Abstract
Short stem hip arthroplasties with predominantly metaphyseal fixation, such as the METHA® stem (Aesculap, Tuttlingen, Germany), are recommended because they are presumed to allow a more physiologic load transfer and thus a reduction of stress-shielding. However, the hypothesized metaphyseal anchorage associated with the aforementioned benefits still needs to be verified. Therefore, the METHA short stem and the Bicontact® standard stem (Aesculap, Tuttlingen, Germany) were tested biomechanically in synthetic femora while strain gauges monitored their corresponding strain patterns. For the METHA stem, the strains in all tested locations including the region of the calcar (87% of the non-implanted femur) were similar to conditions of synthetic bone without implanted stem. The Bicontact stem showed approximately the level of strain of the non-implanted femur on the lateral and medial aspect in the proximal diaphysis of the femur. On the anterior and posterior aspect of the proximal metaphysis the strains reached averages of 78% and 87% of the non-implanted femur, respectively. This study revealed primary metaphyseal anchorage of the METHA short stem, as opposed to a metaphyseal-diaphyseal anchorage of the Bicontact stem.
Key words: short stem hip arthroplasty, standard stem hip arthroplasty, biomechanical testing, strain gauges, strain patterns
Introduction
Short stem total hip arthroplasties (THA) are suggested for implantation in patients under 60 to 70 years of age. Due to positive clinical outcomes and increased longevity of these implants, the indications for short stem THA have been steadily growing.1-3 Such designs also display advantages in the preservation of bone stock and a supposed metaphyseal anchorage.4 A metaphyseal anchorage would theoretically induce a higher proximal strain distribution, rather than transferring the load to the diaphyseal region of the femur via the implant. This more physiological load transfer is intended to reduce the stress-shielding effect. The implantation of a THA into the femur induces an alteration of the physiological strain patterns,5 taking into account that a short stem with primary metaphyseal anchorage reduces the risk of distal locking and proximal offloading.4 According to Wolff’s law, mechanical stimuli regulate the dynamic remodeling of bone, resulting in changes in density and micro-architecture.6 Stress-shielding is often the result of an implant delivering a load through bone while adjacent areas are no longer stressed. This is of clinical importance because it can lead to proximal bone loss depending on the implant design4,5,7 which is a potential risk factor for aseptic loosening of the femoral implant.8-10 The extent of this stress-shielding effect can be estimated by surface strain measurements using strain gauges.6 This determination of the load transfer characteristics is an important step in the process of biomechanically assessing hip prostheses.11 However, for new implants, evidence regarding strain distribution is sparse and inconclusive. To date, strain patterns after implantation of the METHA short stem (Aesculap, Tuttlingen, Germany) or stems with similar concept of anchorage are unknown. Therefore, the aforementioned advantages of short stem prostheses are only hypothesized.
To alleviate concerns about deleterious changes in bone quality and implant stability, the aim of this study was to monitor the strain patterns of the proximal femur after implantation of the METHA. It was of particular interest to investigate whether a metaphyseal anchorage was present, and whether this design restored the strain patterns of the femur without an implanted stem. Therefore, strain patterns after implantation of the METHA were compared to both strain patterns without an implanted stem and strain patterns following implantation of the standard Bicontact stem (Aesculap, Tuttlingen, Germany).
Materials and Methods
Preparation of the femora
Two synthetic femora (4th generation left adult composite femur, Sawbones Europe, Malmö, Sweden) with identical anatomy and material properties were used as it was done in previous biomechanical studies in a comparable setting.10-15 Each femur was embedded distally in a metal cylinder. The distance extending from the proximal potting to the notch of the femoral neck was 300 mm. A form fitted mold of the proximal femur within an adjustable frame, manufactured based on a previous used femur-aligned reference system,11,16-18 guaranteed a standardized embedding procedure (sagittal and frontal plane at 0°) using Methylmethacrylate (Technovit 4004; Heraeus Kulzer GmbH, Wehrheim, Germany).
Implants
The METHA stem is a short cementless hip stem, which is anchored directly within the closed bony ring of the femoral neck and metaphysis (Figure 1). For this study, a size 4 prosthesis with a CCD-angle of 135° was used. The Bicontact stem is meant to be anchored through bone compression, predominantly in the diaphyseal region of the femur (Figure 1). For this study, a size 17 Bicontact H prosthesis was used. Each stem was implanted according to the manufacturer’s recommendation. Thus, the resection height for the Bicontact was more distal, while the one for the METHA stem restored a 5 mm cortical ring of the femoral neck.
Figure 1.

The prostheses investigated in this study: METHA short stem (left) and Bicontact stem (right); anterior views on the left and medial views on the right.
The femoral stems were inserted by an experienced orthopedic surgeon (TF). Several X-ray images were captured to verify correct implant sizes and positioning as well as to measure the offsets of both non-implanted and implanted femora. To restore the original offset as accurately as possible and consequently to avoid experimental errors due to differences in the lever arm, an appropriate head length was selected for the 32 mm-head (size S for the METHA stem; size M for the Bicontact stem).
Strain measurement
Strain measurements represent deformations of the strain gauges, and thus, of the synthetic bone under loading. Eight strain gauges [3/350 RY91; Hottinger Baldwin Messtechnik GmbH (HBM), Darmstadt, Germany] were bonded to the medial and lateral aspects of the femora at four levels (A-D): 45 (30 mm for the lateral strain gauge), 70, 90, and 150 mm distal to the notch of the femoral neck. At level A, two additional strain gauges were attached to the anterior and posterior aspects (Figure 2). For the Bicontact stem, two additional strain gauges were bonded 250 mm distal to the notch (level E). Each strain gauge at level A-D should illustrate the changes in strain in one of the Gruen zones,19 to enable a comparison of strain measurement and DXA scans. Due to different designs of the tested implants, the Gruen zones around the middle and distal part of the stems vary. Thus, for comparison between the METHA and Bicontact stems, the values recorded by the strain gauges were used (Figure 3).
Figure 2.

Illustration of the vertical levels of the strain gauges with an implanted METHA stem. The positions were the same for the METHA and Bicontact stem. Level D corresponded to the distal tip of the Bicontact stem. The two additional strain gauges for the Bicontact stem at level E (250 mm distal to the notch of the femoral neck) are not illustrated.
Figure 3.
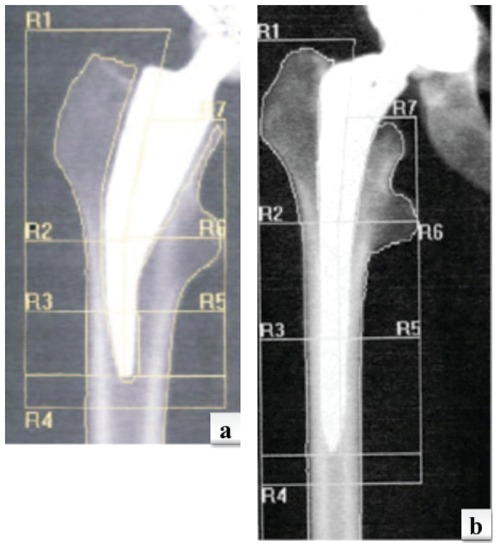
DXA-scans illustrating the Gruen-zones for the METHA (a) and Bicontact (b) stem.
The strain gauges at level D for the METHA and at level E for the Bicontact stem were located approximately 50 mm from the distal end of each implant, far enough so that their measurements should not be affected by the implant’s presence. Thus, the strain gauge readings were able to identify whether identical loading conditions were applied to the non-implanted and implanted femora.16,20
Before mounting the strain gauges the bone surfaces were smoothed with fine sandpaper (#280) and carefully cleaned and degreased with ethanol followed by a cleanser (RMS1, HBM). An optical tracking system based on infrared-marker tracking (Polaris P4, Northern Digital Inc., Waterloo, Ontario, Canada) was used to ensure perpendicular alignment to the longitudinal axis of the femur as well as the precise positioning of strain gauges on each femur. Finally, the strain gauges were bonded with a two-component polymethylmethacrylate adhesive (X60, HBM) and covered with a polyurethane protective (PU 120, HBM). The leads of the gauges were soldered to the wires and connected with a CANHEAD base module (CB1014, HBM) including an amplifier module (CA1030, HBM). The catmanEASY software (Version 3.1, HBM) recorded the data. To avoid heating of the gauges, a bridge excitation voltage of 0.5 volts was selected. Data were attained at a frequency of 100 Hz, with a low-pass cut-off frequency of 10 Hz.
Loading configurations
Under identical set-up and Loading configurations (LCs), the principal strains were first measured on the non-implanted femora and then with the implanted METHA and Bicontact stem, respectively. Six LCs, which have frequently been used in literature,16-18,21 were applied to cover the physiological range of maximum hip-joint angles during a wide range of motor tasks (including single-leg stance, level walking at different speeds, stair climbing and descending, and standing up from seated) (Table 1).
Table 1.
The loading configurations applied in this study. Loading configuration 1 to 4 covered the extreme directions of the hip joint resultant force during a wide range of activities (including level walking at different speeds, single-leg stance, stair climbing and descending, and standing up from seated.21 These configurations did not correspond to any specific motor task.
| Loading configuration | Abduction/adduction | Flexion/extension | Simulation |
|---|---|---|---|
| LC1 | 24° adduction | 0° | Max. adduction |
| LC2 | 0° | 18° flexion | Max. flexion |
| LC3 | 3° adduction | 0° | Max. abduction |
| LC4 | 0° | 3° extension | Max. extension |
| LC5 | 0° | 0° | Force parallel to femoral diaphysis |
| LC6 | 8° adduction | 0° | Single-leg stance |
Mechanical application and measurement protocol
The femora were placed on a 15 kN load cell of a materials testing system (MTS Mini Bionix 858; MTS Systems Corporation, Eden Prairie, Minnesota, USA) using a custom-made jig, consisting of an aluminum cylinder and a platform that allowed a rotation of the femora at a variety of angles (Figure 4). For vertical loading, a floating bearing was attached to the MTS to avoid undesired horizontal forces and moments (Figure 4).
Figure 4.
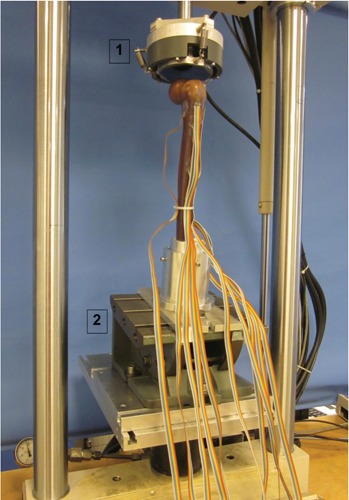
Experimental setup of the biomechanical testing within the Material Testing System including the floating bearing to eliminate horizontal forces (1) and the platform that allowed rotation of the femora at different angles (2). The floating bearing did not touch the greater trochanter.
In order to verify the material linearity and consequentially to determine an appropriate maximum axial force during biomechanical testing, a preliminary measurement was performed where strains were recorded at 100 N loading increments to a maximum load of 800 N at a rate of 10 N/s. At each level, the load was held for 10 seconds and strains were measured for the following 30 seconds. The averages of these data were taken as the result for each loading level. After zeroing the load cell and strain gauges the femora were loaded in a ramp profile up to an axial force of 800 N at a rate of 10 N/s. Using load control, the axial force of 800 N was kept constant for 90 seconds to reduce the influence of the creep effect. After 30 seconds, strains were recorded for the following 60 seconds and the average of these data was taken as the result for this testing. The measurement procedure was repeated five times for each LC. For elastic recovery of the femora, there was an interval of eight minutes between each repetition. This procedure was first conducted on two non-implanted femora for the different LCs. Subsequently, the METHA and Bicontact prostheses were each implanted in one of the tested femora and the measurement protocol was repeated.
The mean values of the principal strains and the angles of the principal strains during the five load repetitions were determined. The coefficient of variance (CoV) was computed for the major principal strains.22 The results from the implanted femora were expressed as a percentage of the strains in the corresponding non-implanted femur. Strain readings from the load application where strains were recorded in 100 N increments were assessed for linearity between force and strain using a coefficient of linear regression R2.
Results
Quality of strain measurement
The CoV of the principal strains within the five repetitions under the same LC was in 92% of the cases less than 1% (average 0.54%), illustrating outstanding measurement repeatability.
There was a strong linear relationship between applied load and strain for all strain gauges and LCs (R2≥0.99 for 92% of all cases), additionally proving the high quality of strain gauge bonding.
After implantation of the stems, strain in the most distal gauges (level D for the METHA stem and level E for the Bicontact stem) was with the exception of LC3 with the METHA stem (+24%) always within a difference of 20% of the strain value in the non-implanted condition, demonstrating consistent loading conditions.16,20
Strain patterns in the non-implanted femora
As expected, negative strains were larger on the medial aspect (i.e. compressive loading) whereas positive strains were larger on the lateral aspect (i.e. tensile loading) for all LCs with the exception of LC1. For LC1, strains were more compressive at the lateral strain gauges of level D and E, and more tensile at the medial strain gauge of level E. These major principal strains are presented in the relevant figures (Figures 5 and 6).
Figure 5.
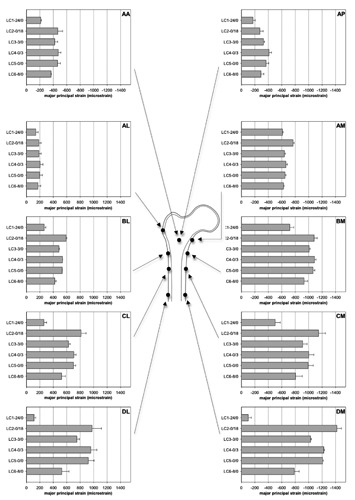
Mean principal compressive (medial, anterior, lateral) and tensile strains (lateral) in the intact femora. Note that strains were compressive for strain gauge DL with loading configuration 1. Averages and standard deviations between the mean values of the five load repetitions of the two femora are reported.
Figure 6.
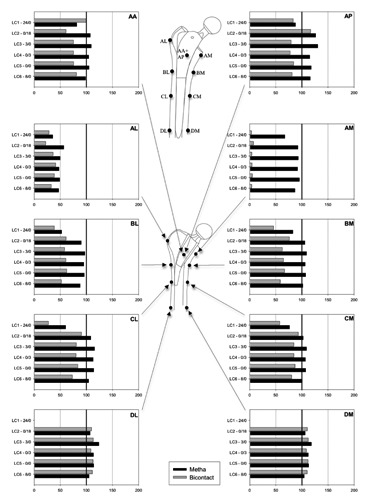
Changes in mean principal compressive (medial, anterior, lateral) and tensile strains (lateral) after implantation of the two stems (in % of the principal strain values in the intact femora). 100% denotes the strain values in the intact femora.
Strain values varied considerably between the locations in the non-implanted femora (Figure 5). The lowest strains were observed on all four aspects at level A, while the highest strains were displayed on the medial side at levels B, C and D. Additionally, the LC had a substantial influence on the principal strains.
The direction of the major principal strains was for all LCs within a few degrees from the axis of the diaphysis on the lateral aspect (and position EM with LC1) and nearly perpendicular to the axis on the medial aspect (and positions DL and EL with LC1), correlating to tensile or compressive loading.
Strain patterns after insertion of stems
Similar to the non-implanted state, the LC had a substantial effect on the largest principal strains for both stems (Figure 6). For all LCs, there were fewer changes in the strain patterns after implantation of the METHA stem compared to the Bicontact stem. Except for the region of the greater trochanter (AL) and three strain gauges with LC1 (BL, CL, AM) the alteration as compared to the non-implanted condition never exceeded 25%. For both stems, an obvious decrease of strain in the region of the greater trochanter (AL) was observed. For the METHA stem, only small decreases were detected in the region of the calcar (AM), compared to larger deviations after implantation of the Bicontact stem. However, the strain values for the Bicontact stem in the anterior and posterior part at level A as well as at the more distal levels C and D were similar to the state without implanted stem.
For both stems, the direction of the major principal strains varied by an average of only 3° (SD 4) between the non-implanted and implanted conditions, with the exception of LC1 for the Bicontact stem, which was on average 70° (SD 10).
Discussion
Although there is insufficient evidence that bone remodeling as a result of stress-shielding directly influences clinical results, it is of paramount concern that the resorption of proximal femoral bone stock has negative effects on the stability and survival of femoral implants.8-10 Thus, the aim of this study was to determine the strain patterns in a proximal femur after implantation of a short stem with supposed primary metaphyseal anchorage under different loading conditions. It was of particular interest to investigate whether signs of metaphyseal load transfer could be determined and whether this design leads to restoration of the strain patterns found with non-implanted femora. Furthermore, a biomechanical testing of an implanted standard Bicontact stem was conducted to enable quantitative comparisons.
The results suggest a greater level of metaphyseal anchorage for the METHA stem compared to the Bicontact stem. We found that the hypothesized reduction of the stress-shielding effect for the METHA short stem compared to a conventional device occurred consistently and measurably. The only location where a substantial change in strain was observed, a reduction of about 50%, was around the greater trochanter. In all other regions, the strains were similar to those in the non-implanted model. The Bicontact stem displayed a metaphyseal-diaphyseal anchorage. At level A in the anterior and posterior part the strain values were similar to the non-implanted state. Due to the different resections, the anatomy of the femora with a small CCD-angle and a different biomechanical concept, the strain in the region of the calcar was dramatically reduced for the Bicontact stem. Thus, the strain values in this region have to be interpreted with care. Around the greater trochanter, the strains were similar to those after implantation of the METHA stem: approximately 50% of the non-implanted model. Below the minor trochanter about 60% of the strains of the non-implanted model were determined for the Bicontact stem. At level C and D, the strains were similar to those of the non-implanted model. Consequently, this may contribute to normal bone remodeling around the stem. Summarizing the data, the METHA short stem seems to induce a metaphyseal anchorage. The bone stock preserving osteotomy, the tapered shape and the bracing of the distal tip of the METHA on the lateral cortex are all intended to restore the load transfer of the non-implanted conditions. The risk of stress-shielding seems to be negligible. For the Bicontact stem, the different resection may explain the dramatic decrease of strain around the calcar. Nevertheless, the strains in the lower levels as well as in the anterior and posterior part of level A demonstrate a combination of metaphyseal and diaphyseal load transfer.
Our findings correspond to the results of other biomechanical studies examining the strain patterns of standard (anatomical) and customized stems.6,8,10,23,24 These studies uniformly revealed a dramatic reduction of the principal strains in the proximal part of the femur for both stem types with the greatest decreases at the calcar especially for the standard stems. Customised proximal fit stems and traditional stems all display non-physiological strain patterns within the proximal femur, with slightly more physiological patterns for the customised stems. When compared with the data from the present study, the METHA short stem seems to reproduce more physiological load transmission to the proximal femur than traditional stems or customised implants.
Other biomechanical studies, comparing the strain distributions of short-stemmed or stemless prosthesis with stem prosthesis, support these findings.8,12,25,26 For example, Decking et al. revealed that in contrast to two conventional stems, which led to decreases in strains in the proximal femur, the bone around the stemless CUT prosthesis (ESKA Implants) showed an increase in the subtrochanteric area and only very few changes in all other areas.8 Bieger et al. evaluated the stress-shielding effect in the proximal femur for a new short stem (Fitmore, Zimmer) in comparison to a clinically successful short stem and standard stem prosthesis (Mayo and CLS, Zimmer) with the result that the reduction of longitudinal cortical strains in the proximal femur was less pronounced for the shorter stem implants.4 According to all these studies including the present study, the stemless as well as short-stemmed prostheses reveal a significantly lower alteration of bone surface deformation after implantation compared to traditional stem prostheses, indicating physiological load transmission and reduced stress-shielding.
Clinical midterm results exist for only a few selected short stem THAs. Due to failure of the thrust plate prosthesis for different reasons,27,28 critics of short stems argue that there is an increased risk of revision and/or inferior functional outcome. However, contemporary short stem devices have a completely different principal design. Due to encouraging results of the Mayo stem – one of the first short stem implants – with a 94% survival rate after 6.2 years,2 other short stems have been developed.29 Thorey et al. published a study with a survival rate of 98% in 148 cases after 5.8 years,30 and Wittenberg et al. with a survival rate of 96.7% for 250 cases after 4.9 years for the short stem tested in this study.31 By changing the biomechanical concept, short stems are intended to improve the load transfer pattern, potentially reducing the failure rate.
Furthermore, there are long-term results after implantation of the Bicontact stem. Swamy et al. reported a survivorship for aseptic loosening of 100% after 12.9 years for 201 prosthesis.32 Ochs et al. published comparable results with an overall survival rate calculated of 95.6% after 17.8 years for 250 THRs.33 These results indicate that the data of the current study cannot be used uncritically to predict the clinical performance of the tested implants. The greater diaphyseal anchorage of the Bicontact stem compared to the METHA short stem seems to support very good implant longevity. Methods such as DXA can only provide indirect information about the stress-shielding effect.5 To directly measure the effects of loading on implants, the present bio-mechanical study was performed using strain gauges located at the different Gruen zones. Thus, biomechanical analysis and DXA-analysis may be correlated. The DXA analysis of Lerch et al. revealed a concentrated load distribution on the medial portion of the femur after implantation of the METHA stem.9 A concentration of bone density indicates load transfer to these regions according to Wolff’s law. In the region of the calcar, BMD exceeded the baseline value by 6.1% two years after implantation. These results are in general agreement with the present study that showed primary metaphyseal anchorage of the METHA stem.
A main limitation of this study was the use of synthetic femora as they cannot perfectly replicate the biological response of human bone. However, cadaveric bone suffers from wide interspecimen variability regarding bone geometry and mechanical properties, which directly affects the results of strain measurements, so that we questioned whether testing on cadaver specimen could illustrate possible differences. Therefore, we decided to use synthetic femora with identical geometry in the first step, whose strong resemblance in mechanical properties to native bone with interspecimen variability of only between 2.6 and 3.1 % for the axial and bending load was proved in previous studies.34 A fairly high number of studies previously also used synthetic bones for similar biomechanical testing.10-15 Due to the small interspecimen variability of synthetic bones it is reasonable to perform the testing on different synthetic femora.10,11,13 However, due to the fact that only one femur for each stem was used, only qualitative differences can be noted. Thus, the results of the implanted femora were illustrated as the percentage of the strains of the non-implanted femur as done in similar studies (e.g. Ganapathi et al.).13
The aim of this study was to examine the influence of the geometry of the stem on the proximal femoral strain patterns. For this aim, other external factors had to be equalized as good as possible. For this reason a repeatable positioning of the strain gauges is highly relevant for the different femora. This was guaranteed by applying a well-defined reference system including an optical tracking system. Thus, this device accounts for very little variability between the different femora.
To avoid bone damage due to repeated loading an axial force of 800 N was applied as done by Ganapathi et al.13 However, as the linearity between force and strain was proven, the strain patterns do not depend on the absolute amount of the applied load, because the results of the implanted femora were expressed as a percentage of the strains in the identical non-implanted femora. Muscles and forces provided by other soft tissue were not simulated during biomechanical testing. However, it has been reported that studies,16 in which the testing set-up did not feature muscles,16-18 can reliable analyze the strain patterns of the proximal femur.
Conclusions
In conclusion, our data indicate that the METHA short stem induced a proximal load transfer, which supports that a primary metaphyseal anchorage occurred. This is in contrast to the pattern following implantation of the traditional Bicontact stem, which demonstrated a metaphyseal-diaphyseal anchorage. However, due to the different scope of this study, these results cannot be used uncritically to predict the clinical outcome of the investigated stems. Whether the different strain patterns observed in the present study are correlated to the clinical outcome has to be shown by long-term clinical follow-up of the two stems.
Acknowledgments
The study was kindly supported by the Hochschulinterne Leistungsförderung (HiLF) of the Hannover Medical School and by Aesculap who provided the implants for the biomechanical testing.
References
- 1.Ettinger M, Ettinger P, Lerch M, et al. The NANOS short stem in total hip arthroplasty: a mid term follow-up. Hip Int 2011;21:583-6 [DOI] [PubMed] [Google Scholar]
- 2.Morrey BF, Adams RA, Kessler M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg Br 2000;82:952-8 [DOI] [PubMed] [Google Scholar]
- 3.Schmidutz F, Grote S, Pietschmann M, et al. Sports activity after short-stem hip arthroplasty. Am J Sports Med 2012;40:425-32 [DOI] [PubMed] [Google Scholar]
- 4.Bieger R, Ignatius A, Decking R, et al. Primary stability and strain distribution of cementless hip stems as a function of implant design. Clin Biomech (Bristol Avon) 2012;27:158-64 [DOI] [PubMed] [Google Scholar]
- 5.Herrera A, Panisello JJ, Ibarz E, et al. Comparison between DEXA and finite element studies in the long-term bone remodeling of an anatomical femoral stem. J Biomech Eng 2009;131:041013. [DOI] [PubMed] [Google Scholar]
- 6.Ostbyhaug PO, Klaksvik J, Romundstad P, et al. An in vitro study of the strain distribution in human femora with anatomical and customised femoral stems. J Bone Joint Surg Br 2009;91:676-82 [DOI] [PubMed] [Google Scholar]
- 7.Huiskes R, Weinans H, Dalstra M. Adaptive bone remodeling and biomechanical design considerations for noncemented total hip arthroplasty. Orthopedics 1989;12:1255-67 [DOI] [PubMed] [Google Scholar]
- 8.Decking R, Puhl W, Simon U, et al. Changes in strain distribution of loaded proximal femora caused by different types of cementless femoral stems. Clin Biomech (Bristol Avon) 2006;21:495-501 [DOI] [PubMed] [Google Scholar]
- 9.Lerch M, von der Haar-Tran, Windhagen H, et al. Bone remodelling around the Metha short stem in total hip arthroplasty: a prospective dual-energy X-ray absorptiometry study. Int Orthop 2011;36:533-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Umeda N, Saito M, Sugano N, et al. Correlation between femoral neck version and strain on the femur after insertion of femoral prosthesis. J Orthop Sci 2003;8: 381-6 [DOI] [PubMed] [Google Scholar]
- 11.Waide V, Cristofolini L, Stolk J, et al. Experimental investigation of bone remodelling using composite femurs. Clin Biomech (Bristol Avon) 2003;18:523-36 [DOI] [PubMed] [Google Scholar]
- 12.Fottner A, Schmid M, Birkenmaier C, et al. Biomechanical evaluation of two types of short-stemmed hip prostheses compared to the trust plate prosthesis by three-dimensional measurement of micromotions. Clin Biomech (Bristol Avon) 2009;24:429-34 [DOI] [PubMed] [Google Scholar]
- 13.Ganapathi M, Evans S, Roberts P. Strain pattern following surface replacement of the hip. Proc Inst Mech Eng H 2008;222: 13-8 [DOI] [PubMed] [Google Scholar]
- 14.Hnat WP, Conway JS, Malkani AL, et al. The effect of modular tapered fluted stems on proximal stress shielding in the human femur. J Arthroplasty 2009;24:957-62 [DOI] [PubMed] [Google Scholar]
- 15.Tai CL, Lee MS, Chen WP, et al. Biomechanical comparison of newly designed stemless prosthesis and conventional hip prosthesis - an experimental study. Biomed Mater Eng 2005;15:239-49 [PubMed] [Google Scholar]
- 16.Cristofolini L, Juszczyk M, Taddei F, et al. Stress shielding and stress concentration of contemporary epiphyseal hip prostheses. Proc Inst Mech Eng H 2009;223:27-44 [DOI] [PubMed] [Google Scholar]
- 17.Cristofolini L, Juszczyk M, Taddei F, et al. Strain distribution in the proximal human femoral metaphysis. Proc Inst Mech Eng H. 2009;223:273-88 [DOI] [PubMed] [Google Scholar]
- 18.Cristofolini L, Conti G, Juszczyk M, et al. Structural behaviour and strain distribution of the long bones of the human lower limbs. J Biomech 2010;43:826-35 [DOI] [PubMed] [Google Scholar]
- 19.Gruen TA, McNeice GM, Amstutz HC. Modes of failure of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 1979:17-27 [PubMed] [Google Scholar]
- 20.Cristofolini L, Viceconti M. In vitro stress shielding measurements can be affected by large errors. J Arthroplasty 1999;14:215-9 [DOI] [PubMed] [Google Scholar]
- 21.Bergmann G, Deuretzbacher G, Heller M, et al. Hip contact forces and gait patterns from routine activities. J Biomech 2001; 34:859-71 [DOI] [PubMed] [Google Scholar]
- 22.Hoffmann K. An introduction of measurements using strain gauges. Darmstadt: Hottinger Baldwin McStechnik GmbH; 1989 [Google Scholar]
- 23.Aamodt A, Lund-Larsen J, Eine J, A, et al. Changes in proximal femoral strain after insertion of uncemented standard and customised femoral stems. An experimental study in human femora. J Bone Joint Surg Br 2001;83:921-9 [DOI] [PubMed] [Google Scholar]
- 24.Kim YH, Kim JS, Cho SH. Strain distribution in the proximal human femur. An in vitro comparison in the intact femur and after insertion of reference and experimental femoral stems. J Bone Joint Surg Br 2001;83:295-301 [DOI] [PubMed] [Google Scholar]
- 25.Steinhauser E, Ellenrieder M, Gruber G, et al. [Influence on load transfer of different femoral neck endoprostheses]. Z Orthop Ihre Grenzgeb 2006;144:386-93 [Article in German]. [DOI] [PubMed] [Google Scholar]
- 26.Westphal FM, Bishop N, Honl M, et al. Migration and cyclic motion of a new short-stemmed hip prosthesis—a biomechanical in vitro study. Clin Biomech (Bristol Avon) 2006;21:834-40 [DOI] [PubMed] [Google Scholar]
- 27.Fink B, Wessel S, Deuretzbacher G, et al. Midterm results of thrust plate prosthesis. J Arthroplasty 2007;22:703-10 [DOI] [PubMed] [Google Scholar]
- 28.Ishaque BA, Wienbeck S, Sturz H. [Midterm results and revisions of the thrust plate prosthesis (TPP)]. Z Orthop Ihre Grenzgeb 2004;142:25-32 [Article in German]. [DOI] [PubMed] [Google Scholar]
- 29.Gulow J, Scholz R, Freiherr von Salis-Soglio. [Short-stemmed endoprostheses in total hip arthroplasty]. Orthopade 2007;36:353-9 [Article in German]. [DOI] [PubMed] [Google Scholar]
- 30.Thorey F, Hoefer C, Abdi-Tabari N, et al. Clinical results of the metha short hip stem: a perspective for younger patients? Orthop Rev (Pavia) 2013;5:e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wittenberg RH, Steffen R, Windhagen H, et al. Five-year results of a cementless short-hip-stem prosthesis. Orthop Rev (Pavia) 2013;5:e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Swamy G, Pace A, Quah C, et al. The Bicontact cementless primary total hip arthroplasty: long-term results. Int Orthop 2012;36:915-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ochs U, Eingartner C, Volkmann R, et al. Prospective long-term follow-up of the cementless bicontact hip stem with plasmapore coating. Z Orthop Unfall 2007;145Suppl 1:S3-8 [DOI] [PubMed] [Google Scholar]
- 34.Heiner AD, Brown TD. Structural properties of a new design of composite replicate femurs and tibias. J Biomech 2001; 34:773-81 [DOI] [PubMed] [Google Scholar]


