Abstract
INTRODUCTION
Inguinal hernia containing bladder carcinoma is a very rare occurrence.
PRESENTATION OF CASE
We report a case of a male patient who presented with a left groin hernia containing an irregular mass. The hernia was repaired without the use of mesh and a partial cystectomy was done.
DISCUSSION
Only 1–3% of all inguinal hernias involve the bladder, with very few reports containing a carcinoma.
CONCLUSION
Treatment consists of removing the tumor and repairing the hernia.
Keywords: Inguinal hernia, Bladder carcinoma
1. Introduction
Minor bladder shift plus inguinal hernia is a relatively rare condition that occurs in only 1–3% of hernias and up to 10% of men over 50 years of age.1 Tumors in inguinal hernias are unusual. Only 22 cases of neoplasm arising within a vesical hernia are cited in published reports. We present a case of a papillary urothelial bladder carcinoma in a direct inguinal hernia.
2. Presentation of case
A 79-year-old man presented to our department with a swelling in the left groin evolving over 10 years without any symptoms. He had undergone right inguinal herniorrhaphy 53 years ago. The patient was operated using the transurethral resection of bladder tumor (TUR-BT) technique 3 months before due to papillary urothelial carcinoma of the prostatic part of the urethra. The physical examination revealed a large painless mass in the left groin. The ultrasound examination was inconclusive showing only a left inguinal hernia while the intravenous pyelography revealed an abnormal position of the urinary bladder. The computed tomography (CT) (Fig. 1) showed a left groin hernia with an irregular mass content which grows from the urinary bladder (probably tumor of the bladder wall). The patient underwent open surgery via an inguinal approach; the tumor was palpated in the herniated portion of the bladder (Fig. 2). A partial cystectomy was done and the inguinal hernia was repaired without the use of mesh. Pathologic examination of the specimen reported a tumor of 8 cm × 5 cm × 5 cm (Fig. 3). The microscopic study (Fig. 4) revealed a high-grade carcinoma with necrosis and characteristics of a papillary urothelial carcinoma with invasion of 1/3 of the muscularis propria (T2a). The postoperative period was uneventful. One year after the operation the patient presented no recurrence of the tumor or hernia.
Fig. 1.
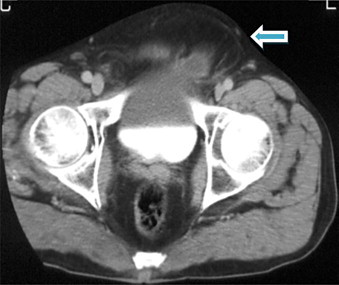
Preoperative CT left groin hernia with an irregular mass content which grows from the urinary bladder.
Fig. 2.
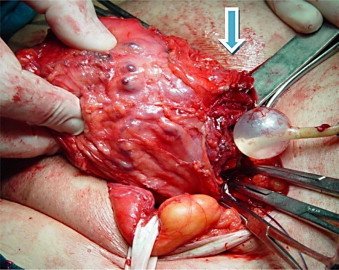
Direct inguinal hernia containing part of the urinary bladder.
Fig. 3.
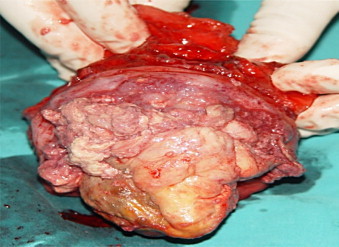
Tumor of the urinary bladder wall 8 cm × 5 cm × 5 cm.
Fig. 4.
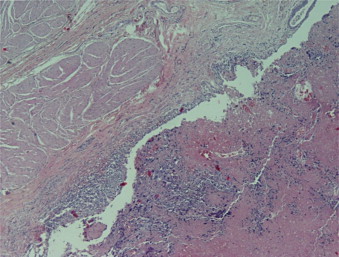
Papillary urothelial carcinoma with invasion of 1/3 of muscularis mucosa (T2a).
3. Discussion
Various studies have reported that 1–3% of all inguinal hernias involve the bladder. Some researchers have estimated the prevalence may be closer to 10% in men.1
According to the relationship with the peritoneum, the hernias are classified as follows: (a) paraperitoneal, which are common (60%) in which the peritoneum covers the external aspect of the herniated bladder, can be direct or indirect, as it was in our case; (b) extraperitoneal, in which the tumors do not cover the peritoneum and are usually small; and intraperitoneal, in which the peritoneum covers the entire portion of herniated bladder.2,3
The most common etiologies of bladder hernias are: obesity, weakness of the pelvic wall, bladder outlet obstruction, and decreased tone of the bladder. In our case the patient had a history of hernia repair 53 years ago, however, whether a history of herniorrhaphy affects the occurrence of bladder hernia is uncertain.4,5
Bladder hernias are usually asymptomatic but are often associated with intermittent swelling in the groin and significant lower urinary tract symptoms. In cases of large hernias the patients typically present with two-stage micturition, involving spontaneous bladder emptying with a second stage manual compression of the hernia.6
The differential diagnosis includes: bladder diverticulum, hernia of a mesenteric cyst, hydrocele and spermatic cord cyst.
The radiological diagnosis can be established by cystography, ultrasonography, and intravenous pyelography or computed tomography.1
The numbers of cases of hernia which contain a tumor of the urinary bladder being published are low (Table 1).
Table 1.
Cases with tumor in the herniated bladder (literature review).
| Author | Year | Number of patients |
|---|---|---|
| Epner SL, et al. | 1993 | 1 |
| Rubio Barbon S, et al. | 1995 | 1 |
| Pardo Garcia JL, et al. | 1997 | 1 |
| Dario Casas J, et al. | 1997 | 1 |
| Pareira Arias, et al. | 1998 | 1 |
| Caterino M, et al. | 2001 | 1 |
| Oruc MT, et al. | 2004 | 14 |
| Das CJ, et al. | 2007 | 1 |
| Pastor Navarro H, et al. | 2010 | 1 |
| Total | 22 | |
The purpose of treatment is to remove the tumor, repair the hernia and correct the obstructive condition of any lower urinary tract. The patient survival is low due to the delay and difficulty in obtaining an accurate diagnosis. Despite the overall poor prognosis the outcome depends on the histologic type and stage regardless of the diagnostic delay.7
4. Conclusion
Inguinal bladder hernias are relatively uncommon, with few (22) reports of tumor in the herniated bladder have been published in the international literature (Medline/Pubmed). The surgical management consists of removing the herniated bladder tissue containing the tumor with a marginal of safety, and repairing the hernia, with careful urological follow up.
Conflict of interest
The authors report no conflict of interest.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient of the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal of request.
Author contributions
Anastasios Katsourakis participated in the design of the study and drafted the manuscript; George Noussios participated in the coordination and helped to draft the manuscript; Christos Svoronos performed the literature review; Michael Alatsakis helped to draft the manuscript; Efthimios Chatzitheoklitos participated in the coordination.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.Epner S.L., Rozenblit A., Gentile R. Direct inguinal hernia containing bladder carcinoma: CT demonstration. Am J Roentgenol. 1993;161:97–98. doi: 10.2214/ajr.161.1.8517332. [DOI] [PubMed] [Google Scholar]
- 2.Escudero J.U., De Campos M.R., Dominguez F.O. Hernias vesicales inguinoescrotales. Arch Esp Urol. 2007;60:231–236. doi: 10.4321/s0004-06142007000300002. [DOI] [PubMed] [Google Scholar]
- 3.Sanchez C., Olmedo E.J., Murillo S.R. Hernia vesical inguinoescrotal gigante, Caso clinico y revision de la literatura. Actas Urol Esp. 2001;25:315–319. doi: 10.1016/s0210-4806(01)72623-x. [DOI] [PubMed] [Google Scholar]
- 4.Bisharat M., Donnell M.E., Thomson T. Complications of iguinoscrotal bladder hernias: a case series. Hernia. 2009;13:81–84. doi: 10.1007/s10029-008-0389-6. [DOI] [PubMed] [Google Scholar]
- 5.Kim K.H., Lee S.W., Hur D.S. Massive inguinal bladder hernia into the scrotum. Korean J Urol. 2001;42:1011–1012. [Google Scholar]
- 6.Kraft K.H., Sweenney S., Fink A.S. Inguinoscrotal bladder hernias: report of a series and review of the literature. Can Urol Assoc J. 2008;2:619–623. doi: 10.5489/cuaj.980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Navarro H.P., Ruiz J.M., Lopez P.C. Tumor inside an iguinoscrotal bladder hernia. Arch Esp Urol. 2010;63:471–476. [PubMed] [Google Scholar]


