Abstract
This study sought to replicate the results of our earlier study, which were published in this Journal (Willoughby et. al 2011), that used mother-reported items from the Achenbach System of Empirically Based Assessment to develop a screening measure of callous unemotional (CU) behaviors for use with preschool-aged children. We further sought to extend those results by exploring the predictive validity of the CU measure with aggression trajectories in early-/mid-childhood. The current study involved secondary data analysis of the NICHD Study of Early Childhood and Youth Development (NICHD-SECCYD) dataset. Factor analyses included N = 1176 children who participated in the age 3 year assessment of the NICHD-SECCYD. Predictive models included N = 1081 children for whom four of the six possible teacher ratings of aggressive behavior were available from annual assessments spanning 1st-6th grades. Consistent with prior work, a three-factor confirmatory factor model, which differentiated CU from oppositional defiant (ODD) and attention deficit/hyperactive-impulsive (ADHD) behaviors, provided the best fit to the data. Among children with disorganized attachment status, the combination of high levels of mother-rated ODD behaviors and CU behaviors, was predictive of stable elevated levels of teacher-rated aggression from 1st-6th grade (predicted probability = .38, compared with a base rate of .07). These results demonstrate that CU behaviors can be reliably measured by parent report in young children and are dissociable from more commonly assessed dimensions of disruptive behavior. Three-year-old children who exhibit elevated levels of ODD and CU behaviors, and who have disorganized attachments, are at increased risk for exhibiting elevated levels of aggression across middle childhood. Results are discussed from the perspective of early assessment and intervention.
Keywords: callous unemotional, oppositional defiance, ADHD, disorganized attachment, factor analysis, aggression
Measuring Callous Unemotional Behaviors in Early Childhood: Factor Structure and Predictive Validity
Callous Unemotional (CU) behaviors include diminished guilt following negative actions, low empathy and fear, poor recognition of fear or distress in others, reduced reactivity to challenging events, an over-focus on reward and insensitivity to punishment (Frick & White, 2008; Kotler & McMahon, 2005). There is growing evidence to support the use of CU diagnosis as way to differentiated among heterogeneous groups of youth with conduct problems (Frick & Moffitt, 2010; McMahon, Witkiewitz, Kotler, & CPRG, 2010; Moran et al., 2009; Rowe et al., 2010).
As interest in CU has grown, an important initial set of questions asked whether parents and teachers could reliably distinguish CU from other, more commonly assessed dimensions of disruptive behavior, including hyperactivity-impulsivity, inattention, oppositional defiance, and conduct problems. At least five studies have utilized confirmatory factor analytic methods to address this question. In the context of a large community sample of children age 4-9 years, Dadds and colleagues (2005) reported that parents distinguished CU behaviors from hyperactivity, conduct, emotional and peer problems. In their study, CU and prosocial behaviors loaded on the same factor, indicating that CU was conceptually more similar to the absence of prosocial behaviors than the presence of conduct problems. Using the Pittsburgh Youth Study (PYS), which included three large cohorts of typically developing boys over-sampled for behavior problems, Pardini and colleagues (2006) reported that CU could be distinguished from hyperactivity, inattention, and conduct problems. This pattern of findings was replicated across all three cohorts (1st, 4th, and 7th graders). Loeber, Pardini and colleagues (2009) later replicated the PYS results in a large sample of girls (i.e., the Pittsburgh Girls Study). Parents (but not teachers) distinguished CU from other dimensions of disruptive behavior across four annual waves of data collection. Finally, two studies—which both independently made use of subsets of the items from the preschool version of the Achenbach System of Empirically Based Assessment (ASEBA) to build a screening measure of CU behaviors—reported that parents could distinguish CU behaviors from other dimensions of disruptive behavior in children as young as three years old (Hyde et al., 2013; Willoughby, Waschbusch, Moore, & Propper, 2011). A key difference between these studies was that whereas Hyde and colleagues drew items from multiple instruments (the ASEBA being only one of them) and focused on deceitful CU behaviors (i.e., ‘cruelty to animals’ and ‘lying’ were indicators of their construct), we drew items exclusively from the ASEBA and focused exclusively on CU items. The first goal of the current study was to provide an independent test of the factor structure of the ASEBA items using the same approach as in our earlier study but using a much larger sample. In light of the previous factor analytic results, we hypothesized that parents would distinguish CU from oppositional defiant and hyperactive-impulsive/inattentive behaviors.
Although the aforementioned studies provided a strong empirical basis for considering CU as distinct dimension of behavior, they also indicated that CU was moderately to strongly correlated (rs = .45 - .85) with behaviors characteristic of attention deficit/hyperactivity (ADHD), and especially oppositional defiant (ODD) and conduct (CD) disorders. Hence, although CU was distinct from other dimensions of disruptive behavior, it was not assumed to be unrelated to them. Moreover, irrespective of the assessment instrument, the internal consistency of CU items tended to be moderate (αs ≈ .60; range = .46 - .89). Consistent with psychometric theory, studies that used larger numbers of items to measure CU reported better estimates of internal consistency. Another goal of this study was to establish how highly correlated CU behaviors were with other dimensions of disruptive behavior, as well as to establish the internal consistency of an ASEBA-based measure of CU using a large sample.
There is evidence that CU behaviors, both alone (Frick, Cornell, Barry, Bodin, & Dane, 2003; Moran et al., 2009) and in combination with conduct problems, are associated with more severe and varied forms of antisocial behavior (e.g., Enebrink, Andershed, & Langstrom, 2005; Rowe et al., 2010). Although we are unaware of any studies that have established this in samples consisting entirely of young children, there are good reasons to do so. Disruptive behaviors are multiply determined in early childhood and, for some subset of children, likely represent transient difficulties associated with emerging self-regulatory and language abilities (Arnold, Kupersmidt, Voegler-Lee, & Marshall, 2012; Cohen & Mendez, 2009; Mathiesen & Sanson, 1999; Rose, Rose, & Feldman, 1989; Shaw, Lacourse, & Nagin, 2005). An open question is whether the co-occurrence of ODD (a developmentally appropriate indicator of conduct problems for young children) and CU behaviors in early childhood might identify that subset of children whose disruptive behaviors are less transient and more likely to persist into middle childhood. As such, the second major goal of this study was to test whether CU behaviors moderate the effects of ODD behaviors at age 3 years in the prediction of stable and elevated aggression in middle childhood. Consistent with evidence from older children, we hypothesized that CU behaviors would moderate the effects of early ODD on later aggression (i.e., the effects of ODD would be conditional on levels of CU). Given the high degree of overlap between ADHD with both ODD and CU, as well as evidence that the combination of ADHD and ODD are associated with negative outcomes (Mathias et al., 2007; Waschbusch, 2002), we also considered ADHD as another moderator. The simultaneous consideration of ADHD and CU as moderators of ODD provided a stronger test of the role of CU than would have been the case had ADHD only been considered a covariate (main effect).
In addition to considering the potential multiplicative associations of early ODD, CU, and ADHD as predictors of later aggressive behavior, we also examined the role of disorganized parent-child attachment quality as a relational risk factor that may have direct or moderating effects influence on later aggressive behaviors. Various aspects of parenting, such as lower levels of sensitive parenting and higher levels of physical punishment, predict higher mean levels of antisocial behaviors over time (Hawes, Dadds, Frost, & Hasking, 2011; Pardini, Lochman, & Powell, 2007). One of the ways in which non-optimal parenting behaviors may influence subsequent child aggression is through the development of disorganized attachment relationships between the child and parent (Fowles & Kochanska, 2000). Children with disorganized attachments likely experience the most extreme (Lyons-Ruth, Bronfman, & Parsons, 1999) and persistent (Mills-Koonce, Gariepy, Sutton, & Cox, 2008) levels of maladaptive parenting behaviors as compared to both children with secure attachments and children with organized but insecure attachments (insecure-avoidant and insecure-ambivalent). They also exhibit higher levels of hostile attribution biases (McElwain, Booth-LaForce, Lansford, Wu, & Dyer, 2008), low empathy and disregard for the mental states of others (Shirtcliff et al., 2009), and appear most vulnerable to subsequent behavior problems (Bureau, Easlerbrooks, & Lyons-Ruth, 2009; Futh, O'Connor, Matias, Green, & Scott, 2008; Green & Goldwyn, 2002; Pasalich, Dadds, Hawes, & Brennan, 2012; Pauli-Pott, Haverkock, Pott, & Beckmann, 2007), including antisocial behaviors (Fearon, Bakermans-Kranenburg, van IJzendoorn, Lapsley, & Roisman, 2010; Green, Stanley, & Peters, 2007). In fact, children with the disorganized attachments, as compared to all others, have consistently evidenced higher levels of aggression in middle childhood, above and beyond other familial factors (Lyons-Ruth, 1996). As such, the third goal of this study was to test whether the prediction of aggressive behavior in middle childhood from ADHD, ODD, and CU—considered alone or in combination—was moderated by attachment disorganization. We hypothesized that disorganization would amplify the effects of early disruptive behaviors on later aggression.
In sum, the study involved secondary data analysis of a large prospective longitudinal sample in order to test whether parents could reliably distinguish CU from other commonly assessed dimensions of disruptive behavior in their 3 year-old children. In addition, this study tested whether ODD behaviors were differentially predictive of persistently elevated levels of aggressive behaviors across middle childhood as a function of CU and/or ADHD behaviors, as well as attachment disorganization. We hypothesized that parents would be able to distinguish CU from ODD and ADHD behaviors and that the predictive power of ODD to later stable aggression would be strong for children who also exhibited high levels of CU and ADHD behaviors and who exhibited disorganized attachments with their primary caregivers.
Methods
Participants
The NICHD Study of Early Child Care and Youth Development (NICHD SECCYD) was a 16-year long prospective longitudinal study that was designed to answer questions about the relationships between child care experiences and children's developmental outcomes (see http://secc.rti.org). A total of N = 1,364 families were recruited shortly after the birth of their first child. In the current study, the 1,176 families who participated in the age 3-year lab visit contributed to factor analyses of the ASEBA, while the 1,081 children who had four or more teacher-ratings of aggressive behavior from annual assessments spanning 1st-6th grade contributed to predictive models. We adopted the same inclusionary criteria and analytic approach as the NICHD SECCYD investigators for purposes of identifying children with stable elevated levels of aggressive behavior in middle childhood (NICHD Early Child Care Network 2004), which included the same N = 1081 children. The prediction of elevated aggression, provided a strong test of our theoretical questions and helped to maintain continuity with previous publications involving this sample (Campbell, Spieker, Burchinal, & Poe, 2006; Campbell et al., 2010).
Participating children (N = 1,081) did not differ from non-participating children (N = 283) with respect to mother-rated ADHD (t[1174] = −0.5, p = .60; participant M = 5.4 vs. non-participant M = 5.2), ODD (t[1174] = 0.2, p = .82; M = 4.1 vs. M = 4.2), or CU (t[1174] = 1.4, p = .18; M = 1.8 vs. 2.0) behaviors, or rates of attachment disorganization (χ2[1] = 0.02, p = .88; 14% vs. 14%), all of which are defined below and were the focal predictors. In contrast, participating children were less likely to be white than non-participants (χ2[1] = 10.7, p = .001; 79% vs. 87% Caucasian) and came from moderately more advantaged homes at the time of their birth, as indicated by higher levels of maternal education (t[1361] = −2.6, p = .009; M = 14.3 vs. 13.9 years of education) and household income (t[1271] = −4.2, p < .0001; income/needs M = 3.0 vs. 2.3). These variables were included as covariates in predictive models.
Measures
Child oppositional defiant, callous/unemotional, and attention deficit/hyperactive behaviors
Mothers completed the Achenbach System of Empirically Based Assessment-Preschool Forms (ASEBA; Achenbach & Rescorla, 2000) at the age 3-year visit. The ASEBA is a 99-item assessment of children's behavioral/emotional problems that have been present within the last two months. In an effort to replicate our previous results (Willoughby et al., 2011), the current study used 17 items to test the dimensionality of disruptive behavior at age 3. Specifically, six items each were drawn from the DSM-IV referenced ADHD (i.e., cannot concentrate, cannot sit still, cannot stand waiting, immediate demands, gets into everything, and shifts activities quickly), and ODD (i.e., defiant, disobedient, angry moods stubborn/sullen, temper tantrums, uncooperative) scales, as were five additional items that represented CU (i.e., does not seem to feel guilty after misbehaving, punishment does not change behavior, seems unresponsive to affection, shows little affection toward people, shows too little fear of getting hurt). We would not expect that these traits would be uncorrelated; however, the clusters of symptoms represented by each trait are expected to be conceptually and empirically distinct.
Attachment disorganization
A modified Strange Situation Paradigm, developed by the MacArthur Working Group on Attachment (Cassidy, Marvin, & Childhood, 1992), was used to assess mother-child attachment at the 3-year visit. The procedure is designed to be moderately stressful to the child in a similar, but more age-appropriate, fashion as the Ainsworth Strange Situation Paradigm (Ainsworth, Blehar, Waters, & Wall, 1978; Network, 2001). The coding system for the modified SSP was comparable to that of the original SSP, with categorical classification of secure, insecure-avoidant, insecure-ambivalent, and insecure-disorganized. Inter-coder agreement was 76% for the 4-way classification scheme with disagreements resulting in the assignment of a consensus classification. Based on previous research, the study hypotheses focused on the associations between attachment disorganization and later child aggression. As such, we compared children with disorganized versus non-disorganized attachments (which collapsed secure, avoidant, and ambivalent classifications) in order to create the most conceptually and statistically parsimonious models.
Teacher reports of aggressive behavior
At each assessment from 1st-6th grade, teachers completed the Teacher Report Form of the Achenbach Child Behavior Checklist (TRF; Achenbach, 1991). The TRF includes 113 items that describe typical, but potentially problematic child behaviors. Teachers rated how descriptive each item was of the child's usual behavior in school over the last 2 months (0 = not true, 1 = somewhat or sometimes true, 2 = very/often true). As elaborated in the Analytic Strategy, in order to replicate the results of Campbell and colleagues (2010), six items that reflected overt physical aggression to people and objects (i.e., destroys own things, destroys others’ things, gets in many fights, threatens others, physically attacks people, and cruelty, bullying, or meanness to others) were selected to measure physical aggression in middle childhood. Raw scores for these items were summed at each age and could range from 0 to 12. These sum scales showed adequate internal consistency across age with coefficient alphas ranging from 0.81 to 0.86.
Demographic characteristics
A number of socioeconomic status (SES) indices were included as statistical controls in the prediction models aggression trajectories, including child race/ethnicity and gender, as well as maternal education and household income. These measures were drawn from the first home visit, when target children were 1 month old, to ensure that they did not contribute to missing data.
Data Analysis
The first research question tested whether caregivers (overwhelming biological mothers in this sample) could reliably differentiate CU from ODD and ADHD behaviors. This question was addressed by testing which of the five confirmatory factor analytic models that were used in our previous study best fit the observed data in the NICHD SECCYD sample. The WLSMV estimator was used to accommodate the ordinal nature of ASEBA items; model fit was evaluated using the likelihood ratio chi square test, as well as Comparative Fit Index (CFI) and the root mean squared error of approximation (RMSEA) fit indices (CFI >= .95 and RMSEA < .05 were indicative of good fit). Nested chi square tests using the DIFTEST option in Mplus version 6.0 (Muthén & Muthén, 1998-2013) were used for model comparisons.
Campbell and colleagues (2010) used semi-parametric finite mixture (SPFM) models (Nagin, 1999) to separately identify boys and girls, in the NICHD SECCYD dataset, who exhibited stable and elevated levels of teacher-rated aggressive behavior from 1st-6th grades. As a prelude to our second research question, we adopted their approach (i.e., we estimated SPFMs separately by gender using PROC TRAJ in SAS version 9.2, assumed that behavioral outcomes followed a Poisson distribution, and adopted their model parameterization) and classified children into trajectory groups based on their posterior probabilities (i.e., children were classified into the stable high aggressive trajectory if their posterior probability was larger for that relative to any other class; posterior probabilities refer to the probability that one's observed data were generated by a given trajectory class). For purposes of the current study, we distinguished children who were classified into the stable high aggressive trajectory group (i.e., 78/1081; N = 52 boys and N = 26 girls) from all of the remaining children. The second research question tested whether (and how) ODD, CU, and ADHD behaviors, as well as disorganized attachment status, were uniquely and/or multiplicatively predictive of membership in the stable high aggression group. This was addressed by estimating a series of logistic regression models, using PROC LOGISTIC in SAS version 9.2, with stable and elevated aggression as the outcome. The initial model included four-way interactions between ODD, CU, ADHD, and attachment disorganization. The final model retained only those higher-order interactions that were statistically significant.
Results
Consistent with the normative nature of the sample, on average, participating mothers completed 2 years of post-secondary education and resided in homes that were three times the federal poverty level given household size. Children were predominantly white and were reported to exhibit low to modest levels of disruptive behavior. As established in previous work in this sample (Campbell et al., 2010), 7% of children were designated as having stable high levels of teacher-reported aggression. As summarized in Table 1, although 14% of parent-child dyads were characterized as having a disorganized attachment, there was no evidence that attachment disorganization was associated with demographic or behavioral differences in mothers or children.
Table 1.
Descriptive Statistics
| Total Sample (N = 1081) | Organized Attachment (N = 932) | Disorganized Attachment (N = 149) | |
|---|---|---|---|
| M(SD) | M(SD) | M(SD) | |
| Mother education (years) | 14.3 (2.5) | 14.4 (2.5) | 14.1 (2.8) |
| Income-to-needs | 3.0 (2.8) | 3.0 (2.7) | 3.1 (3.2) |
| ADHD | 5.4 (2.5) | 5.4 (2.5) | 5.5 (2.6) |
| CU | 1.8 (1.6) | 1.8 (1.6) | 1.9 (1.5) |
| ODD | 4.1 (2.4) | 4.1 (2.4) | 4.0 (2.3) |
| % | % | % | |
| Child race (White) | 78 | 80 | 74 |
| Child race (Black) | 15 | 13 | 22 |
| Child race (Other) | 7 | 7 | 4 |
| Child gender (Male) | 53 | 54 | 50 |
| Attachment (Disorganized) | 14 | 0 | 100 |
| Stable Aggression | 7 | 7 | 7 |
Note: M = mean, SD = standard deviation
Bivariate correlations between all of the study predictors (including covariates), the dichotomous study outcome, and the continuous indicators of aggression that were used to define the study outcome are summarized in Table 2. When considered in isolation, the predictors were weakly related to the dichotomous outcome and time-specific measures of teacher-rated aggression from 1st-6th grades (rs <= .10). This was likely due to the use of different informants and the intervening span of time (age 3 behaviors were rated by parents, while grades 1-6 behaviors were rated by teachers—a nearly 10 year span). In contrast, parent-rated behaviors were positively correlated at age 3 (rs = .53 - .59) and teacher-rated aggression was positively correlated across grades 1-6 (rs = .33 - .49). Although the main effects of parent-rated behaviors at age 3 and teacher-rated behaviors from 1st-6th grades were weak, this did not inform the broader question of interactions between relational and behavioral predictors at age 3 in the prediction of 1st-6th grade outcomes.
Table 2.
Bivariate correlations between predictors and outcomes.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Male | -- | ||||||||||||||
| 2 Black | .01 | -- | |||||||||||||
| 3 Other Race | −.04 | −.11 | -- | ||||||||||||
| 4 Mom Education | −.03 | −.24 | −.05 | -- | |||||||||||
| 5 Income/Needs | −.02 | −.25 | .02 | .42 | -- | ||||||||||
| 6 Disorganized | −.13 | .12 | −.08 | −.06 | .02 | -- | |||||||||
| 7 ADHD | −.03 | −.01 | −.03 | −.01 | −.02 | .03 | -- | ||||||||
| 8 CU | −.09 | .02 | −.02 | −.03 | −.02 | .03 | .54* | -- | |||||||
| 9 ODD | −.02 | .03 | −.03 | −.01 | .00 | −.02 | .59* | .53* | -- | ||||||
| 10 High/Stable Agg | .14 | .04 | .10* | −.06 | .02 | −.02 | −.04 | −.09 | −.10 | -- | |||||
| 11 Teacher Agg G1 | .02 | .02 | .01 | −.01 | .01 | −.06 | −.02 | −.04 | −.04 | .45* | -- | ||||
| 12 Teacher Agg G2 | −.02 | −.02 | .05 | −.03 | .02 | .02 | −.02 | −.06 | −.07* | .58* | .43* | -- | |||
| 13 Teacher Agg G3 | −.01 | −.01 | .08 | −.01 | .02 | .04 | .02 | −.01 | −.03 | .65* | .33* | .48* | -- | ||
| 14 Teacher Agg G4 | −.02 | −.02 | .06 | −.05 | −.01 | .08 | .00 | −.02 | −.05 | .59* | .41* | .47* | .49* | -- | |
| 15 Teacher Agg G5 | −.03 | −.03 | .03 | .02 | .00 | −.02 | −.02 | −.08 | −.06 | .51* | .34* | .40* | .43* | .49* | -- |
| 16 Teacher Agg G6 | −.02 | −.02 | .05 | −.02 | −.01 | .00 | −.03 | −.07 | .03 | .56* | .42* | .35* | .39* | .35* | .43* |
Note. Total N = 1081; Correlations computed using the WLSMV estimator; Agg = Aggression; G1 – G6 = first through sixth grades
p < .05.
Dimensionality of ASEBA Items
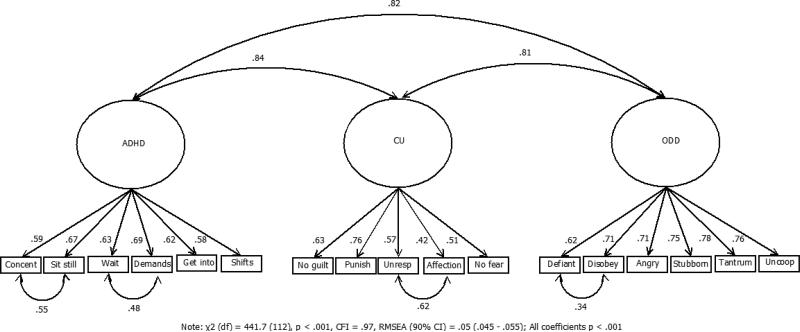
Five competing CFA models were fit to the 17 ASEBA items. As summarized in Table 3, although the 3-factor model provided a statistically better fit to the data than did any of the 1- or 2-factor models, none of the five initial models met conventional standard for good model fit. After reviewing the modification indices from the 3-factor model, we identified four pairs of items—i.e., (1) item 5/can't concentrate, can't pay attention for long & item 6/can't sit still, restless, or hyperactive, (2) item 8/can't stand waiting; wants everything now & item 16/demands must be met immediately, (3) item 15/defiant & item 20/disobedient, and (4) item 67/seems unresponsive to affection & item 70/shows little affection toward people— that were conceptually overlapping and for which the inclusion of residual correlations would improve model fit. A sixth CFA model that introduced these four residual covariances fit the data well, χ2 (112) = 442, p < .001, CFI = .97, RMSEA = .05 (90% confidence interval [90% CI]: .045 - .055). The variances for all three latent variables were statistically significant, indicating substantial individual differences in CU, ODD, and ADHD behaviors. Standardized factor loadings and latent/residual correlations are summarized in Figure 1. The three latent variables were positively correlated, φADHD, CU = .84, φADHD, ODD = .82, and φODD, CU = .81, all ps < .001. The correlations among the manifest scores for CU, ODD, and ADHD (obtained by taking the mean of items for each latent variable) were comparatively much smaller, rs = .53 - .59 (see Table 2), due to attenuation from measurement error.
Table 3.
Synopsis of Confirmatory Factor Models of ASEBA Items
| Model | Description | χ2 (df) | prob | CFI | RMSEA (90% CI) |
|---|---|---|---|---|---|
| 1 | 1 factor | 1386.26 (119) | <.001 | .88 | .095 (.091 - .100) |
| 2 | 2 factor (CU vs. other) | 1289.51 (118) | <.001 | .89 | .092 (.087 - .096) |
| 3 | 2 factor (ODD vs. other) | 1074.99 (118) | <.001 | .91 | .083 (.079 - .088) |
| 4 | 2 factor (ADHD vs. other) | 1027.89 (118) | <.001 | .91 | .081 (.076 - .086) |
| 5 | 3 factor (CU, ODD, ADHD) | 911.42 (116) | <.001 | .92 | .076 (.072 - .081) |
| Model 5 vs. Model 1 | 280.60 (3) | <.001 | -- | -- | |
| Model 5 vs. Model 2 | 204.02 (2) | <.001 | -- | -- | |
| Model 5 vs. Model 3 | 106.50 (2) | <.001 | -- | -- | |
| Model 5 vs. Model 4 | 79.96 (2) | <.001 | -- | -- | |
| 6 | 3 factor with 4 correlated residuals | 441.65 (112) | <.001 | .97 | .050 (.045 - .055) |
Note: N = 1176; chi square difference tests computed using the DIFTEST option in Mplus; prob = probability; CFI = Comparative Fit Index; RMSEA = Root mean squared error of approximation; CI = confidence interval
Figure 1.
Standardized Coefficient from Final Confirmatory Factor Analysis
Maximum reliability is an index of how well a given set of items measure their latent construct (Raykov, 2004). Maximum reliability was computed as .80, .83, and .83 for ADHD, CU, and ODD latent variables, respectively. Chronbach's alpha, a commonly reported index of internal consistency, was computed as .75, .55, and .79 for ADHD, CU, and ODD manifest variables, respectively. These differences in reliability estimates are elaborated in the Discussion.
Prediction of Stable High Aggression
An initial logistic regression model only included basic demographic covariates. Although the overall model provided a statistically significant improvement over the null model, it did a relatively poor job of predicting membership in a stable high aggressive trajectory (max rescaled R2 = .03; see Table 4). Minority (non-white, non-African American; Odds ratio [OR] = 2.4, p = .02) and male (OR = 2.0, p = .01) children were at increased risk for stable elevated aggression in middle childhood.
Table 4.
Synopsis of Logistic Regression Models
| Covariates Only | Full Model | Final Trimmed Model | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Parameter | Beta | SE | p | Beta | SE | p | Beta | SE | p |
| Intercept | −3.02 | 0.77 | <.0001 | −2.93 | 1.00 | .003 | −3.34 | 0.94 | .0003 |
| Black | 0.35 | 0.34 | .30 | 0.44 | 0.35 | .21 | 0.45 | 0.35 | .19 |
| Other Race | 0.86 | 0.37 | .02 | 0.92 | 0.38 | .02 | 0.89 | 0.38 | .02 |
| Male | 0.67 | 0.25 | .01 | 0.74 | 0.26 | .004 | 0.72 | 0.26 | .005 |
| Mother Education | −0.02 | 0.05 | .72 | −0.02 | 0.05 | .74 | −0.02 | 0.05 | .78 |
| Income-to-Needs | 0.06 | 0.04 | .12 | 0.06 | 0.04 | .18 | 0.06 | 0.04 | .19 |
| Disorganized Attachment | −3.50 | 2.81 | .21 | −1.53 | 1.72 | .37 | |||
| ADHD Sx | −0.10 | 0.16 | .54 | 0.03 | 0.12 | .78 | |||
| CU Sx | −0.13 | 0.52 | .80 | 0.39 | 0.25 | .12 | |||
| ODD Sx | 0.02 | 0.20 | .90 | 0.06 | 0.15 | .68 | |||
| ADHD*ODD | 0.11 | 0.09 | .22 | 0.01 | 0.03 | .64 | |||
| CU*ODD | 0.03 | 0.04 | .42 | −0.14 | 0.05 | .01 | |||
| ADHD*CU | −0.07 | 0.13 | .57 | ||||||
| ADHD*CU*ODD | −0.02 | 0.02 | .41 | ||||||
| Disorganized*ADHD | 0.87 | 0.56 | .12 | 0.43 | 0.39 | .27 | |||
| Disorganized*CU | 1.40 | 1.76 | .43 | −0.59 | 0.64 | .36 | |||
| Disorganized*ODD | 0.80 | 0.69 | .25 | 0.46 | 0.41 | .26 | |||
| Disorganized*ADHD*ODD | −0.36 | 0.29 | .21 | −0.18 | 0.09 | .04 | |||
| Disorganized*CU*ODD | −0.26 | 0.14 | .07 | .30 | 0.15 | .05 | |||
| Disorganized*ADHD*CU | −0.03 | 0.35 | .93 | ||||||
| Disorganized*ADHD*CU*ODD | 0.06 | 0.05 | .26 | ||||||
| −2LL | 546.3 | 519.8 | 522.4 | ||||||
| Max Rescaled R2 | .03 | .09 | .09 | ||||||
| Likelihood Ratio χ2 (df) | 14.1 (5) | .02 | 40.5(20) | .004 | 37.9 (16) | .002 | |||
Note: N = 1081
p < .05
** p < .01; SE = standard error; p = probability; LL = log likelihood; Sx = symptom
The second model added ODD, CU, ADHD, and disorganization status (including all possible interactions) as predictors. The second model provided an improved fit relative to the first model, χ2 (df) = 26.5 (15), p = .03 and improved predictive power of the model (max rescaled R2 = .09; see Table 4). However, a number of interaction terms (including the 4-way interaction of ODD, CU, ADHD, disorganization) were not statistically significant. A final model was obtained by eliminating non-significant interaction terms in succession. This third model did not result in a statistically significant decrement in fit relative to the second (full) model, χ2 (df) = 2.6 (5), p = .76, indicating that the set of interaction terms that were removed did not jointly predict the outcome (see Table 4). The final model included two statistically significant three-way interaction terms.
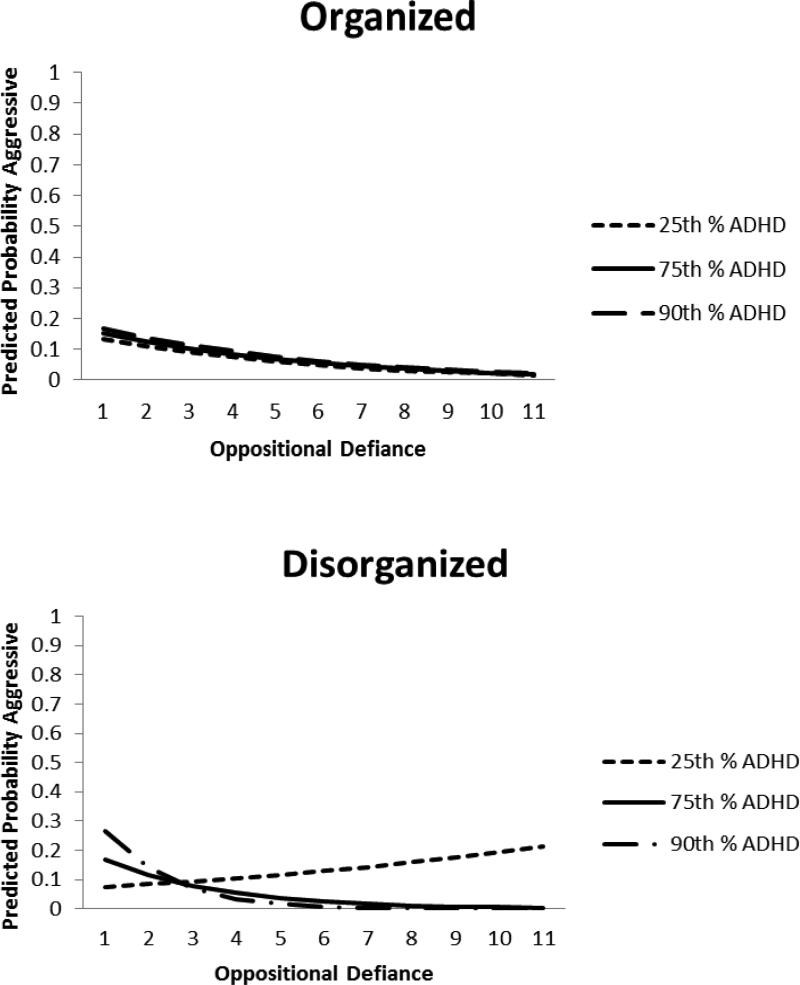
The disorganization × ADHD × ODD term was statistically significant (p = .04). As depicted in Figure 2, children with organized attachments at age 3 were at low risk for stable high aggression in middle childhood, irrespective of their levels of ODD or ADHD. Among children with disorganized attachments, (1) low levels of ODD and clinically high levels (90th percentile) of ADHD and (2) high levels of ODD and low levels (25th percentile) of ADHD were both associated with an increased risk for stable aggression in middle childhood.
Figure 2.
Plots to inform the attachment disorganization × ODD × ADHD interaction
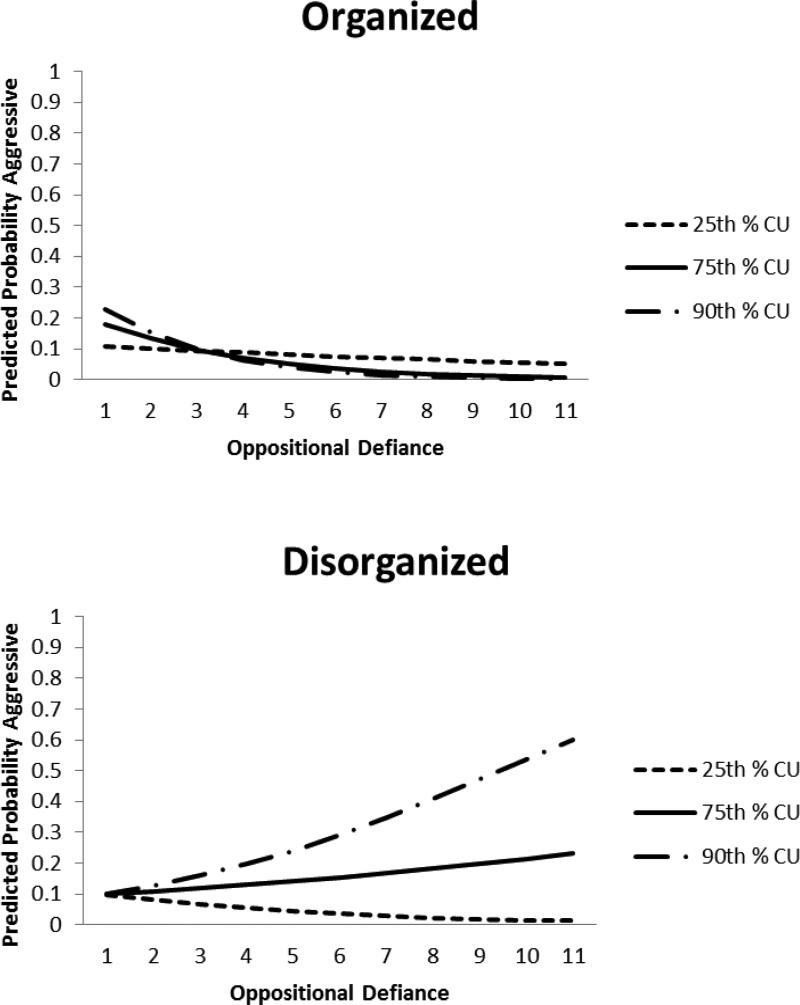
The disorganization × ODD × CU interaction term was also statistically significant (p = .05). As depicted in Figure 3, children with organized attachments were all at low risk for stable high aggression in middle childhood, irrespective of their levels of ODD or CU. In contrast, consistnet with our hypotheses, among children with disorganized attachments, higher levels of ODD at age 3 were associated with a greater risk for stable high aggression when they were accompanied by elevated levels of CU.
Figure 3.
Plots to inform the attachment disorganization × ODD × CU interaction
The presence of two, three-way interactions indicated a complex set of associations between age 3 predictors and risk for stable and elevated aggression in middle childhood. In order to better explicate these associations, predicted probabilities of membership in the stable high aggressive trajectory were computed as a function of attachment status (disorganized, not) and normative (defined as the observed 50th percentile score) versus clinical (defined as the observed 90th percentile score) scores on ADHD, ODD, and CU (see Table 5). To be clear, the predicted probabilities in Table 5, which were based on all N=1081 participants, were generated using both (1) the parameter estimates from the final trimmed model in Table 4 and (2) ADHD, ODD, and CU scores that corresponded to the 50th and 90th percentile scores in this sample. Table 5 does not provide any new results. Rather, following Long and Freese (2003), it provided an alternative representation of the higher-order interaction terms to clarify clinical implications. The results in Table 5 illustrate that 3-year-old children with disorganized attachment, in conjunction with clinically elevated levels of both ODD and CU were at an appreciably higher risk for stable elevated aggression in middle childhood than any other group (predicted probability = .38). The next most risky profile included disorganized attachment and clinically elevated CU (but not ODD or ADHD) behaviors (predicted probability = .20).
Table 5.
Predicted Probability of Membership in Stable High Aggression in Middle Childhood as a Function of Normative versus Clinically Elevated Levels of ODD, ADHD, CU, and Attachment Disorganization at Age 3 Years
| Attachment | ODD | ADHD | CU | Predicted Probability |
|---|---|---|---|---|
| Organized | Normative | Normative | Normative | .09 |
| Organized | Normative | Normative | Clinical | .06 |
| Organized | Normative | Clinical | Normative | .11 |
| Organized | Normative | Clinical | Clinical | .08 |
| Organized | Clinical | Normative | Normative | .05 |
| Organized | Clinical | Normative | Clinical | .02 |
| Organized | Clinical | Clinical | Normative | .08 |
| Organized | Clinical | Clinical | Clinical | .03 |
| Disorganized | Normative | Normative | Normative | .09 |
| Disorganized | Normative | Normative | Clinical | .20 |
| Disorganized | Normative | Clinical | Normative | .04 |
| Disorganized | Normative | Clinical | Clinical | .09 |
| Disorganized | Clinical | Normative | Normative | .09 |
| Disorganized | Clinical | Normative | Clinical | .38 |
| Disorganized | Clinical | Clinical | Normative | .01 |
| Disorganized | Clinical | Clinical | Clinical | .03 |
Note: “Normative” and “Clinical” refer to the observed 50th and 90th percentile scores, respectively.
Discussion
A central challenge of developing life course models of antisocial behavior is distinguishing for which children elevated levels of disruptive behaviors in early childhood represent transient problems associated emerging regulatory and language competence from those for who behaviors will persist across time. The overarching objectives of this study were to test whether parents could distinguish CU behaviors from more commonly assessed dimensions of disruptive behavior and to test whether and how multiple dimensions of disruptive behavior may interact with each other and with disorganized attachment to increase the risk for stable elevated levels of aggression across middle childhood. A three-factor model that distinguished ODD, ADHD, and CU behaviors provided the best fit to caregiver ratings of young children's disruptive behaviors. This is consistent with studies involving older children that have demonstrated that parents can differentiate CU from more commonly assessed dimensions of disruptive behavior and extends that result to a large sample of preschool-aged children. Regression models indicated that specific configurations of behavioral and relational risk (i.e., ADHD × ODD × disorganized attachment; CU × ODD × disorganized attachment) at age 3 years were significantly predictive of stable elevated aggression from 1st – 6th grades.
Although the factor analytic results clearly indicated that mothers were able to distinguish CU from ADHD and ODD behaviors, the discrepancy between estimates of maximal reliability and internal consistency for CU items was noteworthy. Whereas the estimates of maximal reliability indicated comparable measurement quality for CU, ODD, and ADHD items (i.e., all >= .80), the estimates of internal consistency appeared to indicate poorer quality measurement for CU (.55) compared to ODD (.79) and ADHD (.75) items. That is, even though our estimate of internal consistency was similar to that reported in previous studies, the relative discrepancy of CU to ODD and ADHD may raise questions about the utility of a screening measure based on these items. However, it is important to recall that whereas Chronbach's alpha assumes essential tau equivalence of items, maximal reliability does not (Graham, 2006; Raykov, 1997). Tau equivalence implies that all of the items of a screening instrument are equally strong indicators of the underlying construct. An inspection of the standardized factor loadings indicates that this assumption is less tenable for the CU relative to ODD and ADHD items (see Figure 1). As such, we privileged the maximal reliability estimates and concluded that the CU items are equally good for purposes of screening as are the more commonly used ODD and ADHD items.
The finding that disorganized attachment status augmented the likelihood of persistent aggressive behaviors among children with high levels of early-identified ODD and CU is consistent with attachment theory (Kochanska & Kim, 2012) and developmental psychopathology (Burnette & Cicchetti, 2012) models of antisocial behavior. Previous studies have found that only a subset of children with disorganized attachment exhibit later externalizing problems (Moss, Cyr, Dubois-Cotois, 2004), suggesting that attachment disorganization may be better conceptualized as a source of vulnerability in a diathesis-stress model instead of a direct causal factor in a main effects model (Kobac, Cassidy, Lyons-Ruth, & Zi, 2006). When considering disorganized attachment as a moderating factor, there are at least two possible mechanisms through which attachment disorganization may increase a child's risk for later aggressive behavior. First, attachment disorganization is associated with dysregulated biobehavioral responses to stress in both the hypothalamic-pituitary-adrenal (HPA) axis and the autonomic nervous system (Bernard & Dozier, 2010; Hertsgaard, Gunnar, Erickson, & Nachmias, 1995; Spangler & Grossmann, 1993). These patterns of heightened reactivity and poor regulation have been associated with concurrent and future levels of externalizing behaviors, suggesting that attachment disorganization may be a marker of heightened biobehavioral risk for later disorder (Obradović & Boyce, 2012) or biological sensitivity to negative environmental influences (Ellis, Boyce, Belsky, Bakermans-Kranenburg, & van Ijzendoorn, 2011). Second, a disorganized attachment relationship between the child and caregiver may undermine the ability of the caregiver to model and socialize prosocial behaviors or effectively discipline antisocial behaviors (Kochanska & Kim, 2012). For example, disorganized parent-child dyads often exhibit both frightening, frightened, or otherwise typical behaviors on the part of caregivers (Lyons-Ruth et al., 1999) and controlling or rejecting behaviors on the part of the child (Moss, Cyr, & Dubois-Comtois, 2004), the combination of which likely reduces caregiver ability (or willingness) to effectively socialize the child. Such dynamics of increasingly coercive patterns of interaction likely provide fertile ground for early conduct problems and callous-unemotional traits to manifest into both elevated and persistent levels of aggression (Patterson, DeBaryshe, & Ramsey, 1989). Thus, it is possible that attachment disorganization is both a marker of biobehavioral and relational risk for children, and may augment the associations between early ODD and CU on subsequent aggressive behaviors (Pasalich et al., 2012).
In contrast to the expected pattern of results involving attachment disorganization, ODD, and CU, the disorganized × ADHD × ODD effects were less interpretable. Although disorganized attachment status again augmented the likelihood of persistent aggression in middle childhood, the increase risk was for children with high levels of ADHD (but low ODD) or high levels of ODD (but low ADHD). These findings contradicts evidence implicating high levels of ADHD and ODD as a risk for negative long term outcomes (Jensen, Martin, & Cantwell, 1997; Waschbusch, 2002), though previous studies have not considered the combined risk of ADHD and ODD in the presence of attachment disorganization nor have they focused on children this young. We speculate that the increased risk for aggression in middle childhood that resulted from disorganized attachment, high ODD and low ADHD might reflect children's use of oppositional and aggressive behaviors in order to control their environments. This would represent an adaptive strategy for children who are confronted with unpredictable environments. Moreover, the increased risk for aggression in middle childhood that resulted from disorganized attachment, low ODD and high ADHD might reflect children who have exceptionally high levels of impulsivity. High levels of preschool impulsivity in combination with poor caregiver-child relationships are established risk factor for childhood and adolescent aggression (e.g., Olson, Bates, Sandy, & Lanthier, 2000).
Although a variety of items have been used to index CU behaviors in previous studies, the Antisocial Process Screening Device (APSD; Munoz & Frick, 2007) and more recently the Inventory of Callous Unemotional traits (ICU; Kimonis et al., 2008) have been among those mostly widely used. The ASEBA items differ from those in the APSD and ICU in two important ways. First, the APSD and the ICU include items that index prosocial (e.g., feels bad or guilty when s/he has done something wrong) and callous (e.g., the feelings of others are unimportant to him/her) behaviors. In contrast, the ASEBA items exclusively index the presence of callous behaviors (e.g., doesn't seem to feel guilty, shows little affection). Although the inclusion of positive and negatively worded items (on the APSD, ICU, and other scales like them) may guard against response bias, it implicitly assumes that the construct of CU is bi-dimensional. We question this assumption, as the absence of prosocial or empathic behaviors is not necessarily informative about the presence of callous behavior. Second, whereas the APSD and ICU focus exclusively on the affective/emotional components of CU, the ASEBA items that we have used also index fear-related and punishment processes (i.e., shows too little fear of getting hurt, punishment doesn't change behavior). Although the inclusion of these sorts of items are by no means unique to the ASEBA (see e.g., Scholte & Van der Ploeg, 2007), we are particularly interested in the ways in which aberrant fear-related processing, including insensitivity to punishment, on the part of children may interact with the use of harsh or inconsistent parenting to give rise and/or maintain high levels of CU and ODD behaviors (Dadds & Salmon, 2003).
Although some may dislike the idea of measuring CU in early childhood for fear that it connotes “fledgling psychopathy,” it is noteworthy that the behavioral descriptors of CU—including low fear, guilt, empathy and unresponsiveness to punishment—are routinely studied in young children are and undergoing normative developmental change during this age period (Cornell & Frick, 2007; Kochanska, Barry, Jimenez, Hollatz, & Woodard, 2009; Luby et al., 2009; Young, Fox, & Zahn-Waxler, 1999). The study of CU in early childhood may help to advance life-course models of antisocial behavior. In our estimation, this benefit outweighs concerns related to negative stigmatization associated with the inappropriate use of terminology involving callous unemotional behaviors (e.g., “CU traits”).
Clinical Implications
These results suggest that young children with clinically elevated levels of ODD behaviors may benefit from interventions directed at either improving caregiver-child relationship quality (especially attachment disorganization) and/or reducing CU behaviors (e.g., by increasing emotional connectedness). These interventions may help interrupt a developmental cascade of early emerging aggressive behaviors in early childhood that persist throughout middle childhood. One candidate program is the Attachment and Biobehavioral Catchup (ABC) Intervention Program (Dozier, Peloso, Lewis, Laurenceau, & Levine, 2008), which is designed to help children develop long-term regulatory capabilities by helping parents to modify parenting cognitions and behaviors in ways that promote supportive parent-child interactions and organized and secure parent-child attachment relationships. Given that attachment disorganization may signify risk at the child and environmental levels, such a multi-level, multi-target intervention may be critical for reducing long-term risk for aggressive behavior in children. When considered more broadly, these results provide additional evidence for the consideration of environmental factors in the study of CU (Farrington, Ullrich, & Salekin, 2010).
Limitations
This study is characterized by at least three strengths and three weaknesses. Strengths included (1) replication of the factor structure of ASEBA items in a large sample, (2) capitalization of repeated measures that spanned age 3 years through 6th grade, and (3) a multi-informant/method assessment strategy—including parent-rated early child behaviors, observer-rated disorganization, and teacher-rated aggression—that guarded against method variance as an explanation of effects. Limitations included (1) the low-risk/normative nature of the NICHD-SECCYD sample, (2) evidence that attrition was biased toward riskier families, and (3) the reliance on a finite mixture modeling-based definition of stable aggression as the primary study outcome. With regard to the low-risk sample, despite having nearly 1100 participants in our longitudinal predictive models, only 7% (78/1081) of children exhibited stable elevated levels of aggression across middle childhood. The benefits of generalizability that result from using a community sample are offset by having fewer children who exhibit serious behavior problems than would be the case in a clinical sample. Relatedly, we had too few observations with elevated levels of problem behaviors to fully evaluate potential nonlinearities in the effects of CU and ODD in the prediction of stable elevated aggression, though this will be an important direction for future research in studies that involve large at-risk or clinical samples. With regard to our definition of stable elevated aggression, we adopted the same approach as that used by NICHD SECCYD investigators in previous analyses of this dataset. While this facilitated a continuity of these results with previous studies involving this sample and provided a stronger test of the predictive validity of items than would have been the case had single time points been considered in isolation, we fully acknowledge the concerns that have been raised about validity of this strategy for defining “true” risk groups (Sterba & Bauer, 2010).
Conclusion
This study provided additional evidence regarding the merits of using the ASEBA to screen for a wide range of disruptive behaviors in early childhood, including CU. Given its wide-spread use, secondary data analyses involving the ASEBA provide a unique opportunity to expand the knowledge base regarding the developmental origins, continuity, and predictive validity of CU behaviors in early childhood. The combination of secondary data analysis of extant studies with the initiation of new, prospective longitudinal studies that are optimally designed to inform the developmental antecedents and course of CU behaviors, using gold-standard assessments, holds promise for the prevention of life course antisocial behavior.
Acknowledgments
This study was supported by the National Institute of Child Health and Human Development grant 1R03HD065967-01A1.
References
- Achenbach TM. Manual for the Teacher's Report Form and 1991 Profile. University of Vermont Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms and Profiles: An Integrated System of Multi-informant Assessment. University of Vermont Department of Psychiatry; Burlington, VT: 2000. [Google Scholar]
- Ainsworth MD, Blehar MC, Waters E, Wall S. Patterns of Attachment: A Psychological Study of the Strange Situation. Lawrence Erlbaum Associates; Hillside, NJ: 1978. [Google Scholar]
- Arnold DH, Kupersmidt JB, Voegler-Lee ME, Marshall NA. The association between preschool children's social functioning and their emergent academic skills. Early Childhood Research Quarterly. 2012;27(3):376–386. doi: 10.1016/j.ecresq.2011.12.009. doi: DOI 10.1016/j.ecresq.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard K, Dozier M. Examining Infants’ Cortisol Responses to Laboratory Tasks Among Children Varying in Attachment Disorganization: Stress Reactivity or Return to Baseline? Developmental Psychology. 2010;46(6):1771–1778. doi: 10.1037/a0020660. doi: Doi 10.1037/A0020660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau JF, Easlerbrooks MA, Lyons-Ruth K. Attachment disorganization and controlling behavior in middle childhood: maternal and child precursors and correlates. Attachment & Human Development. 2009;11(3):265–284. doi: 10.1080/14616730902814788. doi: Pii 911414522 Doi 10.1080/14616730902814788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnette ML, Cicchetti D. Multilevel approaches toward understanding antisocial behavior: Current research and future directions. Development and Psychopathology. 2012;24(3):703–704. doi: 10.1017/S0954579412000314. doi: Doi 10.1017/S0954579412000314. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Spieker S, Burchinal M, Poe MD. Trajectories of aggression from toddlerhood to age 9 predict academic and social functioning through age 12. Journal of Child Psychology and Psychiatry. 2006;47(8):791–800. doi: 10.1111/j.1469-7610.2006.01636.x. doi: DOI 10.1111/j.1469-7610.2006.01636.x. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Spieker S, Vandergrift N, Belsky J, Burchinal M, Network NECCR. Predictors and sequelae of trajectories of physical aggression in school-age boys and girls. Development and Psychopathology. 2010;22(1):133–150. doi: 10.1017/S0954579409990319. doi: Doi 10.1017/S0954579409990319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy J, Marvin RS, Childhood M. A. W. G. o. t. J. D. a. C. T. M. N. o. t. T. f. I. t. E. Attachment organization in preschool children: Procedures and coding manual. Pennsylvania State University; 1992. Unpublished coding manual. [Google Scholar]
- Cohen JS, Mendez JL. Emotion Regulation, Language Ability, and the Stability of Preschool Children's Peer Play Behavior. Early Education and Development. 2009;20(6):1016–1037. doi: Pii 917713626 Doi 10.1080/10409280903430745. [Google Scholar]
- Cornell AH, Frick PJ. The moderating effects of parenting styles in the association between behavioral inhibition and parent-reported guilt and empathy in preschool children. Journal of Clinical Child and Adolescent Psychology. 2007;36(3):305–318. doi: 10.1080/15374410701444181. [DOI] [PubMed] [Google Scholar]
- Dadds M, Salmon K. Punishment insensitivity and parenting: temperament and learning as interacting risks for antisocial behavior. Clinical Child and Family Psychology Review. 2003;6:69–86. doi: 10.1023/a:1023762009877. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Fraser J, Frost A, Hawes DJ. Disentangling the underlying dimensions of psychopathy and conduct problems in childhood: A community study. Journal of Consulting and Clinical Psychology. 2005;73(3):400–410. doi: 10.1037/0022-006X.73.3.400. [DOI] [PubMed] [Google Scholar]
- Dozier M, Peloso E, Lewis E, Laurenceau JP, Levine S. Effects of an attachment-based intervention on the cortisol production of infants and toddlers in foster care. Development and Psychopathology. 2008;20(3):845–859. doi: 10.1017/S0954579408000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis BJ, Boyce WT, Belsky J, Bakermans-Kranenburg MJ, van Ijzendoorn MH. Differential susceptibility to the environment: An evolutionary-neurodevelopmental theory. Development and Psychopathology. 2011;23(1):7–28. doi: 10.1017/S0954579410000611. doi: Doi 10.1017/S0954579410000611. [DOI] [PubMed] [Google Scholar]
- Enebrink P, Andershed H, Langstrom N. Callous-unemotional traits are associated with clinical severity in referred boys with conduct problems. Nordic Journal of Psychiatry. 2005;59(6):431–440. doi: 10.1080/08039480500360690. doi: Doi 10.1080/08039480500360690. [DOI] [PubMed] [Google Scholar]
- Farrington DP, Ullrich S, Salekin RT. Environmental influences on child and adolescent psychopathy. In: Salekin RT, Lynam DT, editors. Handbook of child and adolescent psychopathy. Guilford Press; New York: 2010. pp. 202–230. [Google Scholar]
- Fearon RP, Bakermans-Kranenburg MJ, van IJzendoorn MH, Lapsley AM, Roisman GI. The Significance of Insecure Attachment and Disorganization in the Development of Children's Externalizing Behavior: A Meta-Analytic Study. Child Development. 2010;81(2):435–456. doi: 10.1111/j.1467-8624.2009.01405.x. [DOI] [PubMed] [Google Scholar]
- Fowles DC, Kochanska G. Temperament as a moderator of pathways to conscience in children: The contribution of electrodermal activity. Psychophysiology. 2000;37(6):788–795. [PubMed] [Google Scholar]
- Frick PJ, Cornell AH, Barry CT, Bodin SD, Dane HE. Callous-unemotional traits and conduct problems in the prediction of conduct problem severity, aggression, and self-report of delinquency. Journal of Abnormal Child Psychology. 2003;31(4):457–470. doi: 10.1023/a:1023899703866. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Moffitt TE. A Proposal to the DSM-V Childhood Disorders and the ADHD and Disruptive Behavior Disorders Work Groups to Include a Specifier to the Diagnosis of Conduct Disorder based on the Presence of Callous-Unemotional Traits. American Psychiatric Association; 2010. [Google Scholar]
- Frick PJ, White SF. Research Review: The importance of callous-unemotional traits for developmental models of aggressive and antisocial behavior. Journal of Child Psychology and Psychiatry. 2008;49(4):359–375. doi: 10.1111/j.1469-7610.2007.01862.x. [DOI] [PubMed] [Google Scholar]
- Futh A, O'Connor TG, Matias C, Green J, Scott S. Attachment narratives and behavioral and emotional symptoms in an ethnically diverse, at-risk sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(6):709–718. doi: 10.1097/CHI.0b013e31816bff65. doi: Doi 10.1097/Chi.0b013e31816bff65. [DOI] [PubMed] [Google Scholar]
- Graham JM. Congeneric and (essentially) tau-equivalent estimates of score reliability - What they are and how to use them. Educational and Psychological Measurement. 2006;66(6):930–944. doi: Doi 10.1177/0013164406288165. [Google Scholar]
- Green J, Goldwyn R. Annotation: Attachment disorganisation and psychopathology: new findings in attachment research and their potential implications for developmental psychopathology in childhood. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2002;43(7):835–846. doi: 10.1111/1469-7610.00102. [DOI] [PubMed] [Google Scholar]
- Green J, Stanley C, Peters S. Disorganized attachment representation and atypical parenting in young school age children with externalizing disorder. Attachment & Human Development. 2007;9(3):207–222. doi: 10.1080/14616730701453820. doi: Doi 10.1080/14616730701453820. [DOI] [PubMed] [Google Scholar]
- Hawes DJ, Dadds MR, Frost ADJ, Hasking PA. Do Childhood Callous-Unemotional Traits Drive Change in Parenting Practices? Journal of Clinical Child and Adolescent Psychology. 2011;40(4):507–518. doi: 10.1080/15374416.2011.581624. doi: Doi 10.1080/15374416.2011.581624. [DOI] [PubMed] [Google Scholar]
- Hertsgaard L, Gunnar M, Erickson MF, Nachmias M. Adrenocortical Responses to the Strange Situation in Infants with Disorganized Disoriented Attachment Relationships. Child Development. 1995;66(4):1100–1106. [PubMed] [Google Scholar]
- Hyde LW, Shaw DS, Gardner F, Cheong J, Dishion TJ, Wilson M. Dimensions of callousness in early childhood: Links to problem behavior and family intervention effectiveness. Development and Psychopathology. 2013;25(2):347–363. doi: 10.1017/S0954579412001101. doi: Doi 10.1017/S0954579412001101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen PS, Martin D, Cantwell DP. Comorbidity in ADHD: implications for research, practice, and DSM-V. Journal of the American Academy Child and Adolescent Psychiatry. 1997;36(8):1065–1079. doi: 10.1097/00004583-199708000-00014. [DOI] [PubMed] [Google Scholar]
- Kimonis ER, Frick PJ, Skeem JL, Marsee MA, Cruise K, Munoz LC, Morris AS. Assessing callous-unemotional traits in adolescent offenders: Validation of the Inventory of Callous-Unemotional Traits. International Journal of Law and Psychiatry. 2008;31(3):241–252. doi: 10.1016/j.ijlp.2008.04.002. doi: DOI 10.1016/j.ijlp.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Kochanska G, Barry RA, Jimenez NB, Hollatz AL, Woodard J. Guilt and Effortful Control: Two Mechanisms That Prevent Disruptive Developmental Trajectories. Journal of Personality and Social Psychology. 2009;97(2):322–333. doi: 10.1037/a0015471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanska G, Kim S. Toward a new understanding of legacy of early attachments for future antisocial trajectories: Evidence from two longitudinal studies. Development and Psychopathology. 2012;24(3):783–806. doi: 10.1017/S0954579412000375. doi: Doi 10.1017/S0954579412000375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotler JS, McMahon RJ. Child psychopathy: Theories, measurement, and relations with the development and persistence of conduct problems. Clinical Child and Family Psychology Review. 2005;8(4):291–325. doi: 10.1007/s10567-005-8810-5. [DOI] [PubMed] [Google Scholar]
- Loeber R, Pardini DA, Hipwell A, Stouthamer-Loeber M, Keenan K, Sembower MA. Are There Stable Factors in Preadolescent Girls’ Externalizing Behaviors? Journal of Abnormal Child Psychology. 2009;37(6):777–791. doi: 10.1007/s10802-009-9320-6. doi: DOI 10.1007/s10802-009-9320-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long JS, Freese J. Regression models for categorical dependent variables using STATA. Stata Press; College Station: 2003. [Google Scholar]
- Luby J, Belden A, Sullivan J, Hayen R, McCadney A, Spitznagel E. Shame and guilt in preschool depression: evidence for elevations in self-conscious emotions in depression as early as age 3. Journal of Child Psychology and Psychiatry. 2009;50(9):1156–1166. doi: 10.1111/j.1469-7610.2009.02077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons-Ruth K, Bronfman E, Parsons E. Maternal frightened, frightening, or atypical behavior and disorganized infant attachment patterns. Monographs of the Society for Research in Child Development. 1999;64(3):67–+. doi: 10.1111/1540-5834.00034. [DOI] [PubMed] [Google Scholar]
- Mathias CW, Furr RM, Daniel SS, Marsh DM, Shannon EE, Dougherty DM. The relationship of inattentiveness, hyperactivity, and psychopathy among adolescents. Personality and Individual Differences. 2007;43(6):1333–1343. doi: DOI 10.1016/j.paid.2007.04.002. [Google Scholar]
- Mathiesen KS, Sanson A. Dimensions of early childhood behavior problems: Stability and predictors of change from 18 to 30 months. Journal of Abnormal Child Psychology. 1999;28:15–31. doi: 10.1023/a:1005165916906. [DOI] [PubMed] [Google Scholar]
- McElwain NL, Booth-LaForce C, Lansford JE, Wu XY, Dyer WJ. A Process Model of Attachment-Friend Linkages: Hostile Attribution Biases, Language Ability, and Mother-Child Affective Mutuality as Intervening Mechanisms. Child Development. 2008;79(6):1891–1906. doi: 10.1111/j.1467-8624.2008.01232.x. doi: DOI 10.1111/j.1467-8624.2008.01232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon RJ, Witkiewitz K, Kotler JS, CPRG Predictive Validity of Callous-Unemotional Traits Measured in Early Adolescence With Respect to Multiple Antisocial Outcomes. Journal of Abnormal Psychology. 2010;119(4):752–763. doi: 10.1037/a0020796. doi: Doi 10.1037/A0020796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills-Koonce WR, Gariepy JL, Sutton K, Cox MJ. Changes in maternal sensitivity across the first three years: are mothers from different attachment dyads differentially influenced by depressive symptomatology? Attachment & Human Development. 2008;10(3):299–317. doi: 10.1080/14616730802113612. [DOI] [PubMed] [Google Scholar]
- Moran P, Rowe R, Flach C, Briskman J, Ford T, Maughan B, Goodman R. Predictive Value of Callous-Unemotional Traits in a Large Community Sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(11):1079–1084. doi: 10.1097/CHI.0b013e3181b766ab. doi: Doi 10.1097/Chi.0b013e3181b766ab. [DOI] [PubMed] [Google Scholar]
- Munoz LC, Frick PJ. The reliability, stability, and predictive utility of the self-report version of the Antisocial Process Screening Device. Scandinavian Journal of Psychology. 2007;48(4):299–312. doi: 10.1111/j.1467-9450.2007.00560.x. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus Users Guide. Seventh Edition Los Angeles, CA: 1998-2013. [Google Scholar]
- Nagin DS. Analyzing developmental trajectories: A semi-parametric, group-based approach. Psychological Methods. 1999;4:139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Network NECCR. Child-care and family predictors of preschool attachment and stability from infancy. Developmental Psychology. 2001;37(6):847–862. [PubMed] [Google Scholar]
- Network NECCR. Trajectories of physical aggression from toddlerhood to middle childhood: Predictors, correlates, and outcomes. Monographs for the Society of Research Child Development. 2004;69(4):1–129. doi: 10.1111/j.0037-976x.2004.00312.x. [DOI] [PubMed] [Google Scholar]
- Obradović J, Boyce WT. The role of stress reactivity for child development: Indices, correlates and future directions. In: Mayes LC, Lewis M, editors. The environment of human development: A handbook of theory and measurement. Cambridge University Press; New York: 2012. [Google Scholar]
- Olson SL, Bates JE, Sandy JM, Lanthier R. Early developmental precursors of externalizing behavior in middle childhood and adolescence. Journal of Abnormal Child Psychology. 2000;28(2):119–133. doi: 10.1023/a:1005166629744. [DOI] [PubMed] [Google Scholar]
- Pardini D, Obradovic J, Loeber R. Interpersonal callousness, hyperactivity/impulsivity, inattention, and conduct problems as precursors to delinquency persistence in boys: A comparison of three grade-based cohorts. Journal of Clinical Child and Adolescent Psychology. 2006;35(1):46–59. doi: 10.1207/s15374424jccp3501_5. doi: DOI 10.1207/s15374424jccp3501_5. [DOI] [PubMed] [Google Scholar]
- Pardini DA, Lochman JE, Powell N. The development of callous-unemotional traits and antisocial behavior in children: Are there shared and/or unique predictors? Journal of Clinical Child and Adolescent Psychology. 2007;36(3):319–333. doi: 10.1080/15374410701444215. [DOI] [PubMed] [Google Scholar]
- Pasalich DS, Dadds MR, Hawes DJ, Brennan J. Attachment and callous-unemotional traits in children with early-onset conduct problems. Journal of Child Psychology and Psychiatry. 2012;53(8):838–845. doi: 10.1111/j.1469-7610.2012.02544.x. doi: DOI 10.1111/j.1469-7610.2012.02544.x. [DOI] [PubMed] [Google Scholar]
- Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. American Psychologist. 1989;44(2):329–335. doi: 10.1037//0003-066x.44.2.329. [DOI] [PubMed] [Google Scholar]
- Pauli-Pott U, Haverkock A, Pott W, Beckmann D. Negative emotionality, attachment quality, and behavior problems in early childhood. Infant Mental Health Journal. 2007;28(1):39–53. doi: 10.1002/imhj.20121. doi: Doi 10.1002/Imhj.20121. [DOI] [PubMed] [Google Scholar]
- Raykov T. Scale reliability, Cronbach's Coefficient Alpha, and violations of essential tau-equivalence with fixed congeneric components. Multivariate Behavioral Research. 1997;32(4):329–353. doi: 10.1207/s15327906mbr3204_2. [DOI] [PubMed] [Google Scholar]
- Raykov T. Estimation of maximum reliability: A note on a covariance structure modeling approach. British Journal of Mathematical & Statistical Psychology. 2004;57:21–27. doi: 10.1348/000711004849295. [DOI] [PubMed] [Google Scholar]
- Rose SL, Rose SA, Feldman JF. Stability of behavior problems in very young children. Development and Psychopathology. 1989;1:5–19. [Google Scholar]
- Rowe R, Maughan B, Moran P, Ford T, Briskman J, Goodman R. The role of callous and unemotional traits in the diagnosis of conduct disorder. Journal of Child Psychology and Psychiatry. 2010;51(6):688–695. doi: 10.1111/j.1469-7610.2009.02199.x. doi: DOI 10.1111/j.1469-7610.2009.02199.x. [DOI] [PubMed] [Google Scholar]
- Scholte EM, Van der Ploeg JD. The development of a rating scale to screen social and emotional detachment in children and adolescents. International Journal of Methods in Psychiatric Research. 2007;16(3):137–149. doi: 10.1002/mpr.222. doi: Doi 10.1002/Mpr.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw DS, Lacourse E, Nagin DS. Developmental trajectories of conduct problems and hyperactivity from ages 2 to 10. Journal of Child Psychology and Psychiatry. 2005;46(9):931–942. doi: 10.1111/j.1469-7610.2004.00390.x. [DOI] [PubMed] [Google Scholar]
- Shirtcliff EA, Vitacco MJ, Graf AR, Gostisha AJ, Merz JL, Zahn-Waxler C. Neurobiology of Empathy and Callousness: Implications for the Development of Antisocial Behavior. Behavioral Sciences & the Law. 2009;27(2):137–171. doi: 10.1002/bsl.862. doi: Doi 10.1002/Bsl.862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spangler G, Grossmann KE. Biobehavioral organization in securely and insecurely attached infants. Child Development. 1993;64:1439–1450. doi: 10.1111/j.1467-8624.1993.tb02962.x. [DOI] [PubMed] [Google Scholar]
- Sterba SK, Bauer DJ. Matching method with theory in person-oriented developmental psychopathology research. Development and Psychopathology. 2010;22(2):239–254. doi: 10.1017/S0954579410000015. doi: Doi 10.1017/S0954579410000015. [DOI] [PubMed] [Google Scholar]
- Waschbusch DA. A meta-analytic examination of comorbid hyperactive-impulsive-attention problems and conduct problems. Psychological Bulletin. 2002;128(1):118–150. doi: 10.1037/0033-2909.128.1.118. [DOI] [PubMed] [Google Scholar]
- Willoughby MT, Waschbusch DA, Moore GA, Propper CB. Using the ASEBA to Screen for Callous Unemotional Traits in Early Childhood: Factor Structure, Temporal Stability, and Utility. Journal of Psychopathology and Behavioral Assessment. 2011;33(1):19–30. doi: 10.1007/s10862-010-9195-4. doi: DOI 10.1007/s10862-010-9195-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SK, Fox N, Zahn-Waxler C. The relations between temperament and empathy in 2-year-olds. Developmental Psychology. 1999;35:1189–1197. doi: 10.1037//0012-1649.35.5.1189. [DOI] [PubMed] [Google Scholar]