Inflammatory bowel disease (IBD) is associated with several dermatologic manifestations, of which the most commonly cited are erythema nodosum and pyoderma gangrenosum. Pyoderma faciale (PF) is a dermatologic condition characterized by a fulminant eruption of inflammatory papules, pustules, and nodules on the face. PF is usually diagnosed in young women and is thought by some doctors to be a variant of rosacea. We present a case of a patient with longstanding inflammatory ileal Crohn’s disease (CD) with complex perianal fistula who presented with the onset of PF while undergoing fistula treatment.
Case Report
A white man, age 34 years, with a history of inflammatory ileal CD with complex perianal fistula was referred to our institution for further management. He received a diagnosis of CD at age 12 years and was initially treated with sulfasalazine with good results. From age 15—32 years, he was in remission and off medical therapy. At age 32 years, abdominal pain, bloating, obstipation, and nausea developed. He was started on mesalamine and ciprofloxacin, with marked improvement in symptoms. A colonoscopy demonstrated active ileitis and a large polypoid lesion with central ulceration at the ileocecal valve. Biopsies of the polypoid lesion did not reveal dysplasia. Two years later, the abdominal pain recurred. A repeat colonoscopy demonstrated that the polypoid lesion was still present and had increased in size. Biopsies of the mass showed acute and chronic inflammation with atypical cells that were suspicious for intramural adenocarcinoma. A repeat colonoscopy at our institution confirmed these findings and demonstrated a draining right lateral perianal fistula. The patient had no evidence of macroscopic or microscopic colitis in the distal colon. He underwent a laparoscopic right hemicolectomy and ileal resection. Pathology demonstrated a poorly differentiated mucinous adenocarcinoma. The cecum surrounding the tumor demonstrated transmural inflammation and granuloma formation.
Postoperatively, the patient was continued on oral mesalamine 2.4 g twice daily. A midline perianal abscess developed, which was treated with oral ciprofloxacin and metronidazole 500 mg twice daily. The patient was continued on metronidazole, but recurrent midline pain and swelling developed. He was presumed to have an infected pilonidal cyst because no fistulous connection could be demonstrated on 2 examinations under anesthesia (EUAs). A new lateral fistula developed, which was treated with an increase in dosage of antibiotics. The patient continued to report perianal pain, and multiple draining fistulae subsequently developed. A repeat EUA was performed with the placement of 5 setons. Infliximab (IFX; Remicade, Janssen Biotech) was given at a dose of 5 mg/kg at Weeks 0, 2, and 6 and then every 8 weeks for maintenance. The patient had a partial response to therapy. Subsequently, 1 seton became dislodged, and recurrent perianal symptoms developed. Amoxicillin/clavulanate was added to the therapeutic regimen without significant improvement. IFX was increased to 10 mg/kg every 6 weeks, and azathioprine was started at 2.5 mg/kg/day and escalated to 3 mg/kg/day without significant improvement. Subcutaneous methotrexate 25 mg weekly was initiated. The patient underwent another EUA with multiple fistulotomies. He entered complete remission and has not had recurrent perianal symptoms.
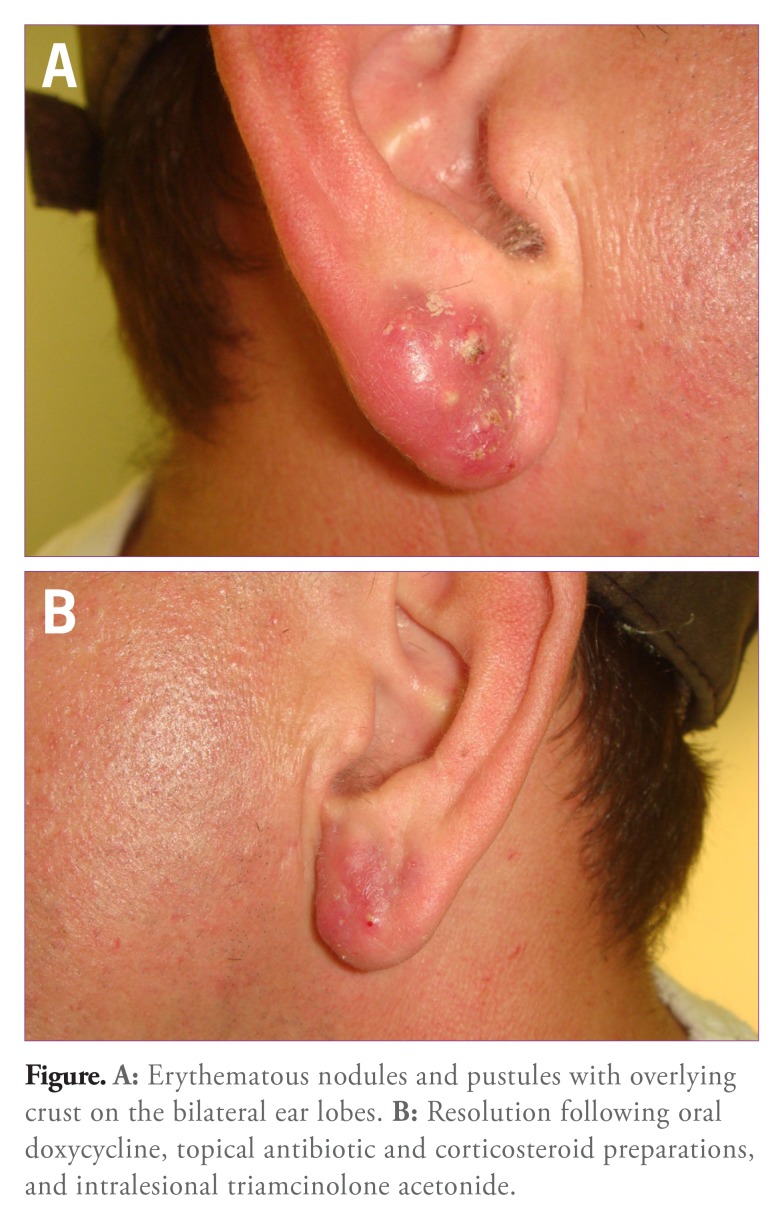
Following 6 months of IFX therapy, a cystic lesion developed on the patient’s left ear that was excised by a general surgeon. Subsequently, a similar lesion developed just below the site of the initial cyst. In addition, multiple tender erythematous nodules and pustules developed on the bilateral ear lobes (Figure A). The patient was evaluated by specialists in the Department of Dermatology due to concern about anti—tumor necrosis factor (TNF)-induced psoriasis. Localized PF limited to the ear lobes was diagnosed. A bacterial culture was obtained from 1 of the pustules and revealed normal skin flora. The patient was given oral doxycycline, topical antibiotic and corticosteroid preparations, and serial intralesional triamcinolone acetonide injections, resulting in slow but progressive improvement of dermatologic symptoms (Figure B).
Figure.
A: Erythematous nodules and pustules with overlying crust on the bilateral ear lobes. B: Resolution following oral doxycycline, topical antibiotic and corticosteroid preparations, and intralesional triamcinolone acetonide.
Discussion
PF, also known as rosacea fulminans, is a rare dermatologic condition that is classically characterized by eruptive inflammatory papules, pustules, nodules, and cysts on the face. Its exact cause is unclear, but it is considered by some doctors to be an acute presentation of rosacea.1 Facial edema can be associated with the lesions, and draining sinuses are frequently seen.1 In addition, the neck, shoulders, chest, and upper arms also can be involved, with lesions typically being asymptomatic.1 The condition has been almost exclusively reported in women who often have a history of rosacea. The lesions have been successfully treated with a combination approach, including oral and topical corticosteroids in addition to tetracycline antibiotics. Isotretinoin has been used successfully in patients with refractory disease. However, recent studies suggest a possible association between isotretinoin use and IBD.2
PF has been infrequently reported in patients with IBD.3-6 Two case reports noted successful treatment of the PF lesions with isotretinoin despite concurrent IBD; no exacerbation of IBD was noted.4,5 To our knowledge, this is the fifth case of PF reported in a patient with IBD. In our case, the lesions developed while the patient was receiving antibiotic and IFX therapy for treatment of perianal CD. The patient was treated conventionally with both topical corticosteroids and tetracycline antibiotics, with good response. Our case of PF was unusual in that the lesions were limited to the ears and occurred in a male patient.
Our case highlights several key points for clinicians who treat patients with IBD. First, clinicians should be aware of common skin-related extraintestinal manifestations (EIMs), as they occur in 3-8% of patients with CD.7 Second, providers should be able to recognize PF because it can be confused with other skin EIMs and adverse effects of IFX therapy. For example, pyoderma gangrenosum would be considered in a patient with draining sinus tracts. Because PF can involve skin surfaces other than the face, both of these disorders would be in the differential diagnosis. Second, although unusual in IBD, Sweet syndrome, characterized by erythematous papules and plaques on the face, neck, and upper extremities, could be confused with PF.8,9 Sweet syndrome can be distinguished from PF by the presence of fever and neutrophilia as well as the finding of a dermal neutrophilic infiltration on biopsy. Lastly, a pustular variant of psoriasis that can involve the hands, feet, and scalp can develop in patients on anti-TNF therapy. As mentioned, psoriasiform eruptions associated with anti-TNF use are usually pustular and have a different distribution than PF, which should distinguish most cases of PF from those of psoriasiform lesions.10 PF should be suspected in young women with a history of rosacea involving the face, neck, chest, and upper arms. Prompt referral to a dermatology specialist is recommended to confirm the diagnosis. If differentiation from other skin EIMs in IBD is difficult, a skin biopsy can be performed.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Plewig G, Jansen T, Kligman AM. Pyoderma faciale. A review and report of 20 additional cases: is it rosacea? Arch Dermatol. 1992;128(12):1611–1617. doi: 10.1001/archderm.128.12.1611. [DOI] [PubMed] [Google Scholar]
- 2.Crockett SD, Porter CQ, Martin CF, Sandler RS, Kappelman MD. Isotretinoin use and the risk of inflammatory bowel disease: a case-control study. Am J Gastroenterol. 2010;105(9):1986–1993. doi: 10.1038/ajg.2010.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McHenry PM, Hudson M, Smart LM, Rennie JA, Mowat NA, White MI. Pyoderma faciale in a patient with Crohn’s disease. Clin Exp Dermatol. 1992;17(6):460–462. doi: 10.1111/j.1365-2230.1992.tb00262.x. [DOI] [PubMed] [Google Scholar]
- 4.Dessoukey MW, Omar MF, Dayem HA. Pyoderma faciale: manifestation of inflammatory bowel disease. Int J Dermatol. 1996;35(10):724–726. doi: 10.1111/j.1365-4362.1996.tb00647.x. [DOI] [PubMed] [Google Scholar]
- 5.Rosen T, Unkefer RP. Treatment of pyoderma faciale with isotretinoin in a patient with ulcerative colitis. Cutis. 1999;64(2):107–109. [PubMed] [Google Scholar]
- 6.Gatzka M, Simon M, Schuler G, Luftl M. Rosacea fulminans, pyostomatitis and pyovulvitis in Crohn’s disease: dapsone as key factor in combination therapy [in German] Hautarzt. 2006;57(10):898–902. doi: 10.1007/s00105-005-1017-3. [DOI] [PubMed] [Google Scholar]
- 7.Rankin GB, Watts HD, Melnyk CS, Kelley ML., Jr. National Cooperative Crohn’s Disease Study: extraintestinal manifestations and perianal complications. Gastroenterology. 1979;77(4 pt 2):914–920. [PubMed] [Google Scholar]
- 8.Ytting H, Vind I, Bang D, Munkholm P. Sweet’s syndrome—an extraintestinal manifestation in inflammatory bowel disease. Digestion. 2005;72(2-3):195–200. doi: 10.1159/000088466. [DOI] [PubMed] [Google Scholar]
- 9.All M, Duerksen DR. Ulcerative colitis and Sweet’s syndrome: a case report and review of the literature. Can J Gastroenterol. 2008;22(3):296–298. doi: 10.1155/2008/960585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cullen G, Kroshinsky D, Cheifetz AS, Korzenik JR. Psoriasis associated with anti-tumour necrosis factor therapy in inflammatory bowel disease: a new series and a review of 120 cases from the literature. Aliment Pharmacol Ther. 2011;34(11-12):1318–1327. doi: 10.1111/j.1365-2036.2011.04866.x. [DOI] [PubMed] [Google Scholar]