Abstract
Objective
To define the impact of hospital teaching status on length of stay and mortality for patients undergoing complex hepatopancreaticobiliary (HPB) surgery in the USA.
Methods
Using the Nationwide Inpatient Sample, we identified 285,442 patient records that involved a liver resection, pancreatoduodenectomy, other pancreatic resection, or hepaticojejunostomy between years 2000 and 2010. Year-wise distribution of procedures at teaching and non-teaching hospitals was described. The impact of teaching status on in-hospital mortality for operations performed at hospitals in the top tertile of procedure volume was determined using multivariate logistic regression analysis.
Results
A majority of patients were under 65 years of age (59.6 %), white (74.0 %), admitted on an elective basis (77.3 %), and had a low comorbidity burden (70.5 %). Ninety percent were operated upon at hospitals in the top tertile of yearly procedure volume. Among patients undergoing an operation at a hospital in the top tertile of procedure volume (>25/year), non-teaching status was associated with an increased risk of in-hospital death (OR 1.47 [1.3, 1.7]). Other factors associated with increased risk of mortality were older patient age (OR 2.52 [2.3, 2.8]), male gender (OR 1.73 [1.6, 1.9]), higher comorbidity burden (OR 1.49 [1.3, 1.7]), non-elective admission (OR 3.32 [2.9, 4.0]), and having a complication during in-hospital stay (OR 2.53 [2.2, 3.0]), while individuals with private insurance had a lower risk of in-hospital mortality (OR 0.45 [0.4, 0.5]). After controlling for other covariates, undergoing complex HPB surgery at a non-teaching hospital remained independently associated with 32% increased odds of death as (OR 1.32, 95 % CI 1.11–1.58; P <0.001).
Conclusions
Even among high-volume hospitals, patients undergoing complex HPB have better outcomes at teaching vs. non-teaching hospitals. While procedural volume is an established factor associated with surgical outcomes among patients undergoing complex HPB procedures, other hospital-level factors such as teaching status have an important impact on peri-operative outcomes.
Keywords: Teaching hospital, Liver resection, Pancreaticoduodenectomy, Length of stay
Introduction
Every year, over 50%of all patients admitted to hospitals in the USA are admitted to a teaching facility even though teaching hospitals constitute only 24 % of all American Hospital Association registered hospitals and 34 % of all hospitals reporting data to the Agency for Healthcare Research and Quality.1,2 Teaching hospitals differ from non-teaching hospitals in many ways, especially in their focus on integrating medical education as part of patient care.3 Differences in hospital teaching status have been reported to impact treatment choices and patient outcomes.4,5 However, past reports on a wide variety of surgical procedures comparing teaching vs. non-teaching hospitals have shown mixed results regarding whether there are differences between in-hospital outcomes. In general, some studies have suggested that outcomes at teaching hospitals were equivalent to non-teaching hospitals for lower risk procedures and perhaps better for high-risk procedures.4,6–9
Improving outcomes for patients undergoing complex hepatopancreaticobiliary (HPB) procedures is of particular importance. HPB surgery commonly includes procedures such as pancreatoduodenectomy (PD) and distal pancreatectomy, as well as partial and anatomical liver resections. While the mortality associated with these procedures has dramatically decreased over that last several decades, the morbidity remains high, with many studies noting complications between 20 and 50%.10–15 A subset of patients undergoing HPB procedures will also have a prolonged hospital length of stay (LOS), and this longer LOS is associated with higher 30-day readmission rates, which, in turn, is associated with increased morbidity and mortality.16
Previous investigations have largely focused on morbidity and mortality as the dependent variables of interest when examining differences in outcomes among HPB surgical patients. Few studies have investigated other important quality metrics such as LOS.10,17 In turn, most investigators have focused on procedural volume as the factor most associated with morbidity, mortality, and prolonged LOS. For example, studies on short-term in-hospital outcomes following complex thoraco-abdominal surgery have shown an association between higher hospital procedure volume and in-hospital outcomes after controlling for patient- and disease-specific factors.9 Reduced morbidity and mortality following PD at high-volume hospitals have also been documented for pancreatectomy18 and liver resection.19 The risk of in-hospital complications and mortality may, however, be related to other factors not related to hospital procedure volume. In particular, teaching hospitals have fundamentally different processes of patient care as compared to non-teaching institutions, and this may have an impact on in-hospital outcomes especially among patients undergoing complex surgical procedures associated with long in-hospital stays such as HPB procedures.3 To our knowledge, no previous study has explicitly assessed the impact of teaching status on in-hospital outcomes in HPB surgery. Therefore, the objective of the current study was to evaluate the impact of teaching hospital status on in-hospital morbidity, length of stay, and mortality among patients undergoing complex HPB surgical procedures, independent of procedural volume.
Methods
Data Source
We utilized the Nationwide Inpatient Sample (NIS) database, which is maintained and distributed by the Agency for Healthcare Research and Quality as part of the Healthcare Cost and Utilization Project. The NIS database is comprised of an approximately 20 % sample of the nationwide discharges from inpatient care that is designed to be maximally representative of all US hospital admissions. Sampling weights are provided to allow nationwide estimates to be made using the dataset. Patients with missing information on hospital teaching status were excluded.
Study Cohort
Using the corresponding ICD-9 procedure codes, we queried the NIS database for discharge records of patients over 18 years of age undergoing complex HPB procedures at any position within the first 15 procedure code fields—partial hepatectomy (50.22), lobectomy of liver (50.3), hepaticojejunostomy (51.37), proximal pancreatectomy (52.51), distal pancreatectomy (52.52), radical subtotal pancreatectomy (52.53), other partial pancreatectomy (52.59), total pancreatectomy (52.6), or radical pancreaticoduodenectomy (52.7). Complications were identified using ICD-9 diagnostic codes corresponding to the HCUP Clinical Classifications Software for ICD-9-CM.20 Patient characteristics (age group, gender, race, and expected primary payer), procedural characteristics (elective vs. other), and in-hospital outcomes (length of stay, occurrence of complications, and mortality) were noted.
Outcomes of interest—length of stay, complications, and inhospital mortality—were compared between patients discharged from teaching and non-teaching hospitals within the top tertile of yearly procedure volume. Yearly procedure volume was calculated as the number of HPB procedures for each facility during the duration of the study and division of this number by the number of years a particular facility contributed data to the NIS.17
Statistical Analysis
Data were analyzed using SAS 9.3 (SAS Corp., Cary, NC, USA), employing the survey procedures included in the software to account for the complex survey design of the NIS, and national estimates for the USA were abstracted. Standard measures of frequencies and central tendency were calculated to summarize characteristics of patients, procedures, and in-hospital outcomes. Length of stay was summarized as medians (standard error) and compared using the extension of the non-parametric Wilcoxon test for complex survey data described by Natarajan et al.21 P value <0.05 was considered statistically significant.
Results
Description of the Cohort
Between years 2000 and 2010, there were 285,442 inpatient hospital stays linked to a complex HPB procedure. Table 1 presents the demographic and clinical characteristics of this cohort. Briefly, 51.6 % of patients were female, 59.6 % were under 65 years of age, 74.0%were white, 77.3%were admitted on an elective basis, and 70.5 % had a low comorbidity burden. Similar proportion of patients had government (46.4 %) and private insurance (46.7 %) as the primary payer for the hospitalization. Among all patients, 90.0 % were operated upon at hospitals in the top tertile of yearly procedure volume (>25 procedures/year); only a small fraction of patients (1.6 %) were operated upon at hospitals in the lowest tertile of HPB procedure volume (<7 procedure/year). Most procedures were carried out at teaching hospitals (81.0 %).
Table 1.
Demographic and clinical characteristics of patients undergoing major HPB surgical procedures at teaching and non-teaching hospitals
| All (n =285,442) | Teaching (n = 231,232) | Non-teaching (n =54,210) | P-value | |
|---|---|---|---|---|
| Patient age (years) | ||||
| <65 | 170,214 (59.6) | 141,974 (61.4) | 28,240 (52.1) | <0.001 |
| 65–74 | 69,933 (24.5) | 55,611 (24.1) | 14,322 (26.4) | |
| ≥75 | 45,295 (15.9) | 33,647 (14.6) | 11,648 (21.5) | |
| Gender | ||||
| Male | 138,171 (48.4) | 112,620 (48.7) | 25,550 (47.1) | 0.01 |
| Female | 147,271 (51.6) | 118,611 (51.3) | 28,660 (52.9) | |
| Race | ||||
| White | 166,712 (74.0) | 133,641 (73.6) | 33,071 (75.8) | 0.38 |
| Black | 21,141 (9.4) | 17,471 (9.6) | 3,669 (8.4) | |
| Hispanic | 20,260 (9.0) | 16,293 (9.0) | 3,968 (9.1) | |
| Other | 17,097 (7.6) | 14,190 (7.8) | 2,907 (6.7) | |
| Charlson comorbidities | ||||
| ≤2 | 201,351 (70.5) | 165,664 (71.6) | 35,687 (65.8) | <0.001 |
| ≥3 | 84,091 (29.5) | 65,568 (28.4) | 18,524 (34.2) | |
| Elective admission | 191,482 (77.3) | 161,065 (79.1) | 30,417 (68.7) | <0.001 |
| Primary payer type | ||||
| Government | 132,420 (46.4) | 104,471 (45.2) | 27,949 (51.6) | <0.001 |
| Private | 133,340 (46.7) | 110,320 (47.7) | 23,020 (42.5) | |
| Other/none | 19,682 (6.9) | 16,441 (7.1) | 3,241 (6.0) | |
| Region of hospital | ||||
| Northeast | 62,449 (21.9) | 56,665 (24.5) | 5,784 (10.7) | <0.001 |
| Midwest | 63,413 (22.2) | 54,082 (23.4) | 9,330 (17.2) | |
| South | 94,054 (33.0) | 71,794 (31.0) | 22,260 (41.1) | |
| West | 65,527 (23.0) | 48,691 (21.0) | 16,836 (31.1) | |
| Hospital volume Tertile | ||||
| 1st | 4,577 (1.6) | 446 (0.2) | 4,131 (7.6) | <0.001 |
| Middle | 24,048 (8.4) | 6,421 (2.8) | 17,626 (32.5) | |
| 3rd | 256,817 (90.0) | 224,365 (97.0) | 32,453 (59.9) | |
| Procedure type | ||||
| Pancreatoduodenectomy | 79,448 (27.8) | 64,911 (28.1) | 14,538 (26.8) | 0.25 |
| Other pancreatectomy | 73,223 (25.7) | 55,829 (24.1) | 17,394 (32.1) | <0.001 |
| Hepatectomy/lobectomy of liver | 114,126 (40.0) | 94,336 (40.8) | 19,791 (36.5) | 0.01 |
| Hepaticojejunostomy | 25,356 (8.9) | 21,924 (9.5) | 3,432 (6.3) | <0.001 |
Missing data on race for 21.3 % of the sample and on admission designations (elective or otherwise) for 13.0 %
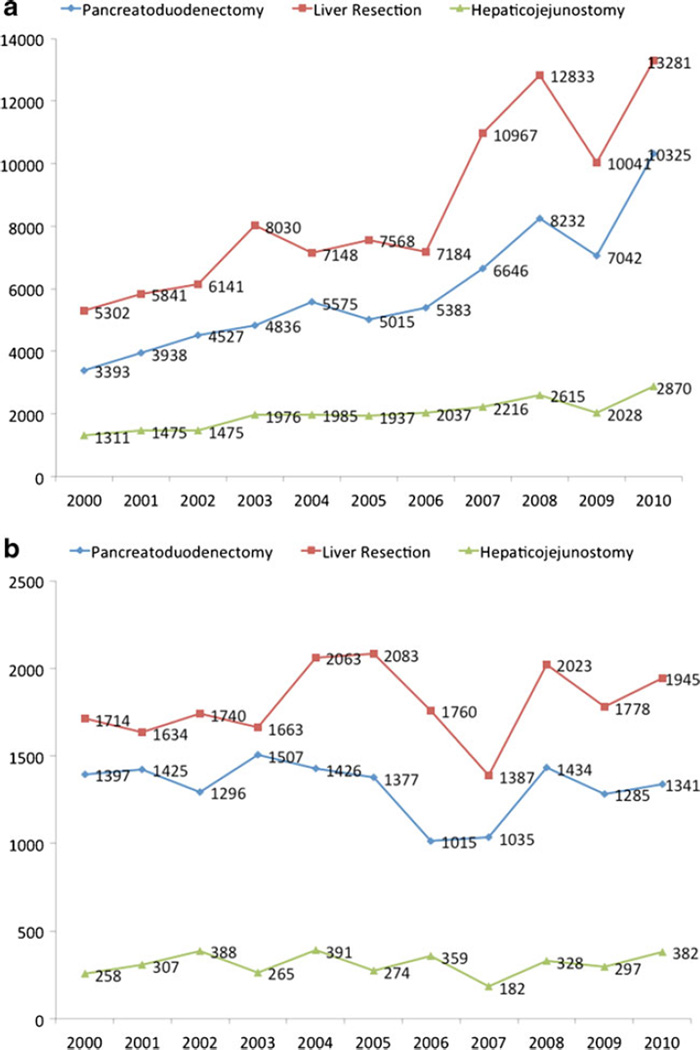
Yearly Trends in Overall Procedure Volumes
In the 11 years considered by the present report, patients underwent 79,448 pancreatoduodenectomies, 73,223 other pancreatic resections, 114,126 liver resections, and 25,356 hepaticojejunostomies. Figure 1 shows the national estimates of frequency of these procedures at teaching (a) and nonteaching (b) hospitals. It is notable that at teaching hospitals, the frequency of pancreatoduodenectomy increased over threefold from 3,393 procedures in year 2000 to 10,325 procedures in year 2010. Similar trends were noted for liver resections which increased from 5,302 to 13,281 over the same time period. Frequency of hepaticojejunostomies doubled between 2000 and 2010. Different trends were noted at non-teaching hospitals—procedure volume for liver resections and hepaticojejunostomy increased slightly between years 2000 (n =1,714 and 258) and 2010 (n =1,945 and 382), respectively. Frequency of pancreatoduodenectomies decreased slightly from 1,397 in year 2000 to 1,341 in year 2010. There was an overall shift of procedures to the teaching hospitals. Among all the hospitals where one or more HPB procedure was performed, the proportion of hospitals with teaching status increased from 34.3 % in year 2000 to 43.1 % in year 2010.
Fig. 1.
Estimated nationwide procedure volume for complex HPB procedures at teaching (a) and non-teaching (b) hospitals
Differences Between Patients at Teaching and Non-teaching Hospitals
Table 1 presents a comparison of the procedures carried out at teaching vs. non-teaching hospitals. Patients at teaching hospitals tended to be younger, and they had a lower comorbidity burden. In fact, patients operated upon at non-teaching hospitals were older (patients <65 years old: non-teaching 52.1 % vs. teaching 61.4 %) and had a higher comorbidity burden (34.2 vs. 28.4 %), as well as fewer elective admissions (68.7 vs. 79.1 %) (all P <0.05). In addition, patients treated at a non-teaching hospital were more likely to have government insurance as the primary payer (51.6 vs. 45.2 %) and live in the Southern USA (41.1 vs. 31.0 %) (both P <0.05).
Ninety-seven percent of the teaching hospitals were in the top tertile of overall hospital procedure volume as compared with only 60 % of the non-teaching hospitals. Table 2 shows the differences in principal diagnoses for patients operated upon at teaching vs. non-teaching hospitals. Non-teaching hospitals were less likely to perform HPB surgery for a principal diagnosis of liver metastasis (9.9 vs. 15.0 %), liver cancer (9.9 vs. 15.0 %), benign liver lesions (1.2 vs. 2.1 %), bile duct obstruction (0.7 vs. 1.2 %), and live donor liver harvesting for transplant (0.1 vs. 1.3 %) of all HPB surgeries (all P <0.05). A smaller proportion of patients at the nonteaching hospitals had a liver resection (36.5 vs. 40.8 %; P = 0.01) and hepaticojejunostomy (6.3 vs. 9.5 %; P <0.001). Of note, 59.9 % of patients undergoing HPB procedures at nonteaching hospitals were operated upon at facilities within the top HPB procedure volume tertile compared with 97.0 % of patients undergoing surgery at teaching hospitals.
Table 2.
Principal diagnosis among patients undergoing major HPB surgical procedures at teaching and non-teaching hospitals
| Teaching (n =231,232) | Non-teaching (n =54,210) | P-value | |
|---|---|---|---|
| Pancreatic cancer | 52,529 (22.7) | 13,367 (24.7) | 0.02 |
| Liver metastases | 34,719 (15.0) | 5,378 (9.9) | <0.001 |
| Liver cancer | 18,089 (7.8) | 2,061 (3.8) | <0.001 |
| Pancreatitis or its sequelae | 15,213 (6.6) | 3,708 (6.8) | 0.59 |
| Bile duct/gallbladder cancer | 14,962 (6.5) | 3,920 (7.2) | 0.02 |
| Benign pancreatic lesion | 11,349 (4.9) | 2,851 (5.3) | 0.29 |
| Carcinoma ampula vater | 6,615 (2.9) | 1,859 (3.4) | 0.01 |
| Benign liver lesions | 4,787 (2.1) | 649 (1.2) | <0.001 |
| Other liver lesions | 2,844 (1.2) | 661 (1.2) | 0.93 |
| Bile duct obstruction | 2,698 (1.2) | 382 (0.7) | <0.001 |
| Live donor liver harvesting | 3,062 (1.3) | 34 (0.1) | <0.001 |
| Other GI malignancies | 2,419 (1.0) | 442 (0.8) | 0.06 |
In-Hospital Outcomes at Teaching vs. Non-teaching Hospitals
Given the well-established volume–outcome relationships for complex HPB surgery, only teaching vs. non-teaching hospitals in the top tertile of overall procedural volume were examined to account for the differences in procedural volume. Table 3 presents the morbidity, mortality, and LOS for the cohort of patients operated upon only at hospitals in the top tertile of HPB volume. Patients undergoing HPB procedures at non-teaching hospitals had a higher incidence of morbidity (32.9 vs. 29.6 %, respectively), with the difference largely being attributable to the frequency of gastrointestinal (12.9 vs. 10.1 %, respectively) and respiratory complications (4.7 vs. 3.2 %, respectively) (all P <0.05). When considering overall mortality for all HPB procedures, patients at non-teaching hospitals were more likely to die during their hospital stay than at teaching hospitals (5.7 vs. 3.9 %, respectively; P < 0.001). A longer median LOS was also noted at non-teaching hospitals compared with teaching hospitals (8.6 vs. 7.7 days; P =0.01). In general, LOS was longer for patients discharged alive following a complication compared with patients who did not suffer a complication (7.1 vs. 11.8 days; P <0.001). Of note, patients suffering a complication at a non-teaching hospital had a longer LOS as compared with patients having a complication at a teaching hospital (12.6 vs. 11.4 days; P = 0.04).
Table 3.
Outcomes among patients at teaching and non-teaching hospital in the top tertiles of procedure volume
| Teaching (n =224,365) | Non-teaching (n =32,453) | P-value | |
|---|---|---|---|
| Complications | |||
| Cardiac complications | 10,752 (4.8) | 1,322 (4.1) | 0.04 |
| Respiratory complications | 7,209 (3.2) | 1,531 (4.7) | <0.001 |
| Gastrointestinal complications | 22,712 (10.1) | 4,186 (12.9) | <0.001 |
| Urinary complications | 2,983 (1.3) | 422 (1.3) | 0.88 |
| Hemorrhage/hematoma | 10,242 (4.6) | 1,590 (4.9) | 0.31 |
| Postoperative infection | 13,639 (6.1) | 1,973 (6.1) | 0.99 |
| Other postoperative complications | 22,418 (10.0) | 3,453 (10.6) | 0.37 |
| Any complication | 66,369 (29.6) | 10,653 (32.9) | 0.01 |
| In-hospital mortality | |||
| All procedures | 8,764 (3.9) | 1,834 (5.7) | <0.001 |
| Pancreatoduodenectomy | 2,743/63,088 (4.3) | 674/9,633 (7.0) | <0.001 |
| Other pancreatectomy | 2,306/53,256 (4.3) | 545/9,106 (6.0) | 0.02 |
| Liver resection | 3,347/92,207 (3.6) | 558/12,444 (4.5) | 0.05 |
| Hepaticojejunostomy | 798/21,523 (3.7) | 104/2,084 (5.0) | 0.20 |
| Length of stay, median (IQR), (days) | |||
| All patients discharged alive | 7.7 (5.4–12.8) | 8.6 (5.7–14.7) | 0.01 |
| Pancreatoduodenectomy | 11.3 (8.0–17.7) | 13.0 (9.0–20.2) | 0.03 |
| Liver resection | 6.0 (4.3–8.6) | 6.3 (4.5–9.7) | 0.20 |
| Hepaticojejunostomy | 8.5 (6.1–14.1) | 9.8 (6.4–16.0) | 0.04 |
| Patients discharged alive without a complication | 6.9 (5.0–10.3) | 7.5 (5.2–11.9) | 0.11 |
| Patients discharged alive following a complication | 11.4 (7.2–19.9) | 12.6 (7.6–21.7) | 0.04 |
| Patients dying in-hospital | 13.0 (4.1–29.1) | 13.1 (4.3–27.3) | 0.81 |
Table 4 presents the results of the univariate and multivariate logistic regression analysis exploring association of teaching status with in-hospital mortality among patients undergoing HPB procedures at hospitals in the top tertile of yearly procedure volume. On univariate analysis, undergoing complex HPB surgery at a non-teaching hospital was associated with an increased risk of in-hospital death (OR 1.47, 95 % CI 1.25– 1.74). Other factors associated with increased risk of mortality were older patient age (OR 2.52, 95 % CI 2.26–2.80), male gender (OR 1.73, 95 % CI 1.59–1.87), higher comorbidity burden (OR 1.49, 95 % CI 1.32–1.68), non-elective admission (OR 3.32, 95 % CI 2.85–4.00), and having a complication during the in-hospital stay (2.53, 95 % CI 2.18–2.95) (all P < 0.05). In contrast, individuals with private insurance had a lower risk of in-hospital mortality (OR 0.45, 95 % CI 0.39– 0.51; P <0.001). After controlling for confounding using multivariate logistic regression, compared with patients who had surgery at a teaching facility, patients undergoing complex HPB surgery at a non-teaching hospital still had a 32 % increased odds of death (OR 1.32, 95 % CI 1.11–1.58; P <0.001). Multivariate adjusted regression analysis also showed that patients operated upon at non-teaching hospitals had a 17 % higher risk of a complication (OR 1.17, 95 % CI 1.02–1.34; P=0.03). Furthermore, patients discharged alive from non-teaching hospitals had a 20% increased risk of having a LOS >14 days (OR 1.20, 95 % CI 1.01–1.45; P=0.04).
Table 4.
Univariate and multivariate logistic regression model exploring association of teaching status with risk of in-hospital death
| Univariate | Multivariate | |||
|---|---|---|---|---|
| OR (95 % CI) | P-value | OR (95 % CI) | P-value | |
| Non-teaching hospital | 1.47 (1.25–1.74) | <0.001 | 1.32 (1.11–1.58) | <0.001 |
| Patient Age (years) | ||||
| <65 | Reference | Reference | ||
| 65–74 | 1.38 (1.22–1.56) | 0.01 | 1.26 (1.07–1.49) | 0.03 |
| ≥75 | 2.52 (2.26–2.80) | <0.001 | 2.18 (1.85–2.56) | <0.001 |
| Male gender | 1.73 (1.59–1.87) | <0.001 | 1.63 (1.46–1.82) | <0.001 |
| Non-white race | 1.24 (1.10–1.41) | <0.001 | 1.08 (0.94–1.25) | 0.27 |
| Charlson comorbidities ≥3 | 1.49 (1.32–1.68) | <0.001 | 1.18 (1.04–1.35) | 0.01 |
| Non-elective admission | 3.36 (2.85–4.00) | <0.001 | 3.23 (2.76–3.78) | <0.001 |
| Primary payer type | ||||
| Government | Reference | Reference | ||
| Private | 0.45 (0.39–0.51) | <0.001 | 0.71 (0.60–0.84) | <0.001 |
| Other/none | 1.11 (0.89–1.38) | 0.13 | 1.27 (1.00–1.60) | 0.05 |
| Procedure | ||||
| Pancreatic surgery | Reference | Reference | ||
| Liver resection | 1.25 (1.09–1.44) | <0.001 | 0.95 (0.83–1.09) | 0.46 |
| Hepaticojejunostomy | 1.13 (0.91–1.40) | 0.26 | 1.35 (1.10–1.66) | <0.001 |
| Any complication | 2.53 (2.18–2.95) | <0.001 | 2.31 (2.01–2.66) | <0.001 |
Discussion
Over the last few decades, there has been an increase in the number of operations performed involving the liver, pancreas, and bile ducts.22 While mortality associated with these complex HPB procedures was considerable in the past, more recently, the incidence of in-patient peri-operative death following HPB surgery has been reported to be less than 3–5 %.18,23,24 Morbidity, however, remains a considerable concern as up to 20–50 % of patients may experience some type of complication following HPB surgery.12,14,25 In turn, in-patient complications can lead to a prolonged hospital LOS and subsequent increased risk of readmission.16 The Center for Medicare & Medicaid Services has increasingly required more transparent reporting of these metrics and has even tied future payments to hospitals based on some of these measures of quality, although this has yet to show any impact on patient outcomes.26 Regardless, there has been an increasing effort toward surgical quality improvement and identification of factors affecting morbidity, mortality, and LOS. In the current study, we chose to examine patients undergoing HPB procedures as these patients often are complex, require a large amount of resources, and can experience significant morbidity. Whereas previous studies have almost exclusively focused on procedural volume relative to outcomes, we investigated the impact of teaching hospital status on mortality, morbidity, and LOS following HPB surgery. Interestingly, we found that most HPB surgical procedures were carried out at teaching hospitals (81.0 %). Furthermore, the number of HPB procedures being done at teaching hospitals increased over the time periods examined. Perhaps more importantly, we also noted that patients undergoing complex HPB surgery at non-teaching hospitals were 32%more likely to die during their hospital stay compared with patients in teaching hospitals, even at high-volume facilities. In addition, patients at teaching hospitals also had fewer complications and an aggregate shorter LOS. Even when patients experienced peri-operative complications, LOS was significantly shorter at teaching hospitals vs. non-teaching hospitals, perhaps suggesting that teaching hospitals may be better equipped to deal with these complications. Collectively, these data are important because they strongly suggest differences in several major quality outcome metrics at teaching vs. non-teaching hospitals.
In-hospital mortality, along with other indicators such as readmission rates, is often used as a surrogate for healthcare quality.27,28 Dimick et al. reported that hospital teaching status was associated with lower in-hospital mortality after complex surgical procedures.9 On final analysis, the authors concluded that the difference in mortality was largely due to hospital procedure volume and not teaching status per se. However, higher patient quality care and outcomes have also been shown at teaching vs. non-teaching hospitals for a variety of other medical conditions not influenced by procedural volume.29 With specific regard to surgical outcomes, some investigators have argued that most hospitals do not perform enough complex surgical procedures to reliably detect differences in mortality as related to healthcare quality.30 To exclude surgical volume as a potential confounder, we expanded on the previous work by Dimick and colleagues by relating hospital teaching status with in-hospital mortality in only hospitals with high-volume HPB surgery. In the current study, we specially did not include volume in the multivariate model. In our opinion, it was not appropriate to adjust for volume in the multivariate model examining the effect of teaching status on outcome. Volume is not a confounder in the relationship between teaching status and certain outcomes such as mortality, morbidity, or LOS. Rather, teaching stay is more likely to be an intermediary in the relationship. Teaching status is highly associated with volume because teaching status has a causal relationship with volume— as teaching status correlates typically with increased volume and not the other way around. If one were to draw a DAG (e.g., drawing and analyzing causal diagrams), it would be evident that volume should not be adjusted for because it is not a confounder—it is an intermediary. Instead, we identified only high-volume hospitals and utilized aggregate data over an 11-year period. This allowed us to detect differences between teaching and non-teaching hospitals with greater accuracy.
In doing this, we showed that even at high-volume facilities, patients undergoing complex HPB surgery at nonteaching hospitals were 32 % more likely to die during their hospital stay than those at teaching hospitals. Furthermore, patients had significantly longer hospital stay, which was largely related to a higher incidence of postoperative gastrointestinal and respiratory complications.
Previous studies have suggested that the subspecialty training of surgeons practicing at teaching hospitals is associated with improved outcomes, although only one study to our knowledge has specifically looked at HPB procedures and showed no effect of subspecialization on patient outcomes.31–33 Certainly, non-teaching hospitals are able to attract subspecialty-trained surgeons, deliver specialty-specific care, and provide the on-site staffing required to improve quality of care. However, as medical care at teaching hospitals has been shown to have an overall higher cost than non-teaching hospitals, the ability of non-teaching hospitals to provide for these extra resources may be limited.34Without the availability of resident physicians and other practitioner trainees whose salaries are subsidized by the government, it may be plausible to consider whether or not nonteaching hospitals can accommodate the added expense of additional trained staff sometime necessary to treat complex HPB patients. Furthermore, the subsidized cost of surgeon trainees has been shown, with proper supervision and training, to have laudable outcomes in complex HPB surgery.35–37 By elucidating the differences in mortality, morbidity, and length of stay following HPB surgery at high-volume teaching hospitals on a national scale, the data presented herein should help in guiding referral practices of complex HPB cases and serve as a benchmark for healthcare quality improvement.
The current study has several limitations that are inherent to many studies utilizing claims and registry data in outcomes research.38 Although errors in procedural codes cannot be completely ruled out, we specifically defined the study cohort based on procedural billing codes, which are known to be more accurate and complete compared with diagnostic codes.39 In the current study, we also classified teaching hospitals by the HCUP designation. It is possible that hospitals did not have surgical training programs and were coded as teaching hospitals based only on non-surgical residency training programs. Several investigators have suggested, however, that teaching status per se is a surrogate for availability of multidisciplinary teams and specialty-specific patient units and services, as well as the presence of medical students, residents, fellows, and advanced practitioners typical of teaching hospitals.8 For example, one previous study reported that adverse outcomes after colon cancer surgery were linked to the presence of cardiac and transplant services, rather than dedicated colorectal services.40 As such, we defined our hospital cohort based on the hospital's overall teaching status designation instead of focusing on the presence of resident or fellows from one specialty.
In conclusion, patients undergoing complex HPB surgery at high-volume teaching hospitals have shorter length of stay, fewer gastrointestinal and respiratory complications, and lower in-hospital mortality compared with high-volume non-teaching hospitals. There is a need to further explore the differences between patient-, disease-, facility-, and provider-related factors leading to this discrepancy. In order to improve outcomes on a national scale, the referral patterns for complex HPB diseases must continue to focus on patients being cared for at hospitals with specialty-specific units, critical-care trained nurses, and on-site availability of multidisciplinary teams. Improvement of surgical quality needs to be a focus for all facilities providing surgical services and not isolated to teaching hospitals.
References
- 1.Association of American Medical Colleges; 2010. Data on teaching hospitals and charity care. [Google Scholar]
- 2.Sorra J, et al. Rockville, MD: Agency for Healthcare Research and Quality; 2012. Hospital Survey on Patient Safety Culture: 2012 User Comparative Database Report. [Google Scholar]
- 3.Khuri SF, et al. Comparison of surgical outcomes between teaching and nonteaching hospitals in the Department of Veterans Affairs. Ann Surg. 2001;234(3):370–382. doi: 10.1097/00000658-200109000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stewart DB, et al. Rectal Cancer and Teaching Hospitals: Hospital Teaching Status Affects Use of Neoadjuvant Radiation and Survival for Rectal Cancer Patients. Annals of Surgical Oncology. 2013;20(4):1156–1163. doi: 10.1245/s10434-012-2769-5. [DOI] [PubMed] [Google Scholar]
- 5.Grosskopf S, Margaritis D, Valdmanis V. Comparing teaching and non-teaching hospitals: a frontier approach (teaching vs. nonteaching hospitals) Health Care Manag Sci. 2001;4(2):83–90. doi: 10.1023/a:1011449425940. [DOI] [PubMed] [Google Scholar]
- 6.Koval KJ, Rust CL, Spratt KF. The effect of hospital setting and teaching status on outcomes after hip fracture. Am J Orthop (Belle Mead NJ) 2011;40(1):19–28. [PubMed] [Google Scholar]
- 7.Lee SL, Yaghoubian A, de Virgilio C. A Multi-Institutional Comparison of Pediatric Appendicitis Outcomes Between Teaching and Nonteaching Hospitals. Journal of Surgical Education. 2011;68(1):6–9. doi: 10.1016/j.jsurg.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Meguid RA, et al. Are surgical outcomes for lung cancer resections improved at teaching hospitals? Annals of Thoracic Surgery. 2008;85(3):1015–1025. doi: 10.1016/j.athoracsur.2007.09.046. [DOI] [PubMed] [Google Scholar]
- 9.Dimick JB, et al. Hospital teaching status and outcomes of complex surgical procedures in the United States. Arch Surg. 2004;139(2):137–141. doi: 10.1001/archsurg.139.2.137. [DOI] [PubMed] [Google Scholar]
- 10.Hyder O, et al. A risk model to predict 90-day mortality among patients undergoing hepatic resection. J Am Coll Surg. 2013;216(6):1049–1056. doi: 10.1016/j.jamcollsurg.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhayani NH, et al. Effect of metabolic syndrome on perioperative outcomes after liver surgery : A National Surgical Quality Improvement Program (NSQIP) analysis. Surgery. 2012;152(2):218–226. doi: 10.1016/j.surg.2012.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwartz GS, et al. Morbidity and mortality after hepatic and pancreatic resections: results from one surgeon at a low-volume urban hospital over thirty years. Am J Surg. 2011;201(4):438–444. doi: 10.1016/j.amjsurg.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Sato M, et al. Mortality and morbidity of hepatectomy, radiofrequency ablation, and embolization for hepatocellular carcinoma: a national survey of 54,145 patients. J Gastroenterol. 2012;47(10):1125–1133. doi: 10.1007/s00535-012-0569-0. [DOI] [PubMed] [Google Scholar]
- 14.Kim JH, et al. Surgical Outcomes of Distal Pancreatectomy. Hepatogastroenterology. 2013;60(126) doi: 10.5754/hge13260. [DOI] [PubMed] [Google Scholar]
- 15.Zhou W, et al. Stapler vs suture closure of pancreatic remnant after distal pancreatectomy:ameta-analysis. Am J Surg. 2010;200(4):529–536. doi: 10.1016/j.amjsurg.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 16.Schneider EB, et al. Patient readmission and mortality after surgery for hepato-pancreato-biliary malignancies. J Am Coll Surg. 2012;215(5):607–615. doi: 10.1016/j.jamcollsurg.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schneider EB, et al. Provider versus patient factors impacting hospital length of stay after pancreaticoduodenectomy. Surgery. 2013 doi: 10.1016/j.surg.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 18.McPhee JT, et al. Perioperative mortality for pancreatectomy: a national perspective. Ann Surg. 2007;246(2):246–253. doi: 10.1097/01.sla.0000259993.17350.3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kohn GP, Nikfarjam M. The effect of surgical volume and the provision of residency and fellowship training on complications of major hepatic resection. J Gastrointest Surg. 2010;14(12):1981–1989. doi: 10.1007/s11605-010-1310-z. [DOI] [PubMed] [Google Scholar]
- 20.(HCUP), H.C.a.U.P. Clinical Classifications Software (CCS) for ICD-9-CM. 2013 [cited 2013 05/27]; Available from: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 21.Natarajan S, et al. An extension of the Wilcoxon rank sum test for complex sample survey data. Journal of the Royal Statistical Society Series C-Applied Statistics. 2012;61:653–664. doi: 10.1111/j.1467-9876.2011.01028.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nathan H, et al. The volume-outcomes effect in hepato-pancreato-biliary surgery: hospital versus surgeon contributions and specificity of the relationship. J Am Coll Surg. 2009;208(4):528–538. doi: 10.1016/j.jamcollsurg.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 23.Kim CG, Jo S, Kim JS. Impact of surgical volume on nationwide hospital mortality after pancreaticoduodenectomy. World J Gastroenterol. 2012;18(31):4175–4181. doi: 10.3748/wjg.v18.i31.4175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dimick JB, et al. Hepatic resection in the United States: indications, outcomes, and hospital procedural volumes from a nationally representative database. Arch Surg. 2003;138(2):185–191. doi: 10.1001/archsurg.138.2.185. [DOI] [PubMed] [Google Scholar]
- 25.Fisher SB, et al. A comparison of right posterior sectorectomy with formal right hepatectomy: a dual-institution study. HPB (Oxford) 2013 doi: 10.1111/hpb.12126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jha AK, et al. The long-term effect of premier pay for performance on patient outcomes. N Engl J Med. 2012;366(17):1606–1615. doi: 10.1056/NEJMsa1112351. [DOI] [PubMed] [Google Scholar]
- 27.AHRQuality Indicators. Inpatient Quality Indicators Technical Specifications. Rockville, Maryland: Agency for Healthcare Research and Quality; 2013. May, Version 4.5. [Google Scholar]
- 28.Milstein A, et al. Improving the safety of health care: the leapfrog initiative. Eff Clin Pract. 2000;3(6):313–316. [PubMed] [Google Scholar]
- 29.Mueller SK, Lipsitz S, Hicks LS. Impact of hospital teaching intensity on quality of care and patient outcomes. Med Care. 2013;51(7):567–574. doi: 10.1097/MLR.0b013e3182902151. [DOI] [PubMed] [Google Scholar]
- 30.Dimick JB, Welch HG, Birkmeyer JD. Surgical mortality as an indicator of hospital quality: the problem with small sample size. JAMA. 2004;292(7):847–851. doi: 10.1001/jama.292.7.847. [DOI] [PubMed] [Google Scholar]
- 31.Gopaldas RR, et al. Impact of surgeon demographics and technique on outcomes after esophageal resections: a nationwide study. Ann Thorac Surg. 2013;95(3):1064–1069. doi: 10.1016/j.athoracsur.2012.10.038. [DOI] [PubMed] [Google Scholar]
- 32.Ben-Haim M, Nakache R, Klausner JM. [Hepato-pancreato-biliary (HPB) surgery and abdominal organ transplantation, a defined subspecialty, integrated within the surgical division: professional, operative and educational aspects] Harefuah. 2009;148(4):215–218. 278. [PubMed] [Google Scholar]
- 33.Csikesz NG, et al. Surgical specialization and operative mortality in hepato-pancreatico-biliary (HPB) surgery. J Gastrointest Surg. 2008;12(9):1534–1539. doi: 10.1007/s11605-008-0566-z. [DOI] [PubMed] [Google Scholar]
- 34.Taylor DH, Jr, Whellan DJ, Sloan FA. Effects of admission to a teaching hospital on the cost and quality of care for Medicare beneficiaries. N Engl J Med. 1999;340(4):293–299. doi: 10.1056/NEJM199901283400408. [DOI] [PubMed] [Google Scholar]
- 35.Castleberry AW, et al. Resident Education in the Era of Patient Safety: A Nationwide Analysis of Outcomes and Complications in Resident -Assisted Oncologic Surgery. Ann Surg Oncol. 2013 doi: 10.1245/s10434-013-3079-2. [DOI] [PubMed] [Google Scholar]
- 36.Kiran RP, et al. Impact of resident participation in surgical operations on postoperative outcomes : National Surgical Quality Improvement Program. Ann Surg. 2012;256(3):469–475. doi: 10.1097/SLA.0b013e318265812a. [DOI] [PubMed] [Google Scholar]
- 37.Jurgaitis J, et al. Controlled-surgical education in clinical liver transplantation is not associated with increased patient risks. Clin Transplant. 2006;20(Suppl 17):69–74. doi: 10.1111/j.1399-0012.2006.00603.x. [DOI] [PubMed] [Google Scholar]
- 38.Nathan H, Pawlik TM. Limitations of claims and registry data in surgical oncology research. Annals of Surgical Oncology. 2008;15(2):415–423. doi: 10.1245/s10434-007-9658-3. [DOI] [PubMed] [Google Scholar]
- 39.SEER-Medicare Training. 2013 [cited 2013; Available from: http://healthservices.cancer.gov/seermedicare/considerations/training.html.
- 40.Billingsley KG, et al. Surgeon and hospital characteristics as predictors of major adverse outcomes following colon cancer surgery: understanding the volume-outcome relationship. Arch Surg. 2007;142(1):23–31. doi: 10.1001/archsurg.142.1.23. discussion 32. [DOI] [PubMed] [Google Scholar]