Abstract
Introduction and hypothesis
The risk for urinary incontinence can be 2.6-fold greater in women after pregnancy and childbirth compared with their never-pregnant counterparts, with the incidence increasing with parity. We tested the hypothesis that the incidence of de novo postpartum urinary incontinence in primiparous women is reduced with the use of spontaneous pushing alone or in combination with perineal massage compared with women who experienced traditional directed pushing for second-stage management.
Methods
This was a prospective clinical trial enrolling and randomizing 249 women into a four-group design: (1) routine care with coached or directed pushing, (2) spontaneous self-directed pushing, (3) prenatal perineal massage initiated in the third trimester, and (4) the combination of spontaneous pushing plus perineal massage. Self-report of incontinence was assessed using analysis of variance (ANOVA) and covariance (ANCOVA) models in 145 remaining women at 12 months postpartum using the Leakage Index, which is sensitive to minor leakage.
Results
No statistical difference in the incidence of de novo postpartum incontinence was found based on method of pushing (spontaneous/directed) (P value=0.57) or in combination with prenatal perineal massage (P value=0.57). Fidelity to pushing treatment of type was assessed and between-groups crossover detected.
Conclusions
Spontaneous pushing did not reduce the incidence of postpartum incontinence experienced by women 1 year after their first birth due to high cross-over between randomization groups.
Keywords: Childbirth, Incontinence, Pelvic floor disorders, Pelvic floor muscle training, Perineal massage, Pregnancy, Second-stage management
Introduction
The risk of urinary incontinence (UI) is 2.0–2.6 fold greater in women after pregnancy and childbirth compared with their never-pregnant counterparts, with the incidence increasing after each child [1]. The National Institutes of Health conference titled “Cesarean Delivery on Maternal Request” [2] cited fear of pelvic floor disorders as a contributor to some women’s desire for elective cesareans. Acknowledging lack of evidence to support elective cesarean as preventative of pelvic floor disorders, the conference report called for identification of modifiable practices during delivery to prevent pelvic floor disorders [2]. A prior investigation indicated that spontaneous compared with directed pushing during second-stage labor was associated with reduced risk of incontinence at 3 months postpartum [3]. Thus, it is reasonable to posit that an intervention encouraging spontaneous pushing may offer an opportunity to reduce risk of incontinence associated with childbirth. Additionally, extensive genital tract trauma (third- and fourth-degree lacerations) is associated with increased risk for pelvic floor damage that may contribute to incontinence [4]. Methods to reduce risk of perineal trauma include avoiding use of episiotomy during childbirth [5]. Use of perineal massage prenatally has also been documented as a preventive measure to reduce genital tract trauma, including use of episiotomy. Thus, use of prenatal perineal massage may provide an additional benefit in preparing for childbirth due to its potential for reducing risk of genital tract trauma [6–8].
The aim of this randomized controlled trial was to test the effect of spontaneous pushing (either with or without prenatal perineal massage) compared with directed pushing on incontinence outcomes in women evaluated 1 year after their first birth. Specifically, we tested the hypothesis that spontaneous pushing with or without prenatal perineal massage lowers de novo persistent postpartum urinary incontinence when compared with routine care (referred to throughout this manuscript as directed pushing) at 12 months postpartum.
Materials and methods
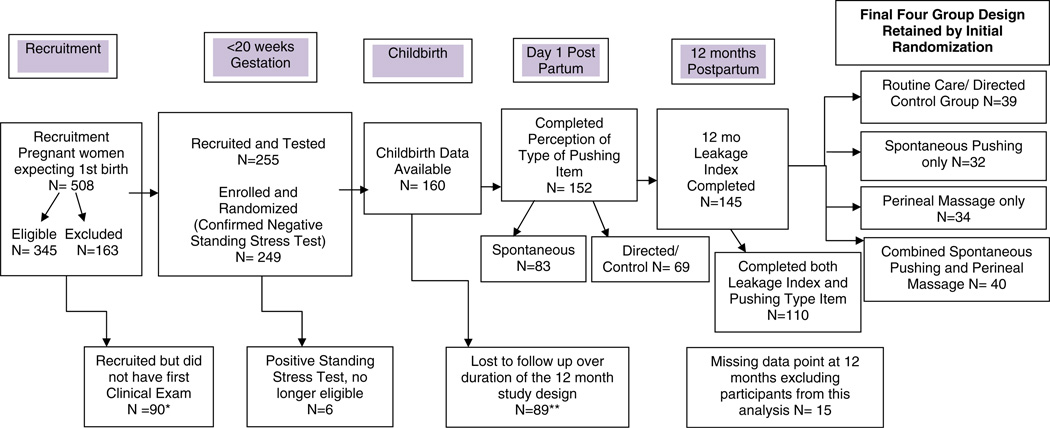
A prospective randomized controlled trial, Promoting Effective Recovery from Labor (PERL), was conducted following Institutional Review Board approval. We recruited pregnant women from prenatal clinics between 2000 and 2006 who were planning to have their first birth at the University of Michigan Women’s Hospital. We posted recruitment posters and encouraged clinic staff in the entire hospital system prenatal clinics to notify women of their potential eligibility for this investigation. Despite providing ongoing staff education and updates about the investigation, the primary mode of recruitment was self-referral based on reading recruitment posters. Figure 1 provides an outline of the study design, group assignment options, recruitment, retention of participants, and final sample size.
Fig. 1.
Study design and sample size with four-group assignment N=145 *Women recruited but who did not participate in first clinical exam or beyond (N=90 total) included those no longer interested/or too busy (N= 31), ill health of participant (N=8), miscarried (N=3), moved (N=7), lost contact (N=20), placenta previa (N=2), assigned ID but not eligible (N=18), not delivering at study hospital (N=1). **Participants lost to follow up after enrollment (N=89 total) included women who miscarried (N=1), moved out of study area (N=9), too busy or no longer interested (N=29), ill health (N=3), lost contact (N=24), became pregnant during in less than 12 months (N=21), not delivering at study hospital (N=1), placenta previa (N=1)
All women who responded to the recruitment materials were screened for enrollment eligibility, which included being able to participate in study follow-up for a year post birth. We screened 508 women for eligibility and identified 345 who were eligible for enrollment. Ninety women who were recruited did not participate in the first clinical exam, which included determination of continence, a requirement for enrollment. Reasons for not enrolling included those no longer interested/or too busy (N=31), ill health (N=8), miscarried (N=3), moved (N=7), lost contact (N=20), placenta previa (N=2), assigned ID but not eligible (N=18), and not delivering at the study hospital (N=1).
We enrolled 249 women who met the recruitment criteria: at least 18 years of age, no history of genitourinary pathology, continent during first 20 weeks of pregnancy by self-report, and continent at 20 weeks’ gestation by negative standing stress test. To confirm exclusion criteria, a standing stress test was performed at the baseline visit by lightly placing a paper towel against the perineum to capture any urine loss during hard coughing and/or Valsalva [9]. To ensure the test was performed with adequate fluid volume in the bladder, women were asked to drink one to two glasses of water an hour before the appointment and refrain from voiding until testing. Full bladder was again confirmed by self-report of felt readiness to void immediately before the test, and voided volume of at least 100 cc immediately after the test. As we were interested in de novo incontinence, women with demonstrable stress incontinence were excluded. Women with a dry standing stress test continued in the study [9]. At this visit, women also had to demonstrate ability to contract the pelvic floor muscles voluntarily as assessed by manual examination.
Upon confirmation of eligibility and informed consent, participants were randomly assigned to one of four groups:
Directed pushing, or coached pushing using a closed glottis Valsalva maneuver, which was routine care provided at the recruitment hospital.
Spontaneous pushing, with instruction provided prenatally via a standardized training video. This method included instructing the woman to follow her bodily sensations and push as she felt the urge.
Prenatal perineal massage initiated in the third trimester with a standardized training regarding its use and then directed pushing during second-stage labor.
Combination of group 2 and 3 treatment, with spontaneous pushing plus perineal massage.
Randomization was determined by a computer-generated table. Care providers were informed of their patients’ group assignment. The study team provided presentations to both the nursing and obstetrical staff regarding the study focus on pushing methods, including pushing types. Thus, neither the participants nor their providers were blinded to the group assignment. The nurse practitioner conducting all clinical assessments and collecting self-reports was blinded to the group assignment. Clinical visits were conducted at four time-points: 20 weeks’ gestation and at 6 weeks, 6 months and 12 months postpartum. We limit this report to the primary research question of incontinence outcomes at 1 year postpartum.
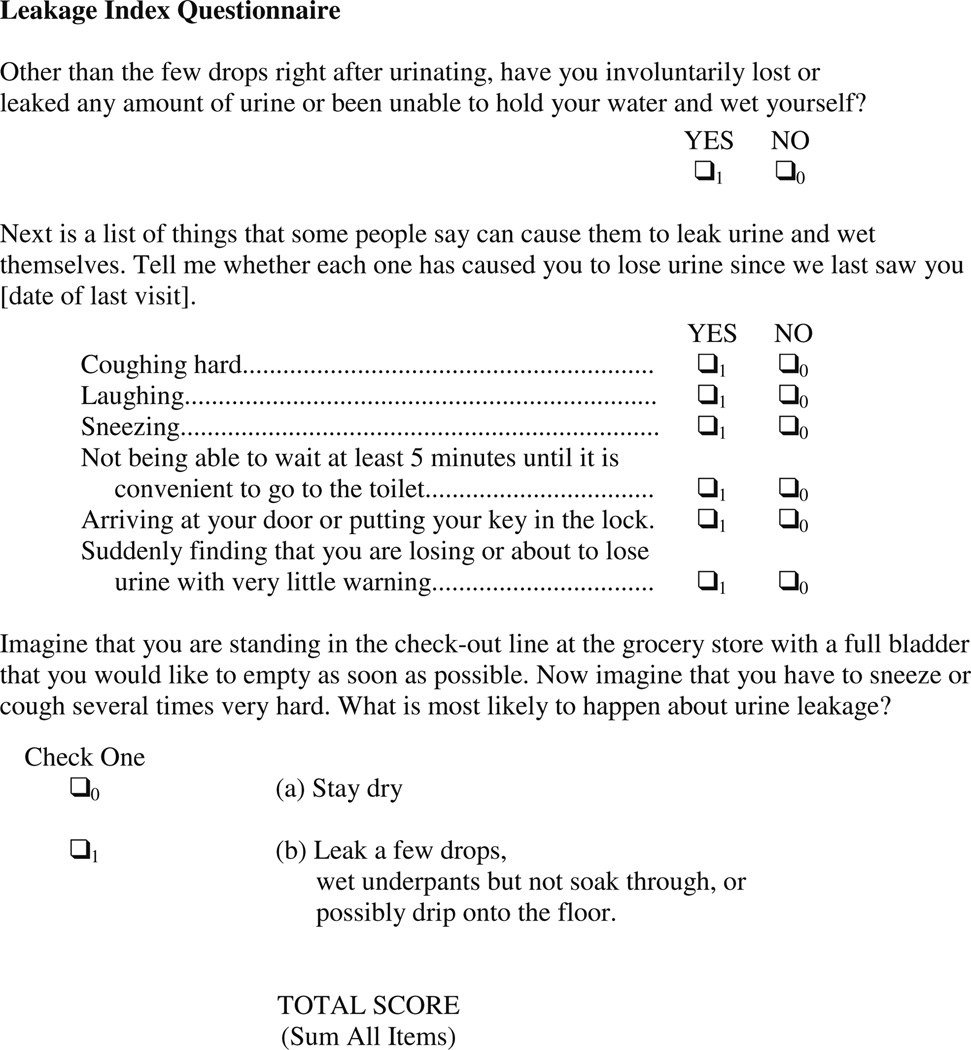
The main outcome variable was measured by the Leakage Index questionnaire [10] developed in a similar large sample of pregnant, previously continent, women studied throughout the first year after delivery. This questionnaire is presented in Fig. 2 and was selected because of its high sensitivity to small-volume and low-frequency incontinence, which is common in this healthy, low-risk pregnant and postpartum population. Potential index scores range from 0 to 8, with larger numbers indicating greater severity of incontinence.
Fig. 2.
Leakage index
All women who were enrolled in the project, regardless of group assignment, received standardized pelvic floor muscle training education. Each woman received instruction in pelvic muscle contraction at her visits and was assigned to an appropriate level of exercise using the Graduated Strength Training Protocol [11]. Pelvic floor muscle training was reinforced through written educational materials and encouragement to keep track of adherence to the exercise routine at home. Thus, all women in the study were educated in pelvic muscle training, with reinforcement instruction at each visit throughout the study.
If the group assignment included use of perineal massage, women were instructed to begin a daily regimen of perineal massage at 34 weeks gestation. The method included self or partner placing fingers/thumbs 1–2 cm into the vagina and pressing downward and outward with a release of pressure when discomfort was felt and repeating for 5–10 min [6]. Women were provided with a diary to record the number of times they completed the perineal massage process as a strategy for motivation. Very few women turned in the diaries, and of those who did, none performed perineal massage at the daily use levels of the technique as instructed. Those in the spontaneous pushing groups received a video that provided instructional information on the technique.
Upon admission to labor, the woman informed the hospital staff that she was a participant in the PERL project; this status was also indicated on her prenatal record. The provider, who was an obstetrician, certified nurse midwife, or family medicine physician, was informed of group assignment in each case, as were the obstetric nurses. Upon entry into second-stage labor, depending on group assignment, care providers were asked to proceed with traditional, standard management of second stage or abide by spontaneous pushing style, allowing the woman to follow her body sensations as per her training from the video. In the spontaneous pushing group, directions given to the woman in any form regarding her pushing position, length of pushing, or how to hold her breath were discouraged. Statements such as “you are so strong” or “good work” were considered supportive, not directive, and were allowed.
As a validity check for the method of pushing actually performed, women were asked to complete a questionnaire immediately postpartum (in an attempt to minimize recall bias) that assessed their perception of the type of pushing method they used. The questionnaire included a summary item asking them to quantify the amount of time they spent in spontaneous pushing compared with directed pushing on a scale of 0–100 %.
In our intention to treat model, women were retained in their assigned group for analysis. With the exception of three women who had a prelabor cesarean delivery due to a diagnosis of placenta previa, all women experienced a trial of labor, so none were excluded for having a cesarean birth. Descriptive analyses were first applied to compare baseline differences in patient demographic and obstetric characteristics between the four treatment groups. Specifically, for continuous variables, we used the one-way analysis of variance (ANOVA) for comparison between three or more groups with normal distribution and the Kruskall–Wallis test for skewed or semicontinuous distribution. For categorical variables, we used the chi-square or Fisher’s exact test, wherever appropriate. Data of participants who withdrew from the study prior to the 12 months’ follow-up were censored. Statistical analyses included the calculation of proportions for categorical variables and standard deviations (SD) for continuous variables. A two-way ANOVA model was employed to study treatment effects (spontaneous pushing and perineal massage) on the primary outcome variable: change in Leakage Index scores from the untreated baseline to the final visit (12 months postpartum). The ANOVA model contained two main factors: factor A, whether spontaneous pushing affects change in Leakage Index scores, and factor B, whether perineal massage affects change in Leakage Index scores. An interaction term of factor A (spontaneous pushing) with factor B (perineal massage) was included to investigate whether the effect of one treatment (spontaneous pushing) was modified by whether the women received the other treatment (perineal massage) simultaneously. If there was no significant interaction effect detected, an ANOVA model with the main effect only was fitted and presented. Furthermore, an analysis of covariance (ANCOVA) was used to assess treatment effects, adjusted for age, body mass index (BMI), race, education, income, and baseline Leakage Index scores.
All the statistical tests were two-tailed, and p<.05 was considered statistically significant in all analyses. Analyses were performed using SAS 9.2 statistical software package.
Results
Initial demographics of the 249 nulliparous women were consistent with the recruitment-site county demographics (Fig. 1). Mean (±SD) age was 29.7 years (±5.0), with 82.7 % being Caucasian and 17.3 % being non-Caucasian. BMI mean at enrollment at 20 weeks gestation was 24.6 (± 5.7), with all being nulliparous, although 14.7 % had experienced a prior pregnancy that did not progress beyond 20 weeks. No statistically significant differences were detected for participants’ baseline demographic or obstetric characteristics among the four groups. Only participants who had complete information on both baseline and the 12-month follow-up visit were included in the final analysis (145, representing a 41 % attrition rate). There were no significant differences detected between the remaining sample and those lost to follow-up with respect to baseline characteristics namely age, height/weight, race/ethnicity, or baseline Leakage Index score. Thus, missing completely at random seemed to be a reasonable assumption when handling those lost to follow up or missing data. Detailed demographics for the final sample are provided in Table 1. Table 2 shows that there was no significant difference by group in variables that might be considered adverse events, that is, number with epidurals, longer length of second stage, or number who delivered by cesarean.
Table 1.
Demographics of participants at 12 months postpartum (N=145)*
| Variable | ||
|---|---|---|
| Continuous variables | Mean ± SD | No. |
| Age | 30.07±4.57 | 145 |
| Weight (pounds) | 148.75±32.72 | 143 |
| Height (inches) | 65.42±3.00 | 143 |
| Body mass index | 24.71±5.77 | 145 |
| Categorical variables | Frequency | No. |
| Race | 148 | |
| Caucasian | 126 (85.14 %) | |
| non-Caucasian | 22 (14.86 %) | |
| Education | 144 | |
| Elementary/secondary | 2 (1.39 %) | |
| College | 74 (51.39 %) | |
| Graduate school | 68 (47.22 %) | |
| Income | 144 | |
| <$20,000/year | 8 (5.56 %) | |
| $20,000–40,999/year | 17 (11.81 %) | |
| $41,000–60,000/year | 22 (15.28 %) | |
| >$60,000/year | 97 (67.36 %) |
The sample size varies due to missing data points for some of the demographics reported
Table 2.
Obstetric characteristics by treatment condition (N=145)
| Assigned treatment condition | |||||
|---|---|---|---|---|---|
| Directed pushing (N=39) |
Perineal massage (N=32) |
Spontaneous pushing (N=34) |
Spontaneous pushing and perineal massage (N=40) |
P value | |
| Epidural | 0.44 | ||||
| Yes | 21 (58.33 %) | 20 (60.61 %) | 21 (60.00 %) | 29 (74.36 %) | |
| No | 15 (41.67 %) | 13 (39.39 %) | 14 (40.00 %) | 10 (25.64 %) | |
| Second-stage length (minutes) | 131.12±91.08 | 130.28±126.67 | 151.69±133.26 | 104.19±88.08 | 0.47 |
| Delivery method | 0.25 | ||||
| Vaginal | 31 (86.11 %) | 27 (81.82 %) | 24 (68.57 %) | 28 (71.79 %) | |
| Cesarean section | 5 (13.89 %) | 6 (18.18 %) | 11 (31.43 %) | 11 (28.21 %) | |
Two-way ANOVA for the interaction effect of spontaneous pushing with perineal massage on postpartum incontinence was not statistically significant (P value=0.33). The ANOVA model was repeated to see if postpartum incontinence was affected by pushing type, and no significant difference on postpartum incontinence was observed by pushing type (P value=0.57) or massage type (P value=0.57) (Table 3).
Table 3.
Comparison of change in urine leakage between baseline and 12 months postpartum in patients randomized to the four treatment groups (N=145)
| Assigned treatment condition | |||||
|---|---|---|---|---|---|
| Directed pushing (N=39) |
Perineal massage (N=32) |
Spontaneous pushing (N=34) |
Spontaneous pushing and perineal massage (N=40) |
P value | |
| Leakage Index | |||||
| Baseline | 1.27±1.87 | 0.97±1.85 | 0.88±1.25 | 1.15±1.61 | |
| 12 months | 2.17±2.5 | 0.97±1.65 | 1.20±1.76 | 1.41±2.01 | |
| Change (final, baseline) | 0.84±1.94 | 0 | 0.35±1.95 | 0.13±1.55 | 0.57 |
Mean scores are reported ± standard error of the mean
To adjust for possible bias, we evaluated the treatment effects by applying an ANCOVA model, which contained factors of treatments (spontaneous pushing, perineal massage), age, BMI, race, education, income, and baseline Leakage Index scores. The absence of treatment effect found in the original two-way ANOVA model remained. Verification of fidelity to the treatment group assignment was included in the assessment measures. Among 252 women originally enrolled in the parent study, a total of 152 completed questionnaires in the early postpartum period documenting self-perception of their pushing type used during labor, independent of their group assignment. Given the high intensity of this early time after birth and the often heavy family needs, many women did not complete the questionnaire in this timeframe.
Consistent with other investigations, >50 % use of one method was used as a cut point to classify the method of pushing as being either spontaneous or directed [12]. Of 152 women with the pushing questionnaire completed, 83 (54.6 %) self-reported using spontaneous pushing while 69 (45.4 %) self-reported using directed pushing (Table 4). However, in those whose original assignment was spontaneous pushing, 23.6 % self-reported using directed pushing, whereas 35 % of those assigned to directed pushing actually reported using spontaneous pushing instead. Thus, a reanalysis comparing the actual pushing group as perceived by the women to the outcome of Leakage Index score was also completed. Among the 152 women whose reports of perceived pushing type were obtained early postpartum, 110 had 12-month follow-up data available (compared with the 145 available for the intention to treat analysis). The treatment group using spontaneous pushing compared with the control group using directed pushing methods did not differ significantly in their demographics or obstetric characteristics. Repeating the same analysis as was used in the intention to treat model, but with the smaller sample size of 110, the ANOVA analysis using the actual method of pushing for the group assignment and the change of Leakage Index score did not significantly differ (0.69±1.81 vs. 0.37±1.76, P value=0.36).
Table 4.
Descriptive comparison of original group assignment and women’s perception of actual pushing method used during labor (N=152)
| Pushing type |
Postpartum woman’s perception | |||
|---|---|---|---|---|
| Directed | Spontaneous | Total | ||
| Original | Spontaneous | 17 | 55 | 72 (47.4 %) |
| Group | Directed | 52 | 28 | 80 (52.6 %) |
| Assignment | Total | 69 (45.4 %) | 83 (54.6 %) | |
Discussion
The outcome of our clinical trial testing the effect of using spontaneous pushing with or without perineal massage and perineal massage alone did not demonstrate a positive effect on reducing postpartum urinary leakage. The findings of this randomized controlled trial differ from a prior investigation that found some reduction in the incidence of postpartum incontinence with spontaneous pushing [3]. An earlier randomized controlled trial (n=128) found postpartum urodynamic measures were poorer in women who were coached during second-stage labor pushing versus those not coached, but only limited urodynamic outcomes were assessed, including time to first void and bladder capacity [3]. Another trial that randomized 320 nulliparous women into coached versus uncoached pushing found that second-stage labors were shorter by an average of 13 min in the spontaneous pushing group but failed to identify any differences in maternal or neonatal outcomes, including incidence of incontinence [13].
Longer duration of second-stage labor has been cited as a risk factor for pelvic floor damage; therefore, methods of pushing that may increase duration of second-stage should be evaluated for their impact on urodynamic outcomes postpartum. In a meta-analysis of investigations comparing spontaneous to Valsalva pushing, second-stage labor duration differed significantly, with Valsalva pushing being 18 min shorter than spontaneous pushing [14]. When one investigation was eliminated that had extremes in duration, the difference was ≪10 min [14]. Despite this difference in duration, urodynamic clinical outcome measures were not consistently applied across studies. Our own study shows high variance in length of second-stage labor in each of the study groups, with no statistically significant difference between groups.
In a secondary analysis of a randomized clinical trial comparing spontaneous to directed Valsalva pushing conducted by Wai [15] of the 320 women in the original trial, multichannel urodynamic testing was conducted with 128 women who returned at 3 months postpartum their first vaginal birth. The analysis reported was an aggregate of outcomes instead of comparing women by their randomized group assignment by pushing type. They also experienced large participant attrition, which may have contributed to not comparing groups but instead reporting on the aggregate findings of incidence of urodynamic changes overall. Other studies using various pushing methods and urodynamic indices have either focused solely on women without epidurals [13]; were underpowered or had research design flaws barring conclusions [16]; or did not include pelvic floor outcomes beyond use of episiotomy for women with epidurals [17, 18]. These limitations impede understanding the implications of using varied pushing strategies and also have inconsistent results.
Another limitation in many trials is lack of confirming fidelity to randomization group. This investigation found crossover common between randomized group assignments in both directions. Another trial of 350 women randomized to spontaneous versus directed pushing reported the majority of women found it difficult to comply with their assigned pushing technique [19]; only 34 % of women in the spontaneous group used the assigned technique for more than half of second stage. The high crossover rates in those investigations and the one reported here limit definitive conclusions for incontinence outcomes based on pushing type. Prior investigations excluded women with epidurals [13], whereas this trial included women with epidurals, possibly contributing to the crossover groups and to the absence of treatment effect in this investigation.
It is also possible that the crossover effect between group assignments more realistically reflects the clinical realities of management of second-stage labor. Clinically, pushing throughout second stage is dynamic and may include variations in methods based on progress being made or not, maternal fatigue, use of an epidural, fetal presentation, and bedside provider preferences. Unlike other studies, this investigation used multiple providers of multiple types (nurse midwives, family medicine, and obstetricians), limiting the ability to control or limit provider behavior, which may have influenced the pushing method actually used during labor despite the standardized instruction provided to each woman by video. These factors combined may have contributed to lack of treatment findings in this investigation. Future investigations may consider employing more reliable assessments of pushing methods used by women during second stage, such as having an observer present to document pushing method or capturing the events of second stage by video or audio recording. This approach would allow for a more accurate quantification process of pushing type; however, each of these strategies may limit women’s desire for participation.
Another possible limiting factor was the 41 % attrition rate in our prospective study, resulting in a small sample size. This rate of attrition, although relatively large, is consistent with studies using a similar age group and time span of data collection [15, 20] and considering the difficulties in general of studying women with multiple visits during their first childbearing year. Importantly, the groups did not differ demographically between those retained and those lost to follow-up. However the smaller sample sizes in prospective clinical trials evaluating urodynamic changes conducted during the childbearing year have been limited by small sample sizes over time. Our investigation is one of the first to attempt an even longer time-frame clinical evaluation of postpartum urodynamic changes to the 1-year mark. Methods to address the challenges of sample attrition included use of newsletters to engage participants between visits, phone confirmation of appointments to maintain direct contact, project branding to encourage provider awareness of the project for referrals and follow-up, and reminder mailings to women about the planned visits. With these concerted efforts to retain participants, our primary analysis was conducted with 145 women.
When the final analysis was conducted using the validity check for pushing method, our sample size was 110. Power analysis was conducted with PASS software [21] to determine the power of analyses using this final sample size to detect what Cohen [22] defined as a medium-sized effect on mean scores on the Leakage Index using ANOVA or t test analysis with alpha of 0.05 two tailed. Cohen defined a medium-sized effect on the mean as a difference of 0.5 times the SD of the score and described it as visible to the naked eye (thus clinically significant). Power analysis for this sized effect indicated a power of 73.8 % with this sample size. Although this is a bit lower than ideal, it is quite sufficient.
A positive outcome from this investigation aimed primarily at prevention is that no increased risk was evident in the intervention groups, as judged by epidural rates, cesarean rates, and length of second stage for the use of spontaneous pushing with or without prenatal perineal massage. Thus, continued use of these interventions can be safely implemented. Strengths of the investigation are longer follow-up postpartum, which allows for recovery from transient early postpartum incontinence, and the use of a sensitive measure for assessing even rare-occurrence leakage. Finally, inclusion of an early postpartum fidelity check prospectively in the study design was important in considering alternative explanations for unexpected outcomes.
We conclude that neither spontaneous pushing nor prenatal perineal massage on their own were shown to reduce birth-related de novo incontinence at 12 months postpartum, though neither proved to be contraindicated and can be safely retained as the preferred method for pushing for positive outcomes beyond continence status. How much time a woman uses one method of pushing compared with another during the process of a dynamic second stage requires further investigation to determine if there is a potential dose response associated with specific outcomes. Evaluation of other second-stage management strategies potentially alterable in a manner that is protective of the pelvic floor is also warranted to measure the changes associated with incontinence following childbirth for otherwise healthy women. This may include exploring the manner in which perineal stretch is managed to reduce risk for genitaltract trauma. Increasing use of epidurals is a feature of second-stage labor management and includes use of Foley or straight catheters to manage bladder volume. The effect of these contemporary maternity-care practices also warrants consideration as further investigations of risk of incontinence and vaginal birth are explored. A key finding from this investigation is that inclusion of an evaluation of fidelity to group assignment in trials of second-stage management is crucial when testing interventions that must take place within the complex environment of labor and delivery.
Acknowledgements
We gratefully acknowledge funding for the PERL Project: Urinary Incontinence Prevention: Reducing Birthing Risk (R01-NR4007) by the National Institute of Nursing Research and additional investigator support from the National Institute of Health through the Office of Research on Women’s Health SCOR on Sex and Gender Factors Affecting Women’s Health (P50 HD 44406).
Footnotes
Conflicts of interest None.
Disclosures John O.L. DeLancey: Kimberly Clark, Johnson and Johnson, American Medical Systems
Contributor Information
Lisa Kane Low, Email: kanelow@umich.edu, School of Nursing and Department of Women’s Studies, University of Michigan, 400 North Ingalls Suite 3320, Ann Arbor, MI 48109, USA.
Janis M. Miller, School of Nursing and Department of Obstetrics and Gynecology, University of Michigan, 400 North Ingalls Suite 3320, Ann Arbor, MI 48109, USA
Ying Guo, School of Public Health, University of Michigan, 1415 Washington Heights, Ann Arbor, MI 48109, USA.
James A. Ashton-Miller, Mechanical Engineering and Biomedical Engineering, College of Engineering, University of Michigan, 2350 Hayward Street, Ann Arbor, MI 48109, USA
John O. L. DeLancey, Department of Obstetrics and Gynecology, School of Medicine, University of Michigan, 1500 East Medical Center Dr. F4200, Ann Arbor, MI 48109, USA
Carolyn M. Sampselle, School of Nursing, University of Michigan, 400 North Ingalls Suite 3320, Ann Arbor, MI 48109, USA
References
- 1.Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. Br J Urol Int. 2008;101:1388–1395. doi: 10.1111/j.1464-410X.2008.07601.x. [DOI] [PubMed] [Google Scholar]
- 2.National Institutes of Health. State of the Science Conference Report: Cesarean Delivery on Maternal Request. [Accessed 15 July 2012];2006 Mar 27–29; http://consensus.nih.gov/2006/cesareanstatement.htm.
- 3.Schaffer JI, Bloom SL, Casey BM, McIntire DD, Nihira MA, Leveno KJ. A randomized trial of the effects of coached vs. uncoached maternal pushing during the second stage of labor on postpartum pelvic floor structure and function. Am J Obstet Gynecol. 2005;192(5):1692–1696. doi: 10.1016/j.ajog.2004.11.043. [DOI] [PubMed] [Google Scholar]
- 4.Kearney R, Miller J, Ashton Miller J, DeLancey JO. Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol. 2006;107(1):144–148. doi: 10.1097/01.AOG.0000194063.63206.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Viswanathan M, Hartmann K, Palmieri R, et al. Evidence reports/technology assessments. No. 112. Rockville, MD: Agency for Healthcare Research and Quality; 2005. The use of episiotomy in obstetrical care: a systematic review. 2005. [PMC free article] [PubMed] [Google Scholar]
- 6.Avery MD, Van Arsdale L. Perineal massage: effect on incidence of episiotomy and lacerations in a nulliparous population. J Nurse Midwifery. 1987;32(3):128–134. doi: 10.1016/0091-2182(87)90095-4. [DOI] [PubMed] [Google Scholar]
- 7.Hinz B. Perineal massage in pregnancy. J Midwifery Womens Health. 2005;50(1):63–64. doi: 10.1016/j.jmwh.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 8.Aasheim V, Nilsen ABV, Lukasse M, Reinar LM. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev. 2011;12:CD006672. doi: 10.1002/14651858.CD006672.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller JM, Ashton-Miller JA, DeLancey JOL. Quantification of cough-related urine loss using the paper towel test. Obstet Gynecol. 1998;91(5):705–709. doi: 10.1016/s0029-7844(98)00045-3. [DOI] [PubMed] [Google Scholar]
- 10.Antonakos CL, Miller JM, Sampselle CM. Indices for studying urinary incontinence and levator ani function in primiparous women. J Clin Nursing. 2003;12:1–8. doi: 10.1046/j.1365-2702.2003.00747.x. [DOI] [PubMed] [Google Scholar]
- 11.Miller J, Kasper C, Sampselle C. Review of muscle physiology with application to pelvic muscle exercise. Urol Nurs. 1994;14(3):92–97. PMID 8826155. [PubMed] [Google Scholar]
- 12.Sampselle CM, Miller JM, Luecha Y, Fischer K, Rosten L. Provider support of spontaneous pushing during second stage labor. J Obstet Gynecol Neonatal Nurs. 2005;34(6):695–702. doi: 10.1177/0884217505281904. [DOI] [PubMed] [Google Scholar]
- 13.Bloom SL, Casey BM, Schaffer JI, McIntire DD, Leveno KJ. A randomized trial of coached versus uncoached maternal pushing during the second stage of labor. Am J Obstet Gynecol. 2006;194:10–13. doi: 10.1016/j.ajog.2005.06.022. [DOI] [PubMed] [Google Scholar]
- 14.Prins M, Boxem J, Lucas C, Hutton E. Effect of spontaneous pushing versus Valsalva pushing in the second stage of labour on mother and fetus: a systematic review of randomised trials. Br J Obstet Gynecol. 2011;118(6):662–670. doi: 10.1111/j.1471-0528.2011.02910.x. [DOI] [PubMed] [Google Scholar]
- 15.Wai C, Antip S, Bloom S. Urodynamic indices and pelvic organ prolapse quantification 3 months after vaginal delivery in primiparous women. postpartum. Int Urogynecol J. 2011;22:1293–1298. doi: 10.1007/s00192-011-1438-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fitzpatrick M, Harkin R, McQuillan K, O’Brien C, O’Connell PR, O’Herlihy C. A randomised clinical trial comparing the effects of delayed versus immediate pushing with epidural analgesia on mode of delivery and fecal continence. Int J Obstet Gynecol (BJOG) 2002;109(12):1359–1365. doi: 10.1046/j.1471-0528.2002.02109.x. [DOI] [PubMed] [Google Scholar]
- 17.Fraser WD, Marcoux S, Krauss I, Douglas J, Goublet C, Boulvain M. Multicenter, randomized, controlled trial of delayed pushing for nulliparous women in the second stage of labor with continuous epidural analgesia. Am J Obstet Gynecol. 2000;182(5):1165–1172. doi: 10.1067/mob.2000.105197. [DOI] [PubMed] [Google Scholar]
- 18.Simpson KR, James DC. Effects of immediate versus delayed pushing during 2nd-stage labor on fetal well-being: a randomized controlled trial. Nurs Res. 2005;54(3):149–157. doi: 10.1097/00006199-200505000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Parnell C, Langhoff-Roos J, Iversen R, Damgaard P. Pushing method in the expulsive phase of labor: a randomized trial. Acta Obstet Gynecol Scand. 1993;72:31–35. doi: 10.3109/00016349309013345. [DOI] [PubMed] [Google Scholar]
- 20.Woldringh C, van den Wijngaart M, Albers-Heitner P, Lycklama a Nijeholt AA, Lagro-Janssen T. Pelvic floor muscle training is not effective in women with UI in pregnancy: a randomized controlled trial. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(4):383–390. doi: 10.1007/s00192-006-0175-x. [DOI] [PubMed] [Google Scholar]
- 21.Hintze JL. Number Cruncher Statistical Software. Kaysville, Utah: 2008. PASS 2008 User’s Guide. [Google Scholar]
- 22.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]