Abstract
Background
The independent and combined influence of smoking, alcohol consumption, physical activity, diet, sitting time, and sleep duration and quality on health status is not routinely examined. This study investigates the relationships between these lifestyle behaviors, independently and in combination, and health-related quality of life (HRQOL).
Methods
Adult members of the 10,000 Steps project (n = 159,699) were invited to participate in an online survey in November-December 2011. Participant socio-demographics, lifestyle behaviors, and HRQOL (poor self-rated health; frequent unhealthy days) were assessed by self-report. The combined influence of poor lifestyle behaviors were examined, independently and also as part of two lifestyle behavior indices, one excluding sleep quality (Index 1) and one including sleep quality (Index 2). Adjusted Cox proportional hazard models were used to examine relationships between lifestyle behaviors and HRQOL.
Results
A total of 10,478 participants provided complete data for the current study. For Index 1, the Prevalence Ratio (p value) of poor self-rated health was 1.54 (p = 0.001), 2.07 (p≤0.001), 3.00 (p≤0.001), 3.61 (p≤0.001) and 3.89 (p≤0.001) for people reporting two, three, four, five and six poor lifestyle behaviors, compared to people with 0–1 poor lifestyle behaviors. For Index 2, the Prevalence Ratio (p value) of poor self-rated health was 2.26 (p = 0.007), 3.29 (p≤0.001), 4.68 (p≤0.001), 6.48 (p≤0.001), 7.91 (p≤0.001) and 8.55 (p≤0.001) for people reporting two, three, four, five, six and seven poor lifestyle behaviors, compared to people with 0–1 poor lifestyle behaviors. Associations between the combined lifestyle behavior index and frequent unhealthy days were statistically significant and similar to those observed for poor self-rated health.
Conclusions
Engaging in a greater number of poor lifestyle behaviors was associated with a higher prevalence of poor HRQOL. This association was exacerbated when sleep quality was included in the index.
Introduction
Engaging in one or more poor lifestyle behaviors such as smoking, risky alcohol consumption, physical inactivity and poor diet increases mortality risk [1]–[4]. These behaviors are associated with mortality risk in a dose-response manner as the number of poor behaviors increases [1]–[4]. Evidence also indicates an association between the time spent sitting and sleeping and poorer health status [3]–[9]. A greater number of hours spent sitting per day is associated with increased risk of chronic disease, CVD and all-cause mortality [7], [10], [11]. In addition, sleeping <7 or >8 hours per night is linked to increased risk of CVD and all-cause mortality [4], [12]. Studies have demonstrated that longer sitting duration or not sleeping 7 to 8 hours per night in combination with smoking, risky alcohol consumption, physical inactivity and poor diet, as part of a lifestyle behavior index, is associated with increased mortality risk in a dose-response manner [3], [4], [13], [14]. However, few studies have examined the association between health status and the aforementioned lifestyle behaviors when both sitting duration and not sleeping 7 to 8 hours per night are included in the analyses [4], [15]. This is important as many adults engage in all these lifestyle behaviors in ways that are considered to pose a risk to their health [1], [7], [10], [15]–[17].
Additionally, sleep duration is only one component of sleep behavior; sleep quality may also impact health status independent of sleep duration [6], [18]. Sleep quality can be defined as difficulty in falling asleep and/or remaining asleep and is commonly assessed in population studies by self-report and user ratings [19], [20]. Up to 41% of adults report sleep difficulties or poor sleep quality [6], [21], yet the impact of sleep quality in combination with a wide variety of other lifestyle behaviors is infrequently examined as a potential influence of health status. Self-rated health and health-related quality of life are overall indicators of health status that are predictive of mortality and chronic disease risk [22]. As such, they are useful indicators to understand how lifestyle behaviors influence the health status. Therefore, the purpose of this study was to 1) examine how smoking, risky alcohol consumption, physical inactivity, poor dietary behaviors, prolonged sitting time, not sleeping 7 to 8 hours per night and poor sleep quality are individually associated with poor self-rated health and frequent unhealthy days, and 2) examine the combined association of these behaviors with poor self-rated health and frequent unhealthy days in two indices, one excluding sleep quality and one including sleep quality.
Methods
Design and Participants
For this cross-sectional study, participants were members of the 10,000 Steps project. 10,000 Steps is a web-based (www.10000steps.org.au) physical activity promotion initiative where participants record the number of steps taken each day. A pedometer is used by participants to quantify their walking activity. The project was launched in 2001 and, as of November 2011 when this study was conducted, had 159,698 registered participants. Registered participants remain in the database but on average participants use the website for approximately 44 days [23]. In November 2011, all members were emailed an invitation to participate in an online survey of lifestyle behaviors, health outcomes and satisfaction with the 10,000 Steps project. This manuscript reports only those measures and results relevant to its purpose. The Central Queensland University Human Research Ethics Committee provided approval for the study and all participants provided informed consent to participate in the study via agreeing to take part in the online survey.
Lifestyle Behavior Measures
A single item was used to classify participants as either a current smoker (at least one cigarette per day for the last month) or non-smoker. Alcohol consumption was assessed using two items: the frequency of consuming alcohol and the number of alcoholic drinks consumed on a day when alcohol was consumed. These items were used to classify participants into lower risk (≤2 drinks per day on a day when alcohol was consumed) or higher risk drinking (≥3 drinks per day on a day when alcohol was consumed). These criteria are similar to Australian guidelines for lower risk drinking over the lifetime [24]. Physical activity during the previous seven days was measured using the International Physical Activity Questionnaire Long Form (IPAQ-LF), a valid and reliable measure of walking, moderate and vigorous intensity physical activity undertaken in domestic, occupational, leisure and transport domains [25]. Standard IPAQ-LF scoring guidelines were applied and participants were classified into either Low, Moderate or High amounts of physical activity. Sitting time over the previous seven days on work and non-work days during travel activities, at work, watching TV, using a computer at home and during other leisure activities was measured using the Workforce Sitting Questionnaire, a valid and reliable instrument of sitting time [26]. Daily sitting time was calculated as the sum of sitting time reported during each activity on a work and non-work day based on the number of days worked in the last seven days [26]. Daily sitting time was subsequently classified into 3 categories (<8 hours per day, ≥8 to <11 hours per day, ≥11 hours per day), as these thresholds of sitting have previously been employed to demonstrate associations between sitting time and risk of all-cause mortality [7]. Sleep behaviors were measured using two items from the reliable and valid Pittsburgh Sleep Quality Index (PSQI) [27]: the duration of sleep each night over the past month (hours per night) and the overall sleep quality in the last month (very good, fairly good, fairly bad, very bad). Sleep duration was classified into three categories (<7 hours per night, ≥7 to <8 hours per night, ≥8 hours per night) based on the associations of not sleeping 7 to 8 hours per night with obesity, cardiovascular disease and all-cause mortality risk [4], [12], [28]. Sleep quality was categorized into three groups, fairly bad (very bad and fairly bad), fairly good and very good based on the distribution of the data and previous use of a trichotomous classification of sleep quality which demonstrated associations with quality of life [29]. Based on a previously used scale [30], dietary behaviors were assessed using four items that evaluated the daily frequency of fruit and vegetable consumption and the number of times soft drinks and fast foods were consumed in the previous 7 days [30]. Higher consumption of fruits and vegetables is associated with lower risk of obesity while greater soft drink and fast food consumption is associated with higher risk of obesity [30]; thus, the four measures were combined into a scale of overall dietary behaviors. Due to different recall periods of the four items, responses were converted to z-scores and summed together. The inverse of the z-scores for soft drink and fast food were used in the summary score of dietary behaviors so that a higher score reflected a better dietary quality. The dietary behaviors score was subsequently classified into tertiles (Highest Tertile (better diet), Middle Tertile (average diet), Lowest Tertile (poorer diet)). Participant socio-demographics assessed included age, sex, education, household income per annum, body mass index (BMI), occupational status, marital status and presence of chronic disease (presence or absence). These socio-demographic characteristics were collapsed into categories as shown in Table 1. The time since the individual registered with 10,000 Steps was obtained from the registration database.
Table 1. Self-rated health, socio-demographic and lifestyle behaviour characteristics of study participants (n = 10,478).
| N = 10,478 | % | |
| Self-Rated Health | ||
| Poor | 1240 | 11.83 |
| Good | 9238 | 88.17 |
| Unhealthy Days | ||
| Frequent Unhealthy Days | 2039 | 19.46 |
| Infrequent Unhealthy Days | 8439 | 80.54 |
| Gender | ||
| Female | 7390 | 70.53 |
| Male | 3088 | 29.47 |
| Age | ||
| 18–34 | 1842 | 17.58 |
| 35–44 | 2359 | 22.51 |
| 45–54 | 3557 | 33.95 |
| 55+ | 2720 | 25.96 |
| Education | ||
| Secondary School or Less | 1703 | 16.25 |
| TAFE | 2339 | 22.32 |
| University | 6436 | 61.42 |
| Paid Employment | ||
| Yes | 9303 | 88.79 |
| No | 1175 | 11.21 |
| Household Income | ||
| <$50,000 per year | 751 | 7.17 |
| $50,001–$100,000 per year | 3187 | 30.42 |
| >$100,000 per year | 4673 | 44.60 |
| other/not reported | 1867 | 17.82 |
| Marital Status | ||
| Never Married | 2928 | 27.94 |
| Separated/other | 1157 | 11.04 |
| Currently Married | 6393 | 61.01 |
| Chronic Disease | ||
| Yes | 5196 | 49.56 |
| No | 5282 | 50.41 |
| BMI | ||
| Healthy Weight (≥18.5 - <25) | 4051 | 38.66 |
| Overweight (25 - <30) | 3753 | 35.82 |
| Obese (≥30) | 2674 | 25.52 |
| Smoking Status | ||
| Non-smoker | 9749 | 93.04 |
| Current Smoker | 729 | 6.96 |
| Alcohol Consumption | ||
| Lower risk | 7433 | 70.94 |
| Higher risk | 3045 | 29.06 |
| Physical Activity | ||
| High | 5091 | 48.59 |
| Moderate | 3927 | 37.48 |
| Low | 1460 | 13.93 |
| Dietary Behaviours | ||
| Highest Tertile (better diet) | 3505 | 33.44 |
| Middle Tertile | 3209 | 30.63 |
| Lowest Tertile (poorer diet) | 3765 | 35.93 |
| Sitting Time | ||
| <8 hrs per day | 4228 | 40.35 |
| 8 to <11 hrs per day | 4226 | 40.33 |
| ≥11 hrs per day | 2024 | 19.32 |
| Sleep Duration | ||
| ≥7 to <8 hrs per night | 4205 | 40.13 |
| <7 hrs per night | 3979 | 37.97 |
| ≥8 hrs per night | 2294 | 21.89 |
| Sleep Quality | ||
| Very Good | 1836 | 17.52 |
| Fairly Good | 6188 | 59.06 |
| Fairly Bad/Very bad | 2454 | 23.42 |
Note: TAFE is provider of vocational non-bachelor education up to level of advanced diploma.
Outcome Measures
Health related quality of life was measured using the CDC Healthy Days Instrument, a valid and reliable measure of self-rated health, frequency of unhealthy days in the last 30 days and activity limitation [31]. This instrument has demonstrated acceptable test-retest reliability and validity when compared to the SF-36 Health Survey [32], [33]. Similar to previous research, the current study uses two outcomes from the Healthy Days instrument: self-rated health, dichotomized as poor (poor or fair) and good health (good, very good or excellent); and unhealthy days, dichotomized as frequent unhealthy days (≥14 unhealthy days out of the past 30 days) or infrequent unhealthy days (<14 unhealthy days out of the past 30 days) [34]–[36].
Analysis
Analysis was limited to participants who provided complete data on the socio-demographics, health-related quality of life, and lifestyle behaviors (n = 10,478). Multi-variable Robust Cox regression with a constant time (time = 1) for all participants was used to estimate the prevalence of poor self-rated health and frequent unhealthy days in relation to lifestyle behaviors [37]. Separate analyses were used to examine the prevalence of study outcomes by each lifestyle behavior when adjusting for socio-demographic characteristics and other lifestyle behaviors. To assess the joint impact of lifestyle behaviors, two lifestyle behavior indices were created. In Index 1, each participant scored a single point for each of the following lifestyle behaviors: current smoker, higher risk alcohol, moderate or low physical activity, middle or lower tertile of dietary behaviors, sitting time of ≥8 hours per day, and sleep duration of <7 hours or ≥8 hours per day (possible Index 1 range was 0 to 6). In Index 2, participants scored a single point for each of the behaviors in Index 1 and scored an additional point if they reported fairly good or fairly bad sleep quality (possible Index 2 range was 0 to 7). This approach to creating Lifestyle Behavior Indices allows this study to examine how multiple lifestyle behaviors influence health status and extends similar studies [3] by the inclusion of smoking, alcohol, physical activity, dietary, sitting and sleep duration to be examined in a single index, which few studies have done previously [4], [15]. It further extends knowledge regarding the influence of multiple lifestyle behaviors on health status by examining all these behaviors when sleep quality is also included [19], [38]. Adding sleep quality in a separate index of multiple lifestyle behaviors will help to demonstrate the relative importance of this infrequently examined factor. Due to the low number of participants with a score of zero in each index (Index 1 = 3.14%; Index 2 = 0.73%), participants with a score of 0 or 1 were collapsed into a single category in each index. Separate analyses were then undertaken to examine the prevalence of study outcomes by each index adjusting for socio-demographic characteristics. Full details of the covariates included in each model are detailed in Tables 2 and 3. Analyses were conducted using STATA 12.0 and a p value of 0.05.
Table 2. Prevalence of Poor Self-rated Health and Frequent Unhealthy Days Across Different Health Behaviors (n = 10,478).
| Poor Self-rated Health | Frequent Unhealthy Days | |||
| Health Behavior | PR (95% C.I)1 | p | PR (95% C.I)1 | p |
| Smoking Status | ||||
| Non Smoker | 1.00 | 1.00 | ||
| Current Smoker | 1.37 (1.17–1.60) | <0.001 | 1.18 (1.04–1.34) | 0.008 |
| Alcohol Consumption | ||||
| Lower Risk | 1.00 | 1.00 | ||
| Higher Risk | 0.98 (0.88–1.09) | 0.736 | 0.88 (0.81–0.96) | 0.003 |
| Physical Activity | ||||
| High | 1.00 | 1.00 | ||
| Moderate | 1.58 (1.40–1.78) | <0.001 | 1.05 (0.96–1.14) | 0.281 |
| Low | 2.17 (1.89–2.48) | <0.001 | 1.34 (1.21–1.48) | <0.001 |
| Dietary Habits | ||||
| Highest Tertile (better diet) | 1.00 | 1.00 | ||
| Middle Tertile | 1.11 (0.95–1.29) | 0.175 | 0.99 (0.90–1.10) | 0.901 |
| Lowest Tertile (poorer diet) | 1.41 (1.23–1.63) | <0.001 | 1.09 (0.99–1.20) | 0.085 |
| Sitting Time | ||||
| <8 hrs per day | 1.00 | 1.00 | ||
| 8 to <11 hrs per day | 1.14 (1.01–1.28) | 0.037 | 1.15 (1.05–1.25) | 0.003 |
| ≥11 hrs per day | 1.33 (1.17–1.52) | <0.001 | 1.32 (1.20–1.46) | <0.001 |
| Sleep Duration | ||||
| 7 to <8 hrs per night | 1.00 | 1.00 | ||
| <7 hrs per night | 1.14 (1.01–1.28) | 0.040 | 1.27 (1.16–1.40) | <0.001 |
| ≥8 hrs per night | 1.30 (1.12–1.50) | <0.001 | 1.26 (1.13–1.42) | <0.001 |
| Sleep Quality | ||||
| Very Good | 1.00 | 1.00 | ||
| Fairly Good | 1.76 (1.42–2.17) | <0.001 | 1.75 (1.49–2.06) | <0.001 |
| Fairly/Very Bad | 3.03 (2.43–3.79) | <0.001 | 3.24 (2.73–3.85) | <0.001 |
Notes: 1. Models were adjusted for length of 10,000 Steps membership, age (18–34; 34–44; 45–54; 55+), gender (male; female), paid employment status (Yes; No), educational level (Secondary School or Less; TAFE; University), annual income (<$50,000 per year; $50,001–$100,000 per year; >$100,000 per year; other/not reported), marital status (Never Married; Separated/other; Currently Married), presence of chronic disease (Yes; No), BMI (Healthy Weight; Overweight; Obese) and all other behaviors listed in the table.
Table 3. Association between multiple poor lifestyle behaviors and the prevalence of Poor Self-Rated Health and Frequent Unhealthy Days (n = 10,478).
| Poor Self-Rated Health | Frequent Unhealthy Days | |||
| Lifestyle Behavior Index | PR (95% C.I)1 | p | PR (95% C.I)1 | p |
| Index 1 | ||||
| 0–1 | 1.00 | 1.00 | ||
| 2 | 1.54 (1.19–1.98) | 0.001 | 1.31 (1.12–1.53) | 0.001 |
| 3 | 2.07 (1.63–2.63) | <0.001 | 1.54 (1.33–1.79) | <0.001 |
| 4 | 3.00 (2.36–3.81) | <0.001 | 1.83 (1.57–2.12) | <0.001 |
| 5 | 3.61 (2.78–4.69) | <0.001 | 1.98 (1.66–2.36) | <0.001 |
| 6 | 3.89 (2.71–5.60) | <0.001 | 2.07 (1.49–2.86) | <0.001 |
| Index 2 | ||||
| 0–1 | 1.00 | 1.00 | ||
| 2 | 2.26 (1.25–4.09) | 0.007 | 1.25 (0.94–1.65) | 0.129 |
| 3 | 3.29 (1.87–5.81) | <0.001 | 1.74 (1.34–2.27) | <0.001 |
| 4 | 4.68 (2.66–8.21) | <0.001 | 2.09 (1.61–2.72) | <0.001 |
| 5 | 6.48 (3.68–11.40) | <0.001 | 2.57 (1.97–3.33) | <0.001 |
| 6 | 7.91 (4.45–14.06) | <0.001 | 2.71 (2.05–3.59) | <0.001 |
| 7 | 8.55 (4.59–15.94) | <0.001 | 2.90 (1.97–4.28) | <0.001 |
Notes: 1. Models were adjusted for length of 10,000 Steps membership, age (18–34; 34–44; 45–54; 55+), gender (male; female), paid employment status (Yes; No), educational level (Secondary School or Less; TAFE; University), annual income (<$50,000 per year; $50,001–$100,000 per year; >$100,000 per year; other/not reported), marital status (Never Married; Separated/other; Currently Married), presence of chronic disease (Yes; No), BMI (Healthy Weight; Overweight; Obese).
Results
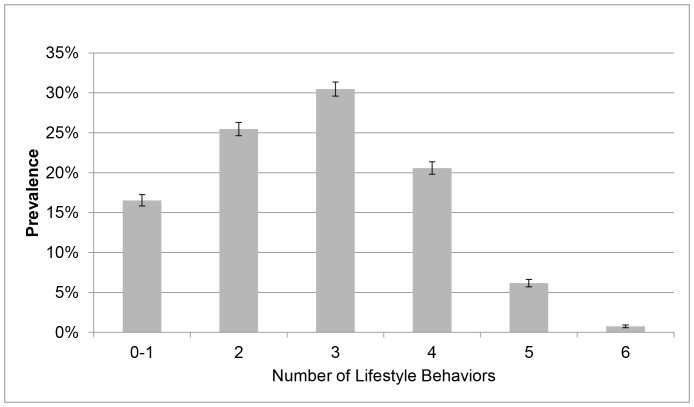
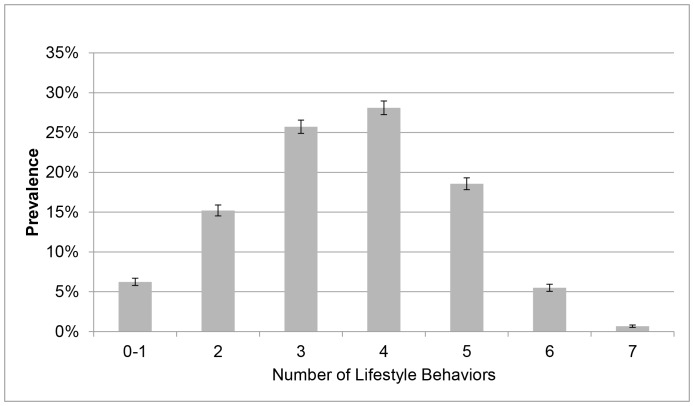
A total of 14,145 individuals completed the survey providing a response rate of 11.66%. The main reasons for non-response to the email invitation were undeliverable emails (e.g., no longer in use, bounce back, out of office reply) (n = 38,434) and decline to participate (n = 2,106). Due to missing data for variables included in the analysis, the current analysis is delimited to 10,478 individuals. The majority of participants were female (70.53%), aged 45–54 years (33.95%), had a University level of education (61.42%) and were in paid employment (88.79%). Approximately 39% of participants were classified as having a healthy BMI (Table 1). The overall prevalence of poor self-rated health and frequent unhealthy days was 11.83% and 19.46%, respectively. The majority of participants reported being non-smokers, consumed alcohol at lower risk levels and engaged in a high level of physical activity (Table 1). Most participants reported sitting less than 11 hours per day and obtaining fairly good sleep quality. For Index 1, over one-half of participants (57.23%) reported 3–5 poor lifestyle behaviors (Figure 1), which increased to nearly three-quarters of participants (72.39%) for Index 2 (Figure 2).
Figure 1. Prevalence of Multiple Poor Lifestyle Behaviors (Index 1).
Figure 1 Notes. The proportion of participants reported zero to one, two, three, four, five and six poor health behaviors was 16.54%, 25.47%, 30.47%, 20.59%, 6.17%, and 0.75%, respectively. Unadjusted prevalence and 95% CI.
Figure 2. Prevalence of Multiple Poor Lifestyle Behaviors (Index 2).
Figure 2 Notes. The proportion of participants reported zero to one, two, three, four, five and six poor health behaviors was 6.24%, 15.20%, 25.72%, 28.10%, 18.57%, 5.50%, and 0.67%, respectively. Unadjusted prevalence and 95% CI.xl.
Table 2 summarizes the associations between individual lifestyle behaviors and health-related quality of life. Current smokers reported a higher prevalence of poor health compared to non-smokers for both outcomes (Table 2). Higher risk alcohol consumption was associated with a lower prevalence of frequent unhealthy days compared to lower risk alcohol consumption. Lower levels of physical activity were associated with a higher prevalence poor self-rated health; however, the association between physical activity and frequent unhealthy days was only significant for low compared to high levels of physical activity. Participants reporting the poorest quality diet had a higher prevalence of poor self-rated health; however, there was no association between the prevalence of frequent unhealthy days and dietary behaviors. Compared to sitting for 8 hours or less per day, sitting for 8 to 11 hours per day and sitting for more than 11 hours per day was associated with poor self-rated health and frequent unhealthy days. Compared to sleeping 7 to 8 hours per night, sleeping <7 hours per night and sleeping ≥8 hours per night was associated with a higher prevalence of poor health for both outcomes. Compared to participants reporting very good sleep quality, reporting fairly good and fairly bad sleep quality was associated with a higher prevalence of both outcomes.
Table 3 shows that the prevalence of poor self-rated health and frequent unhealthy days increases with the number of poor lifestyle behaviors reported. For Index 1, compared to reporting 0–1 poor lifestyle behaviors, participants reporting two poor lifestyle behaviors had a higher prevalence of poor self rated health (PR = 1.54, 95% CI: 1.19–1.98) and frequent unhealthy days (PR = 1.31, 95% CI: 1.12–1.53). Participants reporting the maximum number of poor lifestyle behaviors in Index 1 (six behaviors) had a higher prevalence of poor self-rated health (PR = 3.89, 95% CI: 2.71–5.60) and frequent unhealthy days (PR = 2.07, 95% CI: 1.49–2.86). For Index 2, participants reporting two poor lifestyle behaviors had a higher prevalence of poor self-rated health (PR = 2.26, 95% CI: 1.25–4.09) but not frequent unhealthy days (PR = 1.25, 95% CI: 0.94–1.65). The prevalence of poor self-rated health (PR = 8.55, 95% CI: 4.59–15.94) and frequent unhealthy days (PR = 2.90, 95% CI: 1.97–4.28) was higher in participants reporting the maximum number of poor lifestyle behaviors (seven behaviors) in Index 2 compared to participants reporting 0–1 poor lifestyle behaviors. The prevalence of poor self-rated health is notably higher when sleep quality is considered as a lifestyle behavior.
Discussion
This study demonstrated that smoking, lower levels of physical activity, poor dietary behaviors, higher sitting time, and poor sleep behaviors were independently associated with a higher prevalence of poor self-rated health and frequent unhealthy days. Furthermore, a greater number of poor lifestyle behaviors were associated with a higher prevalence of poorer health. The outcomes of this study extend similar examinations of multiple lifestyle behaviors [3], [4], [13]–[15] by demonstrating that sleep quality exacerbated the association between unhealthy behaviors and health outcomes. This finding is a novel and important aspect of this study given most participants reported less than optimal sleep quality and that 75% of participants reported engaging in more than 3 poor lifestyle behaviors. It also reinforces the notion that reducing the number of people engaging in multiple unhealthy behaviors is an important public health objective [3], [4], [15].
An individual’s risk of poor health increases when they engage in multiple unhealthy lifestyle behaviors [1], [4], [39]. The results of this study, demonstrating that individual poor lifestyle behaviors and each additional poor lifestyle behavior is associated with poorer health, provides strong rationale to intervene on multiple lifestyle behaviors at the population level [5], [40], [41]. There is good evidence regarding the effectiveness of interventions targeting both improvements in physical activity and dietary habits to reduce CVD risk [42] and a large literature base discussing the theoretical, conceptual and methodological issues associated with conducting multiple behavior change interventions [43]–[45]. Although debate exists whether sequential or simultaneous interventions are more effective in changing behaviors [44], interventions have been effective in changing two [46], [47], three [48], and four or more behaviors simultaneously [49], suggesting that it may be possible to intervene on all the lifestyle behaviors examined in the current study. However, as others have noted [39], [50], the challenge lies in disseminating such an intervention to large number of individuals at acceptable cost.
The findings regarding sleep duration and poorer health are consistent with other studies demonstrating that sleeping less than 7 hours per day or sleeping more than 8 hours per day is associated with poorer self-rated health, future risk of type 2 diabetes and increased all-cause mortality [4], [51], [52]. The current study extends these observations by demonstrating that sleep quality is also associated with the prevalence of poor self-rated health when adjusting for a wide range of lifestyle behaviors previously linked to poor self-rated health [1], [16], [53], [54]. It is noteworthy that, compared to other lifestyle behaviors, poor sleep quality was associated with the highest prevalence of poor self-rated health in the current study. Although in some ways a modifiable voluntary behavior, sleep quality is also influenced by aging, chronic health conditions, and obesity [55], [56]. Although the current study statistically adjusted for age, chronic disease status, and BMI, it may be that covariate control was inadequate to fully account for the complex influence of these factors on the relationship between sleep quality and self-rated health [52]. Prospective studies that enable stratified analysis by these factors are needed to disentangle this relationship [52]. Alternatively, it may be that the negative psychophysical consequences of poor quality sleep are sufficient to lower individuals’ perceived health status even after statistically adjusting for other lifestyle behaviors. Further, evidence indicates that physical activity may improve sleep quality [55], [56] Thus, it may be that interventions targeting multiple lifestyle behaviors may enhance the individual behaviors and also create synergistic improvements in targeted behaviors [44].
Consistent with previous studies [54], [57], the current study demonstrated that longer duration of sitting time is associated with poorer self-rated health and extends those studies by demonstrating this relationship when accounting for a number of other lifestyle behaviors including sleep. Sleep behavior is seldom accounted for when examining relationships between sitting and health status despite its impact on health status [4], [5], [15], [40]. As such, this association is a useful contribution to this literature. The prevalence of poor self-rated health and frequent unhealthy days in the current study is comparable to other studies of the general population in other countries, including Australia, suggesting that this population was not biased by higher levels of self-rated health [36], [39]. The association between higher alcohol intake and the lower prevalence of frequent unhealthy days is both in agreement with and in contrast to other studies and may be due to the volumes of alcohol consumed by participants, their pattern of consumption or other unmeasured factors [14], [58]. As this study population had a high proportion of middle-aged females and participants from a higher socio-economic status (based on education and income) it would be useful to confirm if the presence of the associations observed in this study are present in more representative populations. Further limitations to the current study are a reliance on self-report measures of lifestyle behaviors and its cross-sectional nature. The response rate to the current survey was modest compared to other online surveys [59], and was likely impacted by the number of undeliverable emails which is a function of the long period of time that people have been able to register on the 10,000 Steps website. These limitations are offset by the strengths of the study, including the sample size, examination of health indicators that are strongly linked to chronic disease risk and mortality [31], [35], assessment of behaviors and outcomes using measures with good psychometric properties, and the range of lifestyle behaviors examined. Currently there are few studies that have examined sleep duration and quality in conjunction with other lifestyle behaviors such as physical activity, diet and sitting that are more commonly examined in the public health context. This is a significant strength of the current study given the growing recognition of sleep behavior as an important lifestyle behavior to assist in reducing the prevalence of chronic diseases and other public health issues [5], [60]. Furthermore, examining the role of sleep quality is an important extension of previous studies that have only examined sleep duration as a risk factor of poor health.
In conclusion, this study demonstrated that, excluding alcohol intake, each of the poor lifestyle behaviors examined was associated with poor health status and that the prevalence of poor health increased as the number of poor lifestyle behaviors increased. Furthermore, associations when examining the combined influence on unhealthy lifestyle behaviors were exacerbated when sleep quality was included in the index, indicating the importance of sleep quality in maintaining good self-rated health.
Funding Statement
Queensland Health provided funding to Central Queensland University for the development of 10,000 Steps. 10,000 is a joint Australian, State, and Territory Government Initiative under the National Partnership Agreement on Preventive Health. This manuscript was supported by the CQUniversity Health CRN. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Ford ES, Zhao G, Tsai J, Li C (2011) Low-risk lifestyle behaviors and all-cause mortality: findings from the National Health and Nutrition Examination Survey III Mortality Study. Am J Public Health 101: 1922–1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Loef M, Walach H (2012) The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med 55: 163–170. [DOI] [PubMed] [Google Scholar]
- 3.Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, Verschuren WM (2013) Sufficient sleep duration contributes to lower cardiovascular disease risk in addition to four traditional lifestyle factors: the MORGEN study. Eur J Prev Cardiol. [DOI] [PubMed]
- 4. Martinez-Gomez D, Guallar-Castillon P, Leon-Munoz LM, Lopez-Garcia E, Rodriguez-Artalejo F (2013) Combined impact of traditional and non-traditional health behaviors on mortality: a national prospective cohort study in Spanish older adults. BMC Med 11: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Luyster FS, Strollo PJ Jr, Zee PC, Walsh JK (2012) Sleep: a health imperative. Sleep 35: 727–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, van den Berg JF, Verschuren WM (2011) Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN study. Sleep 34: 1487–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A (2012) Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med 172: 494–500. [DOI] [PubMed] [Google Scholar]
- 8. Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA (2011) Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. European heart journal 32: 1484–1492. [DOI] [PubMed] [Google Scholar]
- 9. Chau JY, Grunseit AC, Chey T, Stamatakis E, Brown WJ, et al. (2013) Daily Sitting Time and All-Cause Mortality: A Meta-Analysis. PLoS ONE 8: e80000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. George ES, Rosenkranz RR, Kolt GS (2013) Chronic disease and sitting time in middle-aged Australian males: findings from the 45 and Up Study. Int J Behav Nutr Phys Act 10: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Patel AV, Bernstein L, Deka A, Feigelson HS, Campbell PT, et al. (2010) Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol 172: 419–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sabanayagam C, Shankar A (2010) Sleep duration and cardiovascular disease: results from the National Health Interview Survey. Sleep 33: 1037–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Eguchi E, Iso H, Tanabe N, Wada Y, Yatsuya H, et al. (2012) Healthy lifestyle behaviours and cardiovascular mortality among Japanese men and women: the Japan collaborative cohort study. European heart journal 33: 467–477. [DOI] [PubMed] [Google Scholar]
- 14. Odegaard AO, Koh WP, Gross MD, Yuan JM, Pereira MA (2011) Combined lifestyle factors and cardiovascular disease mortality in Chinese men and women: the Singapore Chinese health study. Circulation 124: 2847–2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ding D, Rogers K, Macniven R, Kamalesh V, Kritharides L, et al. Revisiting Lifestyle Risk Index Assessment in a Large Australian Sample: Are Sedentary Behavior and Sleep Correlated with Health Outcomes? Preventive Medicine: In press. [DOI] [PubMed]
- 16. Li C, Ford ES, Mokdad AH, Balluz LS, Brown DW, et al. (2008) Clustering of cardiovascular disease risk factors and health-related quality of life among US adults. Value Health 11: 689–699. [DOI] [PubMed] [Google Scholar]
- 17. Magee CA, Kritharides L, Attia J, McElduff P, Banks E (2012) Short and long sleep duration are associated with prevalent cardiovascular disease in Australian adults. J Sleep Res 21: 441–447. [DOI] [PubMed] [Google Scholar]
- 18. Altman NG, Izci-Balserak B, Schopfer E, Jackson N, Rattanaumpawan P, et al. (2012) Sleep duration versus sleep insufficiency as predictors of cardiometabolic health outcomes. Sleep Med 13: 1261–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cappuccio FP, D’Elia L, Strazzullo P, Miller MA (2010) Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 33: 414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM (2006) Recommendations for a standard research assessment of insomnia. Sleep 29: 1155–1173. [DOI] [PubMed] [Google Scholar]
- 21. McKnight-Eily L, Liu Y, Perry G, Presley-Cantrell L, Strine T (2009) Perceived Insufficient Rest or Sleep Among Adults – United States, 2008. MMWR 58: 1175–1179. [PubMed] [Google Scholar]
- 22. Ernstsen L, Nilsen SM, Espnes GA, Krokstad S (2011) The predictive ability of self-rated health on ischaemic heart disease and all-cause mortality in elderly women and men: the Nord-Trondelag Health Study (HUNT). Age Ageing 40: 105–111. [DOI] [PubMed] [Google Scholar]
- 23.Mummery W, Hinchliffe A, Joyner K, Duncan MJ, Caperchione C (2008) E-Health promotion: a descriptive analysis of participant use of an online physical activity step log. 10th International Congress of Behavioral Medicine. Tokyo, Japan.
- 24.National Health and Medical Research Council (2009) Australian Guidelines to reduce health risk from drinking alcohol. Canberra: National Health and Medical Research Council, Australian Goverment.
- 25. Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, et al. (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35: 1381–1395. [DOI] [PubMed] [Google Scholar]
- 26. Chau JY, van der Ploeg HP, Dunn S, Kurko J, Bauman AE (2011) A tool for measuring workers’ sitting time by domain: the Workforce Sitting Questionnaire. Br J Sports Med 45: 1216–1222. [DOI] [PubMed] [Google Scholar]
- 27. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28: 193–213. [DOI] [PubMed] [Google Scholar]
- 28. Magee CA, Caputi P, Iverson DC (2010) Is sleep duration associated with obesity in older Australian adults? J Aging Health 22: 1235–1255. [DOI] [PubMed] [Google Scholar]
- 29. Haseli-Mashhadi N, Pan A, Ye X, Wang J, Qi Q, et al. (2009) Self-Rated Health in middle-aged and elderly Chinese: distribution, determinants and associations with cardio-metabolic risk factors. BMC Public Health 9: 368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Smith KJ, McNaughton SA, Gall SL, Blizzard L, Dwyer T, et al. (2009) Takeaway food consumption and its associations with diet quality and abdominal obesity: a cross-sectional study of young adults. Int J Behav Nutr Phys Act 6: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centres for Disease Control and Prevention (2000) Measuring Healthy Days. Atlanta, Georgia.
- 32.Newschaffer C (1998) Validation of Behavioral Risk Factor Surveillance System (BRFSS) HRQOL Measures in a Statewide Sample. Atlanta: CDC.
- 33. Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J (2003) Retest reliability of surveillance questions on health related quality of life. J Epi Community Health 57: 339–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ford ES, Moriarty DG, Zack MM, Mokdad AH, Chapman DP (2001) Self-reported body mass index and health-related quality of life: findings from the Behavioral Risk Factor Surveillance System. Obes Res 9: 21–31. [DOI] [PubMed] [Google Scholar]
- 35. Moriarty DG, Zack MM, Kobau R (2003) The Centers for Disease Control and Prevention’s Healthy Days Measures - population tracking of perceived physical and mental health over time. Health Qual Life Outcomes 1: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Davies CA, Vandelanotte C, Duncan MJ, van Uffelen JG (2012) Associations of physical activity and screen-time on health related quality of life in adults. Prev Med 55: 46–49. [DOI] [PubMed] [Google Scholar]
- 37. Barros AJ, Hirakata VN (2003) Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 3: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chandola T, Ferrie JE, Perski A, Akbaraly T, Marmot MG (2010) The effect of short sleep duration on coronary heart disease risk is greatest among those with sleep disturbance: a prospective study from the Whitehall II cohort. Sleep 33: 739–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tsai J, Ford ES, Li C, Zhao G, Pearson WS, et al. (2010) Multiple healthy behaviors and optimal self-rated health: Findings from the 2007 Behavioral Risk Factor Surveillance System Survey. Preventive Medicine 51: 268–274. [DOI] [PubMed] [Google Scholar]
- 40. Chee MW (2013) Sleep, public health and wellness: the elephant in the room. Annals of the Academy of Medicine, Singapore 42: 105–107. [PubMed] [Google Scholar]
- 41. Owen N, Healy GN, Matthews CE, Dunstan DW (2010) Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev 38: 105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Artinian NT, Fletcher GF, Mozaffarian D, Kris-Etherton P, Van Horn L, et al. (2010) Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation 122: 406–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Noar SM, Chabot M, Zimmerman RS (2008) Applying health behavior theory to multiple behavior change: considerations and approaches. Prev Med 46: 275–280. [DOI] [PubMed] [Google Scholar]
- 44. Prochaska JJ, Spring B, Nigg CR (2008) Multiple health behavior change research: an introduction and overview. Prev Med 46: 181–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Prochaska JJ, Velicer WF, Nigg CR, Prochaska JO (2008) Methods of quantifying change in multiple risk factor interventions. Prev Med 46: 260–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. King AC, Castro CM, Buman MP, Hekler EB, Urizar GG Jr, et al. (2013) Behavioral Impacts of Sequentially versus Simultaneously Delivered Dietary Plus Physical Activity Interventions: the CALM Trial. Annals of behavioral medicine 46: 157–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Vandelanotte C, Reeves MM, Brug J, De Bourdeaudhuij I (2008) A randomized trial of sequential and simultaneous multiple behavior change interventions for physical activity and fat intake. Prev Med 46: 232–237. [DOI] [PubMed] [Google Scholar]
- 48. Hyman DJ, Pavlik VN, Taylor WC, Goodrick GK, Moye L (2007) Simultaneous vs sequential counseling for multiple behavior change. Arch Intern Med 167: 1152–1158. [DOI] [PubMed] [Google Scholar]
- 49. Parekh S, Vandelanotte C, King D, Boyle FM (2012) Improving diet, physical activity and other lifestyle behaviours using computer-tailored advice in general practice: a randomised controlled trial. Int J Behav Nutr Phys Act 9: 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rabin BA, Brownson RC, Kerner JF, Glasgow RE (2006) Methodologic Challenges in Disseminating Evidence-Based Interventions to Promote Physical Activity. Am J Prev Med 31: 24–34. [DOI] [PubMed] [Google Scholar]
- 51. Magee CA, Caputi P, Iverson DC (2011) Relationships between self-rated health, quality of life and sleep duration in middle aged and elderly Australians. Sleep Med 12: 346–350. [DOI] [PubMed] [Google Scholar]
- 52. Holliday EG, Magee CA, Kritharides L, Banks E, Attia J (2013) Short sleep duration is associated with risk of future diabetes but not cardiovascular disease: a prospective study and meta-analysis. PLoS One 8: e82305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sodergren M, McNaughton S, Salmon J, Ball K, Crawford D (2012) Associations between fruit and vegetable intake, leisure-time physical activity, sitting time and self-rated health among older adults: cross-sectional data from the WELL study. BMC Public Health 12: 551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rosenkranz R, Duncan M, Rosenkranz S, Kolt G (2013) Active lifestyles related to excellent self-rated health and quality of life: Cross sectional findings from 196,876 participants in The 45 and Up Study. BMC Public Health 13. [DOI] [PMC free article] [PubMed]
- 55. Kline CE, Irish LA, Krafty RT, Sternfeld B, Kravitz HM, et al. (2013) Consistently high sports/exercise activity is associated with better sleep quality, continuity and depth in midlife women: the SWAN sleep study. Sleep 36: 1279–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Atkinson G, Davenne D (2007) Relationships between sleep, physical activity and human health. Physiol Behav 90: 229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vallance JK, Eurich D, Marshall AL, Lavallee CM, Johnson ST (2013) Associations between sitting time and health-related quality of life among older men. Mental Health and Physical Activity.
- 58. Byles J, Young A, Furuya H, Parkinson L (2006) A drink to healthy aging: The association between older women’s use of alcohol and their health-related quality of life. J Am Geriatr Soc 54: 1341–1347. [DOI] [PubMed] [Google Scholar]
- 59. Duncan MJ, Rashid M, Vandelanotte C, Cutumisu N, Plotnikoff RC (2013) Development and reliability testing of a self-report instrument to measure the office layout as a correlate of occupational sitting. International Journal of Behavioral Nutrition and Physical Activity 10: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Grander MA, Hale L, Moore M, Patel NP (2010) Mortality associated with short duration: the evidence, the possible mechanisms, and the future. Sleep Medicine Reviews 14: 191–203. [DOI] [PMC free article] [PubMed] [Google Scholar]