Abstract
Aim:
The author reports early post-operative outcome and preliminary experience with an alternative form of treatment of cervical degenerative or spondylotic disease leading to spinal canal stenosis that involves fixation-arthrodesis of the affected spinal segment using one or two (double insurance) transarticular screws for each joint.
Materials and Methods:
During the period of months from March 2013 to July 2013, six patients having cervical spondylotic cord compression were treated with transarticular method of screw fixation of the involved segments. The operation involved section of the spinous process at its base, opening up of the facet joint, denuding of articular cartilage, placement of intraarticular cavity bone graft chips and insertion of either a single or two transarticular screws at each level. The fixation was done in four levels in four patients and at two levels in two patients. Japanese Orthopedic Association score, visual analog scale (neck pain) and Odom's criteria were used to monitor the clinical status of the patients before and after the surgery and at follow-up.
Results:
Immediate post-operative and a relatively short-term post-operative outcome was remarkably gratifying. During the average period of follow-up of 6 months (range: 3-8 months); there was varying degree of recovery of symptoms. The procedure resulted in firm stabilization and fixation of the spinal segment and provided a ground for arthrodesis. No patient worsened after treatment. During the period of follow-up, all patients showed remarkable and progressive recovery in symptoms.
Conclusions:
Vertical instability and telescoping, listhesis or overriding of the facets on physical activity seems to be the defining phenomenon in pathogenesis of cervical spondylotic disease. The clinical outcome in our patients suggest that only fixation of the spinal segment can be a rationale form of treatment. Transarticular method of treatment is a simple, safe and effective method of spinal stabilization. The firm stabilization at the fulcrum of cervical spinal movements provided a ground for segmental spinal arthrodesis. Use of two or “double insurance” screws at each facet is possible and provides reassuring stability in selected cases.
Keywords: Arthrodesis, cervical spondylosis, instability, transarticular fixation
INTRODUCTION
In this report, we present an alternative form of treatment for cervical spondylotic myelopathy. The treatment involves only fixation of the involved segments of the cervical spine using one or two transarticular screws for each joint. The proposed treatment is based on the hypothesis that “vertical spinal instability” results in telescoping of the facets and forms the basis of pathogenesis of cervical degenerative spondylosis.[1,2,3] The operation aims at arthrodesis of the affected spinal segments. Fixation of the segments resulted in immediate post-operative and lasting relief from symptoms. The authors present the outcome of six cases with such a form of treatment. The remarkably satisfying patient outcome has prompted this report. The rationale of treatment is presented and the literature on the subject has been briefly reviewed.
MATERIALS AND METHODS
During the period March 2013-July 2013, we treated six cases of cervical degenerative spondylosis using the proposed surgical strategy. These patients were analyzed prospectively. There were all males and their ages ranged from 40 to 73 years (mean 56 years). The patients had characteristic multilevel cervical spondylotic or degenerative disease that resulted in varying degree of cervical myelopathy. The patients had progressive neurological symptoms and failure of non-operative management. Patients having an acute disc herniation or an extruded disc fragment were not included. The presenting clinical symptoms and the outcome are enumerated in Tables 1 and 2. Japanese Orthopedic Association (JOA) score,[4] Odom's criteria[5] and visual analog score[6] were used to evaluate the patients before and after surgery and at a follow-up. All patients were investigated with dynamic (flexion and extension views) plain radiography and computerized tomography (CT) scan and magnetic resonance imaging (MRI) before and after surgery. Four patients underwent a four level and two patients underwent a two level treatment. All radiographic measurements were taken with the neck in neutral position. The radiographic analyses that were performed included assessment of bone fusion.
Table 1.
The presenting clinical and radiological features
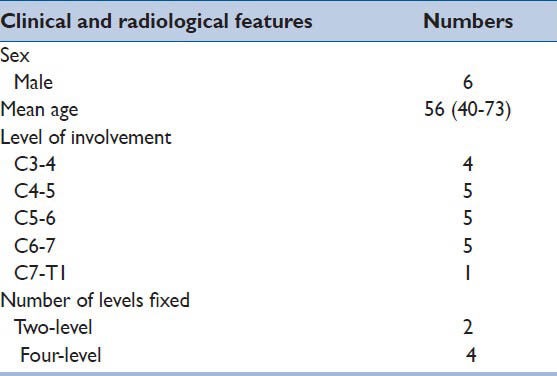
Table 2.
Outcome according to Odom's criteria
Operative technique
The patient was placed in the standard prone position with the head in cervical Gardner-Wells traction that kept the head in a “floating” position, as described and used by us in surgery for craniovertebral junction fixation.[7,8] Traction was deployed essentially to keep the head stable during surgery, keep the neck in a mildly flexed position and to keep the faceoff the head holder avoiding any injury to the eyes and facial skin. Midline incision was taken and employing sub-periosteal dissection the articular joints were exposed widely on both sides. The facets having clear evidence of instability and excessive abnormal movements were considered suitable for the proposed operation. These findings were valuable and were correlated with clinical symptoms and findings on images whilst considering the levels and extent of fixation. The articular capsule was opened and the facets were distracted using varying sizes of osteotomes that were introduced with their flat-sharp edge and then turned 90° to affect distraction. The articular capsule and end plate cartilage was widely denuded using screwing motion of the osteotome and whenever necessary using micro-drill. Bone graft pieces harvested from the spinous process were jammed into the articular cavity. The interspinous-process ligaments are then widely removed. Spinous process is sectioned along its base. Transarticular screw insertion was then done with the technique described earlier by Roy-Camille and Saillant.[9] The screws measured 2.8 mm in diameter and 16-18 mm in length. In two cases, two screws were used at each articular joint [Figure 1]. Such a “double insurance” screw implantation added stability to the implant. Bone graft obtained following sectioning of the adjoining spinous processes is placed over the appropriately prepared host bone area of laminae. In the initial two patients, bone graft was additionally harvested from the iliac crest and placed in the region. The patient is then advised limited cervical movement using external orthrosis for a period of 8 weeks. After this period, all routine activities were permitted.
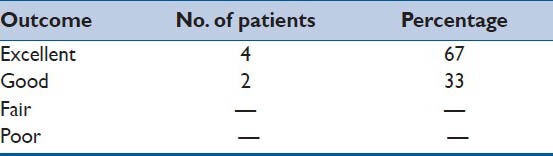
Figure 1.
Images of a 40-year-old male patient (a) T2 weighted sagittal magnetic resonance imaging shows degenerative spinal cord compression, more prominently at C5-6 and C6-7 levels (b) Computerized tomography scan shows presence of posterior osteophytes indenting into the spinal canal at C5-6 and C6-7. (c) Computerized tomography scan image through the facets. (d) Post-operative magnetic resonance imaging shows marginally reduced indentation of the osteophytes into the canal. (e) Post-operative computerised tomography scan showing an increase in the intervertebral and interlaminar spaces following surgery. (f) Image thorough the facets showing transarticular screws. (g) Radiograph showing two transarticular screws at each joint. (h) Lateral radiograph showing the four screws at each level superimposed
RESULTS
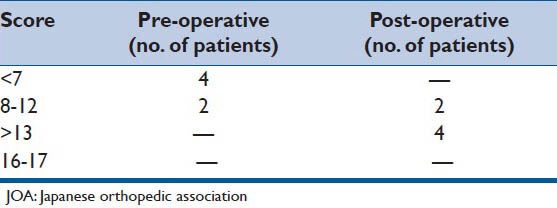
The follow-up period ranged from 3 to 8 months, average being 6 months. Neurological and radiographic assessments were performed by observers independent of the author. The clinical outcome of surgery is elaborated in Tables 2–4. There was no incidence of misplacement or dislodgement of the implant. All patients improved in symptoms following surgery to varying extent. The degree of improvement was monitored as per the JOA score, Odom's criteria and visual analog scale and is elaborated in the Tables 2–4. The evaluation included the location and degree of pre-operative and post-operative pain and myelopathy symptoms using an analog scale, subjective and objective alteration in sensation and weakness, walking difficulty and bowel or bladder changes. All patients are satisfied with the surgery and are back into their pre-operative profession. In none of the cases the operation was repeated or any additional surgical maneuver was done. All patients underwent evaluation on static and dynamic cervical spine radiographs and CT scanning and MRI [Figure 1]. Static neutral lateral radiographs were used to assess cervical sagittal balance, whereas anteroposterior radiographs were used to exclude pre-operative abnormal coronal alignment. There was no implant related complication. Fusion of the spinal segment was defined as the absence of all kinds of motion and alterations in the interlaminar and inter-vertebral body distances on flexion-extension X-ray films done at a follow-up of at-least 3 months. Bone formation was observed inside and across the facets. As per this criterion, successful fusion was obtained in all the treated spinal levels.
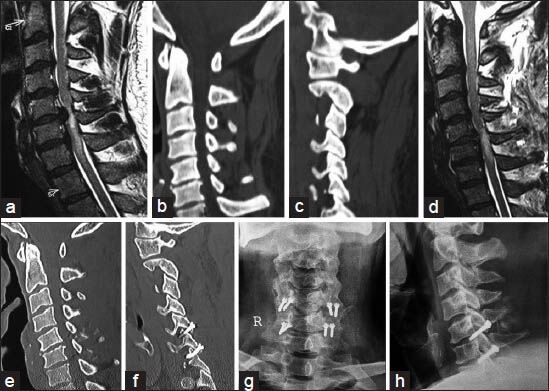
Table 4.
VAS (0-no pain, 10-maximum pain)
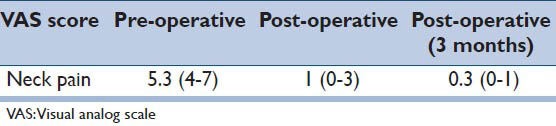
Table 3.
Grading of myelopathy by the JOA score
DISCUSSION
Cervical spondylotic myelopathy is a disabling clinical condition. The pathogenesis has been well-described in the literature.[10,11] The most accepted view of pathogenesis is that it is related to a cascade of processes that start with degeneration of the disc due to its dehydration or herniation. It has been generally accepted that following this primary event, there occurs loss of disc space height, bulge of the posterior annulus/posterior longitudinal ligament, overriding of the facets and/or infolding of the ligamentum flavum and similar such events that ultimately lead to stenosis of the spinal canal and intervertebral neural foramina. Cervical spondylotic myelopathy has been treated by a variety of non-surgical and surgical methods. A range of surgical techniques and elaborate technological tools have been in use for the surgical treatment. It may not be an over-exaggeration to say that there is no standard or gold standard treatment that has a universal acceptance. Bone preserving or saving methods have recently found favor. Although the issue of instability in degenerative cervical spondylosis has been discussed on several occasions, its role as the primary factor in the pathogenesis has not been appropriately addressed or therapeutically exploited. We recently described facetal distraction as an option for the treatment for single and multi-level cervical spondylotic myelopathy.[12] This operation involved an attempt toward realignment of the spinal elements by distraction, fixation and ultimately aims at arthrodesis. Apart from this technique, where no bone, ligament or disc resection was necessary and where the aim of surgery is essentially fixation and arthrodesis, all other techniques either aim at neural decompression alone or aim for decompression and stabilization.[13,14,15]
Our study on the subject shows that subtle manifest instability of the spinal segment may be paramount in the pathogenesis of the entire structural deformation in spondylotic degenerative disease of spine.[1,2,3,12,16] Such instability was rather easily observed on direct visualization of the joint during surgery, even when pre-operative dynamic radiographs do not depict such an event. Our experience with arthritis of the craniovertebral junction and with direct exposure of the atlantoaxial joint cavity over 24 years, suggests that there is a clear evidence of arthritis and instability of the facets in these cases.[17] It is apparent that weakness of the muscles of the nape of the neck leads to their fatigue on exercise and subsequent incompetence may lead to facetal override or telescoping. The radiological effect on the cervical canal size on axial loading has been discussed. It appears that the phenomenon of cervical canal stenosis is “dynamic” in nature and local spinal instability plays a major role in its genesis. Standing human posture, ageing muscles, heavy body weight and sedentary life style may have contributory effects on pathogenesis of cervical spondylotic myelopathy. It does appear that the muscles have a role in keeping the spinal segments apart. Reduction of the articular cavity space and subsequent facetal overriding or telescoping and consequent ligamental laxity and buckling might occur on activity. Decrease in inter-facet height and retrolisthesis can result in reduction in intervertebral canal height that can cause radiculopathy and myelopathy symptoms. It appears that this retrolisthesis is a result of potential or manifest instability of the segment.[1,2,3] Dynamic images do not clearly demonstrate the instability of the facets due to their oblique profile and the difficulty in directly imaging the joints. It may be possible, that the spondylotic disease process actually begins with facetal instability and the discs are involved secondarily. Physiotherapy and traction over the back have been successfully used for decades in the management of cervical spondylosis. We identified that such a form of treatment that involved facetal distraction resulted in reversal of several pathologic events that are related to spondylosis.[12] In the presented series, we fixed the affected spinal segments using transarticular screws, without physically distracting the facets. Although we did not aim for facetal distraction, we impacted bone chips within the joint cavity. Post-operative images showed fixation of the region and in addition showed distraction of the spinal elements in the region of surgery. There was an increase in the interlaminar space and intervertebral spaces as can be seen in Figure 1. The reason for the increase in the intervertebral dimensions could be related to bone graft insertion within the joint and the fact that transarticular fixation was done in the flexed neck position under cervical traction. Our successful outcome in the presented group of patients suggests that stabilization of the spinal segment has a prime role in the treatment of cervical spondylotic myelopathy. Fixation of the involved motion segment assists in eliminating subtle movements that could probably be the cause of pain, radiculopathy and myelopathy symptoms.
The oblique profile, relatively large size, firmness and biomechanical strength of the facets can be used effectively and safely for transarticular screw insertion.[18,19] Transarticular screws have been described earlier in stabilization of the cervical spine.[19,20,21] A number of biomechanical studies are available that suggest that transarticular screws provide satisfactory stability to the cervical spinal segment.[21] We sectioned the spinous process at its base. This procedure provided a possibility of insertion of transarticular screw with a wider angle. The screw could now travel in the lateral third of lamina and subsequently through the facets. Wider exposure of the facets following the spinous process resection and the relatively large size of the facets facilitated insertion of two screws in a transarticular fashion. Insertion of the two screws provided “double-insurance” stabilization. Although navigation provided accuracy to the procedure, even free-hand screw insertion under direct surgical vision seemed to be safe. The screws are inserted after wide removal of the articular cartilage. Such a wide cartilage removal assists in making an otherwise smooth and slippery surface rough for firm fixation of the implant and provides an enhanced opportunity for bone fusion. The remarkable strength of the transarticular screws, at the site of fulcrum of spinal movements, could be appreciated during the process of screw tightening and was also evident by the fact that not a single screw seemed to malfunction or changed its initial deployment position during the period of follow-up. Mineral density of the bones of the facets is significantly superior to that of any other part of the vertebra, imparting greater strength to the process of fixation. The large and bifid spinous process provided ample bone graft material. The spinous process was shredded into small multiple pieces, was placed in the articular cavity after denuding the articular cartilage and was placed over the appropriately prepared host area of laminae. The technique of deployment of screws is simple and significantly quick when compared to most other methods of decompression and fixation. The procedure can be done in isolation or can be employed as a supplement to all other techniques. It can be done when other methods of fixation/decompression have failed. The drawback of this study is that a comparative cohort of patients who had undergone either a traditional or conventional surgery was not performed. Moreover, the exact inclusion/exclusion criteria for deployment of the technique will need to be assessed, evaluated and determined on the basis of further clinical experience. Although movement preserving techniques are gaining acceptance, our technique involves fusion of the region. No adjacent level disc disease was encountered in our series. However, it is clear that longer follow-up on a larger number of cases will be necessary to evaluate this feature. We theorize that stabilization of the cervical spine would obviate the disadvantages of anterior decompression, prevent the development of kyphotic deformity frequently seen after uninstrumented laminectomy, decompress the spinal cord and produce neurological results superior to those achieved by conventional and accepted methods of multilevel anterior and posterior procedures.
The efficacy and safety of the technique is apparent from our successful results. The technique resulted in demonstrated improvements in gait, strength, sensation, pain and degree of myelopathy. The highlight of the technique is that it is simple and significantly quick when compared to all other methods of decompression and fixation. The procedure can be done in isolation or can be employed as a supplement to all other techniques. It can be done when other midline methods of fixation/decompression have failed. The size of the implant is relatively small and use of large sized metal implants extending over multiple levels, as are used in some described stabilization techniques, could be avoided. In no case did we observe recurrent disease, pseudarthrosis, hardware failure or migration. There were no wound infections or host rejections of instrumentation. As the nature of implant and the material employed is rather straight-forward, the hardware cost can be significantly less than the implants currently in commercial use.
CONCLUSION
Fixation of the spinal segment using single or double insurance transarticular screws can be a rational, relatively simple, safe and effective surgical option for single or multi-level cervical spondylotic myelopathy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Goel A. Facet distraction spacers for treatment of degenerative disease of the spine: Rationale and an alternative hypothesis of spinal degeneration. J Craniovertebr Junction Spine. 2010;1:65–6. doi: 10.4103/0974-8237.77669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goel A. Facet distraction-arthrodesis technique: Can it revolutionize spinal stabilization methods? J Craniovertebr Junction Spine. 2011;2:1–2. doi: 10.4103/0974-8237.85306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goel A. ‘Only fixation’ as rationale treatment for spinal canal stenosis. J Craniovertebr Junction Spine. 2011;2:55–6. doi: 10.4103/0974-8237.100049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fujiwara A, Kobayashi N, Saiki K, Kitagawa T, Tamai K, Saotome K. Association of the Japanese Orthopaedic Association score with the Oswestry Disability Index, Roland-Morris Disability Questionnaire, and short-form 36. Spine (Phila Pa 1976) 2003;28:1601–7. [PubMed] [Google Scholar]
- 5.Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc. 1958;166:23–8. doi: 10.1001/jama.1958.02990010025006. [DOI] [PubMed] [Google Scholar]
- 6.Huskisson EC. Measurement of pain. J Rheumatol. 1982;9:768–9. [PubMed] [Google Scholar]
- 7.Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method: A report of 160 treated patients. Neurosurgery. 2002;51:1351–6. [PubMed] [Google Scholar]
- 8.Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994;129:47–53. doi: 10.1007/BF01400872. [DOI] [PubMed] [Google Scholar]
- 9.Roy-Camille R, Saillant G. Surgery of the cervical spine. 2. Dislocation. Fracture of the articular processes. Nouv Presse Med. 1972;1:2484–5. [PubMed] [Google Scholar]
- 10.Baron EM, Young WF. Cervical spondylotic myelopathy: A brief review of its pathophysiology, clinical course, and diagnosis. Neurosurgery. 2007;60(1 Suppl 11):S35–41. doi: 10.1227/01.NEU.0000215383.64386.82. [DOI] [PubMed] [Google Scholar]
- 11.Shedid D, Benzel EC. Cervical spondylosis anatomy: Pathophysiology and biomechanics. Neurosurgery. 2007;60(1 Suppl 11):S7–13. doi: 10.1227/01.NEU.0000215430.86569.C4. [DOI] [PubMed] [Google Scholar]
- 12.Goel A, Shah A. Facetal distraction as treatment for single- and multilevel cervical spondylotic radiculopathy and myelopathy: A preliminary report. J Neurosurg Spine. 2011;14:689–96. doi: 10.3171/2011.2.SPINE10601. [DOI] [PubMed] [Google Scholar]
- 13.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–17. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 14.Mummaneni PV, Kaiser MG, Matz PG, Anderson PA, Groff MW, Heary RF, et al. Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. J Neurosurg Spine. 2009;11:130–41. doi: 10.3171/2009.3.SPINE08728. [DOI] [PubMed] [Google Scholar]
- 15.Faldini C, Leonetti D, Nanni M, Di Martino A, Denaro L, Denaro V, et al. Cervical disc herniation and cervical spondylosis surgically treated by Cloward procedure: A 10-year-minimum follow-up study. J Orthop Traumatol. 2010;11:99–103. doi: 10.1007/s10195-010-0093-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goel A, Shah A, Jadhav M, Nama S. Distraction of facets with intraarticular spacers as treatment for lumbar canal stenosis: Report on a preliminary experience with 21 cases. J Neurosurg Spine. 2013;19:672–7. doi: 10.3171/2011.8.SPINE11249. [DOI] [PubMed] [Google Scholar]
- 17.Goel A, Shah A, Gupta SR. Craniovertebral instability due to degenerative osteoarthritis of the atlantoaxial joints: Analysis of the management of 108 cases. J Neurosurg Spine. 2010;12:592–601. doi: 10.3171/2009.12.SPINE0999. [DOI] [PubMed] [Google Scholar]
- 18.Abdullah KG, Steinmetz MP, Mroz TE. Morphometric and volumetric analysis of the lateral masses of the lower cervical spine. Spine (Phila Pa 1976) 2009;34:1476–9. doi: 10.1097/BRS.0b013e3181a8f649. [DOI] [PubMed] [Google Scholar]
- 19.Barrey C, Mertens P, Jund J, Cotton F, Perrin G. Quantitative anatomic evaluation of cervical lateral mass fixation with a comparison of the Roy-Camille and the Magerl screw techniques. Spine (Phila Pa 1976) 2005;30:E140–7. doi: 10.1097/01.brs.0000155416.35234.a3. [DOI] [PubMed] [Google Scholar]
- 20.Horn EM, Theodore N, Crawford NR, Bambakidis NC, Sonntag VK. Transfacet screw placement for posterior fixation of C-7. J Neurosurg Spine. 2008;9:200–6. doi: 10.3171/SPI/2008/9/8/200. [DOI] [PubMed] [Google Scholar]
- 21.Ferrara LA, Secor JL, Jin BH, Wakefield A, Inceoglu S, Benzel EC. A biomechanical comparison of facet screw fixation and pedicle screw fixation: Effects of short-term and long-term repetitive cycling. Spine (Phila Pa 1976) 2003;28:1226–34. doi: 10.1097/01.BRS.0000065485.46539.17. [DOI] [PubMed] [Google Scholar]


