeMaster JW, Brown SA, Nielsen PJ. Metabolic effects of interventions to increase exercise in adults with type 2 diabetes. Diabetologia. 2007;50(5):913–21. doi: 10.1007/s00125-007-0625-0. [DOI] [PubMed] [Google Scholar]
- 28.Sutton AJ. Publicaton bias. In: Cooper H, Hedges L, Valentine J, editors. The Handbook of Research Synthesis and Meta-Analysis. 2. New York: Russell Sage Foundation; 2009. pp. 435–452. [Google Scholar]
- 29.Albright CL, Pruitt L, Castro C, Gonzalez A, Woo S, King AC. Modifying physical activity in a multiethnic sample of low-income women: one-year results from the IMPACT (Increasing Motivation for Physical ACTivity) project. Ann Behav Med. 2005;30(3):191–200. doi: 10.1207/s15324796abm3003_3. [DOI] [PubMed] [Google Scholar]
- 30.Annesi JJ. Effects of a Cognitive Behavioral Treatment Package on Exercise Attendance and Drop Out in Fitness Centers. European Journal of Sport Science. 2003;3(2):1–16. [Google Scholar]
- 31.Annesi JJ. Relations of changes in exercise self-efficacy, physical self-concept, and body satisfaction with weight changes in obese white and African American women initiating a physical activity program. Ethn Dis. 2007;17(1):19–22. [PubMed] [Google Scholar]
- 32.Ard JD, Rosati R, Oddone EZ. Culturally-sensitive weight loss program produces significant reduction in weight, blood pressure, and cholesterol in eight weeks. J Natl Med Assoc. 2000;92(11):515–23. [PMC free article] [PubMed] [Google Scholar]
- 33.Avila P, Hovell MF. Physical activity training for weight loss in Latinas: a controlled trial. International Journal of Obesity & Related Metabolic Disorders: Journal of the International Association for the Study of Obesity. 1994;18(7):476–82. [PubMed] [Google Scholar]
- 34.Bachar JJM, Lefler LJ, Reed L, McCoy T, Bailey R, Bell R. Cherokee Choices: A Diabetes Prevention Program for AMerican Indians. Preventing Chronic Disease. 2006;3(3):1–9. [PMC free article] [PubMed] [Google Scholar]
- 35.Baranowski T, Simons-Morton B, Hooks P, Henske J, et al. A center-based progam for exercise change among Black-American families. Health Education Quarterly. 1990 Sum;17(2):179–196. doi: 10.1177/109019819001700205. 1990. [DOI] [PubMed] [Google Scholar]
- 36.Becker DM, Yanek LR, Johnson WR, Jr, Garrett D, Moy TF, Reynolds SS, et al. Impact of a community-based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease. Circulation. 2005;111(10):1298–304. doi: 10.1161/01.CIR.0000157734.97351.B2. [DOI] [PubMed] [Google Scholar]
- 37.Bell AC, Swinburn BA, Amosa H, Scragg RK. A nutrition and exercise intervention program for controlling weight in Samoan communities in New Zealand. Int J Obes. 2001;25:920–927. doi: 10.1038/sj.ijo.0801619. [DOI] [PubMed] [Google Scholar]
- 38.Bergeron J, Couillard C, Despres JP, Gagnon J, Leon AS, Rao DC, et al. Race differences in the response of postheparin plasma lipoprotein lipase and hepatic lipase activities to endurance exercise training in men: results from the HERITAGE Family Study. Atherosclerosis. 2001;159(2):399–406. doi: 10.1016/s0021-9150(01)00515-9. [DOI] [PubMed] [Google Scholar]
- 39.Berry D, Savoye M, Melkus G, Grey M. An intervention for multiethnic obese parents and overweight children. Appl Nurs Res. 2007;20(2):63–71. doi: 10.1016/j.apnr.2006.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bond V, Bartels MN, Sloan RP, Millis RM, Zion AS, Andrews N, et al. Exercise training favourably affects autonomic and blood pressure responses during mental and physical stressors in African-American men. J Hum Hypertens. 2009;23(4):267–73. doi: 10.1038/jhh.2008.125. [DOI] [PubMed] [Google Scholar]
- 41.Bond V, Millis RM, Adams RG, Oke LM, Enweze L, Blakely R, et al. Attenuation of exaggerated exercise blood pressure response in African-American women by regular aerobic physical activity. Ethn Dis. 2005;15(4 Suppl 5):S5-10–3. [PMC free article] [PubMed] [Google Scholar]
- 42.Bopp MJ. Evaluation of a faith-based physical activity intervention. University of South Carolina; 2005. [Google Scholar]
- 43.Bouchard C, Leon AS, Rao DC, Skinner JS, Wilmore JH, Gagnon J. The HERITAGE family study. Aims, design, and measurement protocol. Med Sci Sports Exerc. 1995;27(5):721–9. [PubMed] [Google Scholar]
- 44.Burden RW, Kumar RN, Phillips DL, Borrego ME, Galloway JM. Hyperlipidemia in Native Americans: evaluation of lipid management through a cardiovascular risk reduction program. J Am Pharm Assoc (Wash) 2002;42(4):652–5. doi: 10.1331/108658002763029634. [DOI] [PubMed] [Google Scholar]
- 45.Campbell MK, Tessaro I, DeVellis B, Benedict S, Kelsey K, Belton L, et al. Effects of a tailored health promotion program for female blue-collar workers: health works for women. Prev Med. 2002;34(3):313–23. doi: 10.1006/pmed.2001.0988. [DOI] [PubMed] [Google Scholar]
- 46.Cardinal BJ, Cardinal MK. Changes in exercise behavior and exercise identity associated with a 14-week aerobic exercise class. Journal of Sport Behavior. 1997;20(4):377–386. [Google Scholar]
- 47.Cardinal B. Dissertation. Temple University; 1993. The effectiveness of the stages of change model and experimental exercise prescriptions in increasing female adults’ physical activity and exercise behavior. [Google Scholar]
- 48.Cardinal BJ, Sachs ML. Effects of mail-mediated, stage-matched exercise behavior change strategies on female adults’ leisure-time exercise behavior. J Sports Med Phys Fitness. 1996;36(2):100–7. [PubMed] [Google Scholar]
- 49.Chen AH, Sallis JF, Castro CM, Lee RE, Hickmann SA, William C, et al. A home-based behavioral intervention to promote walking in sedentary ethnic minority women: project WALK. Womens Health. 1998;4(1):19–39. [PubMed] [Google Scholar]
- 50.Chen AH-W. The effectiveness of a home-based intervention to promote walking in ethnic minority women. San Diego: University of california San Diego and San Diego State University; 1996. [Google Scholar]
- 51.Christ-Roberts CY, Pratipanawatr T, Pratipanawatr W, Berria R, Belfort R, Kashyap S, et al. Exercise training increases glycogen synthase activity and GLUT4 expression but not insulin signaling in overweight nondiabetic and type 2 diabetic subjects. Metabolism. 2004;53(9):1233–42. doi: 10.1016/j.metabol.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 52.Collins R, Lee RE, Albright CL, King AC. Ready to be physically active? The effects of a course preparing low-income multiethnic women to be more physically active. Health Educ Behav. 31(1):47–64. doi: 10.1177/1090198103255529. [DOI] [PubMed] [Google Scholar]
- 53.Cook C, Simmons G, Swinburn B, Stewart J. Changing risk behaviours for non-communicable disease in New Zealand working men--is workplace intervention effective? N Z Med J. 2001;114(1130):175–8. [PubMed] [Google Scholar]
- 54.Craft L, Freund KM, Culpepper L, Perna FM. Intervention study of exercise for depressive symptoms in women. Journal of Women’s Health. 2007;16(10):1499–1509. doi: 10.1089/jwh.2007.0483. [DOI] [PubMed] [Google Scholar]
- 55.D’Alonzo KT. Effects of an intervention to enhance exercise self-efficacy among Black and Hispanic college-age women. Newark, JJ: Rutgers The State University of New Jersey; 2002. [Google Scholar]
- 56.Doshi NJ, Hurley RS, Garrison ME, Stombaugh IS, et al. Effectiveness of a nutrition education and physical fitness training program in lowering lipid levels in the Black elderly. J Nutr Elder. 1994;13(3):23–33. doi: 10.1300/J052v13n03_02. [DOI] [PubMed] [Google Scholar]
- 57.Duey WJ, O’Brien WL, Crutchfield AB, Brown LA, Williford HN, Sharff-Olson M. Effects of exercise training on aerobic fitness in African-American females. Ethn Dis. 1998;8(3):306–11. [PubMed] [Google Scholar]
- 58.Dutton GR, Martin PD, Welsch MA, Brantley PJ. Promoting physical activity for low-income minority women in primary care. American Journal of Health Behavior. 2007;31(6):622–631. doi: 10.5555/ajhb.2007.31.6.622. [DOI] [PubMed] [Google Scholar]
- 59.Dutton GR. Effects of a primary care weight management intervention on physical activity in low-income African American women. Louisiana State University; 2005. [Google Scholar]
- 60.Early JL, Apovian CM, Aronne LJ, Fernstrom MH, Frank A, Greenway FL, et al. Sibutramine plus meal replacement therapy for body weight loss and maintenance in obese patients. Obesity. 2007;15(6):1464–72. doi: 10.1038/oby.2007.175. [DOI] [PubMed] [Google Scholar]
- 61.Elliott-Loyd MB. The Effect of an 18-Week Walking Program on Body Composition in Black and White Sedentary, Overweight Females (Black Women, White Women, Exercise) Atlanta: Georgia State University; 1998. [Google Scholar]
- 62.Engels H-J, Gretebeck RJ, Gretebeck KA, Jimenez L. Promoting healthful diets and exercise: efficacy of a 12-week after-school program in urban African Americans. J Am Diet Assoc. 2005;105(3):455–9. doi: 10.1016/j.jada.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 63.Fitzgibbon ML, Stolley MR, Ganschow P, Schiffer L, Wells A, Simon N, et al. Results of a faith-based weight loss intervention for black women. J Natl Med Assoc. 2005;97(10):1393–402. [PMC free article] [PubMed] [Google Scholar]
- 64.Fitzgibbon ML, Stolley MR, Schiffer L, Sanchez-Johnsen LAP, Wells AM, Dyer A. A combined breast health/weight loss intervention for Black women. Prev Med. 2005;40(4):373–83. doi: 10.1016/j.ypmed.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 65.Glass JN, Miller WC, Szymanski LM, Fernhall B, Durstine JL. Physiological responses to weight-loss intervention in inactive obese African-American and Caucasian women. J Sports Med Phys Fitness. 2002;42(1):56–64. [PubMed] [Google Scholar]
- 66.Goldfinger J, Arniella G, Wylie-Rosett J, Horowitz C. Project HEAL: Peer eduction leads to weight loss in Harlem. J Health Care Poor Underserved. 2008;19:180–192. doi: 10.1353/hpu.2008.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Grediagin A, Cody M, Rupp J, Benardot D, Shern R. Exercise intensity does not effect body composition change in untrained, moderately overfat women. J Am Diet Assoc. 1995;95(6):661–5. doi: 10.1016/s0002-8223(95)00181-6. [DOI] [PubMed] [Google Scholar]
- 68.Group TW. Cardiovascular Disease Prevention for Women Attending Breast and Cervical Cancer Screening Programs: The WISEWOMAN Projects. Prev Med. 1999;28:496–502. doi: 10.1006/pmed.1999.0462. [DOI] [PubMed] [Google Scholar]
- 69.Harralson TL, Emig JC, Polansky M, Walker RE, Cruz JO, Garcia-Leeds C. Un Corazon Saludable: factors influencing outcomes of an exercise program designed to impact cardiac and metabolic risks among urban Latinas. J Community Health. 2007;32(6):401–12. doi: 10.1007/s10900-007-9059-3. [DOI] [PubMed] [Google Scholar]
- 70.Harvey-Berino J, Rourke J. Obesity prevention in preschool native-american children: a pilot study using home visiting. Obes Res. 2003;11(5):606–11. doi: 10.1038/oby.2003.87. [DOI] [PubMed] [Google Scholar]
- 71.Hong K, Li Z, Wang HJ, Elashoff R, Heber D. Analysis of weight loss outcomes using VLCD in black and white overweight and obese women with and without metabolic syndrome. Int J Obes. 2005;29(4):436–42. doi: 10.1038/sj.ijo.0802864. [DOI] [PubMed] [Google Scholar]
- 72.Kanders BS, Ullmann-Joy P, Foreyt JP, Heymsfield SB, Heber D, Elashoff RM, et al. The black American lifestyle intervention (BALI): the design of a weight loss program for working-class African-American women. J Am Diet Assoc. 1994;94(3):310–2. doi: 10.1016/0002-8223(94)90374-3. [DOI] [PubMed] [Google Scholar]
- 73.Karanja N, Stevens VJ, Hollis JF, Kumanyika SK. Steps to soulful living (steps): a weight loss program for African-American women. Ethn Dis. 2002;12(3):363–71. [PubMed] [Google Scholar]
- 74.Keller C, Trevino RP. Effects of two frequencies of walking on cardiovascular risk factor reduction in Mexican American women. Res Nurs Health. 2001;24(5):390–401. doi: 10.1002/nur.1039. [DOI] [PubMed] [Google Scholar]
- 75.Kennedy BM, Paeratakul S, Champagne CM, Ryan DH, Harsha DW, McGee B, et al. A pilot church-based weight loss program for African-American adults using church members as health educators: a comparison of individual and group intervention. Ethn Dis. 2005;15(3):373–8. [PubMed] [Google Scholar]
- 76.Kochevar AJ, Smith KL, Bernard MA. Effects of a community-based intervention to increase activity in American Indian elders. J Okla State Med Assoc. 2001;94(10):455–60. [PubMed] [Google Scholar]
- 77.Kumanyika SK, Wadden TA, Shults J, Fassbender JE, Brown SD, Bowman MA, et al. Trial of family and friend support for weight loss in African American adults. Arch Intern Med. 2009;169(19):1795–804. doi: 10.1001/archinternmed.2009.337. [DOI] [PubMed] [Google Scholar]
- 78.Kumanyika SK, Shults J, Fassbender J, Whitt MC, Brake V, Kallan MJ, et al. Outpatient weight management in African-Americans: The healthy eating and lifestyle program (HELP) study. Prev Med. 2005;41:488–502. doi: 10.1016/j.ypmed.2004.09.049. [DOI] [PubMed] [Google Scholar]
- 79.Lee Re MMASJFCCMCAHHSA. Active vs. passive methods of recruiting ethnic minority women to a health promotion program. Ann Behav Med. 1997;19(4):378–384. doi: 10.1007/BF02895157. [DOI] [PubMed] [Google Scholar]
- 80.Martin PD, Rhode PC, Dutton GR, Redmann SM, Ryan DH, Brantley PJ. A primary care weight management intervention for low-income African American women. Obesity. 2006;14(8):1412–1420. doi: 10.1038/oby.2006.160. [DOI] [PubMed] [Google Scholar]
- 81.McNabb W, Quinn M, Kerver J, Cook S, Karrison T. The PATHWAYS church-based weight loss program for urban African-American women at risk for diabetes. Diabetes Care. 1997;20(10):1518–1523. doi: 10.2337/diacare.20.10.1518. [DOI] [PubMed] [Google Scholar]
- 82.Mulvihill MM, Hovell MF, Schade DH, Manzano R, Chase TR, Elvine-Kreis B, et al. Effects of a culturally tailored diabetes prevention intervention for low SES Latino women on fitness, exercise, BMI, nutrition/exercise knowledge and dietary fat avoidance. ADA. 1999 Abstracts from the 59th Scientific Session:A303. [Google Scholar]
- 83.Murrock CJ. Dance and physical activity in African American women. Cleveland: Case Western Reserve University; 2007. [Google Scholar]
- 84.Newton RL, Jr, Perri MG. A randomized pilot trial of exercise promotion in sedentary African-American adults. Ethn Dis. 2004;14(4):548–57. [PubMed] [Google Scholar]
- 85.Nichols GJ. Testing a culturally consistent behavioral outcomes strategy for cardiovascular disease risk reduction and prevention in low income African American women. College Park: University of Maryland; 1995. [Google Scholar]
- 86.Nicklas BJ, Dennis KE, Berman DM, Sorkin J, Ryan AS, Goldberg AP. Lifestyle intervention of hypocaloric dieting and walking reduces abdominal obesity and improves coronary heart disease risk factors in obese, postmenopausal, African-American and Caucasian women. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58(2):181–9. doi: 10.1093/gerona/58.2.m181. [DOI] [PubMed] [Google Scholar]
- 87.Nies MA, Artinian NT, Schim SM, Wal JS, Sherrick-Escamilla S. Effects of Lay Health Educator Interventions on Activity, Diet, and Health Risks in an Urban Mexican American Community. Journal of Primary Prevention. 2004 Dec;25(4):441–455. 2004. [Google Scholar]
- 88.Parikh P, Simon EP, Fei K, Looker H, Goytia C, Horowitz CR. Results of a Pilot Diabetes Prevention Intervention in East Harlem, New York City: Project HEED. Am J Public Health. 2010;100 (Suppl 1):S232–239. doi: 10.2105/AJPH.2009.170910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Plescia M, Herrick H, Chavis L. Improving health behaviors in an African American community: the Charlotte Racial and Ethnic Approaches to Community Health project. Am J Public Health. 2008;98(9):1678–84. doi: 10.2105/AJPH.2007.125062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pollock NW, Moreland MR, McCammon MR, Hickner RC, Shaw DK, Poehlman GS. Inability of low-intensity exercise to improve glycemic control in a rural, high-risk community. Med Sci Sports Exerc. 2000;32(5 Suppl):S217. [Google Scholar]
- 91.Poston WS, 2nd, Haddock CK, Olvera NE, Suminski RR, Reeves RS, Dunn JK, et al. Evaluation of a culturally appropriate intervention to increase physical activity. American Journal of Health Behavior. 2001;25(4):396–406. doi: 10.5993/ajhb.25.4.5. [DOI] [PubMed] [Google Scholar]
- 92.Quinn MT, McNabb WL. Training lay health educators to conduct a church-based weight-loss program for African American women... including commentary by Kaplan S. Diabetes Educator. 2001 Mar-Apr;27(2):231–8. doi: 10.1177/014572170102700209. [DOI] [PubMed] [Google Scholar]
- 93.Racette SB, Weiss EP, Obert KA, Kohrt WM, Holloszy JO. Modest lifestyle intervention and glucose tolerance in obese African Americans. Obes Res. 2001;9(6):348–55. doi: 10.1038/oby.2001.45. [DOI] [PubMed] [Google Scholar]
- 94.Resnick B, Shaughnessy M, Galik E, Scheve A, Fitten R, Morrison T, et al. Pilot testing of the PRAISEDD intervention among African American and low-income older adults. J Cardiovasc Nurs. 2009;24(5):352–61. doi: 10.1097/JCN.0b013e3181ac0301. [DOI] [PubMed] [Google Scholar]
- 95.Resnick B, Luisi D, Vogel A. Testing the Senior Exercise Self-efficacy Project (SESEP) for use with urban dwelling minority older adults. Public Health Nurs. 2008;25(3):221–34. doi: 10.1111/j.1525-1446.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- 96.Romero Z. Use of pedometers to promote improvement in selected physiological measurements in an older female Mexican American population. Edinburg: University of Texas-Pan American; 2004. [Google Scholar]
- 97.Santa-Clara H, Szymanski L, Ordille T, Fernhall B. Effects of exercise training on resting metabolic rate in postmenopausal African American and Caucasian women. Metabolism. 2006;55(10):1358–64. doi: 10.1016/j.metabol.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 98.Santa-Clara H, Szymanski L, Fernhall B. Effect of exercise training on blood pressure in postmenopausal Caucasian and African-American women. Am J Cardiol. 2003;91(8):1009–11. doi: 10.1016/s0002-9149(03)00128-0. [DOI] [PubMed] [Google Scholar]
- 99.Skinner JS, Jaskolski A, Jaskolska A, Krasnoff J, Gagnon J, Leon AS, et al. Age, sex, race, initial fitness, and response to training: the HERITAGE Family Study. J Appl Physiol. 2001;90(5):1770–6. doi: 10.1152/jappl.2001.90.5.1770. [DOI] [PubMed] [Google Scholar]
- 100.Speck BJ, Hines-Martin V, Stetson BA, Looney SW. An environmental intervention aimed at increasing physical activity levels in low-income women. J Cardiovasc Nurs. 2007;22(4):263–71. doi: 10.1097/01.JCN.0000278957.98124.8a. [DOI] [PubMed] [Google Scholar]
- 101.Staten L, Gregory-Mercado K, Ranger-Moore J, Will J, Giuliano A, Ford E, et al. Provider counseling, health education, and community health workers: the Arizona WISEWOMAN project. Journal of Women’s Health. 2004;13(5):547–56. doi: 10.1089/1540999041281133. [DOI] [PubMed] [Google Scholar]
- 102.Staten LK, Scheu LL, Bronson D, Pena V, Elenes J. Pasos Adelante: the effectiveness of a community-based chronic disease prevention program. Preventing Chronic Disease. 2005;2(1):A18. [PMC free article] [PubMed] [Google Scholar]
- 103.Stewart AL, Gillis D, Grossman M, Castrillo M, Pruitt L, McLellan B, et al. Diffusing a research-based physical activity promotion program for seniors into diverse communities: CHAMPS III. Preventing Chronic Disease. 2006;3(2):A51. [PMC free article] [PubMed] [Google Scholar]
- 104.Walcott-McQuigg JA, Chen S-P, Davis K, Stevenson E, Choi A, Wangsrikhun S. Weight loss and weight loss maintenance in African-American women. J Natl Med Assoc. 2002;94(8):686–94. [PMC free article] [PubMed] [Google Scholar]
- 105.Wilbur J, McDevitt JH, Wang E, Dancy BL, Miller AM, Briller J, et al. Outcomes of a home-based walking program for African-American women. Am J Health Promot. 2008;22(5):307–17. doi: 10.4278/ajhp.22.5.307. [DOI] [PubMed] [Google Scholar]
- 106.Gannon B, DiPietro L, Poehlman ET. Do African Americans have lower energy expenditure than Caucasians? International Journal of Obesity & Related Metabolic Disorders: Journal of the International Association for the Study of Obesity. 2000;24(1):4–13. doi: 10.1038/sj.ijo.0801115. [DOI] [PubMed] [Google Scholar]
- 107.Shaw KA, Gennat HC, O’Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database of Systematic Reviews. 2006;(4):Art. No.: CD003817. doi: 10.1002/14651858.CD003817.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Walker KZ, O’Dea K, Gomez M, Girgis S, Colagiuri R. Diet and exercise in the prevention of diabetes. Journal of Human Nutrition & Dietetics. 2010;23(4):344–52. doi: 10.1111/j.1365-277X.2010.01061.x. [DOI] [PubMed] [Google Scholar]
- 109.Lee IM, Djousse L, Sesso HD, Wang L, Buring JE. Physical activity and weight gain prevention. JAMA. 2010;303(12):1173–9. doi: 10.1001/jama.2010.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lollgen H, Bockenhoff A, Knapp G. Physical activity and all-cause mortality: an updated meta-analysis with different intensity categories. Int J Sports Med. 2009;30(3):213–24. doi: 10.1055/s-0028-1128150. [DOI] [PubMed] [Google Scholar]
- 111.Cooper H. Research Synthesis and Meta-Analysis. 4. Los Angeles: Sage; 2010. [Google Scholar]
- 112.Lipsey MW, Wilson DB. The way in which intervention studies have “personality” and why it is important to meta-analysis. Eval Health Prof. 2001;24(3):236–254. doi: 10.1177/016327870102400302. [DOI] [PubMed] [Google Scholar]
- 113.Kawachi I, Daniles N, Robinson D. Health disparities by race and class: why both matter. Health Aff (Millwood) 2005;24(2):343–352. doi: 10.1377/hlthaff.24.2.343. [DOI] [PubMed] [Google Scholar]
- 114.Yancey A, Whitt-Glover MC, Auyoung M. Physical Activity. In: Braithwaite RL, Taylor S, Treadwell H, editors. Health Issues in the Black Community. 3. San Francisco: John Wiley & Sons, Inc; 2009. pp. 461–487. [Google Scholar]
- 115.Montgomery K, Schubart K. Health Promotion in Culturally Diverse and Vulnerable Populations. Home Health Care Management & Practice. 2010;22(2):131–139. [Google Scholar]
- 116.Resnicow K, Jackson A, Blissett D, Wang T, McCarty F, Rahotep S, et al. Results of the healthy body healthy spirit trial. Health Psychol. 2005;24(4):339–48. doi: 10.1037/0278-6133.24.4.339. [DOI] [PubMed] [Google Scholar]
- 117.Kumanyika SK, Yancey AK. Physical activity and health equity: evolving the science. Am J Health Promot. 2009;23(6):S4–7. doi: 10.4278/ajhp.23.6.S4. [DOI] [PubMed] [Google Scholar]
- 118.DeHaven MJ, Hunter IB, Wilder L, Walton JW, Berry J. Health programs in faith-based organizations: are they effective? Am J Public Health. 2004;94(6):1030–6. doi: 10.2105/ajph.94.6.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Fitzgibbon ML, Stolley MR. Environmental changes may be needed for prevention of overweight in minority children. Pediatr Ann. 2004;33(1):45–9. doi: 10.3928/0090-4481-20040101-12. [DOI] [PubMed] [Google Scholar]
- 120.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–24. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 121.Sloane D, Nascimento L, Flynn G, Lewis L, Guinyard JJ, Galloway-Gilliam L, et al. Assessing resource environments to target prevention interventions in community chronic disease control. J Health Care Poor Underserved. 2006;17(2 Suppl):146–58. doi: 10.1353/hpu.2006.0094. [DOI] [PubMed] [Google Scholar]