Abstract
Posterior reversible encephalopathy syndrome (PRES) is a clinical-radiologic entity not yet understood, that presents with transient neurologic symptoms and particular radiological findings. Few papers show the differences between pregnant and non-pregnant patients. We review the cases of 38 women diagnosed with PRES, in order to find significant differences between pregnant (18) and non-pregnant (20) patients. We found differences among the age of patients (25.83 years old in pregnant and 29.31 years old in non pregnant; P=0.001); in the mean of highest systolic blood pressure, that was higher in non-pregnant group (185:162 mmHg; P=0.121); and in creatinine levels that was higher in non-pregnant group (3.47:1.04 mg/dL; P=0.001). To our knowledge, just a few papers analyzed whether PRES syndrome presented in the same way in pregnant and non-pregnant patients. The differences and the possible pathophisiology of this syndrome still remain enigmatic.
Key words: posterior reversible encephalopathy syndrome, reversible leukoencephalopathy, eclampsia/pre-eclampsia, brain magnetic resonance image, cerebral autoregulation
Introduction
Posterior reversible encephalopathy syndrome (PRES) is a clinicoradiologic entity characterized by headaches, altered mental status, seizures, and visual loss; it is associated with white matter vasogenic edema predominantly affecting the occipital and parietal lobes of the brain.1 The cause of PRES is not yet understood. Auto-regulatory failure with resultant vasodilation, as seen in hypertensive encephalopathy, is often cited as the underlying mechanism. On the other hand, vasospasm with ischemic change is also observed in some patients.2,3
Several factors can trigger the syndrome, most commonly: acute elevation of blood pressure, abnormal renal function and immunosuppressive therapy.1 Other possible etiologies are eclampsia,4-7 transplantation,8 neoplasia and chemotherapy treatment,9 systemic infections,10 renal disease acute or chronic.11,12
The most characteristic imaging pattern in PRES is the presence of edema involving the white matter of the posterior portions of both cerebral hemispheres, especially the parietooccipital regions, in a relatively symmetric pattern that spares the calcarine and paramedian parts of the occipital lobes (Figure 1).1 However, other structures (such as the brain stem, cerebellum, and frontal and temporal lobes) may also be involved, and although the abnormality primarily affects the subcortical white matter, the cortex and the basal ganglia may also be involved.13
Figure 1.
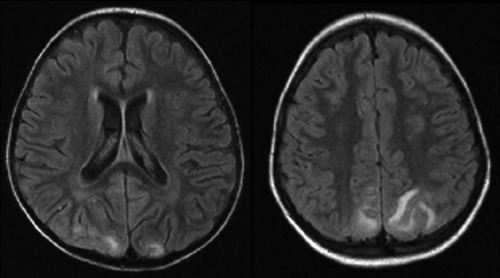
Brain magnetic resonance imaging (FLAIR) showing an increase of signal in both parieto-occipital lobes.
Pre-eclampsia (PE) is one of the most common situations described in association with PRES. PE is a multisystem disorder that complicates 3-8% of pregnancies in Western countries,14,15 and has a complex pathophysiology. Defective invasion of the spiral arteries by cytotrophoblast cells is observed during preeclampsia.16 The crucial issue to understand is that the prime mover of PE is abnormal placentation. Two common theories appear to be interlinked, a genetic theory and an immunological theory.17 Clinical and laboratory tests are intended to define and determine the severity of PE. Headaches, tinnitus, visual disorders, brisk tendon reflexes, and vigilance disorders are related to cerebral edema; oliguria to acute renal failure; uterine contraction, vaginal bleeding to placental abruption; vomiting to HELLP syndrome (Hemolysis Elevated Liver enzymes Low Plaquet count); bandlike epigastric pain to subcapsular hepatic hematoma; and dyspnea to cardiac failure. Eclampsia, the major neurological complication of pre-eclampsia, is defined as a convulsive episode or any other sign of altered consciousness arising in a setting of PE, and which cannot be attributed to a pre-existing neurological condition. Delivery is the only curative treatment for PE.18
Materials and Methods
We realized a study on 38 cases of PRES (18 pregnant and 20 non-pregnant patients), that were admitted to the Neurologic Service of Hospital São Lucas-PUCRS (Brazil) or that were assisted in other units of the same hospital by our services. All the patients underwent a brain magnetic resonance image (MRI): 36 patients (94.73%) were submitted to two brain MRI; 1 was submitted to one brain MRI plus one brain CT; and the other one realized only one exam. The following data was evaluated: age, sex, previous diseases and past medical history, use of medications, the neurologic manifestations, the highest blood pressure during the neurologic presentation, the highest creatinine during the period of observation and the neuroimage alterations in brain MRI.
The highest blood pressure was measured during the 48 hours before the neurologic manifestation and the highest creatinine was analyzed during a mean period of two week before the neurologic manifestation. All the brain MRI were analyzed by a neurologist, who had no contact with the patient’s clinical data. We analyzed the data using the Statistical Package for the Social Sciences (SPSS). We applied Chi-square test or Exact Fischer test for comparing data with non-parametic distribution and the Student t test for comparison of means. A P value <0.05 was considered significant. All of the procedures and protocols executed in this study were approved by the Institutional Ethics Committee from Pontifícia Universidade Católica do Rio Grande do Sul.
Results
It was performed a review of 38 cases of patients with the diagnosis of PRES, that were assisted in Hospital São Lucas-PUCRS. Among this 38 cases, with mean age 25.11 years old (range from 2 to 74) and 78.9% of female, there were three children, that were excluded of some analyzes. The children were excluded of analyze of the creatinine and blood pressure, because in our opinion, their age didn’t premises us to include them in some evaluations (creatinine level and blood pressure). By the way, it was identified 34 patients (eighteen were pregnant or in puerperium period). The other group was composed by four patients with lupus, four with neoplasia in chemotherapy,9,19 four with glomerulonephritis, two patients with hypertension, two patients in use of Tacrolimus after renal transplantation, two patients with Hemolitic Uremic syndrome, one after scorpion sting and one patient with alteration of renal function.20
The mean age of the group of pregnant patients was 25.83 years old and was 29.31 years old in the other group. The group of non-pregnant patients was composed by five men and eleven women.
There was an important difference in the highest systolic blood pressure among both groups. In the non-pregnant group the mean highest systolic blood pressure was 185 mmHg and in the pregnant group was 162 mmHg, but without statistical diference.
The mean creatinine was 3.47 mg/dL in the non-pregnant patients and was 1.04 mg/dL in the pregnant patients.
The most common symptom was headache in both groups 78.8% overall (reported by 88.9% of the pregnant patients and 70% of non-pregnant patients); followed by visual disturbance 65.8% overall (66.7% of pregnant patients and 65% of non-pregnant patients); seizure 63.2% overall (50% in pregnant group and 75% in non-pregnant group) and mental status alteration (22% of pregnant patients and 52% of non-pregnant patients).
The alterations in all patients and the neuroimaging findings are described in Table 1.
Table 1.
Differences among pregnant and non-pregnant patients.
| Pregnant | Non-Pregnant | P | |
|---|---|---|---|
| Age | 25.83 | 29.31 | 0.001* |
| Highest systolic blood pressure, mmHg* | 162 | 185 | 0.121 |
| Patients systolic blood pressure >160 mmHg, % | 66.7 | 81 | 0.308 |
| Patients systolic blood pressure >180 mmHg, % | 16.7 | 61.9 | 0.004* |
| Highest creatinine, mg/dL* | 1.04 | 3.47 | 0.001* |
| Headache (%) | 88.9 (16) | 70 (14) | 0.154 |
| Seizure (%) | 50 (9) | 75 (15) | 0.111 |
| Visual disturbance (%) | 66.7 (12) | 65 (13) | 0.914 |
| Altered mental status (%) | 22 (4) | 55 (11) | 0.039* |
| Magnetic resonance findings (%) Occipital Parietal Frontal Temporal |
83.3 (15) 55.6 (10) 27.8 (5) 22.2 (4) |
100 (20) 65 (13) 30 (6) 30 (6) |
0.057 0.552 0.565 0.587 |
*Patients with less than 12 years old were excluded of analysis.
Discussion and Conclusions
Since 1985, neuro-radiologic findings had been described in the presence of eclampsia and other pregnant dysfunctions.5 After its first description in 1996, many papers were published; however the precise pathophisiological mechanism remains unclear.1 In 2000, Casey et al. proposer the term Posterior Reversible Encephalopathy Syndrome.21 Few papers analyzed if the syndrome presented in pregnant patients was the same described in the other patients with PRES.
In our group of patients, there was a difference in creatinine level; both of them with higher value in non-pregnant group. Even excluding the patient with renal disease (in case of creatinine level analyzes), the difference between the groups remains.
In 2009, Roth explored the differences between pregnant patients and non pregnant patients in a very interesting paper. Studying 21 patients, Roth described few differences in both groups, like headache was more reported by pregnant patients (87.5%) than non-pregnant patients (30.8%) and visual disturbance that was also more reported in pregnant patients than in non-pregnant patients (75% vs 46.2%). In this study, the mean age of pregnant patients was 22 years old and was 49 years old in the group of non-pregnant patients. The blood pressures of both groups were very similar.22
Liman and colleagues performed the investigation of the mean arterial pressure in different groups of patients with PRES and found in infection (131 mmHg), auto-imunes disorders (123 mmHg), eclampsia (119 mmHg) and chemotherapy (110 mmHg).23 Liman also reported that preeclampsia-eclampsia patients had significantly less severe edema, less cytotoxic edema, hemorrhage and contrast enhancement, while more frequent complete resolution of edema and less frequent residual structural lesions were seen on follow-up imaging.24 PRES is commonly seen in the setting of hypertension; probably due to a breakdown of autoregulation.
The autoregulation is an intrinsic function of the vasculature of the brain, designed to maintain a stable blood flow independent of the variation of blood pressure. In animal models, when a severe increase in blood pressure beyond the upper limit of autoregulation was caused, occur an arteriolar dilation, injury to the capillary bed, vasogenic edema and vessel injury with altered artery morphology.25 The upper limits of autoregulation range among the patients. This limits depends primary on the capillary hydrostatic pressure, under the influence of the systolic blood pressure, the integrity of blood-brain barrier and other situations (like medications).26
Evaluating the differences of blood pressure among pregnant and non-pregnant patients, we demonstrated that pregnant patients present breakdown of cerebral autoregulation with lower mean arterial blood pressure. We speculate that the pregnant patients had different triggers of the other patients and the fact of the delivery is the curative treatment for PE can represent the finish of the stimulus for the brain vasogenic edema. Is it the reason that causes differences in the pregnant patients when compared with non-pregnant patients? This paper contributes showing differences of blood pressure and creatinine in this both groups. The precise pathophysiology mechanism of this syndrome remains enigmatic.
References
- 1.Hinchey J, Chaves C, Appignani B, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med 1996;334:494-500 [DOI] [PubMed] [Google Scholar]
- 2.Schwartz RB. Hyperperfusion encephalopathies: hypertensive encephalopathy and related conditions. Neurologist 2002;8:22-34 [DOI] [PubMed] [Google Scholar]
- 3.Bartynski WS, Boardman JF. Catheter angiography, MR angiography, and MR perfusion in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol 2008;29:447-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwartz RB, Feske SK, Polak JF, et al. Preeclampsia-eclampsia: clinical and neuroradiographic correlates and insights into the pathogenesis of hypertensive encephalopathy. Radiology 2000;217:371-6 [DOI] [PubMed] [Google Scholar]
- 5.Colosimo C, Jr, Fileni A, Moschini M, Guerrini P. CT findings in eclampsia. Neuroradiology 1985;27:313-7 [DOI] [PubMed] [Google Scholar]
- 6.Lewis LK, Hinshaw DB, Jr, Will AD, et al. CT and angiographic correlation of severe neurological disease in toxemia of pregnancy. Neuroradiology 1988;30:59-64 [DOI] [PubMed] [Google Scholar]
- 7.Naheedy MH, Biller J, Schiffer M, et al. Toxemia of pregnancy: cerebral CT findings. J Comput Assist Tomogr 1985;9:497-501 [DOI] [PubMed] [Google Scholar]
- 8.Bartynski WS, Tan HP, Boardman JF, et al. Posterior reversible encephalopathy syndrome after solid organ transplantation. AJNR Am J Neuroradiol 2008;29:924-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marrone LC, Marrone BF, Raya JP, et al. Gemcitabine monotherapy associated with posterior reversible encephalopathy syndrome. Case Rep Oncol 2011;4:82-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bartynski WS, Boardman JF, Zeigler ZR, et al. Posterior reversible encephalopathy syndrome in infection, sepsis, and shock. AJNR Am J Neuroradiol 2006;27:2179-90 [PMC free article] [PubMed] [Google Scholar]
- 11.Onder AM, Lopez R, Teomete U, et al. Posterior reversible encephalopathy syndrome in the pediatric renal population. Pediatr Nephrol 2007;22:1921-9 [DOI] [PubMed] [Google Scholar]
- 12.Gokce M, Dogan E, Nacitarhan S, Demirpolat G. Posterior reversible encephalopathy syndrome caused by hypertensive encephalopathy and acute uremia. Neurocrit Care 2006;4:133-6 [DOI] [PubMed] [Google Scholar]
- 13.Lamy C, Oppenheim C, Méder JF, Mas JL. Neuroimaging in posterior reversible encephalopathy syndrome. J Neuroimaging 2004;14:89-96 [PubMed] [Google Scholar]
- 14.Carty DM, Delles C, Dominiczak AF. Preeclampsia and future maternal health. J Hypertens 2010;28:1349-55 [DOI] [PubMed] [Google Scholar]
- 15.Duley L. The global impact of pre-eclamp-sia and eclampsia. Semin Perinatol 2009; 33:130-7 [DOI] [PubMed] [Google Scholar]
- 16.Fisher SJ, McMaster M, Roberts M. The placenta in normal pregnancy and preeclampsia. : Chesley’s hypertensive disorders in pregnancy. Amsterdam: Academic Press, Elsevier; 2009 [Google Scholar]
- 17.Mutze S, Rudnik-Schoneborn S, Zerres K, Rath W. Genes and the preeclampsia syndrome. J Perinat Med 2008;36:38-58 [DOI] [PubMed] [Google Scholar]
- 18.Uzan J, Carbonnel M, Piconne O, et al. Preeclampsia: pathophysiology, diagnosis, and management. Vasc Health Risk Manag 2011;7:467-74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marrone LC Porcello, Marrone BF, Pascoal TA, et al. Posterior reversible encephalopathy syndrome associated with FOLFOX Chemotherapy. Case Rep Oncol Med 2013;2013:306983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marrone LC Porcello, Marrone B Fontana, Neto F Kalil, et al. Posterior reversible encephalopathy syndrome following a scorpion sting. J Neuroimaging 2013;23: 535-6 [DOI] [PubMed] [Google Scholar]
- 21.Casey SO, Sampaio RC, Michel E, Truwit CL. Posterior reversible encephalopathy syndrome: utility of fluid-attenuated inversion recovery MR imaging in the detection of cortical and subcortical lesions. AJNR Am J Neuroradiol 2000;21:1199-06 [PMC free article] [PubMed] [Google Scholar]
- 22.Roth C, Ferbert A. Posterior reversible encephalopathy syndrome: is there a difference between pregnant and non-pregnant patients? Eur Neurol 2009;62:142-8 [DOI] [PubMed] [Google Scholar]
- 23.Liman TG, Bohner G, Heuschmann PU, et al. The clinical and radiological spectrum of posterior reversible encephalopathy syndrome: the retrospective Berlin PRES study. J Neurol 2012;259:155-64 [DOI] [PubMed] [Google Scholar]
- 24.Liman TG, Bohner G, Heuschmann PU, et al. Clinical and radiological differences in posterior reversible encephalopathy syndrome between patients with preeclampsia-eclampsia and other predisposing diseases. Eur J Neurol 2012;19:935-43 [DOI] [PubMed] [Google Scholar]
- 25.Auer LM. The pathogenisis of hypertensive encephalopathy: experimental data and their clinical relevance with special reference to neurosurgical patients. Acta Neurochir Suppl (Wien) 1978;27:1-111 [PubMed] [Google Scholar]
- 26.Feske SK. Posterior reversible encephalopathy syndrome: a review. Semin Neurol 2011;31:202-15 [DOI] [PubMed] [Google Scholar]


