Abstract
Methomyl is a potent pesticide that is widely used in the field of agriculture. The systemic toxic effects of methomyl have been well described. However, the neurological effects of methomyl intoxication are not well understood. In this study, we report a 61-year-old Taiwanese man sent to our emergency department because of altered mental status. His family stated that he had consumed liquid methomyl in a suicide attempt. He was provided cardiopulmonary resuscitation because of unstable vital signs. He was then sent to an intensive care unit for close observation. On the second day of admission, he regained consciousness but exhibited irregular limb and torso posture. On the sixth day, he started to complain of blurred vision. An ophthalmologist was consulted but no obvious abnormalities could be identified. On suspicion of cerebral disease, a neurologist was consulted. Further examination revealed cortical blindness and decorticate posture. Cerebral magnetic resonance imaging (MRI) was arranged, which identified bilateral occipital regions lesions. The patient was administered normal saline and treated with aspirin and piracetam for 3 weeks in hospital. During the treatment period, his symptom of cortical blindness resolved, whereas his decorticate posture was refractory. Follow-up brain MRI results supported our clinical observations by indicating the disappearance of the bilateral occipital lesions and symmetrical putaminal high signal abnormalities. In this article, we briefly discuss the possible mechanisms underlying the cerebral effects of methomyl poisoning. Our study can provide clinicians with information on the manifestations of methomyl intoxication and an appropriate treatment direction.
Key words: methomyl, cortical blindness, decorticate posture, cardiopulmonary resuscitation, cerebral magnetic imaging
Introduction
Methomyl is a carbamate pesticide widely used by farmers to protect agricultural products.1 Ingesting liquid methomyl is life threatening because of the inhibitory effects of methomyl on human acetylcholinesterase.2,3 However, the subsequent neurotoxic effects of the compound, direct or indirect, are not well described. The common manifestations of methomyl poisoning are excessive salivation, fluctuating blood pressure, depressed mental status, and muscle stiffness.2,4,5 In this study, we report a 61-year-old Taiwanese man who presented with reversible cortical blindness and sustained decorticate posture after consuming a large volume of liquid methomyl in a suicide attempt. We also discuss the correlation between the patient’s clinical symptoms and the neuroimaging observations.
Case Report
A 61-year-old Taiwanese man was admitted to our emergency room because of altered mental status. His wife informed the medical personnel that her husband had quarreled with their son a few days previously, and had remained in a bad mood since the incident. That morning, when she awoke at approximately 6:30 am, she found her husband lying on the bathroom floor. An empty can of liquid methomyl was beside him. She estimated that her husband had swallowed approximately 300 cm3 of methomyl. Further examination revealed depressed consciousness (Glasgow Coma Scale, E1M1V1). The patient’s eyes had pinpoint pupils and his blood pressure and pulse were absent. He was also unable to breathe spontaneously. Cardiac arrest was confirmed and the patient underwent cardiac massage for 11 minutes. He was also intubated to maintain his breathing. After cardiopulmonary resuscitation (CPR), his vital signs of blood pressure, temperature, pulse rate, and respiratory rate, returned to within reference rages: 110/70 mmHg, 36.7°C, 68 beats/min, and 29 breaths/min, respectively. An emergency doctor provided a gastric lavage. The patient was sent to an intensive care unit for close observation. On the second day of admission, he regained consciousness and could open his eyes spontaneously and under instruction. However, his posture was irregular (upper extremities flexed upwardly and lower extremities extended). We instructed him to extend his upper extremities but he was unable to follow this order. On the sixth day of admission, the patient was extubated after showing general improvement in condition. However, he started to complain of unclear vision. Although he could sense an object in front of him and could recognize the object when placed in his hands, he was unable to identify the object correctly. Suspecting an eye problem, we consulted an ophthalmologist to determine whether any ocular abnormality existed. A fundoscopy and other eye testing revealed no obvious abnormalities. A neurological examination was also conducted, confirming decorticate posture and cortical blindness. Other neurological findings, including those regarding the patient’s motor and sensory systems, coordination, deep tendon reflexes, and cranial nerves, were all unremarkable. Therefore, we arranged a brain MRI to eliminate possible central visual pathway lesions. The brain MRI revealed lesions in the bilateral tips of the occipital lobe areas (Figure 1A, B). We hydrated the patient with normal saline and administered 75 mg of aspirin once daily and 150 mg of piracetam twice daily. He remained in the hospital for 3 weeks, after which he was discharged for neurology outpatient clinical follow-up. He attended outpatient clinical follow-ups for 2 months after discharge and his vision improved, whereas his decorticate posture remained refractory. A second brain MRI was performed, revealing the disappearance of the bilateral occipital lobe lesions and symmetrical putaminal high signal abnormalities (Figure 2). This patient continues to attend regular follow-ups at the clinic.
Figure 1.

Brain magnetic resonance sequencing diffusion-weighted imaging (A) showed high signal intensities over bilateral occipital regions whereas in Apparent Diffusion Coefficient Mapping (B) showed decreased signals (black arrows).
Figure 2.
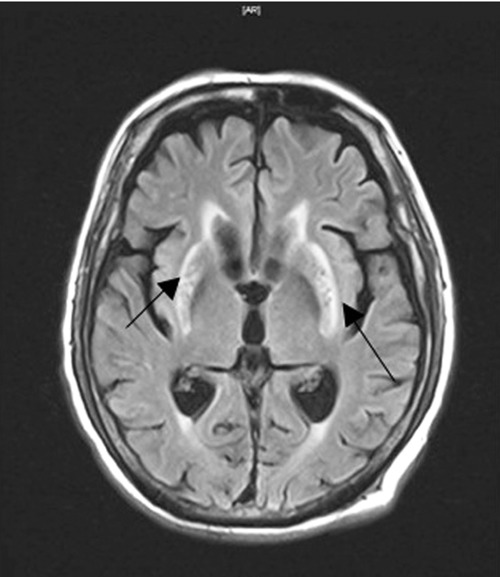
Follow-up brain magnetic resonance imaging - fluid attenuated inversion recovery sequencing showed resolution of bilateral occipital lesions with symmetrical putaminal high signal abnormalities (black arrows).
Discussion
Our patient regained consciousness after aggressive CPR and gastric lavage. Cortical blindness improved after aspirin and piracetam treatment. Our patient had developed decorticate posture and subsequent cortical blindness after methomyl intoxication. Following treatment, his symptom of cortical blindness subsided, whereas his decorticate posture persisted. Brain MRI studies initially revealed occipital lesions, followed by the resolution of these lesions and symmetrical putaminal high signal abnormalities. The order of clinical symptom presentation contrasted with the patient’s cerebral MRI findings.
Hu et al. reported visual impairment after acute insecticide poisoning following the ingestion of malathion.1 Malathion and methomyl share some chemical characteristics.1,2 Previous studies have suggested that the central visual pathway can be intermittently interrupted because of the indirect effect of decreased blood flow to the occipital regions.1,4,5 A post-CPR state can also cause transient cortical blindness,2,6-8 possibly through the disproportionate allocation of cerebral blood flow. Cortical blindness has been reported in children and adult patients.3,8 However, in these patients, unlike our case, their cortical blindness was permanent. The association between the cerebral effects of methomyl intoxication and the anoxic state after CPR remains under investigation.
According to our research, no previous study has reported permanent decorticate posture after a post-CPR state or methomyl intoxication. Taga et al. reported transient decorticate posture after thoracic epidural injection,9 although the underlying mechanisms of such symptoms have yet to be elucidated. In this study, we report a 61-year-old Taiwanese man who developed decorticate posture and cortical blindness after methomyl poisoning. His symptom of cortical blindness improved after aggressive aspirin and piracetam treatment, whereas the symptom of decorticate posture remained refractory. Our results can provide physicians with information on the symptoms of methomyl intoxication and the appropriate treatment direction.
References
- 1.Hu YH, Yang CC, Deng JF, et al. Methomyl-alphamethrin poisoning presented with cholinergic crisis, cortical blindness, and delayed peripheral neuropathy. Clin Toxicol (Phila) 2010;48:859-62 [DOI] [PubMed] [Google Scholar]
- 2.Martinez-Chuecos J, Molinero-Somolinos F, Solé-Violàn J, et al. Management of methomyl poisoning. Hum Exp Toxicol 1990;9:251-4 [DOI] [PubMed] [Google Scholar]
- 3.Liddle JA, Kimbrough RD, Needham LL, et al. A fatal episode of accidental methomyl poisoning. Clin Toxicol 1979;15:159-67 [DOI] [PubMed] [Google Scholar]
- 4.Tsatsakis AM, Bertsias GK, Mammas IN, et al. Acute fatal poisoning by methomyl caused by inhalation and transdermal absorption. Bull Environ Contam Toxicol 2001;66:415-20 [DOI] [PubMed] [Google Scholar]
- 5.Tsatsakis AM, Tsakalof AK, Michalodimitrakis EN. The analysis of methomyl, a carbamate pesticide, in post-mortem samples. Sci Justice 1996;36:41-5 [DOI] [PubMed] [Google Scholar]
- 6.Hoyt WF, Walsh FB. Cortical blindness with partial recovery following acute cerebral anoxia from cardiac arrest. AMA Arch Ophthalmol 1958;60:1061-9 [DOI] [PubMed] [Google Scholar]
- 7.Ye XD, Liu K, Chang TH, et al. Transient cortical blindness after resuscitation in a child having central venous catheterization under general anesthesia. Paediatr Anaesth 2006;16:318-21 [DOI] [PubMed] [Google Scholar]
- 8.El Gatit A, Razeq M Abdul., El Snaini F, et al. Reversible cortical blindness following successful surgical repair of two stab wounds in the heart. Libyan J Med 2008;3:52-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taga K, Tomita M, Watanabe I, et al. Complete recovery of consciousness in a patient with decorticate rigidity following cardiac arrest after thoracic epidural injection. Br J Anaesth 2000;85:632-4 [DOI] [PubMed] [Google Scholar]


