Abstract
Clinical trials are emerging as an important activity in India as it is an essential component of the drug discovery and development program to which India is committed. The only robust way to evaluate a new medicine is by doing properly designed clinical trials. In addition to advancing science, clinical trials offer myriad benefits to the participants. The recent hue that created in India about clinical trials is probably an exaggeration of facts. However, these points to the need for ensuring proper compliance with the regulatory norms and proper training of concerned personnel in good clinical practice (GCP). This will ensure that India continues to reap the benefits of clinical trials and also become a world leader in this field.
Keywords: Clinical trials, good clinical practice, India
INTRODUCTION
India is fast emerging as one of the global hubs for conducting clinical trials. This is due to the so called “India Advantage” which includes availability of large numbers of patients, highly motivated and skilled medical and paramedical personnel, state of the art hospitals and strong information technology (IT) support. Over the years, increasing numbers of pharmaceutical companies and clinical research organizations (CROs) are approaching doctors and medical institutions with requests to conduct clinical trials in India. It is therefore important that clinicians who are the principal investigators in these trials are fully conversant with all aspects of conducting clinical trials.
Primary issue of the need for clinical trials in India
The robust way to evaluate a new medicine is mainly by means of clinical trials and that is why clinical trials need to be done. We may think why clinical trials are needed when there are so many current medicines available: It is because to allow the patients access to better medicines in the future. Scientists and doctors the world over continue the search to understand which treatments are safer and better for their patients. When a patient is enrolled by a doctor in the clinical trials that means he needs the patient's collaboration in an experiment to understand the new medicine.[1]
An attractive destination for conducting clinical trials in recent years is India. India offers rapid completion and reduced cost to the sponsors from Canada, Europe and US. Our standards to conduct trials have already risen to the International requirements and made India ready to participate in more global trials.
Parading Indians as appealing trial participants
Recently the catch phrases are large, diverse, therapy-naïve and large patient pool in acute or chronic diseases in clinical trials. The terms “therapy-naïve” and “large patient pool”- the former simply refers to those who are not able to access treatment and the latter implies that there is a high incidence and prevalence of all kinds of diseases. These are facts which are parading our Indians as trial participants and hence the government of India has started supervising the clinical trials by the licensing authority - Drugs Controller General of India.[2]
The situation in India
In comparison with the US and even with R and D China, the R and D expenditure of India is very less. US is fuelled by high government funding, universities and other academic institutions and hence they are leading in medical research. Government of India is also trying to increase in total R and D spending by increasing the private sector spending up to 50 percent.[2]
Participation of Indian subjects trials by multinational pharmaceutical companies
Multinational pharmaceutical companies are placing more and more clinical trials in India. It is important to state that we are only a part of trials done in other parts of the world as well. Clinical trial patients in India are treated just like their counterparts in other countries in Europe, America, Australia and other South Asian countries.
Challenges in vulnerable populations
The term vulnerable population implies the disadvantaged sub-segment of the community who needs utmost care and ancillary considerations and protection in research.[3] Hence protecting the rights, well-being, safety in context to risk-benefit scales, privacy and confidentiality of vulnerable subjects is of paramount importance.[4]
Informed consent process has an impressive influence on the principle of research with direct implications to comprehension of the proposed study particularly in these groups of participants.[5] It is very important that the Institutional or Independent Ethics Committee Members monitor the study which will be an additional safeguard to the vulnerable subjects.[6]
Surrogate in cognitively impaired patients
The principle of voluntariness and informed consent shall continues to apply even though the subject is incapable of giving consent. The patients who are behaviorally or emotionally challenged are incompetent to provide independent informed consent and hence surrogate consents are required.[7,8] This is applicable for research on disorders like Alzheimer's disease.
Currently, regulations governing research allow proxy consent for research involving the adults who lack decision-making capacity if a “Legally Authorized Representative” (LAR) gives permission.
Research on children
Parents are required to make the decision on their behalf[7] as children are believed to have limited cognitive and emotional capabilities from ethical and legal perspectives. Dedicated pediatric trials may be essential where the disease predominantly affects this age group, uniquely in the scenario of being predisposed to certain medical conditions.[4]
Research on the children needs a lot of guidelines and should be carried out in such a way that the children are protected and the risk is very minimal. Research should be conducted in settings in which the child and parent can obtain adequate medical and psychological support.
As per legal definition, subjects aged less than 18 years (equivalent to age of majority) are considered minors and worldwide are not permitted to provide consent. The child assent or agreement is obtained considering the ambit of the child's understanding; generally a minimum age for which is characterized in the protocol.
About 70 percent of children with cancer are enrolled in clinical trials sponsored by the National Cancer Institute. The recruitment of children, however, may raise the concern that they are being exploited. Therefore, it is of utmost importance that the purpose of the research is to obtain the knowledge relevant to health needs of children.
Protecting women who participate in research studies
Clinical research raises in justice if women are excluded from participating in a study as it deprives the women the possibility of benefit.[9] Therefore, we need to ensure that women are appropriately represented in research studies and this necessitates stringent review of animal studies of the drug effects on reproduction and development, including dose-response relationship and mechanism of toxicity. We should expand access to experimental drugs used to treat serious and life threatening illnesses to all women, regardless of reproductive situation.
Women of child-bearing potential
It is not essential to exclude women of child-bearing potential from participating in clinical studies. We can discuss the potential risks to reproduction and potential offspring in the informed consent process, including, where appropriate, an adequate discussion of birth control. Hence, regular monitoring of subjects for pregnancy during the trial becomes of utmost important. Subjects are also monitored for reproductive and developmental toxicity if pregnancy occurs.
Pregnant and lactating women
Participation of pregnant women is based on the principle that information gleaned from good research leads to augmented standards of maternal and fetal healthcare.[10] As noted from the earlier post marketing research practices, these populations may inadvertently be exposed to high risks of unintentional detrimental effects as a result of their conditions. The fear of including lactating, pregnant and women of child bearing potential originated from scientific and social concerns of anticipated potential risks to the embryo, fetus and neonate.[11] Excluding this population could lead to unjustified deprivation of vital diagnostic, preventative and therapeutic information. A viable justification needs to be provided in the research documents when this population is excluded.[11]
Therefore, pregnant women and nursing mothers are presumed to be eligible for clinical studies; they are competent adults capable of making their own decisions about participating in the clinical studies. Ensure that pregnant women are given adequate information about the potential risks and benefits to themselves, their pregnancies, and their fetuses during the informed consent process.
Nursing mothers should receive adequate information about the potential risks to the child in the informed consent and also during the process of explaining the consent.
Prisoners
Prisoners can be recruited for research only under certain conditions, and usually not at all. Prisoners by nature of their circumstances possess abbreviated freedom to consent or decline consent and hence to be treated as equitably as regular subjects. When considering designing a study that would enroll prisoners, the investigator and institutional review board must determine if it is permissible even to study prisoners. Generally, only research that has the potential to benefit the prisoner is permitted. Institutional Ethics Committee (IEC) should thoroughly screen the informed consent forms as well as the patient information form.[12] Mostly, the research conducted on prisoners pertains to health and social issues with potential direct benefits, confined to their environmental conditions.
Today federal regulations make it much more difficult to use prisoners as subjects in medical research, and little research is conducted in United States prisons.
Students
Students and residents in training are considered vulnerable when a decision to participate is perceived to be required to prevent discrimination, either in determination of course grades or performance evaluation in an academic department. Students and residents may feel compelled to participate, no matter how well-intentioned the instructor.
Students believe that failure to do so will negatively affect their grades, evaluations, and the attitude of the instructor (and perhaps other students and residents) toward them.[13]
An underlying principle of the federal regulations on human-subjects research is that the subject's participation is voluntary. The relationship of instructor and student is inherently of unequal power.
Informed consent and the patient's participation
A well taken informed consent requires the patient to understand that he has the option to not participate in the trial and the trial represents an experiment, that the patient has certain responsibilities should he choose to participate and that there are both potential benefits and risks of participation in the trial.
In case of vulnerable populations, the principles and spirit of good clinical practice (GCP)[14] of respect for persons devoid of prejudice and therapeutic misconception is assured through an effective consent process. The informed consent document (ICD) should also comply with all applicable elements deliberated in the local regulatory norms.[15] It is important that the site personnel checks for the language and literacy capabilities of the potential vulnerable participants.[16]
The acceptable language in ICDs may be equivalent to that of local middle school level of education and essentially non-technical[5] to suit the solicited community. As these consents are also applicable for pediatric and geriatric patients, it is important that the font of the written documentation is easy to read.[15] The ICDs should not be lengthy[17] or at the tail end a frequently asked questionnaire. A simple summary of goals for the study maybe enumerated empowering the comprehension, in achieving a superior caliber of consent.[11]
Data safety monitoring board
This is an independent group of experts who monitor the participant safety and treatment efficacy data while a clinical trial is ongoing. The primary mandate of the data safety monitoring board (DSMB) is to protect the patient's safety. If adverse events of a particularly serious type are more common in the experimental arm compared to the control arm, then the DSMB would recommend the termination of the study. This evaluation has to be made in consideration of risk versus benefit. In many cases, the experimental therapy could cause adverse events during the treatment for example during chemotherapy for some terminal cancer. In such cases the benefits should be weighed against the potential risks before terminating the trial.[18]
Benefits and risks of clinical trials
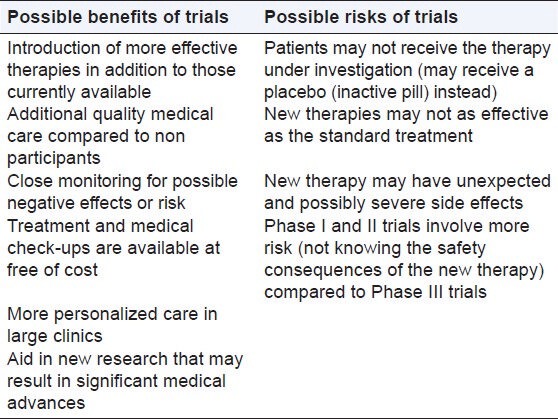
The benefits and risks vary significantly depending on the type and purpose of the trial. Table 1 summarizes the possible benefits and risks in a clinical trial.
Table 1.
Benefits and risks in a clinical trial
Why the controversy regarding drug trials in India?
The recent controversy over conducting clinical trials in India has snowballed into a serious issue. A series of articles in newspapers and public debates on TV have tarnished the entire clinical trials sector. Some NGOs have gone to court with public interest litigations and these have sparked a lot of heat and debate. Unfortunately many of these individuals and organizations are whipping up emotions by portraying only the darker side - showing how some terminally-ill patients did not survive a clinical trial. As the Indian Society for Clinical Research (ISCR) has said, those participating in trials are already afflicted, some very seriously ill. Their death, therefore, may not be due to the drug. If they were terminally ill, at worst, the drug perhaps did not prove to be as effective as it was hoped. That is not the fault of the trialists.
It is important to note that many trials in India are Phase-III trials which are global trials with a stringent common protocol for already well-tested drugs. Hence, the risks to patients are minimal. In any case, without a trial it is impossible to determine, if and how, a drug works. Factors such as racial characteristics, genetic make-up, and biochemical variations also have a bearing on the outcome of a trial.
Trials are usually conducted with the highest degree of transparency and with the complete consent of patients and families, disclosing not just potential benefits but also risks involved. As in any industry, there may be some black sheep among the clinical trialists and they must be dealt with utmost severity. But that does not mean that the entire industry of clinical trials is suspect. The term patients are treated as “guinea pigs” is often used. From the description of the informed consent process and the protection of trial participants described above, it is clear that in the majority of cases these charges are baseless. A few bad people exploiting patients for their own selfish reasons using fraudulent means does not mean all clinical trialists are bad.[19]
The reality is that uninformed media coverage can hinder clinical progress in India. We need to adopt a rational perspective of clinical trials - understand how they are run, realize their criticality to patients and address issues objectively instead of asking to stop trials altogether.
Instead of dismissing all clinical trials as bad, we need to plug any potential loopholes and implement existing laws stringently to ensure that clinical trials are conducted with utmost transparency and diligence. If India curtails clinical trials, pharmacy will shift to other developing countries. We will then only end up with a situation where we have no good data on our Indian patients. An example in point is the Human Genome Project where India refused to participate and today Indian data is sadly missing in that project.
CONCLUSIONS
Conducting clinical trials, in addition to advancing science also has myriad benefits to the participants. India has emerged as a global hub for clinical trials and sufficient regulatory provisions are in place to ensure safety of the participants. Ensuring proper compliance with the regulatory norms and proper training of concerned personnel in GCP will ensure that India continues to reap the benefits of clinical trials.
It is important to note that there is no way a drug could be used except through an evidence-based method involving clinical trials. Even though there could be issues, the present treatment being given to the clinical trials is worse than the problem. Hence, we need to create competencies for clinical trials in the form of better regulation and funding and the training of right human resources so that India can proudly stand among the comity of nations doing clinical trials.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1. [Last accessed on 2013 May 23]. Available from: http://www.iscr.org/Resource/126681048_Clinical%20trial%20India.pdf .
- 2.Bajpai V. Rise of clinical trials industry in India: An analysis. ISRN Public Health, 2013;2013:1–17. [Google Scholar]
- 3.WMA declaration of Helsinki-Ethical principles for medical research involving human subjects. 59th WMA General Assembly; October 2008; Seoul, Korea. [Google Scholar]
- 4.Ethical guidelines for biomedical research on human participants. New Delhi: 2006. Indian Council of Medical Research. [Google Scholar]
- 5.ICH GCP-International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use ICH harmonised tripartite guideline, Guideline for Good Clinical Practice E6 (R1)
- 6.Faden RR, Lewis C, Rimer B. Monitoring informed consent procedures: An exploratory record review. IRB. 1980;2:9–10. [PubMed] [Google Scholar]
- 7.ICH GCP-International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use ICH harmonised tripartite guideline, Guideline for Good Clinical Practice E6(R1) Current Step 4 version dated 10 June 1996.
- 8.Saks ER, Dunn LB, Wimer J, Gonzales M, Kim S. Proxy consent to research: The legal landscape. Yale J Health Policy Law Ethics. 2008;8:37–92. [PubMed] [Google Scholar]
- 9.Women's health: FDA needs to ensure more study of gender differences in prescription drug testing. Washington, DC: Government Printing Office; 1992. United States General Accounting Office. Report No. GAO/HRD 93.17. [Google Scholar]
- 10.Goldenberg MM, editor. Politics and Clinical Trials: The Inclusion of Women. [Last accessed on 2012 Aug, 2003 Dec 28]. Available from: http://www.pharmscope.com/ptjournal/fulltext/28/12/PTJ2812791.pdf .
- 11.US Department of Health and Human Services-Office of Human Research Protections (OHRP) Subpart B, Additional Protections for Pregnant Women, Human Fetuses and Neonates Involved in Research, Code of Federal Regulations Title 45, Part 46 Protection of Human Subjects.
- 12.US Department of Health and Human Services-Office of Human Research Protections (OHRP), Additional Protections Pertaining to Biomedical and Behavioral Research Involving Prisoners as Subjects Subpart C, Code of Federal Regulations Title 45, Part 46 Protection of Human Subjects.
- 13.Schwenzer KJ. Protecting vulnerable subjects in clinical research: Children, pregnant women, prisoners, and employees. Respir Care. 2008;53:1342–9. [PubMed] [Google Scholar]
- 14. [Last accessed on 2013 May 23]. Available from: http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6_R1/Step4/E6_R1Guideline.pdf .
- 15.Schedule Y. Clinical Trial Regulation in India, Drugs and Cosmetics (2nd Amendment) Rules, 2005 Ministry of Health and Family Welfare (Department of Health) Notification. New Delhi: 2005. Jan 20th, [Google Scholar]
- 16.Making written information easier to understand for people with learning disabilities: Guidance for people who commission or produce Easy Read information. revised ed. Department of Health U.K; [Google Scholar]
- 17.Verástegui EL. BMC Medical Ethics. Consenting of the vulnerable: The informed consent procedure in advanced cancer patients in Mexico. 2006. Dec. [Last accessed on 2012 Aug]. Available from: http://www.biomedcentral.com/1472.6939/7/13 . [DOI] [PMC free article] [PubMed]
- 18.Clinical Research Personnel-Page 2 from Cancer Information and Support Network. [Last accessed on 2013 Oct 19]. Available from: http://cisncancer.org/research/how_cancer_is_studied/clinical/research_personnel_02.html .
- 19.Shaw KM. The Economic Times. Need A Rational View on Clinical Trials. 2012. Sep 13, [Last accessed on 2013 Oct 19]. Available from: http://articles.economictimes.indiatimes.com/2012.09.13/news/33817062_1_clinical.trials.iscr.human.trials .


