Abstract
Context:
Treatment of Hangman's fractures is still controversial. Hangman's fractures Type II and IIA are usually treated with surgical procedures.
Aim:
This study aims at describing the Neurospinal Academy (NSA) technique as an attempt to achieve an approximation of the fracture line to the axis body, which may be used for Type II and IIA patients with severe displacement and angulation.
Settings and Design:
NSA technique both pars or pedicle screws are placed bicortically to ensure that anterior surface of C2 vertebral body will be crossed 1-2 mm. A rod is prepared in suitable length and curve to connect the two screws. For placing the rod, sufficient amount of bone is resected from the C2 spinous process. C2 vertebral body is pulled back by means of the screws that crossed the anterior surface of C2 vertebral body.
Materials and Methods:
Hangman II and IIA patient are treated with NSA technique.
Result:
Angulated and tilted C2 vertebral body was pulled back and approximated to posterior elements.
Conclusions:
In Hangman's fractures Type II and IIA with severe vertebral body and pedicle displacement, NSA technique is an effective and reliable treatment alternative for the approximation of posterior elements to the C2 vertebral body, which is tilted, angulated, and dislocated.
Keywords: Hangman's fracture, surgery, Type II, Type IIA
INTRODUCTION
Schneider was the first to introduce the term called “Hangman's Fracture”.[1] Garber suggested the term “traumatic spondylolisthesis of the axis”.[2] Some authors reported that different mechanisms initiated traumatic spondylolisthesis of the atlas that occurs after the trauma and Hangman's fractures that occur after execution.[3,4] While, traumatic spondylolisthesis that usually occurs due to some motor accident is initiated by a hyperextension and compression mechanism, fractures caused due to execution are usually initiated by a hyperextension and distraction mechanism.
Treatment of Hangman's fractures is still controversial. High fusion rates have been reported for Type I fractures treated with conservative methods such as halo and collar immobilization. Hangman's fractures Type II and III are usually treated with surgical procedures. Surgical techniques include C1-2 and C2-3 stabilization from a posterior approach in addition to the anterolateral and transoral C2-3 discectomy and fusion from an anterior approach.[5,6,7,8] Placement of pars and pedicle screws from a posterior approach can be listed among the other techniques.[9,10,11,12]
This study aims at describing the Neurospinal Academy (NSA) technique as an attempt to achieve an approximation of the fracture line to the axis body, which may be used for Type II, IIA, and III patients with severe displacement and angulation.
CLASSIFICATIONS OF HANGMAN'S FRACTURES
Although several classifications were made to categorize Hangman's fractures,[4,13] Effendi et al., divided Hangman's fractures into three categories based on the mechanism of injury. Accordingly Type I was defined as injuries resulted from axial loading with hyperextension, Type II as those resulted from hyperextension and rebound flexion, and Type III as those resulted from flexion and rebound extension.[14] Levine and Edwards modified Effendi et al.'s classification by adding Type IIA that resulted from flexion and distraction.[15] Hangman's fractures were categorized into the following groups according to Levine and Edwards’ classification:
Type 1: Non-displaced fractures with no angulation between C2 and C3 and a fracture dislocation of less than 3 mm,
Type 2: Fracture with significant angulation (>11 degrees) and displacement (>3.5 mm),
Type 2A: Fracture with minimum displacement and significant angulation (>11 degrees),
Type 3: Fractures with severe angulation and displacement associated with unilateral or bilateral C2-3 facet dislocation.
Treatment
Most Hangman's fractures can be treated with cervical immobilization.[4,15] Effendi et al., reported that they used external immobilization for the treatment of patients with Type I fractures, while they treated half of the Type II fracture patients with conservative and the other half with surgical treatment. Pepin and Hawkins reported that they used conservative methods and achieved fusion in 95% of the Hangman's fracture patients.[13] Pepin and Hawkins suggested the primary use of halo vest for Hangman's fractures and recommended surgery for the long-term nonfusion group. In their series, Levin and Edwards reported that they treated Type I, II, and IIA patients with nonsurgical methods.[15] Greene et al., also reported that external immobilization must be the first choice of treatment for Hangman's fractures.[16]
Surgical treatment
Surgical treatment must be performed for Hangman's Fractures, if fusion could not be achieved despite external immobilization. Options include anterior C2-3 and posterior C1-3 surgery. Effendi et al., performed surgery in 42 out of 131 patients. Ten patients were treated with anterior C2-3 fusion, while 32 patients were treated from a posterior approach.[14] They performed anterior C2-3 fusion in four patients, posterior C1-C3 fusion in two patients and posterior C2-C4 fusion in one patient they operated.[4]
Verheggen and Jansen suggested surgical treatment for Type II and III patients.[17] They obtained good results for each one of the 16 patients they operated. Borne et al., performed fixation by using bilateral posterior screw for axis fractures with a broken pedicle and obtained fusion in all patients.[5]
Patients with Type II and III fractures are usually treated surgically. Dalbayrak et al., operated four patients by using the pars screw and obtained fusion in all patients.[12]
NSA technique
The patient is placed on the operating table in prone position under general anesthesia. C3 skin incision is made under the occipitocervical junction to dissect the skin and the subcutaneous tissue. Subperiosteal stripping of the paravertebral muscles is carried out after dissecting the fascia. Exposure of upper and lower cervical vertebrae will be useful for orientation. A suitable point of entry is selected for the placement of C2 pedicle or pars screw.
Forwarding the guide through C2 pars or pedicle opens the route for the screw under repeated scopy controls to ensure that anterior surface of C2 vertebral body will be crossed 1-2 mm [Figure 1a and b]. A probe is used to check whether it is placed inside the bone. Both screws are placed bicortically. A standard rod which is used for posterior cervical fixation rod is prepared in suitable length and curve to connect the two screws [Figure 2a]. For placing the rod, sufficient amount of bone is resected from the C2 spinous process [Figures 2b, c and 3]. Screw heads are placed. Through fastening the screw heads under scopy control, C2 vertebral body is pulled back by means of the screws that crossed the anterior surface of C2 vertebral body. Then, final position of the vertebral body is checked [Figure 4a and b]. We have not used traction intraoperatively. But in some cases it may be useful for the reduction.
Figure 1.
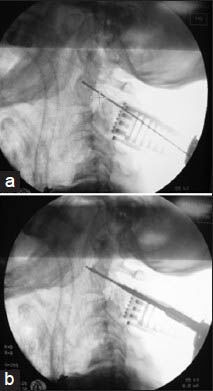
(a and b) Views under repeated scopy controls to ensure that anterior surface of C2 vertebral body will be crossed 1-2 mm
Figure 2.

(a) A rod is prepared to connect the two screws
Figure 2.
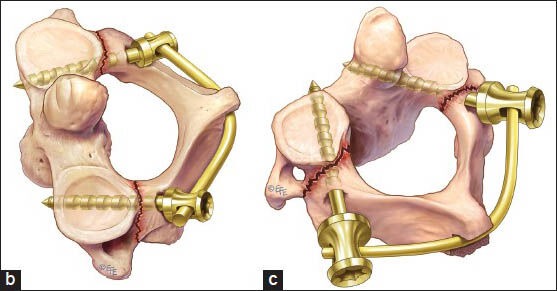
(b and c) Ilustrations of the NSA technique.
Figure 3.
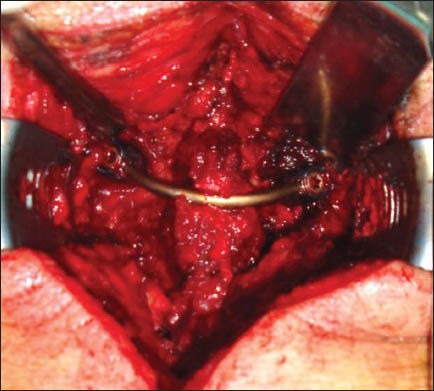
Bone is resected from the C2 spinous process to place the rod
Figure 4.
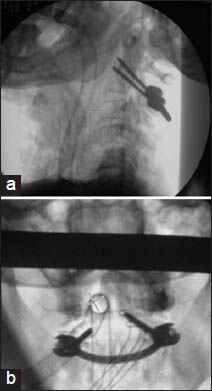
(a and b) Final position of the vertebral body is checked under scopy
DISCUSSION
Hangman's fractures can usually be treated by nonsurgical methods.[4,14] Surgical treatment should be considered for patients with temporal fractures due to a head trauma or for those who cannot wear a halo vest or for patients without fusion despite 3 months of conservative treatment. Surgical method to be used for the treatment of Hangman's fractures is still controversial.
Effendi et al., reported that within the surgical treatment group they performed C2-3 anterior fusion in four patients; whereas, they performed posterior internal fixation and fusion in 11 patients. Within the same series, anterior procedure was performed in one of the Type III patients treated surgically, while four of them were treated from a posterior procedure.[14] Pepin and Hawkins needed surgical intervention in 5% of the patients with Hangman's Fractures, and he performed C2-3 anterior fusion in four patients; whereas, he performed posterior C1-C3 fusion in two and posterior C2-C4 fusion in one.[13] He recommended posterior C2-3 fusion on patients for whom surgical treatment was considered.[13]
There is no access to the pediculoisthmic component through the anterior procedure. However, it enables intervention to the traumatic C2-3 disc. By using the posterior procedure, on the other hand, posterior and anterior surface of C2 vertebra can be approximated and C2-3 segment can be fixed through the posterior approach. Combined approach using anterior-posterior procedure enables the fixation of all structures.
Muthukumar performed fusion with C1-3 lateral mass in three patients with Hangman's fractures (one Type IIA and two Type III) and reported successful results.[18] Alternative methods include the use of C2 pars and pedicle screw through the posterior approach. Posterior structures are approximated to the C2 vertebra by using C2 pars and pedicle screws.[7,19] Dalbayrak et al., reported fusion in each one of the four patients that they used pars screws.[12] Direct fixation crossing the fracture line preserves the movement in the C1-2 segment, which is the main advantage of such an intervention.[10,12]
Verheggen and Jansen reported that they used pedicle screws and obtained significant results for C2-3 dislocation and angulation in 15 patients with Type II, IIA, and III Hangman's fractures.[17] However, pedicle screws are not recommended for use in traumatic discs.[12,17] An effective method is to use C2 pedicle screws alone or with C3 lateral mass screws for Type II, IIA, and III fractures.[12] However, in Hangman's fractures Type II, IIA, and III with severe displacement and angulation it is difficult to approximate the posterior elements to the C2 vertebral body that tilted forward and angulated. The key to preoperative decision-making is to check the presence of discoligamentous injury.[12]
In Hangman's fractures Type II and IIA with severe vertebral body and pedicle displacement, intraoperative difficulties arise during the approximation of posterior elements to the C2 vertebral body, which is tilted, angulated, and dislocated [Figures 5 and 6]. We used the NSA technique to treat one patient with Type II and two patients with Type IIA fractures [Table 1]. Besides, in one patient it was impossible to use the halo vest since he had temporal fracture due to head trauma. For the other two patients we decided to use the NSA technique to let us pull back the forward tilted vertebra, since we considered it was impossible to treat these patients with direct pedicle or pars screws as they had severe forward tilting and angulation in the C2 vertebral body.
Figure 5.
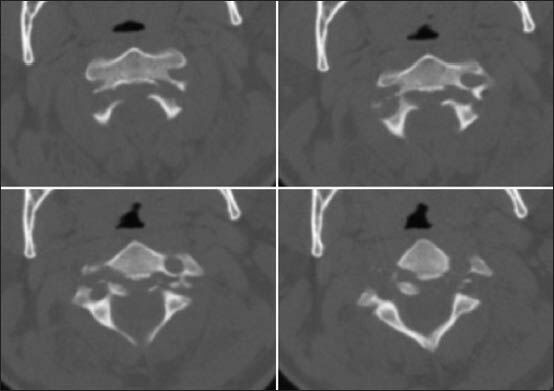
Preoperative axial computed tomography (CT and MRI) images of a Hangman's fracture
Figure 6.
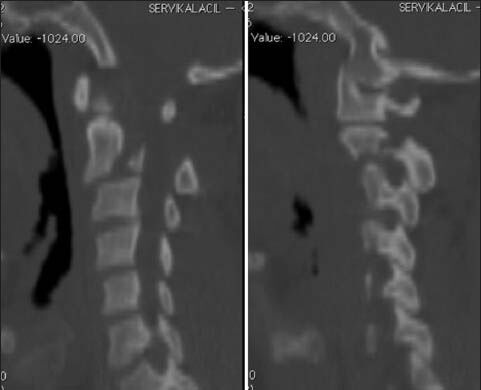
Preoperative sagittal CT images of a Hangman's fracture
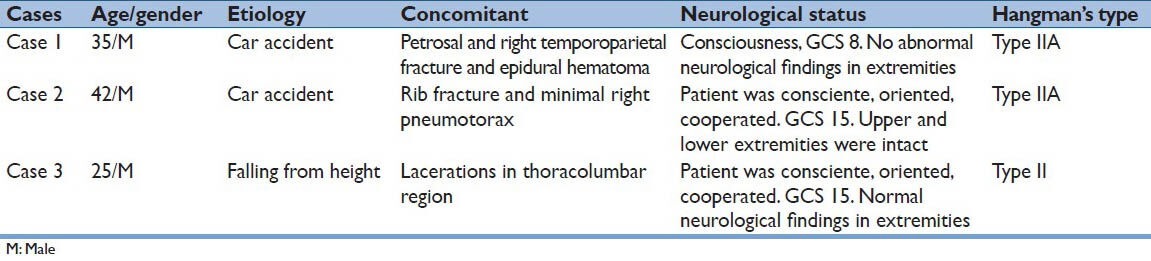
Table 1.
Reasons of trauma of the cases, additional pathologies, clinical evaluation of the patients, and types of Hangman's fracture
This new technique that we call NSA is quite successful at the treatment of patients with Hangman's fractures Type II and IIA, who cannot wear a halo vest or who are with severe forward tilting of the C2 vertebral body, severe displacement of the vertebral body, and posterior elements or with severe angulation. A healthy C2-3 facet joint is required for the NSA technique. Therefore, Type III may not be eligible. In trauma cases with unilateral or bilateral pars fractures where it is impossible to fix the posterior elements to the vertebral body with a pars screw, this technique will enable the approximation and fixation of posterior elements by screws placed directly into the vertebral body. Using this technique, the place for pars or pedicle screws should be prepared bicortically under scopy control [Figure 1a and b]. A rod is prepared in suitable length and curve to connect the two screws [Figure 2]. For placing the rod, sufficient amount of bone is resected from the C2 spinous process [Figure 3]. The lamina is pressed anteriorly, while screw heads are fastened. Through fastening the screw heads under scopy control, C2 vertebral body is pulled back by means of the screws that crossed the anterior surface of C2 vertebral body, and final position of the vertebral body is checked [Figure 4a and b]. In the postoperative control, cervical CT of one of the patients we operated by using the NSA technique, we observed that the previously forward-tilted vertebral body could be pulled back by means of the screws placed bicortically [Figures 7–9].
Figure 7.
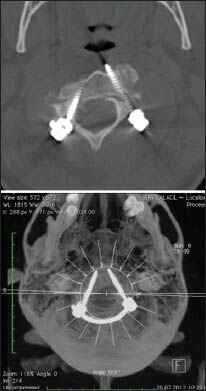
Postoperative axial CT images of a Hangman's fracture
Figure 9.

Postoperative coronal CT images of a Hangman's fracture
Figure 8.

Postoperative sagittal CT images of a Hangman's fracture
CONCLUSION
In Hangman's fractures Type II, IIA, and III with severe vertebral body and pedicle displacement, NSA technique is an effective and reliable treatment alternative for the approximation of posterior elements to the C2 vertebral body, which is tilted, angulated, and dislocated.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Schneider RC, Livingston KE, Cave AJ, Hamilton G. “Hangman's fracture” of the cervical spine. J Neurosurg. 1965;22:141–54. doi: 10.3171/jns.1965.22.2.0141. [DOI] [PubMed] [Google Scholar]
- 2.Govender S, Charles RW. Traumatic spondylolisthesis of the axis. Injury. 1987;18:333–5. doi: 10.1016/0020-1383(87)90055-6. [DOI] [PubMed] [Google Scholar]
- 3.Fielding JW, Francis WR, Jr, Hawkins RJ, Pepin J, Hensinger R. Traumatic spondylolisthesis of the axis. Clin Orthop Relat Res. 1989:47–52. [PubMed] [Google Scholar]
- 4.Francis WR, Fielding JW, Hawkins RJ, Pepin J, Hensinger R. Traumatic spondylolisthesis of the axis. J Bone Joint Surg Br. 1981;63B:313–8. doi: 10.1302/0301-620X.63B3.7263740. [DOI] [PubMed] [Google Scholar]
- 5.Borne GM, Bedou GL, Pinaudeau M. Treatment of pedicular fractures of the axis: A clinical study and screw fixation technique. J Neurosurg. 1984;60:88–93. doi: 10.3171/jns.1984.60.1.0088. [DOI] [PubMed] [Google Scholar]
- 6.Grob D, Magerl F. Surgical stabilization of C1 and C2 fractures. Orthpade. 1987;16:46–54. [PubMed] [Google Scholar]
- 7.Naderi S, Arman C, Guvencer M, Korman E, Seno¡glu M, Tetik S, et al. An anatomical study of the C-2 pedicle. J Neurosurg Spine. 2004;1:306–10. doi: 10.3171/spi.2004.1.3.0306. [DOI] [PubMed] [Google Scholar]
- 8.Wilson AJ, Marshall RW, Ewart M. Transoral fusion with internal fixation in a displaced hangman's fracture. Spine (Phila Pa 1976) 1999;24:295–8. doi: 10.1097/00007632-199902010-00022. [DOI] [PubMed] [Google Scholar]
- 9.Bristol R, Henn JS, Dickman CA. Pars screw fixation of a hangman's fracture: Technical case report. Neurosurgery. 2005;56:E204. doi: 10.1227/01.neu.0000144172.84111.a6. [DOI] [PubMed] [Google Scholar]
- 10.Hakato J, Wrofski J. Operative treatment of hangman's fractures of C2. Posterior direct pars screw repair or anterior plate-cage stabilization? Neurol Neurochir Pol. 2008;42:28–36. [PubMed] [Google Scholar]
- 11.Suchomel P, Hradil J, Barsa P, Buchvald P, Lukas R, Taller S, et al. Surgical treatment of fracture of the ring of axis — “hangman's fracture. Acta Chir Orthop Traumatol Cech. 2006;73:321–8. [PubMed] [Google Scholar]
- 12.Dalbayrak S, Yılmaz M, Firidin M, Naderi S. Traumatic spondylolisthesis of the axis treated with direct c2 pars screw. Turk Neurosurg. 2009;19:163–7. [PubMed] [Google Scholar]
- 13.Pepin JW, Hawkins RJ. Traumatic spondylolisthesis of the axis: Hangman's fracture. Clin Orthop Relat Res. 1981:133–8. [PubMed] [Google Scholar]
- 14.Effendi B, Roy D, Cornish B, Dussault RG, Laurin CA. Fractures of the ring of the axis: A classification based on the analysis of 131 cases. J Bone Joint Surg Br. 1981;63B:319–27. doi: 10.1302/0301-620X.63B3.7263741. [DOI] [PubMed] [Google Scholar]
- 15.Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am. 1985;67:217–26. [PubMed] [Google Scholar]
- 16.Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK. Acute axis fractures: Analysis of management and outcome in 340 consecutive cases. Spine (Phila Pa 1976) 1997;22:1843–52. doi: 10.1097/00007632-199708150-00009. [DOI] [PubMed] [Google Scholar]
- 17.Verheggen R, Jansen J. Hangman's fracture: Arguments in favor of surgical therapy for type II and III according to Edwards and Levine. Surg Neurol. 1998;49:253–61. doi: 10.1016/s0090-3019(97)00300-5. [DOI] [PubMed] [Google Scholar]
- 18.Muthukumar N. C1-C3 lateral mass fusion for type IIa and type III Hangman's fracture. J Craniovertebr Junction Spine. 2012;3:62–6. doi: 10.4103/0974-8237.116541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ebraheim NA, Fow J, Xu R, Yeasting RA. The location of the pedicle and pars interarticularis in the axis. Spine (Phila Pa 1976) 2001;26:E34–7. doi: 10.1097/00007632-200102150-00002. [DOI] [PubMed] [Google Scholar]


